Abstract
Methods of treating obesity in selected cases include endoscopically performed procedures, among them endoscopically placed intragastric balloons. It is a method associated with a low complication rate, traditionally reserved to treat the most obese patients. Balloon rupture or deflation and its migration into the small bowel is one of the possible complications. In some cases, the balloon moves through the digestive tract without side effects. When the balloon’s displacement in the intestine is impossible, gastrointestinal obstruction occurs. We report a case of a patient with a mechanical obstruction of the gastrointestinal tract caused by asymptomatic balloon rupture and its migration into the jejunum.
Keywords: obesity, small bowel obstruction, intra-gastric balloon
Introduction
Obesity is a major health problem on a global scale, and its prevalence is on the rise. The Polish WOBASZ II study demonstrated the prevalence of obesity in males to have increased from 20.0% to 24.2% and in females from 22.3% to 23.4% of the population over the period from 2003 to 2014 [1]. Obesity is estimated to be responsible for 5% to 20% of deaths yearly in the USA and 10% to 13% in Europe [2, 3]. Among various approaches to treating obesity, endoscopic methods are used in selected cases, including endoscopically placed intragastric balloons (IGBs). The IGB therapy is used as a bridge to definitive treatment, to facilitate weight loss and optimal patient management prior to bariatric surgery [4, 5]. Also, it is used to treat extremely obese patients with multiple comorbidities. It is a safe and well-tolerated method, associated with a low complication rate [6]. Below, we report a case of a patient with a mechanical intestinal obstruction after the implantation of an intragastric balloon prior to the scheduled surgical therapy.
Case report
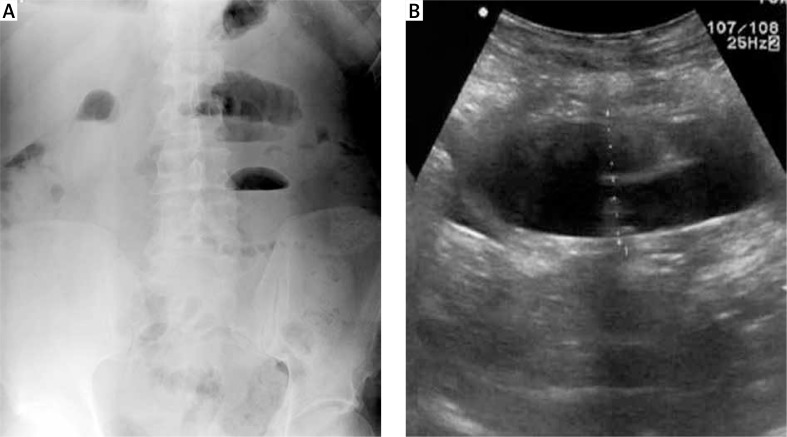
A 59-year-old male patient was admitted into our department, 6 months after endoscopic placement of an intragastric balloon, due to symptoms of intestinal obstruction. The patient reported abdominal pain, abdominal distention and vomiting. He had not passed feces or flatus for 3 days. Physical examination showed dehydration, distended abdomen, tender epigastrium, and high-pitched tinkling bowel sounds. Abdominal ultrasound and radiography performed in a standing position demonstrated intestinal obstruction (Photo 1 A). The ultrasonography (USG) scan also showed the presence of a structure in the intestinal lumen, possibly consistent with a migrated intragastric balloon (Photo 1 B). Endoscopic examination of the upper gastrointestinal tract showed that the balloon was missing from the stomach, thus confirming its migration.
Photo 1.
