Abstract
This paper tested a model of parenting stress as a mediator between maternal depressive symptoms, emotion regulation and child behavior problems using a sample of homeless, substance abusing mothers. Participants were 119 homeless mothers (ages 18-24 years) and their young children (ages 0-6). Mothers responded to questions about their depressive symptoms, emotion regulation, parenting stress and child behavior problems. A path analysis showed that maternal depressive symptoms were positively associated with child behavior problems through increased parenting stress, whereas maternal cognitive reappraisal was negatively associated with child behavior problems through decreased parenting stress. Moreover, maternal expressive suppression was negatively related to child externalizing problems. Findings support the parenting stress theory and highlight maternal parenting stress as a mechanism associated with homeless children’s mental health risk. This study has significant implications for understanding the parenting processes underlying child’s resilience in the context of homelessness and maternal substance use.
Keywords: homeless mothers, parenting stress, depressive symptoms, behavior problems, substance use
Substance abusing homeless mothers experience high levels of parenting stress, which is exacerbated by their depressive symptoms and deficits in regulating emotions (Banyard & Graham-Bermann, 1998; Weinreb, Buckner, Williams, & Nicholson, 2006). Children of these mothers are at great risk of adverse outcomes, especially elevated behavior problems (Yu, North, LaVesser, Osborne, & Spitznagel, 2008; Zima, Wells, Benjamin, & Duan, 1996). However, a limited number of studies have examined maternal factors and child outcomes associated with parenting stress among homeless and substance abusing mothers. The current study adopted the parenting stress theory (Abidin, 1990a), and tested a model of parenting stress as a mediator between maternal depressive symptoms, emotion regulation and child behavior problems. This study highlights parenting stress as a potential mechanism of the intergenerational transmission of risk in mental health, and informs intervention programs designed for this population.
Parenting stress theory
Parenting stress theory (Abidin, 1990a; 1992) places parenting stress in a central role connecting multiple parental characteristics to dysfunctional parenting behaviors, as well as adverse child outcomes. Abidin (1990a) conceptualizes parenting stress as problematic situations concerning parental distress and child difficulties within the family. Clearly, homeless, substance abusing mothers experience high levels of parenting stress which can be associated with their living situation and parenting practices. Homeless mothers experience great financial stress and can lack resources to meet food, hygiene and other physical demands for their children; they are also not likely able to afford quality and consistent child care for their children (Meadows-Oliver, Sadler, Swartz, & Ryan-Krause, 2007). Moreover, in the US, homeless mothers tend to experience high levels of physical and mental health problems and a lack of social support compared to housed mothers, which limit their mental resources for meeting parenting demands (Weinreb et al., 2006). Additionally, US mothers who report problem levels of alcohol and drug use tend to report stressful, conflictual and strained relationships with their young children (Berlin, Shanahan, & Appleyard Carmody, 2014; Herbers et al., 2011). In fact, high rates of childhood abuse and neglect have been reported among children of homeless and substance-using mothers in both US and UK samples (Hogan, 1998; Walsh, MacMillan, & Jamieson, 2003). As such, the parenting stress of homeless, substance using mothers can be challenging. However, parenting stress among these mothers has been largely overlooked by researchers.
When mothers report more parenting stress, their children are at greater risk for internalizing and externalizing problems (Zima et al., 1996; Benzies, Harrison, & Magill-Evans, 2004). A US study compared homeless children to those in low-income families and found that children’s behavior problems were more related to parental stress than housing status (Masten, Miliotis, Graham-Bermann, Ramirez, & Neemann, 1993). Similarly, the security of infant attachment was more related to parenting stress than housing status in the US (Easterbrooks, & Graham, 1999). These findings indicate that in addition to being homeless, parenting stress can explain a great deal of the mental health risk that these children experience. Prior studies also reveal the potential mediating relationship of parenting stress on the link between maternal factors and child outcomes. However, no research has tested a mediation model of parenting stress directly, especially in a sample of homeless, substance abusing mothers. Below, evidence of how maternal depression and emotion regulation are associated with parenting stress is presented.
