Abstract
Background
Multiple studies have reported that risk adjusted rates of 30-day mortality following hospitalization for an acute condition are lower among blacks compared to whites.
Objective
To examine if previously-reported lower mortality for minorities, relative to whites, is accounted for by adjustment for do-not-resuscitate (DNR) status, potentially unconfirmed admission diagnosis, and differential risk of hospitalization.
Research design
Using inpatient discharge and vital status data for patients aged 18 and older in California, we examined all admissions from 1/1/2010 to 6/30/2011 for acute myocardial infarction, heart failure, pneumonia, acute stroke, gastrointestinal bleed, and hip fracture and estimated relative risk of mortality for Hispanics, (non-Hispanic) blacks, (non-Hispanic) Asians and (non-Hispanic) whites. Multiple mortality measures were examined: inpatient, 30-day, 90-day and 180-day. Adding census data we estimated population risks of hospitalization and hospitalization with inpatient death.
Results
Across all mortality outcomes, blacks had lower mortality rate, relative to whites even after exclusion of patients with DNR status and potentially unconfirmed diagnosis. Compared to whites, the population risk of hospitalization was 80% higher and risk of hospitalization with inpatient mortality was 30% higher among blacks. Among Hispanics and Asians, disparities varied with mortality measure.
Conclusions
Lower risk of post-hospitalization mortality among blacks, relative to whites, may be associated with higher rate of hospitalizations and differences in unobserved patient acuity. Disparities for Hispanics and Asians, relative to whites, vary with the mortality measure used.
Keywords: Race/ethnicity, disparities, mortality, hospitalization
Risk of death following hospitalization for acute conditions, such as acute myocardial infarction (AMI), heart failure (HF) and stroke, is a widely-used measure of quality of inpatient care. Over the last two decades national and state-level organizations have adopted and promoted its use for monitoring quality of care, for public reporting of hospital performance, and to financially reward and penalize hospitals.1–4 In comparing this risk between whites and blacks, a series of studies have found an unexpected trend: black patients had lower risk of 30-day mortality than white patients, even after adjustment for patient differences in demographics, health status and socioeconomic status.5–7 This pattern has been confirmed for a broad range of adult population groups, including veterans and Medicare enrollees.5,6,8–10
This finding of lower mortality among hospitalized minority patients is at odds with the prevailing view, and the preponderance of evidence, that minorities are generally at higher risk of receiving inadequate, delayed or poor quality treatment for many health problems11,12. Positing that the unexpected finding of lower mortality among minority patients might be sensitive to the choice of mortality outcome measure and/or indicative of confounding from factors not measured in previous studies, we examined the impact of additional measures of baseline differences in patient status and treatment options. For consistency with previous studies, we examined patients with a discharge diagnosis of one of six conditions: acute myocardial infarction (AMI), congestive heart failure (HF), pneumonia, acute stroke, hip fracture, and gastrointestinal (GI) bleed.5,7 First, we examined mortality differences using different mortality outcome measures (inpatient, 30-day, 90-day and 180-day) and extended prior racial comparisons to four race/ethnic groups: whites, blacks, Hispanics and Asians. Second, we examined if exclusion of patients with advance care planning, including do-not-resuscitate (DNR) orders, affected mortality differences. Prior studies indicate lower rate of advance care planning was (a) associated with lower inpatient mortality13, and (b) more common among minorities.14 Third, identification of hospitalized patient cohorts based on diagnosis codes is susceptible to inclusion of patients who may have been admitted for confirmatory or precautionary reasons but did not experience the indicated acute condition; differential incidence of such cases by race/ethnicity may confound the risk of mortality.15 Fourth, for patients with similar acuity, likelihood of hospitalization may vary systematically across race/ethnicity due to differences in barriers to outpatient care access.10 We examined racial/ethnic differences in population risk of hospitalization for the selected conditions, and in risk of death following such hospitalizations.
Methods
Data Sources
We obtained administrative discharge data covering all non-federal acute care hospitals in California for 2010–2011.16 We chose California based on completeness of patient race-ethnicity data, availability of data on DNR status, and ability to merge these data with the state vital status database for the entire population.17 As the hospitalizations in the discharge data represent a near-universe of all hospitalizations in the state, we merged these data with state census population data (2010–2011), to obtain population rates of hospitalization.18 To adjust for area-level differences in socioeconomic status and provider availability as in previous work,5 we obtained county level income, insurance coverage, provider availability and rural/urban location from other public sources.19,20
Study Cohorts
Discharge cohort
To examine patient mortality following hospitalization, we identified all inpatient admissions from 1/1/2010 to 6/30/2011 for adults aged 18 and older with the principal discharge diagnosis of acute myocardial infraction (AMI), heart failure (HF), pneumonia, acute stroke, gastrointestinal hemorrhage, and for those aged 65 and older, hip fracture. We used the AHRQ Inpatient Quality Indicators (IQI) Version 5.0 protocol to identify the admission cohorts, based on the principal discharge diagnosis code, and excluded: (1) discharges that were transfers to another acute care hospital (4.7% discharges); (2) AMI discharges (1.9% of overall discharges) with patients transferred from another short-term hospital; (3) discharges for patients who were not California residents (1.46%), so as to obtain population rates using state census population; and (4) discharges with missing measures (1.2%). For patients with multiple admissions, the risk of mortality is not independent across individual admissions; following previous work, we randomly selected one discharge.21
Census population cohort
For examination of the risk of hospitalization in the general population, we developed a cohort level data set of the state population stratified by age (18–44, 45–64, 65 and older), sex, race/ethnicity (four groups noted below) and year (2010 and 2011) (N = 48 cohorts).