A – Radiogram of the abdominal cavity taken in a standing position – intestinal obstruction with visible fluid levels. B – Abdominal ultrasound – visible enlarged intestinal loops with the balloon impacted within the lumen
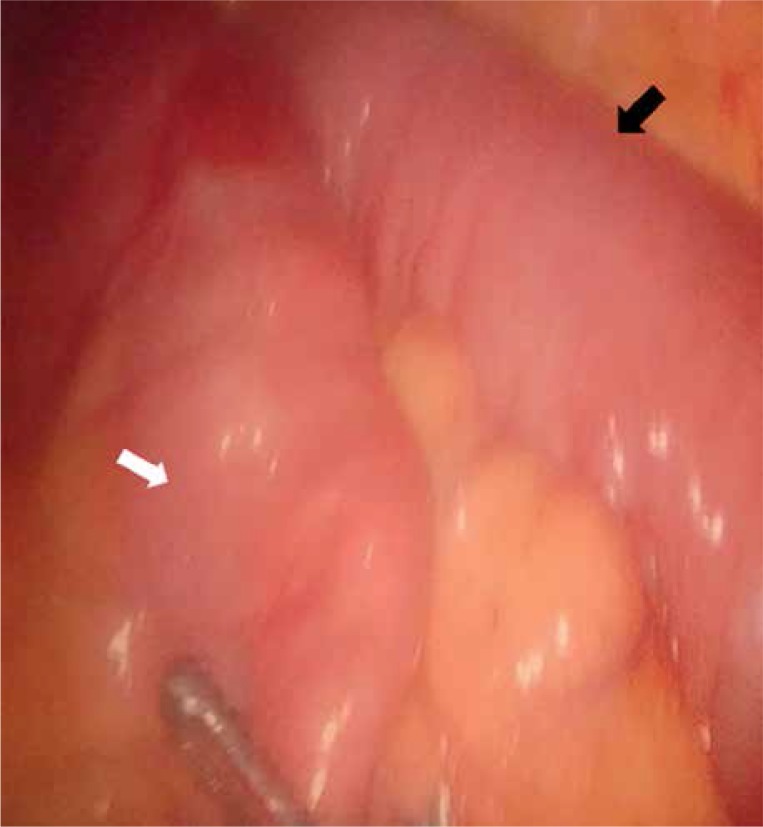
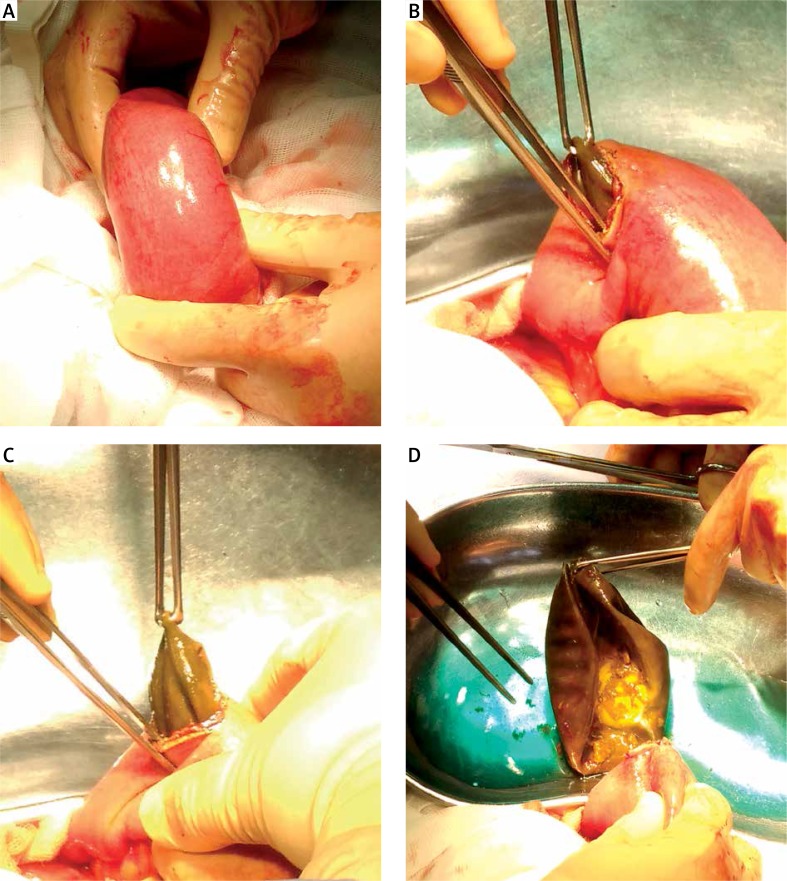
The patient noticed no blue color when urinating, a symptom that would have served as an alert that the balloon had deflated or ruptured (the balloon had been filled with methylene blue solution). He did not report any other adverse symptoms prior to the occurrence of the abdominal discomfort and pain. Exploratory laparoscopy was performed. Jejunal distention approximately 50 cm below the ligament of Treitz (Photo 2) was found, and the migrated balloon was identified. The balloon was retrieved on median minilaparotomy (Photo 3). No complications were observed in the postoperative period. The patient was discharged on day 5 after surgery, in general good condition.