Maternal depression
Homeless mothers experience significant psychosocial stress, and one of the most common mental health challenges is depression (Crawford, Trotter, Hartshorn, & Whitbeck, 2011; Padgett et al., 2006). Among a sample of US homeless mothers, the lifetime prevalence of major depressive disorder was 45.0% with a one-month prevalence rate of 9.6%, while the lifetime prevalence of a substance use disorder was 41.1% (one-month prevalence rate was 4.6%). These rates are twice as high as those in a US nationally representative sample (Bassuk et al., 1998; Crawford et al., 2011). Moreover, US studies found that homeless mothers were more likely to experience higher rates of depression compared to homeless women without children (Bassuk et al., 1998; Marra et al., 2009).
The parenting stress theory posits that depressive mood contributes to parenting stress of homeless mothers and elucidates contributing factors to parenting stress, which include parental depression, ability to regulate emotions, and parent-child attachment (Abidin, 1990a; 1992). Further, US researchers report that the association between depression and stress is amplified with the experience of homelessness (Banyard & Graham-Bermann, 1998). Elevated depressive symptoms create coping difficulties and increase tension in the mother-child relationship (Goodman, 2007). Additionally, depressed mothers tend to rate their children as having more problematic behaviors (Webster-Stratton, & Hammond, 1988), and rate themselves as less competent with parenting (Gelfand, Teti, & Radin Fox, 1992). However, more recent studies examining the relationship between depression and stress among homeless mothers are sparse, and the combined effects of maternal depression and other aspects of psychological functioning, such as emotion regulation, are largely unexplored.
Emotion regulation
Mothers’ ability to regulate her own emotions is central to the distress that she experiences, and the parenting behaviors that she practices (Lorber, 2012). Emotion regulation is conceptualized as one’s ability to experience, express, and modulate emotions in adaptive ways (Thompson, 1994; Gross & John, 2003). Two commonly used emotion regulative strategies (Gross & John, 2003) include cognitive reappraisal and expressive suppression. Cognitive reappraisal occurs when an emotion-eliciting situation is re-conceptualized in a way that changes its emotional impact (Gross & John, 2003; Lazarus & Alfert, 1964). Expressive suppression is a form of response modulation that inhibits on-going emotion-expressive behaviors (Gross, 1998; Gross & John, 2003). Use of cognitive reappraisal is usually related to decreased stress, and increased positive experience and well-being, whereas use of expressive suppression is commonly related to elevated stress and decreased emotional well-being (Gross & John, 2003; Moore, Zoellner & Mollenholt, 2008).
Maternal capacities to regulate emotions are associated with family functioning and child problematic behaviors (Crandall, Ghazarian, Day, & Riley, 2016). Specifically, maternal cognitive reappraisal is associated with less harsh parenting (Lorber, 2012), whereas previous findings about maternal suppression is mixed. In a sample of healthy and housed US mothers, maternal suppression of emotion expression was found to be associated with less maternal negativity, negative emotions experienced and expressed by mothers (Lorber, 2012). However, in a higher risk US sample, where mothers were below the age of 30, low-income and experiencing partner’s psychological aggression, maternal suppression of emotion expression was found to be positively associated with poor maternal maladjustment, aggression towards children, and more externalizing problems in toddlers (Lorber, Del Vecchio, Feder, & Slep, 2017). Lorber argued that in the context of family aggression, parents can use suppression in situations where it is likely to generate more intense negative expressions later (Lorber et al., 2017).
The interaction patterns between homeless, substance using mothers and their children can be very different, since their life can be chaotic and unstructured, and these mothers tend to be disengaged and neglectful towards their children (Hogan, 1998; Walsh et al., 2003). Current research on regulatory processes among homeless, substance abusing mothers is limited. One US study found that homeless mothers used more avoidant regulation strategies than housed mothers, but no difference on cognitive strategies were found (Banyard & Graham-Bermann, 1998). However, more research is needed to examine emotion regulation and how it is associated with parenting stress and child functioning among this special population of at-risk mothers.
The current study
Given high rates of parenting stress among homeless mothers and the association with child problems, the current study sought to expand the current literature by specifying the mechanisms underlying maternal depressive symptoms, emotion regulation and child problems by considering parenting stress as a potential mediator. Two mediating hypotheses were tested. In particular, elevated maternal depressive symptoms were expected to be associated with increased child behavior problems through greater parenting stress. Also, less cognitive reappraisal and more expressive suppression were expected to be associated with increased child behavior problems through greater parenting stress (Figure 1).
Figure 1.
A conceptual model of the current study.