Race/ethnicity
Using separate race and ethnicity indicators in the raw database, we identified five groups: Hispanics, (non-Hispanic) blacks, (non-Hispanic) Asians, (non-Hispanic) whites and Others.22 Race/ethnicity reporting was largely complete; for 0.6% discharges with missing race/ethnicity we followed AHRQ methodology ("hot-deck" imputation) and randomly assigned these discharges by hospital to one of the five race-ethnicity categories in the same proportion as observed among discharges from that hospital with reported race-ethnicity.23
Outcomes
For the discharge cohort, we merged patient discharge data with date of death information from the vital status database to identify four indicators of patient death based on timing: inpatient, and within 30, 90 or 180 days of admission date. For the census population cohort, we examined two outcomes: number of persons with at least one hospitalization and number of persons with hospitalizations resulting in inpatient death, per 1,000 census population.
Covariates
For analysis of the discharge cohort, we followed previous studies and identified indicators of demographics (age, sex, race/ethnicity), patient health risk (comorbid conditions using the Elixhauser grouping24) county-level socioeconomic status (median household income, percent uninsured, primary care provider shortage, urbanicity), hospital characteristics (fixed effects specification, as noted below) and year of discharge.5,6
We identified presence of advance directives using the discharge record do-not-resuscitate (DNR) indicator of “directive from a physician in a patient’s current inpatient medical record instructing that the patient is not to be resuscitated in the event of a cardiac or pulmonary arrest”.16 This indicator has been validated and applied in several studies.13,25
To examine if hospitalizations for confirmatory or preventive reasons differed by race/ethnicity and indirectly affect mortality differences, we followed the Centers of Medicare and Medicaid Services (CMS) Hospital Compare program, wherein hospitalizations for AMI, HF and pneumonia are not included in examination of 30-day mortality for patients discharged alive on the day of admission or the following day ("because it is unlikely they had significant AMI, HF, or pneumonia")26, and applied this criterion for all patients in our hospitalized study cohort.
Analysis
In estimating mortality differences by race/ethnicity in the discharge cohort we used linear probability models, adjusting for patient demographics, patient health status, area-based socioeconomic status and hospital-level fixed effects.5 Hospital fixed effects take into account systematic differences in the race/ethnic profile of hospital patients. The hospital fixed effects specification adjusts for systematic and time-invariant differences across hospitals, such as differences in hospital practice patterns, including affecting readmission risk.27 We estimated the models by admission cohort and all admissions combined; in the latter case, we included admission condition as a covariate. We also estimated the models by age (18–64 and 65+). Based on the regression estimates, we obtained adjusted mortality rates for each race/ethnic group, measured as number of deaths per 100 hospitalizations conditional on identical distribution of covariates and receipt of care at an average-performance hospital.28 We obtained heteroskedasticity-consistent robust standard error estimates adjusting for clustering at the hospital level.29 The linear probability model is our preferred approach as it enables adjustment for systematic (unobserved) differences across hospitals. As a sensitivity analysis we also estimated corresponding logistic models; as the hospital fixed effects specification is inapplicable for hospitals with no deaths, we instead used a hospital random effects specification.29 We estimated a series of models, treating the model with the previously noted covariates (demographics, patient health status and socioeconomic status) as the "base" model. We then re-estimated the model after (a) excluding DNR discharges, (b) excluding discharges with patient discharged alive the day of admission or the following day, and (c) excluding both types of discharges. As inpatient mortality has been shown to be sensitive to length of stay, we conducted a sensitivity analysis by including patient length of stay as a covariate in the previously estimated models.30
Using the census population cohort data, we estimated negative binomial regressions models with the number of hospitalizations and number of hospitalizations with inpatient death as outcome measures, census population as the exposure measure, and patient demographics as covariates. We report the risk ratio for minority race/ethnicity groups treating whites as the reference group.
This study was approved by the Institutional Review Board at the last author's institution. All statistical analyses were performed using Stata 14.0.31
Results
Our final discharge cohort consisted of 370,993 patients; out of 469,445 discharges for these patients, we randomly selected one discharge per patient. Their racial/ethnic composition was: Hispanics (18.8%), blacks (8.7%), Asians (9.4%) and whites (63.1%) (Table 1, Supplementary Materials AT1). For all four mortality outcomes (inpatient, 30-day, 90-day and 180-day mortality), observed rates were highest for whites, with the exception of inpatient mortality, where the highest rate was among Asians. When examined separately by age the pattern was more mixed; among patients aged 18–64 inpatient mortality was lower than whites among blacks but not among Hispanics and Asians (Supplementary Materials AT2 and AT3). White patients also had the highest mean age. The composition of patients by admission condition varied by race/ethnicity; the share of HF was highest among blacks (31.4%), while that of AMI and hip fracture were highest among whites. DNR prevalence was highest among whites (15.1%), followed by Asians (8.4%), Hispanics (6.8%) and blacks (4.8%). The proportion of patients with potentially unconfirmed diagnosis was highest among blacks (12.3%), followed by Hispanics (11.1%), whites (10.5%) and Asians (9.9%). There was considerable variation in prevalence of comorbid conditions; whites had higher rates of valvular disease, neurological disorders, hypothyroidism, and metastatic cancer, while minorities had higher rates of diabetes, renal failure and deficiency anemia. Blacks and Hispanics were more likely to live in areas with lower income, higher uninsurance and higher primary care provider shortage.
