Abstract
Background
Emotion recognition skills are essential for social communication. Deficits in these skills have been implicated in mental disorders. Prior studies of clinical and high-risk samples have consistently shown that children exposed to adversity are more likely than their unexposed peers to have emotion recognition skills deficits. However, only one population-based study has examined this association.
Methods
We analyzed data from children participating in the Avon Longitudinal Study of Parents and Children, a prospective birth cohort (n=6,506). We examined the association between eight adversities, assessed repeatedly from birth to age 8 (caregiver physical or emotional abuse; sexual or physical abuse; maternal psychopathology; one adult in the household; family instability; financial stress; parent legal problems; neighborhood disadvantage) and the ability to recognize facial displays of emotion measured using the faces subtest of the Diagnostic Assessment of Non-Verbal Accuracy (DANVA) at age 8.5 years. In addition to examining the role of exposure (vs. non-exposure) to each type of adversity, we also evaluated the role of the timing, duration, and recency of each adversity using a Least Angle Regression variable selection procedure.
Results
Over three-quarters of the sample experienced at least one adversity. We found no evidence to support an association between emotion recognition deficits and previous exposure to adversity, either in terms of total lifetime exposure, timing, duration, or recency, or when stratifying by sex.
Conclusions
Results from the largest population-based sample suggest that even extreme forms of adversity are unrelated to emotion recognition deficits as measured by the DANVA, suggesting the possible immutability of emotion recognition in the general population. These findings emphasize the importance of population-based studies to generate generalizable results.
Keywords: sensitive periods, children, emotion recognition, ALSPAC, adversity
Introduction
Numerous studies have documented the consequences of exposure to child adversity, including poverty (Brooks-Gunn and Duncan, 1997), abuse or maltreatment (Slopen et al., 2014, Widom et al., 2007), and family disruption or dysfunction (Gilman et al., 2003) on mental health outcomes. Overall, the effects of childhood adversity persist across the lifespan, at least doubling the risk of youth- and adult-onset mental disorders (Gilman et al., 2015, McLaughlin et al., 2010, McLaughlin et al., 2012). Given the strong evidence that childhood adversities are common, affecting upwards of 60% of the US (Koenen et al., 2010, Gilbert et al., 2009) and global populations (McLaughlin et al., 2012, Kessler et al., 2010), their associated mental health problems could affect large segments of the population. Yet, despite the ubiquity of adversity worldwide, the mechanisms linking adversity to psychopathology remain poorly characterized.
Here, we examined whether deficits in emotion recognition could be one pathway linking adversity to subsequent mental health problems. Emotion recognition skills, or the ability to recognize facial displays of emotion, are essential for navigating social interactions and interpreting communication signals indicating trustworthiness, intent, and empathy (Frith, 2009). Deficits in emotion recognition abilities have been linked to the etiology, course, and treatment of a wide range of psychiatric disorders including, depression, anxiety, autism, and schizophrenia (Bourke et al., 2010, Button et al., 2013, Boraston et al., 2007, Kohler et al., 2003). Many studies have also shown that children exposed to severe adversity – especially cases of abuse and maltreatment that come to the attention of authorities – are more likely than their unexposed peers to experience both biases and inaccuracies in detecting emotions (Cicchetti and Toth, 2005, Perlman et al., 2008, Pollak and Tolley-Schell, 2003, Striano et al., 2002). A smaller number of studies have also linked exposure to other types of adversity, including maternal depression, poverty, and institutional rearing, to emotion recognition difficulties (Bornstein et al., 2011, Evans, 2004, Parker et al., 2005)
Yet, prior work on the relationship between childhood adversity and emotion recognition deficits is limited in four important ways. First, most studies examine the effect of a single adversity, rather than multiple types, thus failing to account for a holistic set of experiences that might be driving emotion recognition (see a recent exception by: (Germine et al., 2015)). Second, few prior studies have examined how the developmental timing and duration of adversity influences emotion recognition deficits, even though emotion recognition skills are fine-tuned into adolescence in response to one’s unique social experiences. Third, only a handful of longitudinal studies exist; among these tend to be small-scale studies (n≤~100 children) that have almost exclusively focused on clinical samples (e.g., children with autism or at risk for schizophrenia), or high-risk samples of children exposed to extreme adversity (e.g., children in institutional care or with documented cases of child abuse and neglect) (Bouhuys et al., 1999, Kohler et al., 2000). Relatedly, there is a shortage of population-based studies, making the generalizability of prior findings unclear. To our knowledge, the only population-based study completed found no association between adversity and face emotion discrimination impairments (Germine et al., 2015); this cross-sectional study was conducted in a sample of over 5,000 adults where participants completed an emotion-recognition test anonymously through a website and retrospectively reported about their exposure to childhood adversity. Efforts to bring a population perspective to the fields of social, cognitive, and developmental neuroscience are needed as part of the movement towards “population neuroscience” (Falk et al., 2013).
In the current study, we addressed these limitations by examining whether exposure to a comprehensive set of childhood adversities predicted subsequent emotion recognition deficits within a large, population-based sample that prospectively followed children from infancy through middle childhood. Our primary aim was to determine if exposure to adversity at any point between birth and age 8 was associated with emotion recognition skills deficits at age 8.5. As a secondary aim, we sought to determine the extent to which the characteristics of adversity, including its timing and accumulation, could affect emotion recognition skills; to our knowledge, no other prior studies have examined such associations. We therefore tested three of the most popular models from lifecourse theory, each of which describes the association between an exposure and health outcome (Ben-Shlomo and Kuh, 2002), to determine which one (or more) models best fit with the data. The three models examined were: (a) a sensitive period model (Knudsen, 2004) in which the effect of adversity depends on the developmental time period of the exposure; (b) an accumulation model (Evans et al., 2013), in which the effect of adversity increases with the number of occasions exposed, regardless of timing; and (c) a recency model (Shanahan et al., 2011), in which the effect of adversity is stronger for more proximal events.