Method
Participants
This study utilized preliminary data from a larger randomized controlled trial testing a housing intervention with homeless mothers and their young children. Mothers (n = 119) were recruited through a local drop-in center and other locations that young homeless mothers access, such as shelters, libraries, bus stops, and medical facilities, in US. To be eligible for the study, women had to (1) be between the ages of 18 and 24, (2) meet criteria for homelessness as defined by the McKinney-Vento Act (2002), (3) have physical custody of a biological child 6 years old and younger, (4) meet criteria for a substance use disorder (SUD) as determined by the Structured Clinical Interview for DSM-5 Disorders (SCID-5) (First, Williams, Karg, & Spitzer, 2015). The Ohio State University Institutional Review Board approved all study procedures.
Mother’s ages ranged from 18-24 years (mean = 21.61 years, SD = 1.81) whereas children (66 boys) were 0-6 years old (mean = 2.32, SD = 1.61). The majority of mothers were African American (84.0%), whereas 16.0 % were White, non-Hispanic, or other races. A majority of women (89.9%) were single mothers. Many mothers were currently unemployed (63.0%) and had not completed a high school diploma or equivalency (43.5%).
Procedure
Mothers were engaged and screened in a private office by a study research assistant. Following the initial screening, the informed consent was signed and mothers continued with formal eligibility testing using the SCID-5 (First et al., 2015) sections on substance use disorder and schizophrenia. Women who were identified as eligible for the study continued with baseline assessment interview consisting of several individual and family measures. The baseline assessment interview required approximately 2.5 hours to complete and mothers were compensated with a $40 dollar Walmart gift card.
Measures
Mother’s depressive symptoms
Mother’s depressive symptoms were measured using the Beck Depression Inventory II (BDI-II; Beck et al., 1996). The BDI-II is a frequently used self-report instrument for the assessment of mood, cognitive and somatic aspects of depression over the past two weeks. It contains 21 items. It has demonstrated high test-retest reliability and the measure appears sensitive to depression severity across community and clinical populations including mothers (Huprich, Pouliot, & Bruner, 2012). Example items of the BDI include rating the level of one’s ‘sadness’ and ‘loss of interest’. About half of the mothers (45.4%) suffered from moderate to severe depressive symptoms in the current study. The reliability of this form in the current study was 0.93.
Maternal parenting stress
Maternal parenting stress was measured using the Parenting Stress Inventory Short Form (PSI/SF; Abidin, 1995). The PSI/SF is 36-item version of the Parenting Stress Index (PSI; Abidin, 1990b) using a 5-point scale. A total stress score yields from three subscales: parental distress, parent-child dysfunctional interaction, and difficult child. An example item of PSI/SF is “my child does a few things which bother me a great deal”. The PSI/SF has demonstrated strong internal consistency with lower SES, primarily African American mothers (Reitman, Currier, & Stickle, 2002). Cronbach α was 0.90 in the current study.
Maternal emotion regulation
Maternal emotion regulation was measured by the Emotion Regulation Questionnaire (ERQ; Gross & John, 2003). The ERQ consists of 10 items assessing two factors: cognitive reappraisal and expressive suppression using a 7-point Likert scale. Examples of the two subscales include “When I want to feel more positive emotion (such as joy or amusement), I change what I’m thinking about” and “I control my emotions by not expressing them,” respectively. The ERQ has demonstrated strong psychometric properties (Gross & John, 2003). The reliability of the cognitive reappraisal and expressive suppression subscales were 0.84 and 0.64, respectively.
Child behavior problems
Child behavior problems, specifically, child externalizing and internalizing behavior problems were measured using a maternal report of the Child Behavior Checklist for Ages 1.5-5 (CBCL; Achenbach & Rescorla, 2000). The CBCL is a 120-item instrument that elicits parent’s report of their child’s behavior problems on a 3-point scale for the past two months. Example items for externalizing and internalizing subscales include “defiant” and “cries a lot,” respectively. This measure has demonstrated high reliability, validity, and consistency across a variety of samples. The reliability of the externalizing and internalizing problem subscales were 0.94 and 0.89, respectively.
Covariates
Covariates included child age, sex, maternal age, race and education, and were measured by a demographic questionnaire that assessed core variables necessary to characterize the sample.