Table 1.
Study population characteristics
| Whites | Blacks | Hispanics | Asians | All | |
|---|---|---|---|---|---|
| N (%) | 234,080 (63.1%) | 32,399 (8.7%) | 69,603 (18.8%) | 34,911 (9.4%) | 370,993 |
| Mortality, % | |||||
| Inpatient mortality. | 5.4% | 3.6% | 4.6% | 6.0% | 5.2% |
| 30-day mortality | 10.7% | 6.0% | 7.6% | 9.0% | 9.5% |
| 90-day mortality | 16.2% | 10.5% | 11.5% | 13.7% | 14.6% |
| 180-day mortality | 20.1% | 14.0% | 14.4% | 17.0% | 18.2% |
| Admission cohort, % | |||||
| AMI | 12.9% | 9.4% | 12.0% | 12.3% | 12.4% |
| HF | 20.5% | 31.4% | 22.8% | 20.2% | 21.8% |
| Pneumonia | 25.5% | 22.2% | 26.3% | 24.0% | 25.2% |
| Stroke | 16.5% | 19.1% | 17.9% | 21.2% | 17.4% |
| GI Bleed | 14.0% | 15.7% | 16.3% | 16.7% | 14.9% |
| Hip fracture | 10.6% | 2.2% | 4.7% | 5.6% | 8.3% |
| Age, % | |||||
| 18–44 | 4.6% | 10.8% | 10.8% | 5.9% | 6.4% |
| 45–64 | 21.5% | 40.5% | 31.2% | 22.6% | 25.1% |
| 65+ | 73.9% | 48.7% | 58.0% | 71.5% | 68.5% |
| Female, % | 51.5% | 52.3% | 47.8% | 48.5% | 50.7% |
| DNR, % | 15.1% | 4.8% | 6.8% | 8.4% | 12.0% |
| Discharged alive same or next day, % | 10.5% | 12.3% | 11.1% | 9.9% | 10.7% |
| Area income, % | |||||
| High income | 58.2% | 28.7% | 34.3% | 55.9% | 50.9% |
| Moderate Income | 23.2% | 23.2% | 31.1% | 26.3% | 25.0% |
| Low Income | 18.6% | 48.0% | 34.6% | 17.9% | 24.1% |
Adjusted for demographics, patient health status, socioeconomic status and hospital effects, inpatient mortality rate (per 100 admissions) was higher among whites (5.29) than blacks (4.28, p-value < 0.05) and Hispanics (5.00, p-value < 0.05), and similar to that among Asians (5.33) (Table 2a and Supplemental Materials AT2a). Adjusted 30-day, 90-day and 180-day mortality rates were also higher among whites than among all the minority groups, with a margin of difference of at least 15% in all comparisons. Estimates of risk ratios using logistic regression indicated a similar pattern; for all mortality outcomes, mortality risk was highest among whites, compared to other groups, except for inpatient mortality where the risk was similar between whites and Asians (Table 2b and Supplemental Materials AT2b). Estimated separately by admission condition, adjusted mortality rates were generally higher among whites, although the differences did not attain statistical significance for some conditions (Supplemental Materials AT2c).
Table 2.
Adjusted mortality rates by race/ethnicity: Base model
| a. Adjusted mortality rate = # deaths / 100 hospitalizations | ||||
|---|---|---|---|---|
|
| ||||
| Mortality outcome | Whites | Blacks | Hispanics | Asians |
|
| ||||
| Inpatient mortality | 5.29 | 4.28* | 5.00* | 5.34 |
| 30-day mortality | 10.10 | 7.88* | 8.82* | 8.52* |
| 90-day mortality | 15.40 | 13.10* | 13.43* | 13.12* |
| 180-day mortality | 19.09 | 16.92* | 16.64* | 16.27* |
| b. Odds ratio of adjustment mortality differences from non-Hispanic whites | |||
|---|---|---|---|
|
| |||
| Mortality outcome | Blacks | Hispanics | Asians |
|
| |||
| Inpatient mortality | 0.75* | 0.94* | 1.02 |
| 30-day mortality | 0.70* | 0.84* | 0.83* |
| 90-day mortality | 0.80* | 0.83* | 0.81* |
| 180-day mortality | 0.83* | 0.81* | 0.79* |
Notes:
1) For Table 2a, the adjusted rate of mortalitywere estimated using a linear probability model of mortality with the following covariates besides race/ethnicity: age, sex, Elixhauser comorbidity indicators, and area level indicators of income, uninsurance rate, provider availability, rural/urban location and hospital fixed effects.
2) For Table 2b, the odds ratio (reference=non-Hispanic Whites) were estimated using a random effects (hospital) logistic model of mortality with the same covariates as for Table 2a.
