Abstract
Objectives:
The use of non-prescribed antibiotics has become a public health concern, and this behavior continues to thrive in many countries of the world including Nigeria. Evidence from previous studies suggests that increased antibiotic prescriptions and patients’ past experiences are some of the factors contributing to the use of non-prescribed antibiotics. The present investigation was aimed at determining the factors driving this behavior and the extent of usage among people living in a sub-urban Nigerian community.
Methods:
A community-based, cross-sectional study was conducted in Nsukka, South-East Nigeria using a semi-structured and self-administered questionnaire. An estimated sample size of approximately 400 respondents, with ages ranging from 18 to 60 years participated in the study. A number of males were 233 and 197 were females.
Results:
Demographics showed that the majority of respondents were well educated. The behavior appeared to be common regardless of gender, age, and educational level. Results showed that more than 86% of the respondents use non-prescribed antibiotics for treatment or prevention or both. A significant percentage uses it to treat cold and cough. The most frequently used antibiotics where the penicillins (58%) followed by quinolones (22%). Tetracycline, aminoglycosides, and cephalosporin represented 20.75%, 14.75%, and 11% usage, respectively.
Conclusion:
This study revealed a substantial use of over-the-counter antibiotics, with this behavior cutting across gender, age and levels of education. However, participants’ knowledge and awareness of the hazards associated with this behavior were lacking.
Keywords: Antibiotics, bacteria, non-prescription use, resistance, self-medication
Background
Since the discovery of antibiotics by Alexander Fleming, this class of drugs has played significant roles in the treatment of bacterial infections. Over the years post-discovery, the use of antibiotics has improved clinical outcomes in the treatment of bacterial infections as well as transforming positively the management of infectious diseases. However, the effectiveness of these profoundly important agents has diminished in recent time due to reduced response of bacteria to the drugs as is reported.[1] Researchers[2,3] blamed this phenomenon on inappropriate use of antibiotic as self-medication. In Turkey, the rate of inappropriate use of antibiotics in their hospitals is reported to be on the increase.[4] This has resulted in the emergence of resistant bacteria manifesting in nosocomial infections. Thus creating a situation which could affect the microbial environment of the hospital, negatively.[4] Literature reveals that the use of non-prescribed antibiotics appears to be rampant across developing economies. In Brazil, they are purchased from vendors, while in Bangladesh, reports show that 95% of antibiotics are used without a prescription.[5,6] In Ghana, the situation is not different as a significant number of the populace were reported to purchase non-prescribed antibiotics from the open market.[7] Thus, the development of bacterial resistance to antimicrobials could be due to a fallout of non-prescribed use of antibiotics.[8] The consequences of this irrational use of antibiotics have been known to be associated with poor prognosis as well as safety issues. Both the developed and underdeveloped nations of the world seem not to be exempted from this phenomenon as earlier reports[9] indicated the use of non-prescribed antibiotics in developed countries such as the US and Europe. It is stipulated that in the US and Europe, self-medication practices have been reported especially for diseases such as colds and other upper respiratory tract viral infections.[9] This attitude of self-medicating is[10] unnecessary in most cases, tending to lead to the likelihood of insufficient and incorrect drug dosage. Thus, the use of antibiotics without prescription or guidance is extremely grave, a leading cause in the emergence and subsequent spread of resistance by bacteria to antimicrobials as well as constituting to a major global public health problem.[11] Report shows that about 50% of antibiotics used worldwide are non-prescribed and are sourced from community pharmacies and in other cases, from street vendors.[12] In the developing economies, the situation of antibiotic self-medication is widespread due to the high cost of health care, which is unaffordable to the populace. In addition, there are no adequate regulations, and when available, the laws are not being enforced.