Methods
Sample and Procedures
Data came from the Avon Longitudinal Study of Parents and Children (ALSPAC), a prospective, longitudinal birth-cohort of children born to mothers who were living in the county of Avon England (120 miles west of London) with estimated delivery dates between April 1991 and December 1992 (Boyd et al., 2013). ALSPAC was designed to increase knowledge of the pathways to health across the lifespan, with an emphasis on genetic and environmental determinants. Approximately 85 percent of eligible pregnant women agreed to participate (n=14,541), and 76% of eligible live births who were alive at 12 months of age (n=13,988 children) were enrolled. Response rates to data collection have been good (75% have completed at least one follow-up). Ethics approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committee. More details are available on the ALSPAC website (www.bristol.ac.uk/alspac) including a fully searchable data dictionary.
There were 7,303 children who began the emotion recognition task, described below. We excluded from our analysis 797 children (10.9% of those who began the task) because the interviewer noted at the end of the task that the child had: (1) completed fewer than 23 out of the 24 emotion recognition trials (n=501); (2) appeared confused (n=40), dishonest (n=36), or bored with the task (n=139); or (3) did not seem to make a good attempt at the task (n=88). Children included in our analytic sample (n=6,506; 89.1% of the total sample who participated in the age 8 clinic assessment) did not differ from those who were excluded (n=797) with respect to age, race, sex, poverty level, parental educational status, previous pregnancies, or geographic location (all p-values >0.05).
Measures
Exposure to Adversity
We examined eight types of adversity, measured using parent mailed questionnaires. These adversities are commonly used to define early life adversity (Felitti et al., 1998, Slopen et al., 2014). Each adversity was measured on at least five occasions before age 8 years (Table 1).
Table 1.
Exposure to childhood adversity in the total sample and by the age at exposure
| Physical or emotional abuse |
Sexual or physical abuse (by anyone) |
Maternal psychopathology |
One adult in the household |
Family instability |
Financial stress |
Parent legal problems |
Neighborhood Disadvantage |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | N | (%) | |
|
|
||||||||||||||||
| Unexposed | 5517 | 85 | 5733 | 88 | 4651 | 72 | 5459 | 84 | 3534 | 54 | 4088 | 63 | 6131 | 94 | 5623 | 86 |
| Exposed | 989 | 15 | 773 | 12 | 1855 | 28 | 1047 | 16 | 2972 | 46 | 2418 | 37 | 375 | 6 | 883 | 14 |
| Age at Exposure | ||||||||||||||||
| Infancy | ||||||||||||||||
| Age 8 mo. | 217 | 3.7 | --- | --- | 593 | 10.2 | 235 | 4.1 | --- | --- | 715 | 12.3 | 72 | 1.2 | --- | --- |
| Age 1.5/1.75 | 240 | 4.2 | 139 | 2.4 | 583 | 10.4 | 279 | 5 | 1157 | 19.8 | 705 | 15.5 | 82 | 1.5 | 489 | 8.8 |
| Age 2.5/2.75 | 335 | 6.1 | 227 | 4.1 | 802 | 14.8 | 340 | 6.2 | 1168 | 20.9 | 653 | 11.9 | 99 | 1.8 | 405 | 7.5 |
| Preschool | ||||||||||||||||
| Age 3.5 | --- | --- | 183 | 3.3 | 749 | 14.1 | --- | --- | 1095 | 19.6 | 1255 | 20.1 | --- | --- | --- | --- |
| Age 4/4.75 | 279 | 5 | 201 | 3.7 | --- | --- | 389 | 7.2 | 729 | 13.3 | --- | --- | 96 | 1.8 | --- | --- |
| Age 5/5.75 | 378 | 7 | 174 | 3.3 | --- | --- | --- | --- | 599 | 11.3 | --- | --- | 83 | 1.6 | 303 | 5.7 |
| Middle Childhood | ||||||||||||||||
| Age 6/6.75 | 307 | 5.8 | 162 | 3 | 825 | 15.7 | --- | --- | 487 | 9.1 | --- | --- | 85 | 1.6 | --- | --- |
| Age 7 | --- | --- | --- | --- | --- | --- | 487 | 9.1 | --- | --- | 1137 | 18.3 | --- | --- | 242 | 4.5 |
| Age 8 | --- | --- | --- | --- | --- | --- | 505 | 9.4 | 467 | 8.4 | --- | --- | --- | --- | --- | --- |
Percentages for each age represent proportions of those exposed out of the total population.
--- indicates that the variable was not assessed at the corresponding time point
Caregiver physical or emotional abuse
Children were coded as having been exposed to physical or emotional abuse if the mother, partner, or both responded affirmatively to any of the following items: (1) Your partner was physically cruel to your children; (2) You were physically cruel to your children; (3) Your partner was emotionally cruel to your children; (4) You were emotionally cruel to your children.
Sexual or physical abuse
Exposure to sexual or physical abuse was determined through an item asking the mother to indicate whether or not the child had been exposed to either sexual or physical abuse from anyone.
Maternal psychopathology
Maternal psychopathology was determined using data from: (1) the Crown-Crisp Experiential Index (CCEI), which includes separate subscales for anxiety and depression (Crown and Crisp, 1979); (2) the Edinburgh Postnatal Depression Scale (EPDS) (Cox et al., 1987); and (3) a question asking about suicide attempts in the past 18 months. Consistent with prior ALSPAC studies (Enoch et al., 2010) and previous cut-points established in the literature (see below), we coded children as exposed to maternal psychopathology if one or more of the following criteria occurred: (1) the mother had a CCEI depression score greater than 9 (Crown and Crisp, 1979); (2) the mother had a CCEI anxiety score greater than 10 (Crown and Crisp, 1979); (3) the mother had an EPDS score greater than 12 (Cox et al., 1987); or (4) the mother reported a suicide attempt since the time of the last interview.