3) In both Tables 2a and 2b, * denotes significant difference compared to non-Hispanic whites with p <0.05
Excluding discharges with DNR directives led to a sharp decrease in all mortality indicators for all groups; among whites, the inpatient mortality rate decreased from 5.29 to 3.61 (Table 3; Supplemental Materials AT3a–AT3c). However, except for inpatient mortality, whites continued to exhibit the highest rates for the other mortality indicators, relative to all minority groups; inpatient mortality rate for whites (3.61) was higher than that among blacks (3.07; p-value<0.05), similar to that among Hispanics (3.47) and lower to that among Asians (3.92; p-value<0.05). Excluding discharges where patients were discharged on the day of admission or the following day resulted in increase in all mortality indicators for all groups; however, the relative differences remained similar to that in the base model. Exclusion of both types of discharges led to the same pattern as exclusion of DNR discharges. Analogous estimation using logistic models exhibited identical patterns (Supplementary Materials AT2b, AT3d); however, the two exclusions resulted in reduction in white vs. non-white differences in cases with higher mortality among whites. The pattern of disparities in mortality over longer time (30-, 90- and 180-day mortality) was mixed; white-black mortality difference decreased over longer run mortality, but that for white-Hispanic and white-Asian differences remained constant (Supplementary Materials AT3d). This pattern is generally repeated for individual admission cohorts, although differences did not attain statistical significance for all conditions (Supplemental Materials AT3e). Although blacks and Hispanics were more likely to have multiple discharges, adjusting for the presence of multiple discharges resulted in no change in these estimates (Supplementary Materials Tables AT3f1, AT3f2). Also adjusting for admission through ED resulted in no change in these estimates (Supplementary Materials Tables AT3g1, AT3g2).
Table 3. Adjusted mortality rates by race/ethnicity.
Mortality rate = # deaths / 100 hospitalizations
| Adjustment | Whites | Blacks | Hispanics | Asians |
|---|---|---|---|---|
| Inpatient mortality | ||||
|
| ||||
| Base model | 5.29 | 4.28* | 5.00* | 5.34 |
| After exclusion of DNR discharges | 3.61 | 3.07* | 3.47 | 3.92* |
| After exclusion of patients discharged live same/next day | 5.95 | 4.75* | 5.58* | 5.89 |
| After both exclusions | 4.08 | 3.44* | 3.89 | 4.35* |
|
| ||||
| 30-day mortality | ||||
|
| ||||
| Base model | 10.10 | 7.88* | 8.82* | 8.52* |
| After exclusion of DNR discharges | 6.94 | 5.54* | 6.10* | 6.09* |
| After exclusion of patients discharged live same/next day | 10.88 | 8.41* | 9.50* | 9.17* |
| After both exclusions | 7.56 | 5.99* | 6.65* | 6.60* |
|
| ||||
| 90-day mortality | ||||
|
| ||||
| Base model | 15.40 | 13.10* | 13.43* | 13.12* |
| After exclusion of DNR discharges | 11.54 | 10.06* | 10.09* | 10.09* |
| After exclusion of patients discharged live same/next day | 16.48 | 13.89* | 14.38* | 14.06* |
| After both exclusions | 12.45 | 10.76* | 10.92* | 10.88* |
|
| ||||
| 180-day mortality | ||||
|
| ||||
| Base model | 19.09 | 16.92* | 16.64* | 16.27* |
| After exclusion of DNR discharges | 14.9 | 13.60* | 13.05* | 12.98* |
| After exclusion of patients discharged live same/next day | 20.33 | 17.87* | 17.71* | 17.35* |
| After both exclusions | 15.97 | 14.48* | 14.01* | 13.89* |
Notes:
1) Adjusted rates of mortality were estimated using a linear probability of mortality with the following covariates besides race/ethnicity: age, sex, Elixhauser comorbidity indicators, and area level indicators of income, uninsurance rate, provider availability, rural/urban location and hospital fixed effects.
2) * denotes p<0.05 in difference compared to non-Hispanic whites
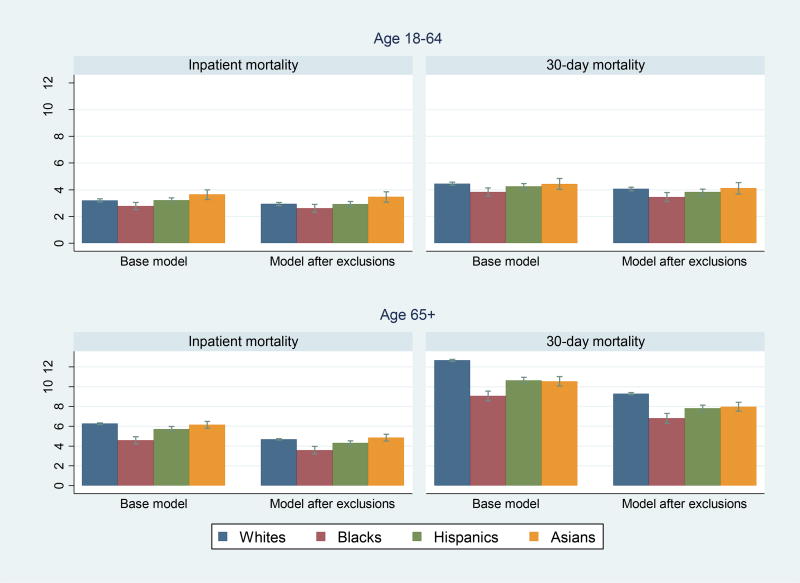
Repeating the analyses separately by age, racial/ethnic differences in mortality were generally larger and significant among patients 65 and older than among those 18 to 64 (Figure 1 and Supplementary Tables AT4a–4f). The pattern of differences among the older group was identical to that for the overall population. Among patients aged 18–64, in the base model, inpatient mortality among whites was higher than that among blacks, similar to that among Hispanics and lower than that among Asians; after both exclusions, inpatient mortality for whites and blacks are similar. The exclusions did not affect the relative mortality differences for 30-day mortality among adults aged 18–64. There was a mixed pattern of white vs. non-white differences in mortality over longer periods (i.e., inpatient, 30-day, 90-day and 180-day) by minority group and age.
