Highlights
-
•
We made Roux-en-Y hepaticojejunostomy without transhepatic billiary stent and also without Witzel drainage one month after iatrogenic high transectional lesion (Class E) of both hepatic ducts during laparoscopic cholecystectomy was performed.
-
•
We created a part of anastomosis between the jejunum and liver capsula with polydioxanone suture (PDS) 4-0 because of poor quality of the remaining parts of the hepatic ducts. We had to made two separate hepaticojejunal anastomoses (left and right) that we partly connected to the liver capsule, where we had a defect of hepatic ducts, without Witzel enterostomy and transhepatic biliary stent.
-
•
There were no significant postoperative complications.
-
•
We did magnetic resonance cholangiopancreatography (MRCP) one year after the surgical procedure, which showed the proper width of the intrahepatic bile ducts, with no signs of stenosis of anastomoses.
-
•
We tried and managed to avoid such types of drainage and proved that in this way, without those types of drainage, we can successfully do duplex hepaticojejunal anastomoses and that they can survive without complications.
-
•
Our case indicates that this approach can be successfully used for surgical repair of iatrogenic lesion of both hepatic ducts.
Keywords: Laparoscopic cholecystectomy, Iatrogenic bile duct injuries, Roux-en-Y hepaticojejunostomy without Witzel enterostomy and transhepatic biliary stent
Abstract
Introduction
Most of the case reports about high type iatrogenic hepatic duct injuries reports how to treat and make Roux-en-Y hepaticojejunostomy below the junction of the liver immediately after this condition is recognised during surgical procedure when the injury was made. Hereby we present a case where we made Roux-en-Y hepaticojejunostomy without transhepatic billiary stent and also without Witzel drainage one month after the iatrogenic injury.
Presentation of case
A 21-year-old woman suffered from iatrogenic high transectional lesion of both hepatic ducts during laparoscopic cholecystectomy in a local hospital. Iatrogenic injury was not immediately recognized. Ten days later due to patient complaints and large amount of bile in abdominal drain sac, second surgery was performed to evacuate biloma. Symptoms reappeared again, together with bile in abdominal sac, and then patient was sent to our Clinical Center.
After performing additional diagnostics, high type (Class E) of iatrogenic hepatic duct injury was diagnosed. A revision surgical procedure was performed. During the exploration we found high transection lesion of right and left hepatic duct, and we decided to do Roux-en-Y hepaticojejunostomy. We created a part of anastomosis between the jejunum and liver capsule with polydioxanone suture (PDS) 4-0 because of poor quality of the remaining parts of the hepatic ducts. We made two separate hepaticojejunal anastomoses (left and right) that we partly connected to the liver capsule, where we had a defect of hepatic ducts, without Witzel enterostomy and transhepatic biliary stent. There were no significant postoperative complications. Magnetic resonance cholangiopancreatography (MRCP) was made one year after the surgical procedure, which showed the proper width of the intrahepatic bile ducts, with no signs of stenosis of anastomoses.
Discussion
In most cases, treatment iatrogenic BDI is based on primary repair of the duct, ductal repair with a stent or creating duct-enteric anastomosis, often used and drainage by Witzel (Witzel enterostomy). Reconstructive hepaticojejunostomy is recommended for major BDIs during cholecystectomy. Considering that the biliary reconstruction with Roux-en-Y hepatojejunostomy is usually made with transhepatic biliary stent or Witzel enterostomy. What is interesting about this case is that these types of drainages were not made. We tried and managed to avoid such types of drainage and proved that in this way, without those types of drainage, we can successfully do duplex hepaticojejunal anastomoses and that they can survive without complications.
Conclusion
Our case indicates that this approach can be successfully used for surgical repair of iatrogenic lesion of both hepatic ducts.