Data Analyses
Analyses were conducted using the lavaan package (Rosseel, 2012) in R (R Core Team, 2014). A path analysis model was estimated testing the mediation model. The root mean squared error of approximation (RMSEA) and comparative fit index (CFI) were used to evaluate the model fit, with a RMSEA of .05 and below and CFI of .95 and above indicating good fit and a RMSEA of .05-.08 and CFI of .90-.95 indicating acceptable fit (Hu & Bentler, 1995). The mediation effects were analyzed based on procedures recommended by Preacher and colleagues (2007). The bootstrap sampling method (Shrout & Bolger, 2002) was used to estimate the mediation effect and the conditional indirect effect. One advantage of the bootstrap method is that it does not assume a normally distributed parameter estimate, thus providing a more powerful test in detecting indirect effects, as the distribution of the indirect effects tend to be skewed (Mackinnon, Lockwood, Hoffman, West, & Sheets, 2002; Shrout & Bolger, 2002).
Results
Descriptive statistics and the bivariate correlations of the study variables are shown in Table 1. Maternal parenting stress was related to higher depressive symptoms (r = .33, p <.001) and lower cognitive reappraisal (r = −.25, p <.01). Maternal parenting stress was associated with elevated child externalizing (r = .43, p <.001) and internalizing problems (r = .41, p <.001). Maternal depressive symptoms were positively associated with externalizing problems (r = .18, p =.05).
Table 1.
Descriptive statistics and correlations of study variables.
| N | Percentage | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child sex | 119 | 55.46% | ||||||||||||
| 2. Child age | 119 | 2.32 | 1.60 | −.04 | ||||||||||
| 3. Maternal race | 119 | 84.03% | .12 | .10 | ||||||||||
| 4. Maternal age | 119 | 21.61 | 1.81 | −.06 | .33* | .12 | ||||||||
| 5. Maternal education | 115 | 11.30 | 1.47 | .07 | .15 | .17 | .41*** | |||||||
| 6. Maternal depressive symptoms | 119 | 19.43 | 11.68 | .08 | .09 | −.07 | .14 | −.01 | ||||||
| 7. Maternal cognitive reappraisal | 119 | 29.70 | 8.63 | .00 | −.02 | .03 | −.05 | −.02 | −.20* | |||||
| 8. Maternal expressive suppression | 119 | 18.92 | 5.31 | .00 | −.01 | .15 | −.05 | −.02 | .03 | .31*** | ||||
| 9. Maternal parenting stress | 119 | 85.71 | 20.77 | .14 | .04 | −.01 | .17 | .07 | .33*** | −.25** | .02 | |||
| 10. Child externalizing problems | 119 | 13.75 | 10.78 | .08 | .16 | .06 | .19* | .22* | .18* | −.06 | −.17 | .43*** | ||
| 11. Child internalizing problems | 119 | 9.77 | 8.69 | .07 | .25** | .02 | .20* | .18 | .13 | −.09 | −.07 | .41*** | .78*** |
Note.
p < .05,
p < .01,
p < .001. Child sex: 0 = female, 1 = male. Maternal race: 0 = White and other, 1 = Black.
A path model was then estimated with maternal parenting stress mediating the pathways between maternal depressive symptoms, cognitive reappraisal, expressive suppression regulation, and child behavior problems. The model yielded a good fit, χ2(18) = 22.47, p = .21; RMSEA = .046 (CI.90 = .000, .098); CFI = .979. The R-squared value was 0.27 for externalizing problems, and 0.24 for internalizing problems. As shown in Figure 2, maternal depressive symptoms were positively associated with parenting stress (B = .45, SE = .15, t = 2.94, p < .01). Maternal cognitive reappraisal was negatively correlated with parenting stress (B = −.49, SE = .22, t = −2.25, p = .03). Maternal expressive suppression was negatively associated with externalizing problems (B = −.44, SE = .17, t = −2.57, p = .01), whereas maternal parenting stress was positively related to externalizing (B = .22, SE = .05, t = 4.91, p < .001) and internalizing problems (B = .17, SE = 0.04, t = 4.50, p < .001). Among the covariates, only child age was a significant predictor of children’s internalizing behaviors (B = 1.17, SE = 0.46, t = 2.53, p = .01).
Figure 2.