Photo 2.
Enlarged intestinal loop with the impacted balloon – black arrow, collapsed intestine beneath the obstruction – white arrow
Photo 3.
Laparotomy – successive stages of balloon retrieval. A – Enlarged and rigid intestinal loop, B – incision of the intestinal wall showed the impacted migrated balloon, C – balloon retrieval, D – examination of the retrieved balloon showed remnant methylene blue solution
Discussion
Endoscopically placed intragastric balloons have been used to treat obesity for 30 years now [7]. The indications for the therapy include body mass index (BMI) > 27 kg/m2 and inadequate weight loss associated with lifestyle modifications, medication and behavioral therapy [8]. In our department, the IGB is also used to treat patients who have contraindications for surgical treatment. It is frequently utilized prior to surgery as a bridge therapy, to achieve a better therapeutic effect [4, 9–11]. Optimal therapy outcomes are typically achieved in patients with BMI of 30 mg/kg2 to 40 mg/kg2 [12, 13].
An IGB is implanted using endoscopy for 6 months, and then endoscopically retrieved. In the case of nausea, vomiting or other symptoms suggesting intolerance, balloon deflation or rupture, emergency endoscopy is performed, and the balloon is retrieved immediately. In such cases, where endoscopic or conservative treatment proves ineffective, laparoscopy or laparotomy is necessary [14].
Balloon migration within the lumen of the gastrointestinal (GI) tract should be considered as the possible cause in the case of every IGB patient showing clinical symptoms of intestinal obstruction.
The reported complications of IGBs most commonly include esophagitis, necrosis and gastric ulcers. Balloon rupture and its migration into the small intestine, potentially causing bowel obstruction, is another possible complication [12, 15]. Intestinal obstruction, however, is considered a very rare IGB occurrence. In a study conducted on a group of 4240 patients, obstruction caused by the migration of a deflated balloon was found in only 7 (0.17%) cases [12]. An early symptom of balloon rupture or deflation is typically blue-colored urine, due to the absorption of methylene blue injected into the balloon immediately on implantation [16]. In the case we are reporting, the patient did not notice any changes in the color of urine, hence the delayed diagnosis of balloon rupture, facilitated only when the symptoms of a mechanical intestinal obstruction were already present.
Contraindications for IGB include a history of bariatric or gastric surgery, large hiatal hernia, inflammatory conditions of the GI tract, increased risk for bleeding from the upper GI tract, pregnancy, untreated psychiatric conditions and alcohol or drug dependency [8, 17].
Conclusions
Migration of the balloon to the distal part of the gastrointestinal tract should be considered in patients with clinical signs of gastrointestinal obstruction after gastric balloon implantation.
An urgent endoscopic examination of the upper gastrointestinal tract allows one to see if there is a missing balloon from the stomach, which confirms its migration.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Stepaniak U, Micek A, Waskiewicz A, et al. Prevalence of general and abdominal obesity and overweight among adults in Poland. Results of the WOBASZ II study (2013-2014) and comparison with the WOBASZ study (2003-2005) Pol Arch Med Wewn. 2016;126:662–71. doi: 10.20452/pamw.3499. [DOI] [PubMed] [Google Scholar]
- 2.Masters RK, Reither EN, Powers DA, et al. The impact of obesity on US mortality levels: the importance of age and cohort factors in population estimates. Am J Public Health. 2013;103:1895–901. doi: 10.2105/AJPH.2013.301379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO WHO. http://www.euro.who.int/en/health-topics/noncommunicable-diseases/obesity/obesity.