One adult in the household
Mothers indicated the number of adults (>18 years of age) living in the household. Children were coded as exposed if there were fewer than two adults in the household.
Family instability
Mothers indicated whether the child had been: (1) taken into care; (2) separated from their mother for two or more weeks; (3) separated from their father for two or more weeks; or (4) acquired a new parent. Children were coded as exposed if any of these events occurred.
Financial stress
Mothers indicated using a Likert-type scale (1=not difficult; 2=slightly difficult; 3=fairly difficult; 4=very difficult) the extent to which the family had difficulty affording the following: (1) items for the child; (2) rent or mortgage; (3) heating; (4) clothing; (5) food. Children were coded as exposed if their mothers reported at least slight difficulty for three or more items; this cut-point roughly corresponded to the top quartile.
Parent legal problems
Mothers indicated whether or not the child’s parents had experienced any encounters with the legal system. Children were coded as exposed if either or both parents had legal problems.
Neighborhood disadvantage
Mothers indicated the degree to which the following were problems in their neighborhood: (1) noise from other homes; (2) noise from the street; (3) garbage on the street; (4) dog dirt; (5) vandalism; (6) worry about burglary; (7) mugging; and (8) disturbance from youth. Response options to each item were: 2=serious problem, 1=minor problem, 0=not a problem or no opinion. Items were summed, yielding scores ranging from 0–16. Children with scores of eight or greater, which generally corresponded to the 95th percentile, were classified as exposed to neighborhood disadvantage.
Recognizing Facial Affect
The ability to recognize facial displays of emotion was measured using the faces subtest of the Diagnostic Assessment of Non-Verbal Accuracy (DANVA) at age 8.5 (Norwicki and Duke, 1994). In this computer-based task, the faces subtest consists of 24 colored photos of child faces (both male and female children who were primary school age). Each face displays one of four emotions: (a) happiness; (b) sadness; (c) anger; or (d) fear. Half of the photos were presented at a high intensity (e.g., extreme anger); the other half at a low intensity (e.g., mild anger). Following a two-second presentation, the child was asked to indicate the emotion displayed by the photo. The DANVA has been shown in studies of typically developmentally children to have good internal consistency reliability across age groups (α=0.77–0.88) and to correlate highly with indices of personal and social adjustment (e.g., self-esteem; relationship to peers) (Norwicki and Duke, 1994).
Consistent with prior literature (Barona et al., 2015, Kothari et al., 2013, Pollak et al., 2000, Gollan et al., 2008, Buhlmann et al., 2011, Sato et al., 2009, Surguladze et al., 2004, Gibb et al., 2009), we derived two sets of variables from these data. First, we examined the number of emotion-specific misattributions, meaning the total number of faces incorrectly identified as a specific emotion. For instance, children could have incorrectly identified a happy face as sad; this error would be classified as a misattribution of sad. We therefore summed the total number of faces misattributed as happy (range=0–13), sad (range=0–11), angry (range=0–7), or fearful (range=0–8). Second, we examined the incorrect identification of emotions generally, meaning a global measure indicating the total number of misattributions across all emotions. This variable was derived by summing across the emotion-specific misattributions (range=0–22).
Covariates
We controlled for the following covariates, measured at child birth: singleton v. multiple birth; number of previous pregnancies; maternal marital status; highest level of maternal education; maternal age; homeownership; and parent social class (see Appendix S1). These measures were shown here and elsewhere to correlate strongly with exposure to adversity and/or emotion recognition skills (Edwards et al., 2002, Schmidt et al., 2010).
Analyses
We began by running univariate and bivariate analyses to examine the distribution of covariates and exposure to adversity in the total analytic sample. Next, we used multiple linear regression to examine the association between exposure to each type of adversity (0=unexposed; 1=exposed at any time point) on the emotion recognition outcomes as well as a total adversity score indicating the total number of times exposed to each type of adversity (range 0–27). We then used a novel two-stage structured lifecourse modeling approach (SLCMA; Smith et al., 2015, Smith et al., 2016) to evaluate which of the three lifecourse theoretical models (sensitive period, accumulation, recency) could best explained this relationship. The major advantage of the SLCMA relative to other methods (e.g., standard multiple regression; structural equation modeling) is that it provides an unbiased way to compare multiple competing theoretical models simultaneously and identify the most parsimonious explanation for the observed outcome variation (see Appendix S1).
We also conducted two secondary analyses. First, we reran the primary analyses (described above) stratified by sex, given that prior studies have found sex differences in the prevalence of adversity (Koenen et al., 2010) as well as emotion recognition development and abilities (McClure, 2000). Second, building from the SLCMA, we fitted a linear regression model containing all possible theoretical models; this saturated model allowed us to determine if any hypothesized association (or combination of hypothesized associations) was present in the data.
To reduce potential bias and minimize loss of power due to attrition, we conducted all analyses using a multiply imputed dataset (see Appendix S1).
We also performed two sensitivity analyses to assess the robustness of our findings. First, we reran our analysis to modify our inclusion criteria, so that children were included in the analysis if they had completed at least 23 of the 24 trials and were reported by the interviewer to be bored, confused, dishonest, or gave a poor attempt at the task. Including these children (n=303) eliminated the possibility that children who had impairments in recognizing emotional faces were inappropriately excluded from the analysis. Second, given that prior literature has focused on both misattributions (where a face is incorrectly identified as expressing another emotion) as well as errors in recognizing a specific emotion, we also reran our primary analyses focusing on errors made in recognizing each of the four emotions and errors made across all emotions. These variables were derived by summing the total number of errors made in recognizing happy (range=0–6), sad (range=0–6), angry (range=0–6), or fearful faces (range=0–6) as well as the total number of errors made across all emotions (range=0–24).