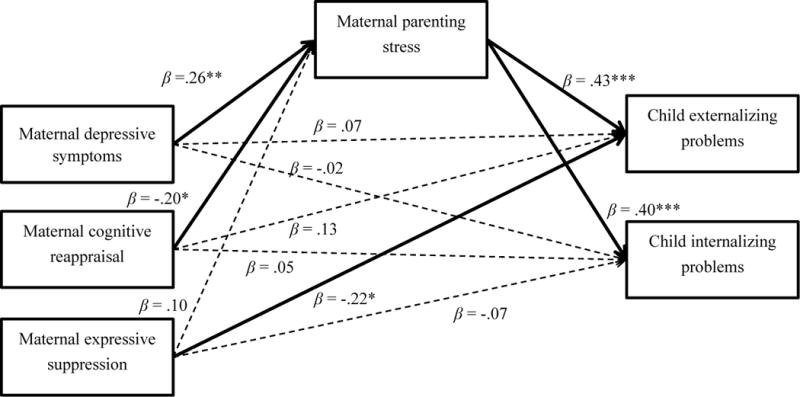
The path model.
Note. * p < .05, ** p < .01, *** p < .001. Covariates: child sex, child age, maternal age, race, maternal education. Child sex: female = 0 male = 1. Maternal race: 0 = White and other, 1 = Black.
Mediating pathways were tested from maternal depressive symptoms and emotion regulation to child behavior problems, based on 5000 bootstrap samples. Results indicated that maternal parenting stress mediated the links between maternal depressive symptoms and child externalizing problems (coefficient = .10, SE = .04, CI.90 = .03, .19) and internalizing problems (coefficient = .08, SE = .03, CI.90 = .02, .15); maternal parenting stress also mediated the relations between maternal cognitive reappraisal and child externalizing problems (coefficient = −.11, SE = .06, CI.90 = −.23, −.006) and internalizing problems (coefficient = −.08, SE = .05, CI.90 = −.19, −.004). The pathways from maternal expressive suppression to child behavior problems through parenting stress were not significant. Therefore, as expected, maternal depressive symptoms were associated with increased child problem behaviors through elevated parenting stress, whereas maternal cognitive reappraisal was associated with decreased problem behaviors through lower parenting stress.
Because of the study’s cross-sectional nature, it is possible that alternative model paths exist. It is likely that maternal parenting stress and less adaptive emotion regulation contribute to maternal depressive symptoms, which would also be associated with child behavior problems. Thus, an alternative model was tested with maternal depressive symptoms as a mediator between maternal parenting stress, emotion regulation and child behavior problems. The model fit was good (χ2(16) = 21.01, p = .18; RMSEA = .05 (CI.90 = .00, .11); CFI = .98. However, results showed that the indirect effects from depressive symptoms or emotion regulation to child behavior problems through parenting stress were not significantly different from zero. Thus, the model that maternal depressive symptoms mediated the links between maternal parenting stress, emotion regulation and child behavior problems was not supported by the current data.
Discussion
This study sought to advance our understanding of parenting stress among homeless, substance abusing mothers by testing a mediation model to reveal how risks of maternal mental health are conveyed to the mother’s children. Findings supported the parenting stress theory (Abidin, 1990a; 1992) and provide insight into the role of parenting stress in the intergenerational transmission of emotional problems among homeless families.
In particular, two mediating pathways were significant in the current study. The first one showed that maternal depressive symptoms were positively related to child externalizing and internalizing problems through elevated parenting stress. These findings are consistent with previous studies that reported homeless mothers’ depressive symptoms contributed to her reported stress (Weinreb et al., 2006). Similar findings were reported in samples from the general population of housed but depressed mothers (e.g., Gelfand, Teti, & Radin Fox, 1992; Leigh & Milgrom, 2008). Depressed mothers likely have a negative bias in perceptions of their children’s behaviors, thus exacerbating parenting stress (e.g., Webster-Stratton & Hammond, 1988). It is also likely that depressed mothers direct more energy to coping with their own distress (Goodman, 2007), and focus less attention on external stimuli, including their children. Notably, although maternal stress and depression tend to be inter-correlated (Hammen, 2005), and although this was a cross-sectional study, the path analysis model revealed that maternal depressive symptoms were predictive of parenting stress, rather than vice versa. This finding provides a basis for future hypotheses, and will need to be confirmed using a longitudinal design. Depressed mothers experiencing homelessness might experience more negative life events such as job loss and stress in interpersonal relationships than those who are not depressed, given that the symptoms of depression can lead to problems in social role functioning (Goodman, 2007), which may ultimately contribute to their parenting stress.
