Abstract
Intrauterine devices (IUDs) are the most common form of contraceptive used worldwide. The imaging features of IUDs and their potential complications are crucial to recognize in order to determine adequate positioning and ultimately function of the IUD. Herein, we report a rare case of a copper IUD embedded in the left fallopian tube that required surgical removal. Only a few such cases have been reported in the literature to date.
Keywords: IUD, Fallopian tube, Copper IUD, Embedment
1. Introduction
Intrauterine devices (IUDs) are a commonly used form of contraception worldwide and have a 98%-99% effectiveness in prevention of pregnancy [1]. IUDs can be divided into 3 basic types: inert, copper containing, and hormone containing [2]. IUDs prevent pregnancy by producing chronic inflammatory changes of the endometrium and fallopian tubes that have spermicidal effects, inhibit fertilization, and create an inhospitable environment for implantation [1], [3], [4]. Ultrasonography is the most common initial method of evaluation of IUDs due to its cost-effectiveness, lack of ionizing radiation, and excellent detail of pelvic anatomy [2]. The correct positioning of an IUD within the uterus is that of a T-shape. The stem and the arms of the “T” should be identified, with the proximal end toward the internal os and the distal end in the fundal region within the endometrium [5]. Malpositioning and/or migration of the IUD from its normal position in the uterine fundus is a frequent complication. Extrauterine migration and embedment in the fallopian tube is an extremely rare complication of IUD placement. Only a few other cases of copper-containing IUD embedment in the fallopian tube have been reported in the literature to date. Herein, we present an additional case, detailing the complications and importance of recognizing translocated IUDs.
2. Case report
A 42-year-old female who was gravida 4, para 3 presented for IUD evaluation. The patient had the copper-containing IUD inserted 1 month prior to presentation and reported no gynecologic symptoms at this time. IUD strings, however, were not identified in physical exam and ultrasound was recommended. The gynecologic exam was otherwise unremarkable. Blood chemistries and physical exam findings were within normal limits. Upon transvaginal ultrasound examination, the IUD was not identified, at which time abdominal radiograph was recommended for further evaluation (Fig. 1). Abdominal radiograph demonstrated the IUD projecting in the pelvic region, thereby confirming that it had not been expelled (Fig. 2). Further evaluation with computed tomography showed the IUD in an extrauterine location posterior to the bladder (Fig. 3). The patient underwent laparoscopic removal of the IUD, which was identified partially embedded in the left fallopian tube. The IUD was noted to be in close proximity to the bladder, but did not perforate it. Of note, the patient had a previous IUD device placed 3 months prior, 1 month postpartum, which was also malpositioned and removed. The patient recovered from the surgery well and opted for an alternative method of contraception.
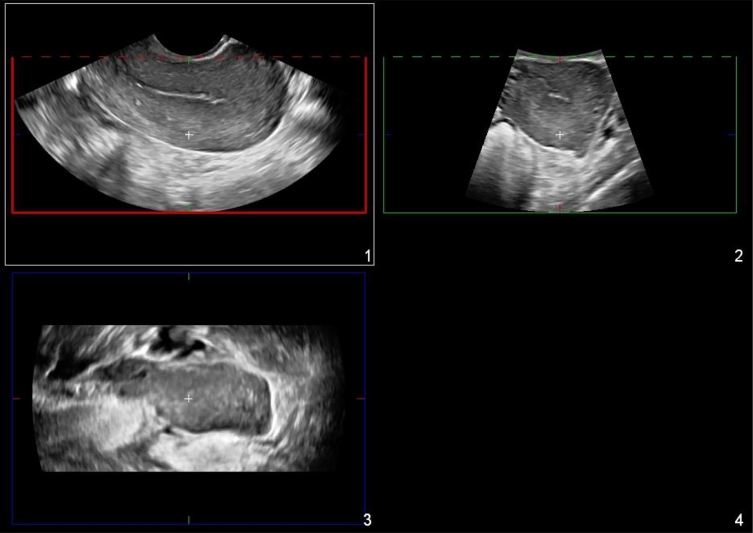
Fig. 1.