Results
Sample Characteristics
The analytic sample was gender-balanced (50.5% female) and comprised of predominately White (96.1%) children from families whose parents were married and owned their home (Table S1).
Distribution of Exposure to Adversity and Emotion Recognition Skills
Most children (78%; n=5,063) experienced at least one adversity at some point in their life. Family instability (46%), financial stress (37%), and maternal psychopathology (28%) were the three most reported adversities (Table 1). Parent legal problems was the least reported adversity (6%). Age at exposure to adversity varied by type (Table 1). Within each adversity type, exposures were correlated over time (Table S1), with neighboring time points being generally more highly correlated than distant time points.
Children made the most emotion-specific misattributions in recognizing faces as happy (mean errors=2.13, median=2, SD=1.39), followed by sad (mean errors=1.24, median=1, SD=1.31) and fearful faces (mean errors=0.80, median=0, SD=1.09). The fewest misattributions were made in recognizing faces as angry (mean errors= 0.49, median=0, SD=.91). On average, children made 4.69 misattributions across all four emotions (median= 4, SD=2.74)
Exposure to any adversity was patterned by socio-demographic factors, though emotion recognition deficits were not (Table S2).
Association between Adversity and Emotion Recognition Models
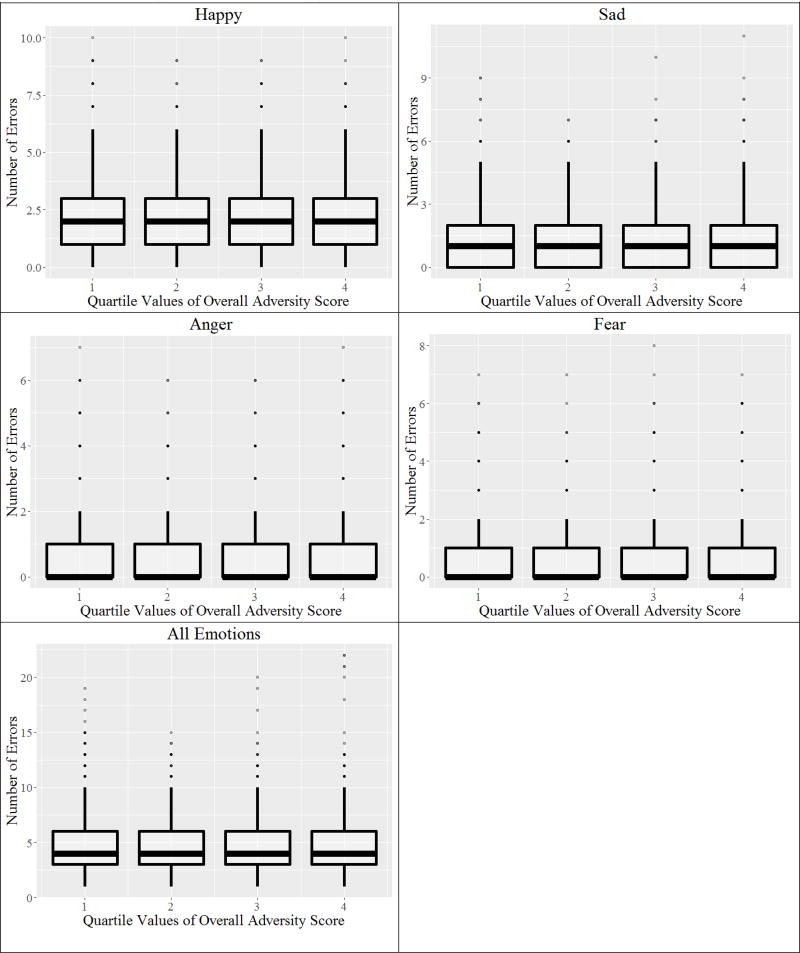
Results of the linear regression yielded little evidence of an association between exposure to each type of adversity (ever vs. never exposed) as well as the total adversity score on number of emotion recognition errors (all p-values >0.07; Table 2), with even extreme levels of adversity being unassociated (Figure 1).
Table 2.
Results of linear regression models examining ever vs. never exposed on multiply imputed data for each type of misattribution of a face as that emotion (N=6506)
|
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Happy | Sad | Angry | Fear | All Emotions | |||||||||||
|
|
|||||||||||||||
| Beta | 95% CI | p-value | Beta | 95% CI | p-value | Beta | 95% CI | p-value | Beta | 95% CI | p-value | Beta | 95% CI | p-value | |
| Exposed (vs. unexposed) | |||||||||||||||
| Physical or emotional abuse | 0.05 | −0.04, 0.15 | 0.27 | 0.02 | −0.07, 0.11 | 0.69 | 0.02 | −0.04, 0.09 | 0.49 | −0.04 | −0.12, 0.03 | 0.27 | 0.05 | −0.15, 0.24 | 0.62 |
| Sexual or physical abuse | −0.10 | −0.20, 0.01 | 0.07 | −0.02 | −0.10, 0.09 | 0.97 | −0.01 | −0.07, 0.07 | 0.97 | 0.06 | −0.02, 0.15 | 0.15 | −0.04 | −0.25, 0.17 | 0.72 |
| Maternal psychopathology | < 0.01 | −0.07, 0.08 | 0.96 | −0.02 | −0.10, 0.05 | 0.53 | −0.01 | −0.06, 0.04 | 0.75 | −0.04 | −0.10, 0.02 | 0.20 | −0.07 | −0.22, 0.08 | 0.37 |
| One adult in the household | 0.05 | −0.05, 0.15 | 0.32 | −0.07 | −0.16, 0.02 | 0.15 | 0.01 | −0.05, 0.08 | 0.70 | 0.01 | −0.08, 0.09 | 0.87 | < 0.01 | −0.20, 0.20 | 0.99 |
| Family instability | −0.01 | −0.09, 0.06 | 0.72 | −0.05 | −0.12, 0.01 | 0.12 | −0.04 | −0.09, 0.01 | 0.08 | −0.02 | −0.07, 0.04 | 0.57 | −0.12 | −0.27, 0.02 | 0.09 |
| Financial stress | −0.04 | −0.12, 0.03 | 0.28 | −0.04 | −0.11, 0.03 | 0.24 | −0.02 | −0.07, 0.03 | 0.44 | 0.01 | −0.05, 0.07 | 0.75 | −0.09 | −0.24, 0.05 | 0.22 |
| Parent legal problems | 0.04 | −0.11, 0.18 | 0.60 | −0.09 | −0.23, 0.05 | 0.19 | −0.02 | −0.12, 0.08 | 0.69 | 0.01 | −0.11, 0.13 | 0.89 | −0.07 | −0.36, 0.23 | 0.66 |
| Neighborhood disadvantage | −0.05 | −0.15, 0.05 | 0.31 | 0.01 | −0.08, 0.10 | 0.84 | < 0.01 | −0.07, 0.07 | 0.95 | 0.05 | −0.03, 0.13 | 0.26 | < 0.01 | −0.19, 0.20 | 0.96 |
| Cumulative exposure | −0.04 | −0.13, 0.05 | 0.38 | −0.02 | −0.11, 0.07 | 0.64 | <0.01 | −0.06, 0.07 | 0.88 | 0.05 | 0.03, 0.12 | 0.23 | −0.01 | −0.19, 0.17 | 0.90 |
Cell entries are betas, 95% confidence intervals, and p-values derived from nine multiple linear regression (one for each type of adversity plus a model for cumulative exposure). Cumulative exposure was defined as a total of all adversity exposures over all time periods.