Figure 1. Adjusted mortality rates by age.
Mortality rate = # deaths / 100 hospitalizations
Notes:
1) Adjusted rates of mortality were estimated using a linear probability model of mortality with the following covariates besides race/ethnicity: age, sex, Elixhauser comorbidity indicators, and area level indicators of income, uninsurance rate, provider availability, rural/urban location and hospital fixed effects.
Using census population cohort data, we estimated the population risks of (a) hospitalization for the selected conditions, and (b) hospitalization resulting in inpatient death (Table 4 and Supplementary Tables AT5a–AT5b). Among whites, for every 1000 person-years, there were 11.9 persons with a hospitalization and 1.27 persons with a hospitalization resulting in inpatient death. Relative to whites, among blacks, the risk of hospitalization was 80% higher and the risk of hospitalization with inpatient death was 30% higher; in contrast, among Hispanics and Asians, both risks were lower. Also, among blacks the contrast in estimates by age was striking. In the 18–64 population, relative to whites, risk of hospitalization was 118% higher and risk of hospitalization with inpatient death was 91% higher among blacks; but in the 65 and older population, the corresponding risks were 11% higher and 27% lower.
Table 4. Population incidence of acute admissions and acute admissions with inpatient deaths by race/ethnicity, California, 2010–2011.
Population: Age 18 and older
| Census population 2010–2011 (person years) |
# admissions for acute conditions |
Crude rate of acute admissions per 1,000 person years |
Adjusted risk ratio of acute admissions per 1,000 person years (reference=Whites) |
# acute conditions admissions with inpatient death |
Crude rate of acute admissions with inpatient death per 1,000 person years |
Adjusted risk ratio of acute admissions with inpatient death per 1,000 person years (reference=Whites) |
|
|---|---|---|---|---|---|---|---|
| All | |||||||
|
| |||||||
| Whites | 19,669,525 | 234,075 | 11.9 | 1.0 | 24,900 | 1.27 | 1.0 |
| Blacks | 2,494,215 | 32,396 | 13.0 | 1.80* | 1,959 | 0.79 | 1.30 |
| Hispanics | 14,077,451 | 69,621 | 4.9 | 0.76* | 5,246 | 0.37 | 0.73* |
| Asians | 5,988,108 | 34,901 | 5.8 | 0.59* | 3,174 | 0.53 | 0.62* |
|
| |||||||
| Age 18–64 | |||||||
|
| |||||||
| Whites | 15,565,896 | 61,021 | 3.9 | 1.0 | 2,678 | 0.17 | 1.0 |
| Blacks | 2,157,499 | 16,629 | 7.7 | 2.18* | 623 | 0.29 | 1.91* |
| Hispanics | 12,921,196 | 29,268 | 2.3 | 0.73* | 1,252 | 0.10 | 0.84* |
| Asians | 5,107,035 | 9,940 | 1.9 | 0.54* | 481 | 0.09 | 0.65* |
|
| |||||||
| 65+ | |||||||
|
| |||||||
| Whites | 4,103,629 | 173,054 | 42.2 | 1.0 | 22,222 | 5.42 | 1.0 |
| Blacks | 336,716 | 15,767 | 46.8 | 1.11* | 1,336 | 3.97 | 0.73* |
| Hispanics | 1,156,255 | 40,353 | 34.9 | 0.83* | 3,994 | 3.45 | 0.64* |
| Asians | 881,074 | 24,961 | 28.3 | 0.68* | 2,693 | 3.06 | 0.57* |
Notes:
1) Overall census population figures for California during 2010 and 2011 were obtained from the Census Bureau online database. Note that since we examined admissions for only the first 6 months of 2011, we have used half of the 2011 census population figures.
2) Risk ratio of the two outcomes are estimated by negative binomial regression at the cohort level (N=48) using age, sex, race/ethnicity and discharge year as covariates.
Discussion
Adjusting for potential confounders not previously studied, our re-examination of racial/ethnic differences in risk of patient death following hospitalization for an acute condition highlights four findings. First, even after exclusion of patients with DNR directives and discharges with a potentially unconfirmed diagnosis, 30-, 90- and 180-day adjusted mortality rates, for all conditions combined, remained lower among black, Hispanic and Asian patients, relative to white patients. Second, this pattern differed for inpatient mortality. Third, at the general population level, the risk of hospitalization was higher among blacks than whites. Fourth, the pattern of survival advantage among minorities is more pronounced and widespread in the over-65 age group than in the 18–64 age group.