1. Introduction
Iatrogenic bile duct injuries (BDI) are most frequently caused by laparoscopic cholecystectomy (LC), which is one of the most common surgical procedures in the world, because now LC is the gold standard for gallbladder removal in the management of symptomatic cholelithiasis [1]. The most common reasons for iatrogenic BDI are: existence of acute inflammation of the gallbladder, obesity, misidentification of biliary anatomy before clipping, bleeding in the surgical area and anatomic variations. These local risk factors seem to be presented in 15%–35% of iatrogenic BDI. Abnormal biliary anatomy, such as a short cystic duct or a cystic duct entering into the right hepatic duct also may increase the incidence of iatrogenic BDI [2].
There are many classifications of common bile duct injury, but injuries of both left and right hepatic ducts during elective cholecystectomy are extremely rare and represent serious injuries; accordingly, their management is a particular challenge in hepatobiliary surgery [3]. The early and proper diagnosis of iatrogenic BDI is very important for surgeons and gastroenterologists because unrecognized BDI leads to serious complications such as biliary cirrhosis, hepatic failure and even death [4].
Complications of the biliary leak such as cholangitis, bleeding, anastomotic strictures and biliary cirrhosis remain a major concern affecting a patient’s outcome after the surgical operation is done [5]. Bile duct lesions were more common in laparoscopic cholecystectomy, the incidence is about 0.6% than in laparotomy method where the incidence is about 0.1% [[6], [7], [8], [9]].
In most cases, treatment of iatrogenic BDI is based on primary repair of the duct, ductal repair with a stent, or creating duct-enteric anastomosis, often used and drainage by Witzel (Witzel enterostomy). Reconstructive hepaticojejunostomy is often recommended for major iatrogenic BDI during cholecystectomy [10].
The aim of our case is to show that both hepaticojejunal anastomosis were functional and without stenosis after 1 year of surgical repair of iatrogenic lesion of both hepatic ducts. Anastomoses were created one month after lesions of both hepatic ducts were made, as soon as the lesions are recognized, and without the use of biliary stents and Witzel enterostomy. While we were writing this case report, we have followed the SCARE guidelines [14].
2. Case presentation
A 21-year-old woman without previous medical history, underwent laparoscopic cholecystectomy in local hospital. After the surgery, she complained about pain in the upper right abdomen, nausea and night fever. Larger amounts of bile content were found in abdominal drain sac, and therefore the ultrasonography (US) of abdomen was performed. US showed a presence of free intraabdominal fluid and the audit surgery was made 10 days after the first surgical procedure (cholecystectomy), also in the local hospital. During that audit surgery the biloma was evacuated, and toilette of abdominal cavity with drainage was done.
The third day after the second surgery the patient started complaining about frequent pain in the upper abdomen, feeling of sickness, fever and occasional vomiting. Laboratory tests indicated hyperbilirubinaemia, increased levels of aspartate transaminase (AST), alanine aminotransferase (ALT), C-reactive protein (CRP) and white blood cells (WBC). After recurrence of biliary content in abdominal drain sac, the abdominal US was carried out and it showed presence of free intraabdominal fluid. The patient was then sent to Department of Surgery in our Clinical Center for further diagnostic and surgical treatment.
After patient presented to our Clinical Center (1 month after the first, and 20 days after the second surgery) she complained about the frequent pain in the upper abdomen, feeling of sickness and fever. We found 200 ml of bile content in her abdominal drain sac. We made complete diagnostic evaluation. Laboratory tests upon patient’s arrival showed the following results: Total bilirubin was 21.05 (3–19 umol/L), Indirect bilirubin 6.20 (0–19 umol/L), Direct bilirubin 15.30 (0–5 umol/L), CRP 115 (0.0–3.3 mg/L), Amylase (u) 447 (0–400 U/L), Amylase (s) 62 (25–125 U/L), AST 24 (9–36 U/L), ALT 56 (15–60 U/L), WBC 12.30 (3.40–9.70 × 10*9/L). The abdominal US showed presence of free intraabdominal fluid. A CT of abdomen was performed, which showed extravasation of the contrast agent in the region of both hepatic ducts and presence of lesions of the left and right hepatic duct. It also showed presence of biloma and intraabdominal abscess collection (Fig. 1).
Fig. 1.
Preoperative CT of abdomen cavity.