Another significant mediating pathway was that maternal cognitive reappraisal was related to less child behavior problems through decreased parenting stress. These results are in line with findings in the general population that cognitive reappraisal tends to be related to less stress and general well-being (Gross & John, 2003) and that maternal ability to regulate emotions is associated with less child problems (e.g., Crandall et al., 2016). It has been suggested that mothers with high cognitive appraisal may be able to adaptively interpret/experience life events in a manner that lowers their own stress (Lorber, 2012), thereby reducing environmental risk for their children.
Unexpectedly, maternal expressive suppression was negatively associated with child externalizing problems, such that when mothers suppressed their negative affect expression, children showed fewer externalizing problems. The opposite relationship was found among housed mothers experiencing partner psychological aggression, such that maternal expressive suppression was related to more child externalizing problems (Lorber et al., 2017). Given that children of homeless, substance abusing mothers experience an unstable, stressful and chaotic life (Bassuk & Rubin, 1987), maternal excessive expression of negative emotion might intensify the negative environment, and could serve to model, in a negative way, how these emotions are overly expressed and communicated in these families. That is, whereas appropriate expression of negative affect is likely healthy in non-homeless families, when stress is high, homeless mothers with substance use disorders and other psychopathologies may have difficulty expressing negative affect appropriately. Especially, a number of homeless, substance using mothers suffer from serious and chronic comorbid psychopathologies such as depression, anxiety, PTSD, or personality disorders (Weinreb et al., 2006), which may disrupt healthy expression of emotions. Thus, suppression of negative emotion expressions among homeless, substance using mothers might actually be protective in their children’s development of externalizing problems, including throwing tantrums, harsh and aggressive expression of anger, and even physical aggression.
Taken together, results of this study support the parenting stress theory (Abidin, 1990a; 1992). As the theory suggests, this study revealed that parenting stress served as a mediator between maternal depressive symptoms, cognitive appraisal and child behavior problems. Elevated stress is likely associated with maladaptive parenting behaviors (Abidin, 1990a; Anthony et al., 2005), which are further associated with adverse child outcomes (e.g., Benzies et al., 2004). Also in line with the theory, stressed parents were more likely to report that their children had higher internalizing and externalizing problems. In either of these cases, more perceived child problems can intensify parenting stress, which can be associated with increasing strain in the parent-child relationship, as well as negative child outcomes. However, longitudinal studies and transactional models are needed to further elucidate the relationships among maternal mental health, parenting stress, and child outcomes. Notably, the age of mothers in this sample is very young, and some of the mothers may have experienced teenage pregnancy. Although maternal age was not a significant predictor of child maladjustment after controlling for maternal psychological functioning and stress, teenage pregnancy can place adolescent mothers at unique risk for low education levels, unemployment, and psychological distress, thus conveying adverse child outcomes (Meadows-Oliver et al., 2007).
Limitations of this study also highlight future directions for research. First, this study is cross-sectional, not allowing us to make conclusions regarding the temporal ordering of predictive factors. Future studies should include a longitudinal design to test prospective relations between variables. Second, the variables used in this study were based solely on self-report, which were limited to the available options of instruments and may be biased by social desirability. Also, the associations among maternal depressive symptoms, stress and child outcomes may be inflated due to shared method variance, since depressed and stressed mothers tend to report their children’s behaviors as more problematic (Webster-Stratton & Hammond, 1988). Future studies should take a multi-method and multi-informant approach and assess maternal depressive symptoms, emotion regulation, parenting stress and child behavior problems using both maternal report and observational measures.
Despite these limitations, this study has several notable strengths. First, this study attempted to unravel the multifaceted relationship between maternal mental health (depressive symptoms), parenting stress and child internalizing and externalizing problems in a very high-risk sample, indicating differences from housed mothers and children. Second, mother’s own emotion regulation was taken into account to understand the internal regulatory processes of mothers, which has been less investigated. Third, this study highlights parenting stress as a potential mechanism of intergenerational transmission for mental health concerns among their children.