Figure 1.
Relationship between the adversity score and misattribution of a face as each emotion
In the SLCMA analysis all lifecourse theoretical models were weak and inconclusive predictors of emotion recognition (p>0.17; Table 3).
Table 3.
Results of LARS models on multiply imputed data for each type of misattribution of a face as that emotion (N=6506)
| Happy | Sad | Fear | Anger | All Emotions | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Model(s) selected |
p-value | Model(s) selected |
p-value | Model(s) selected |
p-value | Model(s) selected |
p-value | Model(s) selected |
p-value | |
|
|
||||||||||
| Physical or emotional abuse | 2.75 Years | 0.31 | 2.75 Years | 0.73 | 5 Years | 0.96 | 8 Months | 0.61 | 6 Years | 0.95 |
| Sexual or physical abuse | 1.5 Years | 0.74 | 1.5 Years | 0.75 | 2.5 Years | 0.17 | Recency | 0.88 | 4.75 Years | 0.36 |
| Maternal psychopathology | 1.75 Years | 0.48 | 6 Years | 0.75 | 1.75 Years | 0.21 | 5 Years | 0.97 | 6 Years | 0.45 |
| One adult in the household | 6 Years | 0.19 | 7 Years | 0.43 | 8 Months | 0.54 | 2.75 Years | 0.78 | 6 Years | 0.83 |
| Family instability | 3.5 Years | 0.79 | 2.5 Years | 0.40 | 4.75 Years | 0.96 | Accumulation | 0.57 | 3.5 Years | 0.85 |
| Financial stress | 2.75 Years | 0.75 | 7 Years | 0.54 | 2.75 Years | 0.59 | 7 Years | 0.93 | 7 Years | 0.99 |
| Parent legal problems | 8 Months | 0.98 | 6 Years | 0.65 | 5 Years | 0.94 | 4 Years | 0.83 | 5 Years | 0.51 |
| Neighborhood disadvantage | 5 Years | 0.81 | 5 Years | 0.86 | 2.75 Years | 0.78 | 1.75 Years | 0.89 | 2.75 Years | 0.76 |
The table indicates the set of theoretical models chosen by LARS, after adjusting for covariates.
These results were robust to stratification by sex. Lifetime exposure to adversity was unassociated with emotion recognition deficits in both boys and girls (Table S3). The lifecourse theoretical models did not explain substantial variability (Table S4), even when all theoretical models were considered simultaneously in the saturated model (Table S5).
Sensitivity Analysis
Results with the more inclusive sample (n=6694), which included children who were initially excluded, were nearly identical to the results from the smaller, less inclusive sample (n=6506). Specifically, no significant associations were detected between lifetime exposure to adversity and emotion specific misattributions in the inclusive sample (Table S6). Further, the SLCMA analysis showed no significant associations between any of the lifecourse theoretical models and misattributions (Table S7).
Furthermore, there was little evidence of an association between exposure to each type of adversity whether in errors made un recognizing each emotion or all emotions combined. Only 2 out of 45 significant associations were detected, which showed an increased risk of making errors in recognizing happy faces among children exposed to sexual or physical abuse (β= 0.09; p=0.001; OR= 0.04–0.14) and an increased risk of making errors in recognizing fearful faces among children who experienced neighborhood disadvantage (β= −0.13; p= 0.036; OR = −0.22– −0.01) (Table S8). However, all lifecourse theoretical models were weak and inconclusive predictors of the total number of emotion recognition errors (Table S9).
Discussion
The major finding of this study is that exposure to adversity appears unassociated with emotion recognition deficits in this population-based sample of children. This lack of association was observed regardless of how we characterized adversity (e.g., focusing on its timing, duration, recency or severe forms), whether we examined adversities individually or all together, and whether we conducted the analyses in the total sample or stratified by sex. Our results are consistent with the one other population-based study conducted, which also found no association between adversity and face emotion discrimination impairments (Germine et al., 2015). Our study differed from this prior study (Germine et al., 2015) in that our work uses prospective data collection, making the reports of timing and adversity more likely to be accurate; furthermore, our study uses a validated clinical measure administered by trained testers as opposed to an internet questionnaire. However, our results differ from dozens of studies using more selective samples, which have generally found robust associations between exposure to adversity and emotion recognition deficits (Pollak and Tolley-Schell, 2003, Pollak, 2008).