Three-dimensional reformatted ultrasound images of uterus without intrauterine device identified. Further evaluation with abdominal radiograph was recommended.
Fig. 2.
Abdominal radiograph shows the intrauterine device projecting over the pelvis, confirming that it had not been expelled.
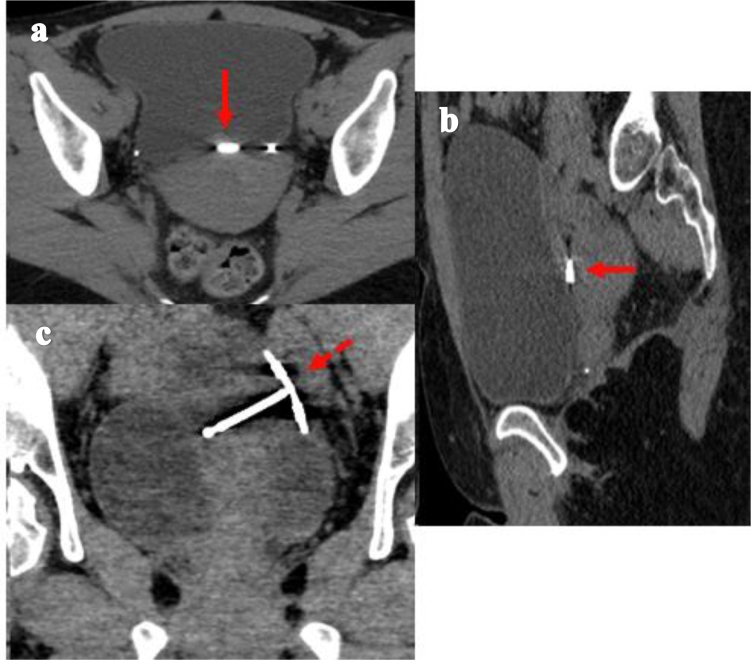
Fig. 3.
Axial (a), sagittal (b), and coronal (c) computed tomography images show the intrauterine device (IUD) within the uterine-vesicular pouch (arrow). The stem of the IUD is oriented horizontally and the arms of the IUD are oriented vertically in the left adnexa (dashed arrow).
3. Discussion
IUDs are an effective, safe, and widely used form of birth control, accounting for 16.5% use in undeveloped countries and 9.4% use in developed countries [1], [6]. The incidence of uterine perforation by IUD is reported to be between 1.3 and 1.6 per 1000 insertions [5]. Uterine perforation is a relatively rare but very serious complication. Perforations of IUD can occur anytime, either immediately by improper insertion or years after insertion secondary to device migration [6]. Serious complications can result secondary to extrauterine migration including perforation and embedment into the adjacent organs. Misplaced IUDs have been presented and described from several organs such as the intestinal tract, including the rectum and appendix, urinary bladder and even buried in the omentum [7], [8], [9], [10], [11]. Recognizing the imaging features of misplaced IUDs is crucial in initiating the appropriate workup to locate the device and remove it if necessary.
The risk of IUD perforation is increased with the placement by inexperienced operators, early IUD placement <6 months postpartum, in women with fewer prior pregnancies and in women with an increased number of miscarriages [1]. During the lactation period, endometrial atrophy due to hypoestrogenic state and accelerated involution of the uterus also leads to increased susceptibility to uterine perforation [7], [12]. In a study by Andersson and colleagues, at least 80% of their patients with perforated IUD were in the lactation period at the time of insertion [12]. Perforation of an IUD typically occurs at the time of insertion or within 1 year [7].