Findings of this study can inform prevention/intervention programs targeted at homeless families. Specific intervention programs should be tailored towards promoting effective emotion regulation, reducing depressive symptoms, and enhancing adaptive mother-child interactions among homeless, substance abusing mothers, beyond providing housing and connecting mothers to social services. In particular, programs should be directed towards reducing expression of negative emotions and increasing positive emotions between dyads, as well as managing stress among mothers so they can be more attentive and supportive to their children’s developmental needs. These efforts can reduce the prevalence of mental health problems in homeless families and promote healthy mother-child relationships.
Acknowledgments
This study was funded by NIDA grant #R01DA023062, awarded to second author. The Ohio State University Institutional Review Board approved all study procedures. All authors disclosed no conflict of interest in this study.
Footnotes
All authors declare that they have no conflict of interest.
Compliance with Ethical Standards
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all adult participants included in the study.
References
- Abidin RR. Introduction to the special issue: The stresses of parenting. Journal of Clinical Child Psychology. 1990a;19:298–301. [Google Scholar]
- Abidin RR. Parenting Stress Index (PSI) Charlottesville, VA: Pediatric Psychology Press; 1990b. [Google Scholar]
- Abidin RR. The determinants of parenting behavior. Journal of Clinical Child Psychology. 1992;21(4):407–412. [Google Scholar]
- Abidin RR. Parenting Stress Index: Professional Manual. 3rd. Odessa, FI: Psychological Assessment Resources; 1995. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA preschool forms & profiles. Burlington, VT: University of Vermont Research Center for Children, Youth, and Families; 2000. [Google Scholar]
- Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, Shaffer S. The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Infant and Child Development. 2005;14:133–154. [Google Scholar]
- Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, Low C. Pre‐school children with and without developmental delay: behaviour problems and parenting stress over time. Journal of Intellectual Disability Research. 2003;47:217–230. doi: 10.1046/j.1365-2788.2003.00484.x. [DOI] [PubMed] [Google Scholar]
- Banyard VL, Graham-Bermann SA. Surviving poverty: stress and coping in the lives of housed and homeless mothers. American Journal of Orthopsychiatry. 1998;68:479. doi: 10.1037/h0080357. [DOI] [PubMed] [Google Scholar]
- Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. American Journal of Psychiatry. 1998;155:1561–1564. doi: 10.1176/ajp.155.11.1561. [DOI] [PubMed] [Google Scholar]
- Bassuk E, Rubin L. Homeless children: a neglected population. American Journal of Orthopsychiatry. 1987;57:279. doi: 10.1111/j.1939-0025.1987.tb03538.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. General Psychiatry. 1996;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benzies KM, Harrison MJ, Magill-Evans J. Parenting stress, marital quality, and child behavior problems at age 7 years. Public Health Nursing. 2004;21:111–121. doi: 10.1111/j.0737-1209.2004.021204.x. [DOI] [PubMed] [Google Scholar]
- Berlin LJ, Shanahan M, Appleyard Carmody K. Promoting supportive parenting in new mothers with substance‐use problems: A pilot randomized trial of residential treatment plus an attachment‐based parenting program. Infant Mental Health Journal. 2014;35:81–85. doi: 10.1002/imhj.21427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandall A, Ghazarian SR, Day RD, Riley AW. Maternal emotion regulation and adolescent behaviors: The mediating role of family functioning and parenting. Journal of Youth and Adolescence. 2016;45:2321–2335. doi: 10.1007/s10964-015-0400-3. [DOI] [PubMed] [Google Scholar]
- Crawford DM, Trotter EC, Hartshorn KJS, Whitbeck LB. Pregnancy and mental health of young homeless women. American Journal of Orthopsychiatry. 2011;81:173. doi: 10.1111/j.1939-0025.2011.01086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easterbrooks M, Graham CA. Security of attachment and parenting: Homeless and low-income housed mothers and infants. American Journal of Orthopsychiatry. 1999;69:337. doi: 10.1037/h0080408. [DOI] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV) American Psychiatric Association; Arlington, VA: 2015. [Google Scholar]
- Gelfand DM, Teti DM, Radin Fox CE. Sources of parenting stress for depressed and nondepressed mothers of infants. Journal of Clinical Child and Adolescent Psychology. 1992;21:262–272. [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology. 1998;74:224–237. doi: 10.1037//0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85:348. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Herbers JE, Cutuli JJ, Lafavor TL, Vrieze D, Leibel C, Obradović J, Masten AS. Direct and indirect effects of parenting on the academic functioning of young homeless children. Early Education & Development. 2011;22:77–104. [Google Scholar]