What could explain such discrepancies between our study and the prior literature? First, the faces subtest of the DANVA could have been unable to detect subtle differences in facial emotion recognition, even though both high and low intensity of emotions were presented. More recent emotion recognition tasks capture both subtle and dramatic changes in emotional states and the social context in which the child was reporting (e.g., through vignettes, either read aloud or acted out, that are matched to emotional faces) (Button et al., 2013). Additionally, the limited number of trials in the DANVA, which were 24 in total (6 for each emotion), could not have resulted in enough between-subject variation. Nevertheless, the measure should have been sensitive to capture meaningful differences, if they existed, given that there was a range of scores in our sample (though scores were skewed towards lower values), and the DANVA has been used successfully in other population-based samples, including ALSPAC, to differentiate children who are at risk for eating disorders, have social communication difficulties, and are at risk for autism or ADHD (Kothari et al., 2015, Kothari et al., 2013, Ingersoll and Lalonde, 2010, McKown et al., 2013).
Second, our measurement of emotion recognition skills (at 8.5 years of age) could be poorly timed. Prior studies have focused on children outside of this age, namely toddlers (3–5 years) (Pollak et al., 2000, Perlman et al., 2008), or teenagers (10 years and up) (Joormann et al., 2010, Dadds et al., 2012). However, research in the development of emotion recognition suggests that emotion recognition skills develop and change not only in early childhood, but well through the teenage years (Thomas et al., 2007). Thus, our study appears to capture an understudied, but relevant, developmental stage.
Lastly, it is possible that emotion recognition deficits are not observed following exposure to adversity among typically developing children. Our sample was comprised of predominately white families who were married and owned their own home; children growing-up in this type of traditional family likely have very different social and other experiences as compared to children growing-up in less stable environments. Adversity may only affect emotion recognition abilities in very extreme samples. It is also possible that methodological limitations led prior studies to identify associations that were explained by other factors including current mental health problems. Indeed, among the two longitudinal studies we identified, neither controlled for prior mental health problems, which could result in residual confounding.
Notably, our study was powered to detect even small effect estimates. A post-hoc power calculation suggested our analytic sample size was capable of detecting between group differences of at least small effect (Cohen’s d=0.07–0.11) given at least 80% power and with our observed lifetime prevalence of adversity at 6–46%. As most prior studies have found effect estimates an order of magnitude larger than ours, our results do not appear attributable to low power, especially given the narrow confidence intervals observed, rather they suggest the association between adversity and emotion recognition is inconclusive.
Several limitations are noted. Our adversity measures came primarily from parent-reported questionnaires, which prior studies suggest may lead to under-reporting (Goodman and Goodman, 2011). Some measures of adversity were also derived from single items, which could affect the precision of these estimates. However, the prevalence of exposure to each adversity in ALSPAC, which ranged from 6–46%, were similar to prevalence estimates derived from nationally-representative epidemiological samples in the United States, which have found that close to 40% of adolescents have experienced some type of childhood adversity (McLaughlin et al., 2012, Gilbert et al., 2009). Although experiences of adversity may be less well-characterized in our sample compared to others, as some of our measures were derived from single-item questionnaires rather than more in-depth assessments, the use of these questionnaires allowed for a significantly larger sample size than has been previously used. We were also unable to examine the effect of exposure to multiple types of adversity during the same developmental period, as each adversity was measured at a different time point. We were also limited by how the adversities were originally collected. Notably, the variables caregiver physically and emotional abuse and sexual or physical abuse were derived from different surveys and question sets, thus creating overlap between the two variables in children who were physically abused by a caregiver. Additionally, as with any longitudinal study, there was attrition over time, which we attempted to address using multiple imputation. Finally, our inability to capture perceptions of neutral faces, which are omitted from the DANVA, is also a limitation, though the DANVA has been well validated without neutral faces.
In summary, our results suggest that exposure to childhood adversity does not impair emotion recognition abilities among children in the general population. The results highlight the importance of generating and triangulating results across multiple study samples to identify general versus specific effects of adversity on emotion recognition.
Supplementary Material
Key Points.
Emotion recognition skills are essential for effective social communication, and deficits in these skills have been implicated in mental health problems.
Prior studies of clinical and high-risk samples have consistently shown that children exposed to adversity are more likely than their unexposed peers to have emotion recognition skills deficits.
However, only one population-based study has examined this association.
In this large-population-based sample, we found no evidence to support an association between emotion recognition deficits and previous exposure to adversity.
These findings underscore the need for population-based studies to generate generalizable results.
Acknowledgments
The UK Medical Research Council and the Wellcome Trust (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. This publication is the work of the authors, who will serve as guarantors for the contents of this paper. This research was specifically funded by the National Institute of Mental Health of the National Institutes of Health under Award Number K01MH102403, a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation, and the Medical Research Council and the University of Bristol (MC_UU_12013/6). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses.
Abbreviations
- ALSPAC
Avon Longitudinal Study of Parents and Children
- DANVA
Diagnostic Assessment of Non-Verbal Accuracy
- LARs
Least Angle Regression
Footnotes
The authors have declared that they have no competing or potential conflicts of interest.