[13] The extent and subsequent effects of self-medication worldwide are unknown, and this could be due to both non-prescription antibiotic usage as well as the attitude of pharmacist.[14] There is no doubt that one of the key drivers of bacterial resistance is as a result of irrational antibiotic use with researchers[15] describing this relationship as a complex one. Studies have also shown that resistance to an antibiotic can be transferred among people including relations and coworkers, which could portend dangers of hard to treat infections within a community. Vulnerable individuals such as children, elderly and people with diseases will be at risk of drug failure. Part of the problems associated with self-medication is related to knowledge, attitudes and beliefs, all of which are said to influence this behavior.[16]
A recent study conducted in Nsukka on the antibiotic susceptibility pattern of Staphylococcus aureus isolated from University students displayed a varying degree of resistance with the highest seen with beta-lactam antibiotics.[17] In addition, bacteria isolated from diabetic wounds from the same study area revealed multidrug-resistant S. aureus.[18] This points to the fact that there is the presence of multidrug-resistant (MDR) bacterial isolates in this region. Therefore, to preserve antibiotic effectiveness and ensure their continuous clinical benefits, a paradigm shift in community attitudes regarding the use of non-prescribed antibiotics and consequences will be an important approach. Objective of this study was to survey and estimate the extent, prevalence, attitude, and trends in the use of non-prescription antibiotics and awareness of its potential consequences among the Nsukka population of South Eastern Nigeria. The study also looked into identifying the drivers of non-prescription antibiotic use among the community where possible.
Materials and Methods
Ethical approval
Both verbal and written consent was obtained from participants before administering the questionnaire/interview, and the purpose of the study explained in details. The Department of Microbiology, School of Basic Medical Sciences Ethical Committee for Research, University of Nigeria, Nsukka, approved the study protocol and each interviewee identity was held in confidence.
Study design
This study was conducted at Nsukka, in the South-Eastern region of Nigerian. Nsukka is a University town with a high population of first university degree holders. The town is located in Nsukka local government area of Enugu state. It lies between with borders of Eastern region and middle belt part of Nigeria. It is estimated that about 89% of its inhabitant’s age is between 18 years and above. Interviews were conducted in both the local language (Igbo) of the region and English language. The questionnaire was semi-structured and self-administered.
Sample size
A convenient sample method was used as an approach for the recruitment of respondents for the study. Using the online sample size calculator, i.e., RaoSoft®, minimum effective sample 377 was calculated at the confidence interval of 95% (RaoSoft).[19] However, to minimize the chance of error, a total of n = 450 respondents were approached for their participation in this study. Of whom n = 400 agreed to respond to the questionnaires. The inclusion criteria were for those within the age range of 18 and above. In addition, they must have been local residents of the community for at least 1 year.
Method
A cross-sectional study tool was designed in the form of semi-structured interview/questionnaire guide and was administered to male and female participants. The study was conducted for 7 months from March 2012 to September 2012. Using a 17-item questionnaire, the first four-item mainly addressed the demography of respondents and their health status. The remaining 13 items, explored the respondents’ rationale for the use of non-prescribed antibiotics, sources and what common antibiotic they usually purchase over-the-counter. In addition, the questionnaire also addressed issues such as how often these drugs are purchased, respondent’s knowledge and awareness of subsequent consequences.
Statistical analysis
Data collected were analyzed with the aid of SPSS version 19, 2012. Descriptive statistics were expressed as frequency and percentages. Associations of dependent (use of non-prescription antibiotics) with independent variables were evaluated. Pearson Chi-square test was used to identify the relationship between usage and other variables as well as between groups. It was also used to test for significant association between them, which was set at P < 0.05.