A CT of abdomen was performed, which showed extravasation of the contrast agent in the region of both hepatic ducts and presence of lesions of the left and right hepatic duct. It also showed presence of biloma and intraabdominal abscess collection (Fig. 1).
We prescribed all necessary medication and infusion therapy (adequate fluid replenishment and electrolyte, low molecular weight heparin, antiemetic, proton pump inhibitor, high proteins preparations as well as analgesic and double antibiotic therapy. We decided that the third surgery is necessary.
We performed the Orr incision to open the abdominal cavity. The surgical procedure was performed by a surgeon with many years of experience in hepatobiliary surgery.
During the exploration we found high type (Class E) transection lesion of right and left hepatic duct, and we decided to do Roux-en-Y hepaticojejunostomy. Because of the lesion of the both hepatic ducts in the hilus of the liver, biliary peritonitis and poor quality of the remaining part of the hepatic ducts, we created a part of anastomosis between the jejunum and liver capsule with polydioxanone suture (PDS) 4-0 without Witzel enterostomy and transhepatic biliary stent. We made two separate hepaticojejunal anastomoses (left and right) that we partly connected to the liver capsule, where we had a defect of hepatic ducts (portoenterostomia) (Fig. 2). After that we made entero-entero anastomoses to continue the continuity of the digestive tube. With the evacuation of the abscess collections, the abdominal cavity toilet and the placement of abdominal drain, we completed the surgical procedure. There was no blood loss during the operative procedure. The operation lasted for 3 h.
Fig. 2.
Intraoperative duplex Roux-en-Y hepatojejunostomy.
We performed the Orr incision to open the abdominal cavity. During the exploration we found high type (Class E) transection lesion of right and left hepatic duct, and we decided to do Roux-en-Y hepaticojejunostomy. Because of the lesion of the both hepatic ducts in the hilus of the liver, biliary peritonitis and poor quality of the remaining part of the hepatic ducts, we created a part of anastomosis between the jejunum and liver capsule with polydioxanone suture (PDS) 4-0 without Witzel enterostomy and transhepatic biliary stent. We made two separate hepaticojejunal anastomoses (left and right) that we partly connected to the liver capsule, where we had a defect of hepatic ducts (portoenterostomia) (Fig. 2). After that we made entero-entero anastomoses to continue the continuity of the digestive tube. With the evacuation of the abscess collections, the abdominal cavity toilet and the placement of abdominal drain, we completed the surgical procedure.
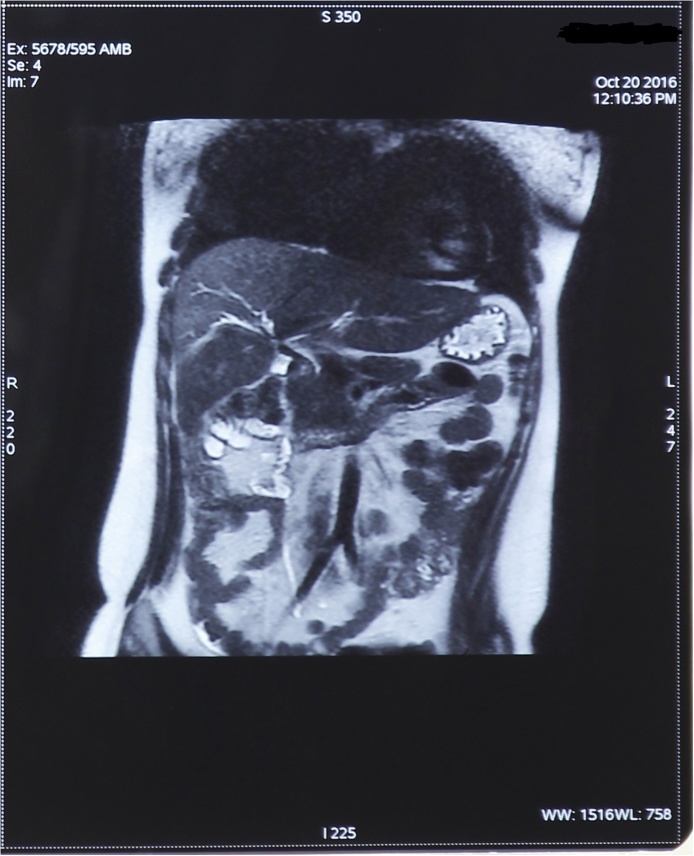
There were no significant postoperative complications. On the first postoperative day, the nasogastric tube (NG) was removed, and the next day we gave a tea to the patient. Over the next few days, patient has been properly set up gastrointestinal functions. The control laboratory tests showed normal reference values. Seven days after surgery we removed abdominal drain. The eighth day after the procedure the patient was discharged from our clinic, with good general and local status and established gastrointestinal functions. We monitored this patient during the next year; the laboratory parameters showed normal reference values, patient had no pain and no gastrointestinal problems. We did magnetic resonance cholangiopancreatography (MRCP) one year after the surgical procedure, which showed the proper width of the intrahepatic bile ducts, with no signs of stenosis of anastomoses (Fig. 3).