Additional Supporting Information may be found in the online version of this article:
References
- Barona M, Kothari R, Skuse D, Micali N. Social communication and emotion difficulties and second to fourth digit ratio in a large community-based sample. Mol Autism. 2015;6:68. doi: 10.1186/s13229-015-0063-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chroic disease epidemiology: conceptual models, empirical challenges, and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31:285–293. [PubMed] [Google Scholar]
- Boraston Z, Blakemore SJ, Chilvers R, Skuse D. Impaired sadness recognition is linked to social interaction deficit in autism. Neuropsychologia. 2007;45:1501–1510. doi: 10.1016/j.neuropsychologia.2006.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornstein MH, Arterberry ME, Mash C, Manian N. Discrimination of facial expression by 5-month-old infants of nondepressed and clinically depressed mothers. Infant Behav Dev. 2011;34:100–106. doi: 10.1016/j.infbeh.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouhuys AL, Geerts E, Gordijn MC. Depressed patients' perceptions of facial emotions in depressed and remitted states are associated with relapse: a longitudinal study. J Nerv Ment Dis. 1999;187:595–602. doi: 10.1097/00005053-199910000-00002. [DOI] [PubMed] [Google Scholar]
- Bourke C, Douglas K, Porter R. Processing of facial emotion expression in major depression: a review. Aust N Z J Psychiatry. 2010;44:681–696. doi: 10.3109/00048674.2010.496359. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort Profile: the 'children of the 90s'--the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks-Gunn J, Duncan GJ. Effects of poverty on children. The future of Children. 1997;7:55–71. [PubMed] [Google Scholar]
- Buhlmann U, Gleiss MJ, Rupf L, Zschenderlein K, Kathmann N. Modifying emotion recognition deficits in body dysmorphic disorder: an experimental investigation. Depress Anxiety. 2011;28:924–931. doi: 10.1002/da.20887. [DOI] [PubMed] [Google Scholar]
- Button K, Lewis G, Penton-Voak I, Munafo M. Social anxiety is associated with general but not specific biases in emotion recognition. Psychiatry Res. 2013;210:199–207. doi: 10.1016/j.psychres.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1:409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Crown S, Crisp AH. Manual of the Crown-Crisp Experiential Index. London: Hodder and Stoughton; 1979. [Google Scholar]
- Dadds MR, Cauchi AJ, Wimalaweera S, Hawes DJ, Brennan J. Outcomes, moderators, and mediators of empathic-emotion recognition training for complex conduct problems in childhood. Psychiatry Res. 2012;199:201–207. doi: 10.1016/j.psychres.2012.04.033. [DOI] [PubMed] [Google Scholar]
- Edwards J, Jackson HJ, Pattison PE. Emotion recognition via facial expression and affective prosody in schizophrenia: a methodological review. Clin Psychol Rev. 2002;22:789–832. doi: 10.1016/s0272-7358(02)00130-7. [DOI] [PubMed] [Google Scholar]
- Enoch M-A, Steer CD, Newman TK, Gibson N, Goldman D. Early Life Stress, MAOA, and Gene-Environment Interactions Predict Behavioral Disinhibition in Children. Genes, brain, and behavior. 2010;9:65–74. doi: 10.1111/j.1601-183X.2009.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW. The environment of childhood poverty. Am Psychol. 2004;59:77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychological Bulletin. 2013;139:342–396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Falk EB, Hyde LW, Mitchell C, Faul J, Gonzalez R, Heitzeg MM, Keating DP, Langa KM, Martz ME, Maslowsky J, Morrison FJ, Noll DC, Patrick ME, Pfeffer FT, Reuter-Lorenz PA, Thomason ME, Davis-Kean P, Monk CS, Schulenberg J. What is a representative brain? Neuroscience meets population science. Proc Natl Acad Sci U S A. 2013;110:17615–17622. doi: 10.1073/pnas.1310134110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards VJ, Koss MP, Marks JS. Relationships of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Frith C. Role of facial expressions in social interactions. Philos Trans R Soc Lond B Biol Sci. 2009;364:3453–3458. doi: 10.1098/rstb.2009.0142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germine L, Dunn EC, Mclaughlin KA, Smoller JW. Childhood adversity is associated with adult theory of mind and social affiliation, but not face processing. PLoS One. 2015;10:e0129612. doi: 10.1371/journal.pone.0129612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb BE, Schofield CA, Coles ME. Reported history of childhood abuse and young adults' information-processing biases for facial displays of emotion. Child Maltreat. 2009;14:148–156. doi: 10.1177/1077559508326358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R, Spatz Widom C, Browne K, Fergusson D, Webb E, Janson S. Child maltreatment 1: Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL. Family disruption in childhood and risk of adult depression. American Journal of Psychiatry. 2003;160:939–946. doi: 10.1176/appi.ajp.160.5.939. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Ni MY, Dunn EC, Breslau J, Mclaughlin KA, Smoller JW, Perlis RH. Contributions of the social environment to first-onset and recurrent mania. Mol Psychiatry. 2015;20:329–336. doi: 10.1038/mp.2014.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollan JK, Pane HT, Mccloskey MS, Coccaro EF. Identifying differences in biased affective information processing in major depression. Psychiatry Res. 2008;159:18–24. doi: 10.1016/j.psychres.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman A, Goodman R. Population mean scores predict child mental disorder rates: validating SDQ prevalence estimators in Britain. J Child Psychol Psychiatry. 2011;52:100–108. doi: 10.1111/j.1469-7610.2010.02278.x. [DOI] [PubMed] [Google Scholar]