To our knowledge, none of the previous studies that reported lower mortality among blacks, relative to whites, took account of DNR directives.5–8,14 In our data, the proportion of white patients with DNR directive (15.1%) was over three times that among black patients (4.8%); also, the proportion of potentially unconfirmed cases, measured as those with same- or next-day live discharges, was higher among blacks (12.3%) than whites (10.5%). Although both exclusions resulted in reduction in white-black differences in 30-, 90- and 180-day mortality, risk adjusted mortality remained lower among blacks, indicating the presence of other factors that account for the apparent survival advantage. Our study also found that post-hospitalization survival advantage is not limited only to blacks. Extending the comparisons to other racial/ethnic minority groups, we found lower 30-, 90- and 180-day mortality also among Hispanics and Asians, relative to whites.
This apparent survival advantage does not extend to inpatient mortality. Compared to whites, adjusted inpatient mortality was 19% lower among blacks, similar among Hispanics and 8% higher among Asians.32–36 Prior literature has been largely silent on differential findings when examining inpatient mortality vs. mortality 30 to 180 days after admission. Inpatient mortality is a validated measure of the quality of inpatient care.37 Given that median length of hospitalization is 4 days, inpatient mortality may be more sensitive to care received during the index hospitalization than 30 day (or later) mortality.38,39 Conversely, mortality after 30 days after admission may be influenced by a multitude of factors beyond the inpatient care received, including continuity of outpatient care and other determinants of life expectancy in the community setting. Our use of a hospital-level fixed effects specification also indicates that the patterns of survival advantage or disadvantage found are not associated with systematic differences in hospital treatment patterns or quality. Therefore, factors according survival advantage may be prevalent outside the hospital setting.
Our study also identifies differences in hospitalization risk across the general population as a potential determinant of survival advantage among blacks. We found that blacks had 80% more hospitalizations than whites, they experienced 30% more inpatient deaths; the disproportionately smaller number of additional inpatient deaths points to lower mortality among hospitalized black patients. The reasons for the higher rate of hospitalization among blacks are unclear. One previous study found that among patients whose hospitalization is affected by limited outpatient care access, average patient severity may be lower than among other patients.10 Poorer outpatient care access among blacks may lead some to seek ED care for primary care treatable conditions, leading to higher possibility of being hospitalized, particularly for symptoms involving greater discretion in treatment protocols (e.g., heart failure).40,41 However, this conjecture needs to be examined empirically by studying the joint risk of hospitalization and mortality
Having estimated mortality differences in a variety of distinct contexts – different mortality measures, minority groups and exclusion conditions – survival advantage among minorities was more pronounced and robust in the older (age 65+) than among younger (age 18–64) adults. In the younger group, there was no survival advantage in inpatient mortality for any minority group and in 30-day mortality for Hispanics and Asians. In contrast, among the older patients, survival advantage in 30-day mortality was found among all minority groups and in inpatient mortality among blacks and Hispanics. Difference by age was also found in the risk of hospitalization among blacks. Therefore, study of the joint risk of hospitalization and mortality may help explain the variation in mortality findings by age.
Overall our study points to increased complexity in the characterization of post-hospitalization survival advantage noted among blacks in previous studies. First, care is needed regarding how mortality is measured; inpatient death and 30-day mortality cannot be conflated as this distinction clearly affects the findings. Also, this pattern reinforces the view that mortality differences by race/ethnicity are unlikely to be associated with the quality of inpatient care, since these are more likely to affect inpatient mortality than 30-day mortality; using hospital fixed-effects regression specification, all our estimation was based on comparison of patients by race/ethnicity within each hospital.5,7 Second, Second, racial and ethnic differences in advance care planning need to be incorporated into analyses. We found that adjusting for DNR status resulted in reduction of survival advantage estimates; however, as our data did not include actual use of goal concordant care care (in terms of aggressive life-saving and life-extending interventions administered) further research is needed to better assess the role of end-of-life interventions on survival differences by race/ethnicity.42 Finally, our study also found systematic differences in the risk of hospitalization for acute conditions, with higher rates of admission among blacks, relative to whites; this risk also varied by age. While some of this difference may arise from prevalence or severity of health problems, differential use of ED and hospital care due to non-clinical factors (e.g., access barriers) may lead to differences in patient severity at admission. If there is systematic racial or ethnic bias in the use of severity codes (i.e., to justify hospital admissions for people who are not as sick) standard case-mix adjustment may not appropriately control for mortality risk.
We recognize several limitations of this study. First, administrative data is limited in the ability to adequately distinguish differences in severity of patient status. Second, previously-reported limitations of identifying race and ethnicity in administrative data also apply here.43 However, for California data, there is evidence of good concordance between self-reported race/ethnicity with that documented in administrative data for some admission cohorts, and there was minimal missing data.22 Third, our study findings are based only on data from non-federal hospitals in California; in spite of the high concordance with previous findings from other data sources, evidence from other regions also needs to be examined for generalizability of findings. Also more recent data on mortality differences should also be studied to incorporate potential changes arising from policy interventions in improving access and quality of care.
To summarize, among patients hospitalized for acute conditions, the pattern of lower 30-day mortality among racial/ethnic minorities, relative to whites, did not change after exclusion of discharges with DNR status or potentially unconfirmed diagnosis, although the differences were reduced. Future work using data on actual use of life-saving interventions during and after the index hospitalizations may better measure the fuller effect of differences in end-of-life care. We found that the pattern of survival advantage varied with mortality outcome, minority group and patient age, and that this variation was associated with differential risk of hospitalization. Further research in quantifying this risk and the accompanying differences in patient status and severity may help further clarify the complexity of patterns in survival advantage.