Fig. 3.
MRCP one year after surgery procedure.
We did magnetic resonance cholangiopancreatography (MRCP) one year after the surgical procedure, which showed the proper width of the intrahepatic bile ducts, with no signs of stenosis of anastomoses (Fig. 3).
3. Discussion
Since laparoscopic procedures are the standard treatment of symptomatic cholecystolithiasis, these types of injuries are more frequent, so their treatment should be proper in order to prevent for those complications. In most cases, treatment iatrogenic BDI is based on primary repair of the duct, ductal repair with a stent or creating duct-enteric anastomosis, often used and drainage by Witzel (Witzel enterostomy). Reconstructive hepaticojejunostomy is recommended for major BDIs during cholecystectomy [11]. Considering that the biliary reconstruction with Roux-en-Y hepatojejunostomy is usually made with transhepatic biliary stent or Witzel enterostomy [12]. What is interesting about this case is that these types of drainages were not made. We tried and managed to avoid such types of drainage and proved that in this way, without those types of drainage, we can successfully do duplex hepaticojejunal anastomoses and that they can survive without complications. Our anastomoses were functional and without stenosis 1 year after the surgical procedure (anastomoses were made 1 month after hepatic ducts injury was made, when it was recognised). The immediate post-operative recovery was satisfactory, and the patient was discharged 8 days after the third surgery. We monitored this patient during the next year, the laboratory parameters were the reference values, there was no pain and no gastrointestinal problems. The majority of case reports about hepatic duct injuries of high type were written about how to treat and make Roux-en-Y hepaticojejunostomy below the junction of the liver immediately after it is recognised during the operation when the injury happened [13]. We made Roux –en- Y hepaticojejunostomy without transhepatic billiary stent and also without Witzel drainage one month after the lesion was made.
4. Conclusion
In conclusion, hepaticojejunostomy is a safe and reliable method for treatment of benign lesions of the bile ducts even in young patients who are in need of a long-term biliary bypass even without transhepatic biliary stent and Witzel drainage.
Conflicts of interest
All Authors have read and approved the manuscript completely and take full public responsibility for it. The authors have no disclosure or conflict of interest related to this manuscript.
Sources of funding
We do not have any sponsors. This case report did not receive any specific grant from funding agencies in the public commercial, or not-for-profit sectors.
Ethical approval
The study was approved by local ethics committee (Number: 04-09/2-27/18).
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
All authors participated equally in the presentation of the case report. Data collection, data analysis, writing the paper.
Zijah Rifatbegovic drafted the manuscript, performed surgery, and followed-up the patient. Maja Kovacevic and Branka Nikic participated in the surgery and supervised the writing of the manuscript. Maja Kovacevic contributed the data extraction and postoperative management. Branka Nikic and Maja Kovacevic contributed to preoperative assessment. Zijah Rifatbegovic and Maja Kovacevic contributed to the revision of the manuscript. All authors read and approved the final manuscript. Zijah Rifatbegovic gave final approval of this manuscript.
Registration of research studies
researchregistry3977.
Guarantor
Zijah Rifatbegovic.