- 4.Genco A, Lorenzo M, Baglio G, et al. Does the intragastric balloon have a predictive role in subsequent LAP-BAND((R)) surgery? Italian multicenter study results at 5-year follow-up. Surg Obes Relat Dis. 2014;10:474–8. doi: 10.1016/j.soard.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 5.Buzga M, Kupka T, Siroky M, et al. Short-term outcomes of the new intragastric balloon End-Ball® for treatment of obesity. Videosurgery Miniinv. 2016;11:229–35. doi: 10.5114/wiitm.2016.63988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitura K, Garnysz K. Tolerance of intragastric balloon and patient’s satisfaction in obesity treatment. Videosurgery Miniinv. 2015;10:445–9. doi: 10.5114/wiitm.2015.54047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nieben OG, Harboe H. Intragastric balloon as an artificial bezoar for treatment of obesity. Lancet. 1982;1:198–9. doi: 10.1016/s0140-6736(82)90762-0. [DOI] [PubMed] [Google Scholar]
- 8.Laing P, Pham T, Taylor LJ, et al. Filling the void: a review of intragastric balloons for obesity. Dig Dis Sci. 2017;62:1399–408. doi: 10.1007/s10620-017-4566-2. [DOI] [PubMed] [Google Scholar]
- 9.Saruc M, Boler D, Karaarslan M, et al. Intragastric balloon treatment of obesity must be combined with bariatric surgery: a pilot study in Turkey. Turk J Gastroenterol. 2010;21:333–7. doi: 10.4318/tjg.2010.0117. [DOI] [PubMed] [Google Scholar]
- 10.Leeman MF, Ward C, Duxbury M, et al. The intra-gastric balloon for pre-operative weight loss in bariatric surgery: is it worthwhile? Obes Surg. 2013;23:1262–5. doi: 10.1007/s11695-013-0896-0. [DOI] [PubMed] [Google Scholar]
- 11.Zerrweck C, Maunoury V, Caiazzo R, et al. Preoperative weight loss with intragastric balloon decreases the risk of significant adverse outcomes of laparoscopic gastric bypass in super-super obese patients. Obes Surg. 2012;22:777–82. doi: 10.1007/s11695-011-0571-2. [DOI] [PubMed] [Google Scholar]
- 12.Dumonceau JM. Evidence-based review of the Bioenterics intragastric balloon for weight loss. Obes Surg. 2008;18:1611–7. doi: 10.1007/s11695-008-9593-9. [DOI] [PubMed] [Google Scholar]
- 13.Alfredo G, Roberta M, Massimiliano C, et al. Long-term multiple intragastric balloon treatment: a new strategy to treat morbid obese patients refusing surgery: prospective 6-year follow-up study. Surg Obes Relat Dis. 2014;10:307–11. doi: 10.1016/j.soard.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Vanden Eynden F, Urbain P. Small intestine gastric balloon impaction treated by laparoscopic surgery. Obes Surg. 2001;11:646–8. doi: 10.1381/09608920160556913. [DOI] [PubMed] [Google Scholar]
- 15.Zdichavsky M, Beckert S, Kueper M, et al. Mechanical ileus induces surgical intervention due to gastric balloon: a case report and review of the literature. Obes Surg. 2010;20:1743–6. doi: 10.1007/s11695-010-0114-2. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Nava G, Bautista-Castano I, Jimenez-Banos A, et al. Dual intragastric balloon: single ambulatory center Spanish experience with 60 patients in endoscopic weight loss management. Obes Surg. 2015;25:2263–7. doi: 10.1007/s11695-015-1715-6. [DOI] [PubMed] [Google Scholar]
- 17.Ozturk A, Akinci OF, Kurt M. Small intestinal obstruction due to self-deflated free intragastric balloon. Surg Obes Relat Dis. 2010;6:569–71. doi: 10.1016/j.soard.2009.11.013. [DOI] [PubMed] [Google Scholar]