Supplementary Material
Acknowledgments
This research has been supported by NIH grants (1R01MD007705-01, A. Hanchate, PI and 1U01HL105342-01, N. Kressin, PI). Dr. Kressin is supported in part by a Senior Research Career Scientist award from the Department of Veterans Affairs, Health Services Research & Development Service (RCS 02-066-1). Dr. López thanks the Robert Wood Johnson Foundation Harold Amos Faculty Development Program and NIDDK 1K23DK098280-01. Dr. Hanchate received computing and information technology support from BU's Clinical and Translational Institute through CTSA grant U54-TR001012. Dr. Amresh Hanchate had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
None of the authors have a conflict of interest.
The views expressed in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health, Boston University, MedSTAR Washington Hospital Center, Donald and Barbara Zucker School of Medicine, UCSF, or the Department of Veterans Affairs.
References
- 1.Shahian DM. Public reporting of cardiac surgery performance: introduction. The Annals of Thoracic Surgery. 2011;92(3 Suppl):S1. doi: 10.1016/j.athoracsur.2011.06.102. [DOI] [PubMed] [Google Scholar]
- 2.Bernheim SM, Grady JN, Lin Z, et al. National Patterns of Risk-Standardized Mortality and Readmission for Acute Myocardial Infarction and Heart Failure: Update on Publicly Reported Outcomes Measures Based on the 2010 Release. Circulation: Cardiovascular Quality and Outcomes. 2010;3(5):459–467. doi: 10.1161/CIRCOUTCOMES.110.957613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Department of Veterans Affairs. VA Hospital Compare. 2013 http://www.hospitalcompare.va.gov/
- 4.Blumenthal D, Jena AB. Hospital value-based purchasing. J Hosp Med. 2013;8(5):271–277. doi: 10.1002/jhm.2045. [DOI] [PubMed] [Google Scholar]
- 5.Polsky D, Jha AK, Lave J, et al. Short- and Long-Term Mortality after an Acute Illness for Elderly Whites and Blacks. Health Services Research. 2008;43(4):1388–1402. doi: 10.1111/j.1475-6773.2008.00837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polsky D, Lave J, Klusaritz H, et al. Is lower 30-day mortality posthospital admission among blacks unique to the Veterans Affairs health care system? Medical Care. 2007;45(11):1083–1089. doi: 10.1097/MLR.0b013e3180ca960e. [DOI] [PubMed] [Google Scholar]
- 7.Volpp KG, Stone R, Lave JR, et al. Is thirty-day hospital mortality really lower for black veterans compared with white veterans? Health Serv Res. 2007;42(4):1613–1631. doi: 10.1111/j.1475-6773.2006.00688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285(3):297–303. doi: 10.1001/jama.285.3.297. [DOI] [PubMed] [Google Scholar]
- 9.Rathore SS, Foody JM, Wang Y, et al. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. Jama. 2003;289(19):2517–2524. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 10.Auble TE, Hsieh M, Yealy DM. Differences in initial severity of illness between black and white emergency department patients hospitalized with heart failure. American Heart Journal. 2009;157(2):306–311. doi: 10.1016/j.ahj.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Unqual Treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 12.Agency for Healthcare Research & Quality. National Healthcare Disparities Report 2013. Rockville, MD: 2013. [Google Scholar]
- 13.Walkey AJ, Weinberg J, Wiener R, Cooke CR, Lindenauer PK. Association of do-not-resuscitate orders and hospital mortality rate among patients with pneumonia. JAMA Intern Med. 2015:1–8. doi: 10.1001/jamainternmed.2015.6324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garrido MM, Harrington ST, Prigerson HG. End-of-life treatment preferences: a key to reducing ethnic/racial disparities in advance care planning? Cancer. 2014;120(24):3981–3986. doi: 10.1002/cncr.28970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation. 2015 Condition-Specific Measures Updates and Specifications Report: Hospital-Level 30-day Risk-Standardized Mortality Measures. 2015 www.qualitynet.org.
- 16.Office of Statewide Health Planning and Development. Hospital Inpatient Discharge Data. 2014 https://www.oshpd.ca.gov/HID/Data_Request_Center/documents/DataDictionary_Nonpublic_PDD.pdf.
- 17.California Department of Public Health. Vital Statistics Data. 2014 https://www.cdph.ca.gov/data/dataresources/requests/Pages/VitalStatisticsBirthDeathFetalDeathMarriageData.aspx.
- 18.Population Estimates. [Accessed 3/30/2014];U.S. Census Bureau. 2014 http://www.census.gov/popest/index.html.