The pathophysiology of IUD migration is not well understood. Specifically, tubal migration of an IUD is very rare and has not been extensively described in the literature. Of the few reported cases in the literature, there is only 1 case of tubal migration involving a copper-containing IUD that resulted in pyosalpinx. This is the only such case reported with IUD embedment in the fallopian tube. In our case, the copper-containing IUD was inserted during the lactation period and only 3 months postpartum. In our patient, IUD translocation occurred twice in a period of 3 months, with both IUDs being inserted <6 months postpartum and during lactation. It has been suggested that tubal migration may result from the penetration of part of the IUD into the tubal ostium at the time of insertion or the device may have been forced to migrate toward the tubal ostium by uterine contractions [13], [14]. Similarly, IUD migration into an adjacent organ may occur through movements of the omentum [7], [15], [16], [17]. The enlarged uterus in unintended pregnancies and tubal ectopic pregnancy may also cause IUD migration [7]. Another theory is 2-step migration where first the IUD perforates the uterine wall, and then at a later time perforates the wall of the fallopian tube [8]. Once the IUD perforates and specifically embeds in the fallopian tube, the accumulation of copper in the fallopian tube can induce morphologic changes and infiltration by inflammatory cells, resulting in hydrosalpinx or pyosalpinx as reported by Özdemir and colleagues [13].
Given that migrant IUDs may remain asymptomatic for many years, the actual frequency is likely underreported. Although some patients have signs and symptoms suggestive of IUD perforation including pelvic pain, bleeding, and/or infection, many patients seem apparently asymptomatic [7]. Extrauterine perforation, however, can result in serious complications including injuries to adjacent structures, including bowel and bladder. Adhesions that form as a result of a foreign body reaction to the perforated IUD can involve the fallopian tubes and result in permanently decreased fertility [2]. In addition, in a hormone-containing IUD, the serum hormone levels can be up to 10 times higher when the IUD is in a peritoneal location than when it is intrauterine [5].
Management of the migrated IUD is a matter of controversy; it can be debated whether the extrauterine IUD in an asymptomatic woman should be removed at all [13]. However, it has been recommended to remove a copper IUD located in the abdominal cavity, even in an asymptomatic patient, because the presence of copper can lead to adhesion formation and subsequent abdominal pain, bowel obstruction, or infertility [7], [13]. The standard treatment of mislocated IUDs is surgical and can be performed either laparoscopically or via laparotomy [7], [10]. The preferred surgical treatment is laparoscopy; however, the treatment depends on the degree of perforation and clinical symptoms. Laparoscopy can pose specific difficulties due to intra-abdominal adhesions, which may result in injury to the bowel [13]. Endoscopic techniques such as colonoscopy, hysteroscopy, and cystoscopy can be used for diagnosis and treatment depending on the location of the IUD [7]. There are several case reports in the literature about removing an IUD in the colonic lumen with colonoscopy [7], [17]. A review of surgical techniques to remove IUD by Akpinar and colleagues revealed that 93% of the reported cases in literature were attempted laparoscopically, but cases of both abdominal and pelvic organ perforations have an open surgery rate of 57.1% [7].
Although rare, missing strings should prompt concern for extrauterine displacement of an IUD, especially if it occurs in early postpartum insertion as presented here. If the IUD cannot be identified on ultrasound, the patient should proceed to abdominal radiographs to ensure that the device has not been expelled. If the device is still not visualized, further evaluation with computed tomography can be performed. Cross-sectional imaging can be useful in identifying the precise location of the IUD within the abdominal cavity, and assists in directing management regarding the optimal method of device retrieval. In our case, the location of the displaced IUD posterior to the bladder required surgical retrieval.