Results
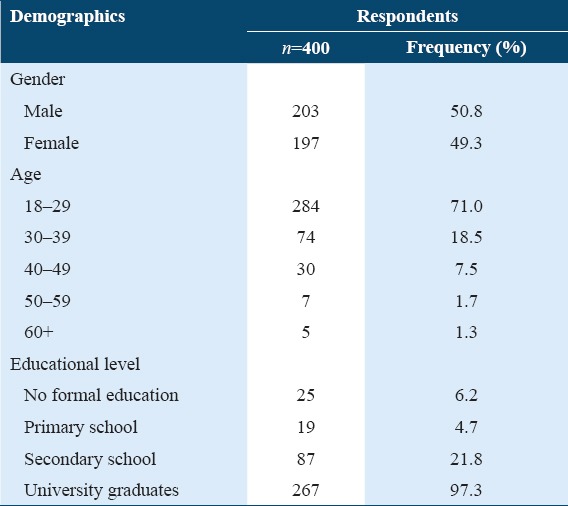
A total of 400 adults participated in the survey. Of these, 203 were males and 197 females. All participants were group into four demographic details as shown in Table 1. The highest numbers of participants were aged between 18 and 29 years, constituting 71% of the study group. The age group of between 40–49 and 50–59 was the least, constituting, 7.5% and 7.25%, respectively, of the participants. About the educational status of the participants, 67.3% of them were university graduates with an at least first degree, 6.3% said they had received no formal education while secondary and primary school certificate holders were 21.8% and 4.8%, respectively, as shown also in Table 1. However, there were no significant differences between levels of education, usage and knowledge. Furthermore, age and gender did not have any significant effect on usage. This means that everybody is involved in this behavior regardless of gender, age, and educational level.
Table 1.
Demographic information of respondents
Diseases for which non-prescribed antibiotics were used
Antibiotics were said to have been taken for ailments such as asthma (5.7%), sore throat (13.8%), cold and cough (42.7%), acne (13.3%), fever (16%), diarrhea, and wound healing (3.2%) [Figure 1]. In general, 35.3% of the participants had employed the use of antibiotics for the treatment of illness while 39.8% for both treatment and prevention. The reasons for using non-prescription antibiotics showed a good association with usage (P < 0.01), particularly for cold and cough.
Figure 1.
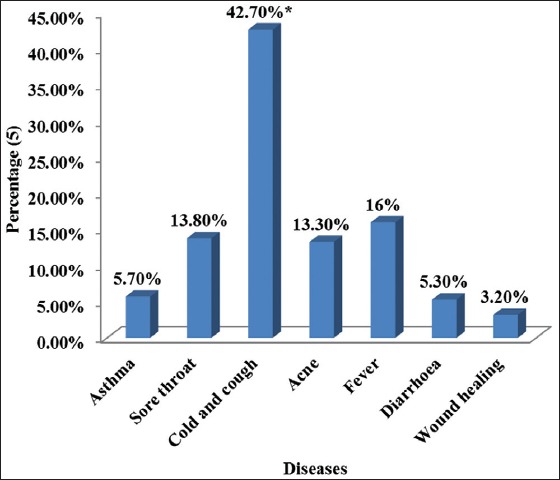
Display of different disease states, the reasons why respondents use non-prescribed antibiotics (*P < 0.01)
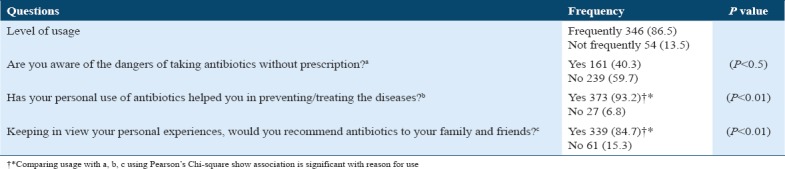
Results for the reason, knowledge, attitude, and frequency and the driving factors for the use of non-prescribed antibiotics are presented in Table 2.
Table 2.