Contributor Information
Zijah Rifatbegovic, Email: drzooro@gmail.com.
Maja Kovacevic, Email: majaak@hotmail.com.
Branka Nikic, Email: bnbrankanikic@gmail.com.
References
- 1.Laparoscopic cholecystectomy: the new “gold standard”? Arch. Surg. 1992;127(September (8)):917–921. doi: 10.1001/archsurg.1992.01420080051008. discussion 921–923. [DOI] [PubMed] [Google Scholar]
- 2.Parmeggiani D., Cimmino G., Cerbone D., Avenia N., Ruggero R., Gubitosi A. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir. 2010;31(January–February (1–2)):16–19. [PubMed] [Google Scholar]
- 3.Rossi R.L., Schirmer W.J., Braasch J.W., Sanders L.B., Munson J.L. Laparoscopic bile duct injuries. Risk factors, recognition, and repair. Arch. Surg. 1992;127(May (5)):596–601. doi: 10.1001/archsurg.1992.01420050124016. discussion 601–602. [DOI] [PubMed] [Google Scholar]
- 4.Jabłońska Beata, Lampe Paweł. Iatrogenic bile duct injuries: etiology, diagnosis and managment. World J. Gastroenterol. 2009;15(September (33)):4097–4104. doi: 10.3748/wjg.15.4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes R.M., Doctor N.H. Predictors of outcome after reconstructive hepatico- jejunostomy for post cholecystectomy bile ductinjuries. Trop. Gastroenterol. 2015;36(October–December (4)):229–235. doi: 10.7869/tg.296. [DOI] [PubMed] [Google Scholar]
- 6.Sicklick J.K., Camp M.S., Lillemoe K.D., Melton G.B., Yeo C.J., Campbell K.A., Talamini M.A., Pitt H.A., Coleman J., Sauter P.A., Cameron J.L. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy: perioperative results in 200 patients. Ann. Surg. 2005;241:786–795. doi: 10.1097/01.sla.0000161029.27410.71. View ArticlePubMedPubMed CentralGoogle Scholar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rauws E.A., Gouma D.J. Endoscopic and surgical management of bile duct injury after laparoscopic cholecystectomy. Best Pract. Res. Clin. Gastroenterol. 2004;18:829–846. doi: 10.1016/j.bpg.2004.05.003. View ArticlePubMedGoogle Scholar. [DOI] [PubMed] [Google Scholar]
- 8.Ponsky J.L. Complications of laparoscopic cholecystectomy. Am. J. Surg. 1991;161:393–395. doi: 10.1016/0002-9610(91)90605-d. View ArticlePubMedGoogle Scholar. [DOI] [PubMed] [Google Scholar]
- 9.Deziel D.J., Millikan K.W., Economou S.G., Doolas A., Ko S.T., Airan M.C. Complications of laparoscopic cholecystectomy: a national survey of 4,292 hospitals and an analysis of 77,604 cases. Am. J. Surg. 1993;165:9–14. doi: 10.1016/s0002-9610(05)80397-6. View ArticlePubMedGoogle Scholar. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt S.C., Langrehr J.M., Hintze R.E., Neuhaus P. Long-term results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br. J. Surg. 2005;92(1):76–82. doi: 10.1002/bjs.4775. [DOI] [PubMed] [Google Scholar]
- 11.Holte K., Bardram L., Wettergren A., Rasmussen A. Reconstruction of major bile duct injuries after laparoscopic cholecystectomy. Dan. Med. Bull. 2010;57(February (2)) [PubMed] [Google Scholar]
- 12.Lillemoe K.D., Martin S.A., Cameron J.L. Major bile duct injuries during laparoscopic cholecystectomy. Follow-up after combined surgical and radiologic management. Ann. Surg. 1997;225(5):459–471. doi: 10.1097/00000658-199705000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanto D.W., Douglas W. Perspective on biliary surgery. In: Zinner M.J., Ashley S.W., editors. Maingot’s Abdominal Operations. 12th ed. McGraw-Hill Education/Medical; New York: 2012. p. 1089. Chapter 53A. [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., Afifi R. The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]