- Ingersoll B, Lalonde K. The impact of object and gesture imitation training on language use in children with autism spectrum disorder. J Speech Lang Hear Res. 2010;53:1040–1051. doi: 10.1044/1092-4388(2009/09-0043). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joormann J, Gilbert K, Gotlib IH. Emotion identification in girls at high risk for depression. J Child Psychol Psychiatry. 2010;51:575–582. doi: 10.1111/j.1469-7610.2009.02175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Mclaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Aguilar-Gaxiola S, Alhamzawi AO, Alonso J, Angermeyer M, Benjet C, Bromet E, Chatterji S, De Girolamo G, Demyttenaere K, Fayyad J, Florescu S, Gal G, Gureje O, Haro JM, Hu C-Y, Karam EG, Kawakami N, Lee S, Lépine J-P, Ormel J, Posada-Villa J, Sagar R, Tsang A, Üstün TB, Vassilev S, Viana MC, Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. The British Journal of Psychiatry. 2010;197:378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen E. Sensitive periods in the development of the brain and behavior. J Cogn Neurosci. 2004;16:1412–1425. doi: 10.1162/0898929042304796. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Roberts A, Stone D, Dunn EC. The epidemiology of early childhood trauma. In: Lanius R, Vermetten E, editors. The hidden epidemic: The impact of early life trauma on health and disease. New York, NY: Oxford University; 2010. pp. 13–24. [Google Scholar]
- Kohler CG, Bilker W, Hagendoorn M, Gur RE, Gur RC. Emotion recognition deficit in schizophrenia: association with symptomatology and cognition. Biol Psychiatry. 2000;48:127–136. doi: 10.1016/s0006-3223(00)00847-7. [DOI] [PubMed] [Google Scholar]
- Kohler CG, Turner TH, Bilker WB, Brensinger CM, Siegel SJ, Kanes SJ, Gur RE, Gur RC. Facial emotion recognition in schizophrenia: intensity effects and error pattern. Am J Psychiatry. 2003;160:1768–1774. doi: 10.1176/appi.ajp.160.10.1768. [DOI] [PubMed] [Google Scholar]
- Kothari R, Barona M, Treasure J, Micali N. Social cognition in children at familial high-risk of developing an eating disorder. Front Behav Neurosci. 2015;9:208. doi: 10.3389/fnbeh.2015.00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kothari R, Skuse D, Wakefield J, Micali N. Gender differences in the relationship between social communication and emotion recognition. J Am Acad Child Adolesc Psychiatry. 2013;52:1148–1157. e1142. doi: 10.1016/j.jaac.2013.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcclure EB. A meta-analytic review of sex differences in facial expression processing and their development in infants, children, and adolescents. Psychol Bull. 2000;126:424–453. doi: 10.1037/0033-2909.126.3.424. [DOI] [PubMed] [Google Scholar]
- Mckown C, Allen AM, Russo-Ponsaran NM, Johnson JK. Direct assessment of children's social-emotional comprehension. Psychol Assess. 2013;25:1154–1166. doi: 10.1037/a0033435. [DOI] [PubMed] [Google Scholar]
- Mclaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication II: Associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mclaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. JAMA Psychiatry. 2012;69:1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norwicki S, Duke MP. Individual differences in the nonverbal communication of affect: The diagnostic analysis of nonverbal accuracy scale. Journal of Nonverbal Behavior. 1994;18:9–36. [Google Scholar]
- Parker SW, Nelson CA, BUCHAREST EARLY INTERVENTION PROJECT CORE, G An event-related potential study of the impact of institutional rearing on face recognition. Dev Psychopathol. 2005;17:621–639. doi: 10.1017/S0954579405050303. [DOI] [PubMed] [Google Scholar]
- Perlman S, Kalish C, Pollak S. The role of maltreatment experience in children's understanding of the antecedents of emotion. Cognition & Emotion. 2008;22:651–670. [Google Scholar]
- Pollak SD. Mechanisms linking early experience and the emergency of emotions: Illustrations from the study of maltreated children. Current directions in psychological science. 2008;17:370–375. doi: 10.1111/j.1467-8721.2008.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollak SD, Cicchetti D, Hornung K, Reed A. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology. 2000;36:679–688. doi: 10.1037/0012-1649.36.5.679. [DOI] [PubMed] [Google Scholar]
- Pollak SD, Tolley-Schell SA. Selecting attention to facial emotion in physically abused children. Journal of Abnormal Psychology. 2003;112:323–338. doi: 10.1037/0021-843x.112.3.323. [DOI] [PubMed] [Google Scholar]
- Sato W, Uono S, Matsuura N, Toichi M. Misrecognition of facial expressions in delinquents. Child Adolesc Psychiatry Ment Health. 2009;3:27. doi: 10.1186/1753-2000-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt AT, Orsten KD, Hanten GR, Li X, Levin HS. Family environment influences emotion recognition following paediatric traumatic brain injury. Brain Inj. 2010;24:1550–1560. doi: 10.3109/02699052.2010.523047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanahan L, Copeland WE, Costello EJ, Angold A. Child-, adolescent- and young adult-onset depressions: differential risk factors in development? Psychol Med. 2011;41:2265–2274. doi: 10.1017/S0033291711000675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Koenen KC, Kubzansky LD. Cumulative adversity in childhood and emergent risk factors for long-term health. Journal of Pediatrics. 2014;164:631–638. doi: 10.1016/j.jpeds.2013.11.003. [DOI] [PubMed] [Google Scholar]
- Smith AD, Hardy R, Heron J, Joinson CJ, Lawlor DA, Macdonald-Wallis C, Tilling K. A structured approach to hypotheses involving continuous exposures over the life course. Int J Epidemiol. 2016 doi: 10.1093/ije/dyw164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AD, Heron J, Mishra G, Gilthorpe MS, Ben-Shlomo Y, Tilling K. Model Selection of the Effect of Binary Exposures over the Life Course. Epidemiology. 2015;26:719–726. doi: 10.1097/EDE.0000000000000348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striano T, Brennan PA, Vanman EJ. Maternal Depressive Symptoms and 6-Month-Old Infants' Sensitivity to Facial Expressions. Infancy. 2002;3:115–126. [Google Scholar]
- Surguladze SA, Young AW, Senior C, Brebion G, Travis MJ, Phillips ML. Recognition accuracy and response bias to happy and sad facial expressions in patients with major depression. Neuropsychology. 2004;18:212–218. doi: 10.1037/0894-4105.18.2.212. [DOI] [PubMed] [Google Scholar]
- Thomas J, Knowles R, Tai S, Bentall RP. Response styles to depressed mood in bipolar affective disorder. J Affect Disord. 2007;100:249–252. doi: 10.1016/j.jad.2006.10.017. [DOI] [PubMed] [Google Scholar]
- Widom CS, Dumont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.