Usage, reasons, knowledge, attitude, frequency and factors driving the use of non-prescription antibiotics by respondents
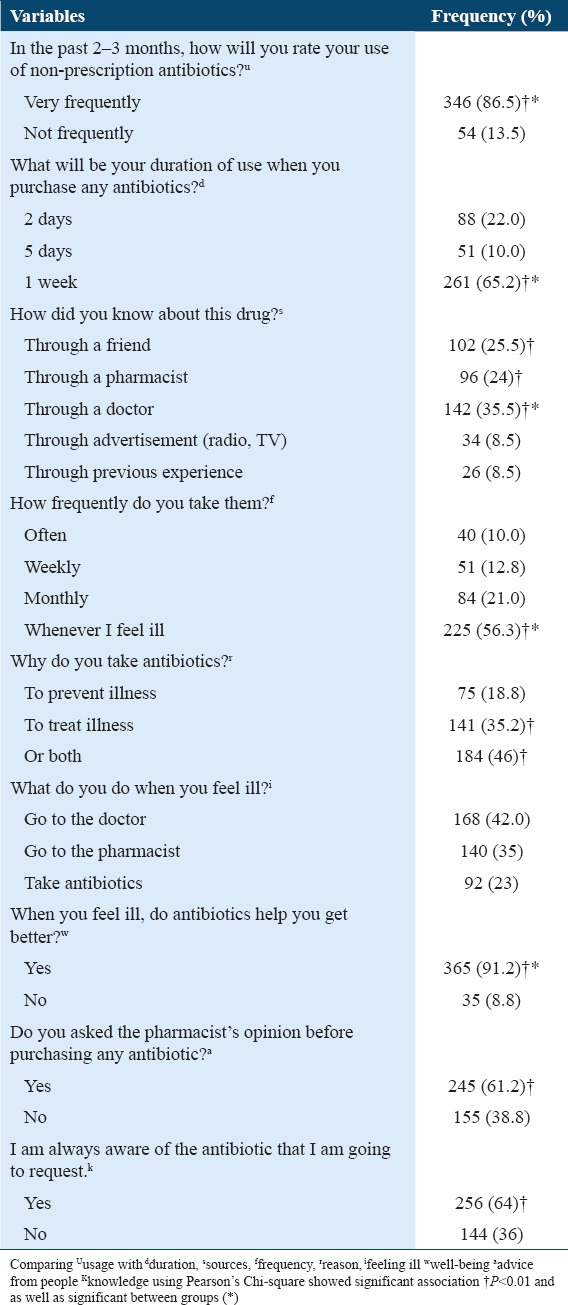
Frequency and duration of using non-prescribed antibiotics
Results on the rate of antibiotics usage within 2–3 months before the study showed that 86.5% of the participants used non-prescribed antibiotics frequently while 13.5% were not frequent users. The length of time for which these antibiotics were used appeared to vary, ranging from 1 week to as long as a month. Some (10%) said often, others (12.8%) weekly, 21% said monthly while the majority (56.3%) overwhelmingly said whenever they felt unwell. The frequency and duration exhibited by participants showed a statistical significance difference (P < 0.01), and good association with usage and the results are presented in Table 2.
Source of knowledge and usage
Table 2 also shows the results on how the participants came to know about the drugs they used. These sources of information were either through information from friends (18.8%) or from the pharmacist (24%) or through previous visits to their doctors or general practitioner (GP) (35%). Some of the participants (6.6%) did not give their source of information. 8.5% each of the respondents had their information from radio and television advertisements as well as experience from the previous usage. Statistical analysis on sources of knowledge of antibiotics showed a good relationship with usage (P < 0.01). In addition, knowledge and usage had a good association with a significant difference at P < 0.001. The results also indicated that due to participants’ knowledge of antibiotics, they were used for both prevention and treatment, and this was significant compared with usage (P < 0.05). The feeling of well-being expressed by participants after use in sickness, showed a significant difference when compared with knowledge and usage (P < 0.01).