4. Conclusion
Migration of an IUD into the fallopian tube is an extremely rare and not well-understood complication of IUDs. IUD migration may be asymptomatic in some patients and result in complications at any point during their implantation. Imaging plays a critical role in locating a malpositioned IUD, assessing potential complications, and aiding in the surgical planning process.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Boortz H.E., Margolis D.J., Ragavendra N., Patel M.K., Kadell B.M. Migration of intrauterine devices: radiologic findings and implications for patient care. Radiographics. 2012;32(2):335–352. doi: 10.1148/rg.322115068. [DOI] [PubMed] [Google Scholar]
- 2.Nowitzki K.M., Hoimes M.L., Chen B., Zheng L.Z., Kim Y.H. Ultrasonography of intrauterine devices. Ultrasonography. 2015;34(3):183. doi: 10.14366/usg.15010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaislasuo J., Suhonen S., Gissler M., Lähteenmäki P., Heikinheimo O. Uterine perforation caused by intrauterine devices: clinical course and treatment. Human Reprod. 2013;28(6):1546–1551. doi: 10.1093/humrep/det074. [DOI] [PubMed] [Google Scholar]
- 4.Croxatto H.B. Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action. Contraception. 2007;75(6):S16–S30. doi: 10.1016/j.contraception.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Peri N., Graham D., Levine D. Imaging of intrauterine contraceptive devices. J Ultrasound Med. 2007;26(10):1389–1401. doi: 10.7863/jum.2007.26.10.1389. [DOI] [PubMed] [Google Scholar]
- 6.Akpinar F., Ozgur E.N., Yilmaz S., Ustaoglu O. Sigmoid colon migration of an intrauterine device. Case Rep Obstet Gynecol. 2014;2014 doi: 10.1155/2014/207659. Article ID 207659, 3 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benacerraf B.R., Shipp T.D., Bromley B. Three‐dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol. 2009;34(1):110–115. doi: 10.1002/uog.6421. [DOI] [PubMed] [Google Scholar]
- 8.Key T.C., Kreutner A.K. Gastrointestinal complications of modern intrauterine devices. Obstet Gynecol. 1980;55(2):239–244. [PubMed] [Google Scholar]
- 9.Demirci D., Ekmekçioğlu O., Demirtaş A., Gülmez İ. Big bladder stones around an intravesical migrated intrauterine device. Int Urol Nephrol. 2003;35(4):495–496. doi: 10.1023/b:urol.0000025624.15799.8d. [DOI] [PubMed] [Google Scholar]
- 10.Kriplani A., Garg P., Sharma M., Agarwal N. Laparoscopic removal of extrauterine IUCD using fluoroscopy guidance: a case report. J Gynecol Surg. 2005;21(1):29–30. [Google Scholar]
- 11.Ohana E., Sheiner E., Leron E., Mazor M. Appendix perforation by an intrauterine contraceptive device. Eur J Obstet Gynecol Reprod Biol. 2000;88(2):129–131. doi: 10.1016/s0301-2115(99)00142-6. [DOI] [PubMed] [Google Scholar]
- 12.Andersson K., Ryde-Blomqvist E., Lindell K., Odlind V., Milsom I. Perforations with intrauterine devices: report from a Swedish survey. Contraception. 1998;57(4):251–255. doi: 10.1016/s0010-7824(98)00029-8. [DOI] [PubMed] [Google Scholar]
- 13.Özdemir S., Özdemir S., Cihangir N., Görkemli H., Emlik D. Pyosalpinx caused by the tubal migration of an intrauterine device—a case report. Eur J Contracept Reprod Health Care. 2008;13(3):320–322. doi: 10.1080/13625180802254563. [DOI] [PubMed] [Google Scholar]
- 14.Zakin D., Stern W.Z., Rosenblatt R. Complete and partial uterine perforation and embedding following insertion of intrauterine deives: I. Classification, complications, mechanism, incidence, and missing string. Obstet Gynecol Surv. 1981;36(7):335. doi: 10.1097/00006254-198107000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Johri V., Vyas K.C. Misplaced intrauterine contraceptive devices: common errors; uncommon complications. J Clin Diagn Res. 2013;7(5):905. doi: 10.7860/JCDR/2013/5287.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaplanoğlu M., Bülbül M., Yüce T., Kaplanoğlu D., Aban M. Mislocated extrauterine intrauterine devices: diagnosis and surgical management. J Turk Ger Gynecol Assoc. 2015;16(2):91. doi: 10.5152/jtgga.2015.15243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Medina T.M., Hill D.A., DeJesus S., Hoover F. IUD removal with colonoscopy: a case report. J Reprod Med. 2005;50(7):547–549. [PubMed] [Google Scholar]