- Hogan DM. The psychological development and welfare of children of opiate and cocaine users: Review and research needs. The Journal of Child Psychology and Psychiatry and Allied Disciplines. 1998;39(5):609–620. [PubMed] [Google Scholar]
- Hu L, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Thousand Oaks, CA: Sage; 1995. pp. 76–99. [Google Scholar]
- Huprich SK, Pouliot GS, Bruner R. Self-other representations mediate the relationship between five-factor model depression and depressive states. Psychiatry: Interpersonal & Biological Processes. 2012;75:176–189. doi: 10.1521/psyc.2012.75.2.176. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Alfert E. Short-circuiting of threat by experimentally altering cognitive appraisal. Journal of Abnormal and Social Psychology. 1964;69:195–205. doi: 10.1037/h0044635. [DOI] [PubMed] [Google Scholar]
- Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC psychiatry. 2008;8:24. doi: 10.1186/1471-244X-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber MF. The role of maternal emotion regulation in overreactive and lax discipline. Journal of Family Psychology. 2012;26:642. doi: 10.1037/a0029109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorber MF, Del Vecchio T, Feder MA, Slep AMS. A Psychometric Evaluation of the Revised Parental Emotion Regulation Inventory. Journal of Child and Family Studies. 2017;26:1–12. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marra JV, McCarthy E, Lin HJ, Ford J, Rodis E, Frisman LK. Effects of social support and conflict on parenting among homeless mothers. American Journal of Orthopsychiatry. 2009;79:348. doi: 10.1037/a0017241. [DOI] [PubMed] [Google Scholar]
- Masten AS, Miliotis D, Graham-Bermann SA, Ramirez M, Neemann J. Children in homeless families: risks to mental health and development. Journal of Consulting and Clinical Psychology. 1993;61:335. doi: 10.1037//0022-006x.61.2.335. [DOI] [PubMed] [Google Scholar]
- Meadows-Oliver M, Sadler LS, Swartz MK, Ryan-Krause P. Sources of stress and support and maternal resources of homeless teenage mothers. Journal of Child and Adolescent Psychiatric Nursing. 2007;20(2):116–125. doi: 10.1111/j.1744-6171.2007.00093.x. [DOI] [PubMed] [Google Scholar]
- McKinney-Vento Homeless Assistance Act, Re-Authorized. 42 U.S.C.11431 et seq. 2002:725. [Google Scholar]
- Moore SA, Zoellner LA, Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behaviour Research and Therapy. 2008;46:993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padgett DK, Gulcur L, Tsemberis S. Housing first services for people who are homeless with co-occurring serious mental illness and substance abuse. Research on Social Work Practice. 2006;16:74–83. [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate behavioral research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short Form. Journal of Clinical Child & Adolescent Psychology. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Rosseel Y. lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software. 2012;48:1–36. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422. [PubMed] [Google Scholar]
- Thompson RA. Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development. 1994;59:25–52. [PubMed] [Google Scholar]
- Walsh C, MacMillan HL, Jamieson E. The relationship between parental substance abuse and child maltreatment: findings from the Ontario Health Supplement. Child Abuse & Neglect. 2003;27:1409–1425. doi: 10.1016/j.chiabu.2003.07.002. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Maternal depression and its relationship to life stress, perceptions of child behavior problems, parenting behaviors, and child conduct problems. Journal of Abnormal Child Psychology. 1988;16:299–315. doi: 10.1007/BF00913802. [DOI] [PubMed] [Google Scholar]
- Weinreb LF, Buckner JC, Williams V, Nicholson J. A comparison of the health and mental health status of homeless mothers in Worcester, Mass: 1993 and 2003. American Journal of Public Health. 2006;96:1444–1448. doi: 10.2105/AJPH.2005.069310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu M, North CS, LaVesser PD, Osborne VA, Spitznagel EL. A comparison study of psychiatric and behavior disorders and cognitive ability among homeless and housed children. Community Mental Health Journal. 2008;44:1–10. doi: 10.1007/s10597-007-9100-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zima BT, Wells KB, Benjamin B, Duan N. Mental health problems among homeless mothers: Relationship to service use and child mental health problems. Archives of General Psychiatry. 1996;53:332–338. doi: 10.1001/archpsyc.1996.01830040068011. [DOI] [PubMed] [Google Scholar]