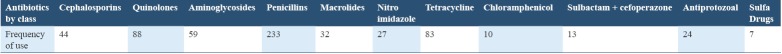
Types and frequency of antibiotics used
Antibiotics bought by participants without prescription within 2–3 months of the investigation were grouped into 11 classes as shown in Table 3. The result shows that usage of non-prescription antibiotics cuts across the entire spectrum of different antimicrobial agents. However, beta-lactam agents appear to be frequently used, in particular penicillin. Penicillin (58%) was the most regularly used antibiotics, followed by quinolones (22%). Tetracycline, aminoglycosides, and cephalosporin had 20.75%, 14.75%, and 11%, respectively [Figure 2]. Statistically, there was a positive correlation when knowledge, frequency, and disease were compared. In relation with usage, results were
Table 3.
Types of non-prescribed antibiotics commonly purchased by the participants
Figure 2.
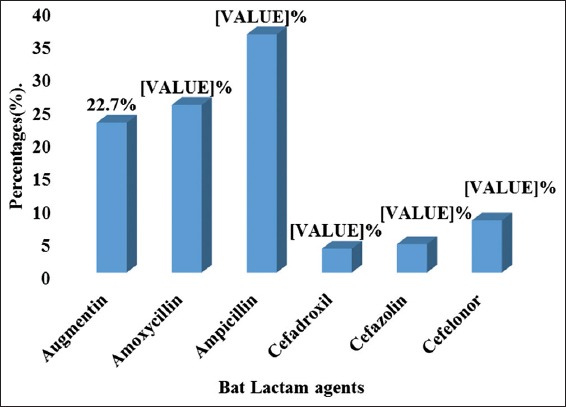
Illustrates the breakdown of different beta-lactam agents used for self-medication highly significant (P < 0.002).
Prior awareness of the adverse effects
In terms of awareness on adverse effects from the use of non-prescribed antibiotics by the respondents, results showed that 40.3% of them were aware of the consequences of this behavior while about half (59.7%) indicate that they were not aware. Therefore, not understanding the attendant consequences of this behavior shows that participants appear to be ignorant and the prognosis is not good. In addition, a high percentage (75.5%) of the respondents affirmed that personal use of antibiotics had helped them in either prevention or treatment of diseases, which appeared to be significant (P < 0.05). Based on their personal experiences, more of them (82%) said they would recommend antibiotics to their family members and friends. Comparing their willingness to recommend with knowledge and usage, a significant statistical difference (P < 0.05) with a good association was displayed. The results are presented in Table 4.
Table 4.
The awareness of adverse effects from use of non-prescription of antibiotics by respondents
Discussion
This study has highlighted the potential dangerous trend of the use of non-prescribed antibiotics. In the face of diminishing antibiotics options, the rise in infections caused by resistant bacteria and a consequent increase in treatment costs could be detrimental to health-care management. Another report from Cairo,[20] indicated that inappropriate antibiotics use is rife and that it cuts across socioeconomic strata of the entire populace. Our findings are similar to theirs as well as the factors driving this behavior and types of drugs purchased.
All classes of antibiotics have been used by the respondents in the present investigation and for a list of ailments ranging from flu to acne. There is confirmation that non-prescription use of antibiotics is widespread within this community sequel to our previous findings of MDR S. aureus isolated from diabetic wounds and from nasal snares.[17,18] Earlier reports[21] had drawn attention to the use of outpatient non-prescribed antibiotics in this region of the world. Other regions of the developed world seem not to be exempted as researchers[22,23] had reported findings from Spain and Jordan, respectively. There is, however, published evidence of these countries putting in place some regulations aimed at mitigating the dispensing of non-prescribed antibiotics by community pharmacies.[22]
Furthermore, China is reported to have a high rate of antibiotic use as well as an equally high prevalence of antibiotic resistance.[23] Consistent with the findings of the present investigation is the report from another West African country, Ghana which, revealed that patients believe that antibiotics are an effective medication for cold and flu.[24] The present findings are also similar to earlier reports.[25] The demographic information of the respondents in this study showed that age, gender, educational background seemed not to have had any effect on the inclination to use non-prescribed antibiotics, meaning that everybody is involved in this behavior regardless of gender, age, and educational level. The reasons, knowledge, attitude, frequency, and factors driving are the use of non-prescribed antibiotics given by the respondents also varied as revealed in this study. These reasons showed a good association with usage (P < 0.01), particularly for cold and cough. Earlier reports by Afolabi[26] showed that the reason for non-consultation of medical personnel by patients could be due to poverty, inadequate health facilities, congestion in doctors’ clinics and ignorance. These reasons seem not to have changed over the years as is shown from the results of the present investigation. Low income and high unemployment level remain a problem in Nigeria. Respondents might, therefore, find it a waste of scarce resources visiting a health-care facility or clinic to see trained personnel who might not carry out an appropriate test before prescribing medication. Similar findings had been reported[27] showing a high rate of self-medication use of antimicrobial agents among out-patients in another part of South-eastern Nigeria and this had been attributed to the unwillingness of the majority of patients to consult qualified personnel.