- 19.Health Resources and Services Administration. User Documentation for the Area Healthcare Resource File. Washington, DC: U.S. Department of Health and Human Services; 2016. [Google Scholar]
- 20.US Department of Agriculture. [Accessed 1/20/2014];Measuring Rurality -- Rural-Urban Continuum Codes. 2006 http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 21.Yale New Haven Health Services Corporation/Center for Outcomes Research and Evaluation. 2014 Measures Updates and Specifications Report: Hospital-Level 30-Day Risk-Standardized Mortality Measures. 2014 [Google Scholar]
- 22.Zingmond DS, Parikh P, Louie R, et al. Improving Hospital Reporting of Patient Race and Ethnicity—Approaches to Data Auditing. Health Services Research. 2015;50:1372–1389. doi: 10.1111/1475-6773.12324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coffey RM, Barrett M, Houchens R, et al. Methods Applying AHRQ Quality Indicators to Healthcare Cost and Utilization Project (HCUP) Data for the Tenth (2012) National Healthcare Quality Report (NHQR) and National Healthcare Disparities Report (NHDR) U.S. Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- 24.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Goldman LE, Chu PW, Osmond D, Bindman A. Accuracy of do not resuscitate (DNR) in administrative data. Med Care Res Rev. 2013;70(1):98–112. doi: 10.1177/1077558712458455. [DOI] [PubMed] [Google Scholar]
- 26.Bernheim SM, Wang Y, Grady JN, et al. 2011 Measures Maintenance Technical Report: Acute Myocardial Infarction, Heart Failure, and Pneumonia 30-Day Risk-Standardized Mortality Measures. 2011 [Google Scholar]
- 27.Krumholz HM, Lin Z, Keenan PS, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. Jama. 2013;309(6):587–593. doi: 10.1001/jama.2013.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.StataCorp. Stata14 help for margins. College Station, TX: 2016. https://www.stata.com/help.cgi?margins. [Google Scholar]
- 29.Cameron AC, Trivedi PK. Microeconometrics: Methods and Applications. New York: Cambridge University Press; 2005. [Google Scholar]
- 30.Drye EE, Normand S-LT, Wang Y, et al. Comparison of Hospital Risk-Standardized Mortality Rates Calculated by Using In-Hospital and 30-Day Models: An Observational Study With Implications for Hospital Profiling. Annals of Internal Medicine. 2012;156(1_Part_1):19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2016. [Google Scholar]
- 32.Agency for Healthcare Research and Quality. 2015 National Healthcare Quality and Disparities Report and 5th Anniversary Update on the National Quality Strategy. Rockville, MD: Agency for Healthcare Research & Quality; Sep 12, 2016. 2016. [Google Scholar]
- 33.Andrews RM, Moy E. Racial differences in hospital mortality for medical and surgical admissions: variations by patient and hospital characteristics. Ethn Dis. 2015;25(1):90–97. [PubMed] [Google Scholar]
- 34.Hines AL, Andrews RM, Moy E, Barrett ML, Coffey RM. Disparities in rates of inpatient mortality and adverse events: race/ethnicity and language as independent contributors. Int J Environ Res Public Health. 2014;11(12):13017–13034. doi: 10.3390/ijerph111213017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xian Y, Holloway RG, Noyes K, Shah MN, Friedman B. Racial Differences in Mortality Among Patients With Acute Ischemic Stroke. Annals of Internal Medicine. 2011;154(3):152–159. doi: 10.1059/0003-4819-154-3-201102010-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanchate AD, Schwamm LH, Huang W, Hylek EM. Comparison of ischemic stroke outcomes and patient and hospital characteristics by race/ethnicity and socioeconomic status. Stroke; a journal of cerebral circulation. 2013;44(2):469–476. doi: 10.1161/STROKEAHA.112.669341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agency for Healthcare Research and Quality. Guide to Inpatient Quality Indicators: Quality of Care in Hospitals - Volume, Mortality and Utilization. Rockville, MD: AHRQ; 2011. [Google Scholar]
- 38.Bilimoria KY, Cohen ME, Ingraham AM, et al. Effect of postdischarge morbidity and mortality on comparisons of hospital surgical quality. Ann Surg. 2010;252(1):183–190. doi: 10.1097/SLA.0b013e3181e4846e. [DOI] [PubMed] [Google Scholar]
- 39.Damhuis RAM, Wijnhoven BPL, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. British Journal of Surgery. 2012;99(8):1149–1154. doi: 10.1002/bjs.8813. [DOI] [PubMed] [Google Scholar]
- 40.Jeffery MM, Bellolio MF, Wolfson J, Abraham JM, Dowd BE, Kane RL. Validation of an algorithm to determine the primary care treatability of emergency department visits. BMJ Open. 2016;6(8):e011739. doi: 10.1136/bmjopen-2016-011739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Safavi KC, Dharmarajan K, Kim N, et al. Variation exists in rates of admission to intensive care units for heart failure patients across hospitals in the United States. Circulation. 2013;127(8):923–929. doi: 10.1161/CIRCULATIONAHA.112.001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hanchate A, Kronman AC, Young-Xu Y, Ash AS, Emanuel E. Racial and Ethnic Differences in End-of-Life Costs: Why Do Minorities Cost More Than Whites? Arch Intern Med. 2009;169(5):493–501. doi: 10.1001/archinternmed.2008.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Geppert JJ, Singer SJ, Buechner J, Ranbom L, Suarez W, Xu W. State collection of racial and ethnic data. In: Ver Ploeg M, Perrin E, editors. M. Ver Ploeg E. Perrin & National Research Council (US). Panel on DHHS Collection of Race and Ethnicity Data.(Eds.), Eliminating health disparities: Measurement and data needs. Washington DC: National Academies Press; 2004. pp. 232–248. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.