Furthermore, worth noting is the list of diseases for which respondents employ the use of non-prescribed antibiotics in the present investigation. High on the list is the treatment of flu symptoms and usage for preventive measures. Again, all it takes to motivate those getting non-prescribed antibiotics from a pharmacy is either a recommendation from a friend, or through a previous experience, or even, through a TV advertisement. As radio and television advertisements continue, the influence of direct-to-patient advertising by pharmaceuticals cannot remain ignored.[27] Regulating pharmaceutical advertisement might, therefore, bring a desperately needed succor to this problem.[28]
It is a general norm to visit a GP or a clinic when needing medical attention. However, in the present investigation, only 40% of the respondents said they visited a clinic when feeling unwell, 35% said they went to the pharmacy. It was not ascertained whether or not the pharmacist refused to treat without a prescription. But with 35% of the respondents indicating their preference for the pharmacy, points to a non-refusal by pharmacists. Carl and Josep[22] reported that in Spain, 47.2% of pharmacists who did not sell non-prescribed antibiotics, did so purely on an administrative basis, referring to prohibition. This, therefore, suggests that the willingness or unwillingness demonstrated by pharmacists might be a contributory factor in curtailing this menace of use of non-prescription antibiotics. On the other hand, pharmacist in the region of the present investigation might simply be handicapped. Health care in the region is not free and does not come cheap either; neither is there a visible subsidy. Regarding the adverse effects from the use of non-prescribed antibiotics, majority said they were not aware of such dangers. However, a significant number of the respondents were affirmative that the use of non-prescribed antibiotics had helped in preventing or treating diseases. This point to the fact that it is a route likely to be taken again in future. Furthermore, that a huge number said they would recommend antibiotics to families and friends further highlights the magnitude of the dangers posed by the use of non-prescribed antibiotics and the continual development of microbial resistance. From this study, beta-lactam agents appear to be on the forefront and very popular among users in this region. This confirms our previous study, where our finding showed a high degree of beta-lactam resistant organisms.[17] Another report from Jordan disclosed a similar trend.[29] Evidence of the presence of multidrug-resistant (MDR) S. aureus isolated from diabetic wounds of patients among the community under investigation was revealed in a study.[18] Therefore, there is a need for more attention to be paid by the Health Regulatory Agencies as the world continues to face the problem of MDR antibiotics. There is also the need to look into the socioeconomic status of the health-care consuming population with the view of providing feasible solutions.
Strengths and limitations
This study confirms that non-prescription use of antibiotics is widespread within this community sequel to our previous findings on MDR S. aureus isolated from diabetic wounds and from nasal snares. This non-prescribed antibiotic usage transcends gender. Knowledge did not appear to influence this behavior. In addition, participant sampling was representative of community as majority were graduates and analysis of data was rigorous. Being a university town, participants were open and willing to participate in the survey. Participants sampled were a representative of the Nsukka population though the study could have done with an increased number, only those who were willing to participate in the survey were included. However, limitations in this study include the inability of authors to verify the extent of selling non-prescription antibiotics by pharmacists despite existing regulations not to do so. Second, we did not ascertain if participants were counseled by any health-care provider against buying over-the-counter antibiotics in relation with the consequences.
Acknowledgment
The authors hereby acknowledge Dr Tahir Khan, of Faculty of Pharmacy, Monash University, and Selangor, Malaysia, for his statistical input. We also thank the School of Basic Sciences, University of Nigeria, Nsukka, for their assistance.
References
- 1.Antimicrobial resistance:Revisiting the tragedy of the commons. Bull World Health Organ. 2010;88:805–6. doi: 10.2471/BLT.10.031110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larsson M, Kronvall G, Chuc NT, Karlsson I, Lager F, Hanh HD, et al. Antibiotic medication and bacterial resistance to antibiotics:A survey of children in a vietnamese community. Trop Med Int Health. 2000;5:711–21. doi: 10.1046/j.1365-3156.2000.00630.x. [DOI] [PubMed] [Google Scholar]
- 3.Oyetunde OO, Olugbake OA, Famudehin KF. Evaluation of use of antibiotic without prescription among young adults. [[Last accessed on 2010 Oct 18]];Afr J Phar Pharma. 2010 4:760–2. Available from: http://www.academicjournals.org/ajpp . [Google Scholar]
- 4.Sözen H, Gönen I, Sözen A, Kutlucan A, Kalemci S, Sahan M. Application of ATC/DDD methodology to evaluate of antibiotic use in a general hospital in Turkey. Ann Clin Microbiol Antimicrob. 2013;12:23. doi: 10.1186/1476-0711-12-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marlière GL, Ferraz MB, dos Santos JQ. Antibiotic consumption patterns and drug leftovers in 6000 Brazilian households. Adv Ther. 2000;17:32–44. doi: 10.1007/BF02868029. [DOI] [PubMed] [Google Scholar]
- 6.Hossain MM, Glass RI, Khan MR. Antibiotic use in a rural community in Bangladesh. Int J Epidemiol. 1982;11:402–5. doi: 10.1093/ije/11.4.402. [DOI] [PubMed] [Google Scholar]
- 7.Tagoe D, Attah C. A study of antibiotic use and abuse in Ghana:A case study of the cape coast metropolis. Internet J Health. 2009;11:1–5. [Google Scholar]
- 8.Bronzwaer SL, Cars O, Buchholz U, Mölstad S, Goettsch W, Veldhuijzen IK, et al. A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg Infect Dis. 2002;8:278–82. doi: 10.3201/eid0803.010192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grigoryan L, Burgerhof JG, Haaijer-Ruskamp FM, Degener JE, Deschepper R, Monnet DL, et al. SAR group. Is self-medication with antibiotics in Europe driven by prescribed use? J Antimicrob Chemother. 2007;59:152–6. doi: 10.1093/jac/dkl457. [DOI] [PubMed] [Google Scholar]
- 10.Matuz M, Benko R, Doro P, Hajdu E, Soos G. Non-prescription antibiotic use in Hungary. Pharm World Sci. 2007;29:695–8. doi: 10.1007/s11096-007-9132-0. [DOI] [PubMed] [Google Scholar]
- 11.Togoobaatar G, Ikeda N, Ali M, Sonomjamts M, Dashdemberel S, Mori R, et al. Survey of non-prescribed use of antibiotics for children in an urban community in Mongolia. Bull World Health Organ. 2010;88:930–6. doi: 10.2471/BLT.10.079004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cars O, Nordberg P. Antibiotic resistance-the faceless threat. Int J Risk Saf Med. 2005;17:103–10. [Google Scholar]
- 13.Byarugaba DK. A view on antimicrobial resistance in developing countries and responsible riskfactors. [[Last accessed on 2004 Feb 15]];Int J Antimicrob Agents. 2004 24:105–10. doi: 10.1016/j.ijantimicag.2004.02.015. Available from: https://www.dx.doi.org/10.1016/j.ijantimicag . [DOI] [PubMed] [Google Scholar]
- 14.Emeka PM, Al-Omar MJ, Khan TM. A qualitative study exploring role of community pharmacy in the irrational use and purchase of non-prescription antibiotics in al ahsa. [[Last accessed on 2014 Feb 14]];Eur J Gen Med. 2012 9:230–4. Available from: https://www.dx.doi.org/10.1016%2Fj.jsps . [Google Scholar]
- 15.Ling Oh A, Hassali MA, Al-Haddad MS, Syed Sulaiman SA, Shafie AA, Awaisu A. Public knowledge and attitudes towards antibiotic usage:A cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries. 2011;5:338–47. doi: 10.3855/jidc.1502. [DOI] [PubMed] [Google Scholar]
- 16.McNulty CA, Boyle P, Nichols T, Clappison P, Davey P. Don't wear me out-the publics knowledge of and attitudes to antibiotic use. J Antimicrob Chemother. 2007;59:727–38. doi: 10.1093/jac/dkl558. [DOI] [PubMed] [Google Scholar]
- 17.Emeka LI, Emeka PM, Okoli CL. Evaluation of antibiotic susceptibility ofStaphylococcus aureusisolated from nasal and thumbprints of university students and their resistance pattern. IOSR J Dent Med Sci. 2013;5:59–64. [Google Scholar]
- 18.Emeka LI, Emeka PM, Tahir MK. Antimicrobial activity of nigella sativa linn. Seed oil against multidrug resistantStaphylococcus aureusisolated from diabetic wounds. Pak J Med Sci. 2015;28:1985–90. [PubMed] [Google Scholar]
- 19.Raosoft Inc. Raosoft Sample Calculator. Seattle, WA: Raosoft Inc; 2004. [Google Scholar]
- 20.Elmasry AA, Bakr AS, Kolkailah DA, Khaskia MA, Mohammed ME, Mohamed OH, et al. Pattern of antibiotic abuse-a population based study in Cairo. Egypt J Chest Dis Tuberc. 2013;62:189–95. [Google Scholar]
- 21.Abosede OA. Self-medication:An important aspect of primary health care. Soc Sci Med. 1984;19:699–703. doi: 10.1016/0277-9536(84)90242-9. [DOI] [PubMed] [Google Scholar]
- 22.Llor C, Cots JM. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis. 2009;48:1345–9. doi: 10.1086/598183. [DOI] [PubMed] [Google Scholar]
- 23.Ammar A, Tareq L, Mukattash JH. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer Adherence. 2015;9:1389–95. doi: 10.2147/PPA.S91649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Currie J, Lin W, Zhang W. Patient knowledge and antibiotic abuse:Evidence from an audit study in China. J Health Econ. 2011;30:933–49. doi: 10.1016/j.jhealeco.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Scaioli G, Gualano MR, Gili R, Masucci S, Bert F, Siliquini R. Antibiotic use:A cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS One. 2015;10:e0122476. doi: 10.1371/journal.pone.0122476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7:120–7. doi: 10.4103/1596-3519.55666. [DOI] [PubMed] [Google Scholar]
- 27.Esimone CO, Nworu CS, Udeogaranya OP. Utilization of antimicrobial agents with and without prescription by out-patients in selected pharmacies in South-eastern Nigeria. Pharm World Sci. 2007;29 doi: 10.1007/s11096-007-9124-0. [DOI] [PubMed] [Google Scholar]
- 28.Shapiro MF. Regulating pharmaceutical advertising:What will work? CMAJ. 1997;156:359–61. [PMC free article] [PubMed] [Google Scholar]
- 29.Almaaytah A, Mukattash TL, Hajaj J. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer Adherence. 2015;9:1389–95. doi: 10.2147/PPA.S91649. [DOI] [PMC free article] [PubMed] [Google Scholar]