Recent years have shown exponential growth in interest in 3D printing techniques in the field of medicine. One of the last specialties to adopt this novelty is cardiology, owing to the complexity of the cardiovascular system. Over the last year our team has gained a great deal of experience by adopting 3D printed heart models in daily clinical practice in all its fields – student education, patient counselling and pre-procedural planning and simulation [1]. We present an exemplary case of such 3D printed model application.
Melody valve implantation is considered one of the most complex procedures in structural interventions. We were challenged with a case of a 34-year-old man born with tetralogy of Fallot (TOF) palliated with B-T shunt at the age of 3 and 6 years, and treated with a homograft at the age of 8 years. Due to homograft stenosis, the patient underwent balloon angioplasty twice – at the ages of 18 and 33. In the most recent cardiac catheterization the right ventricular systolic pressure (RVSP) was 85 mm Hg with a trans-homograft pressure gradient of 64 mm Hg, and due to the recoil the balloon angioplasty did not provide a lasting effect; thus the patient was qualified for Melody valve implantation.
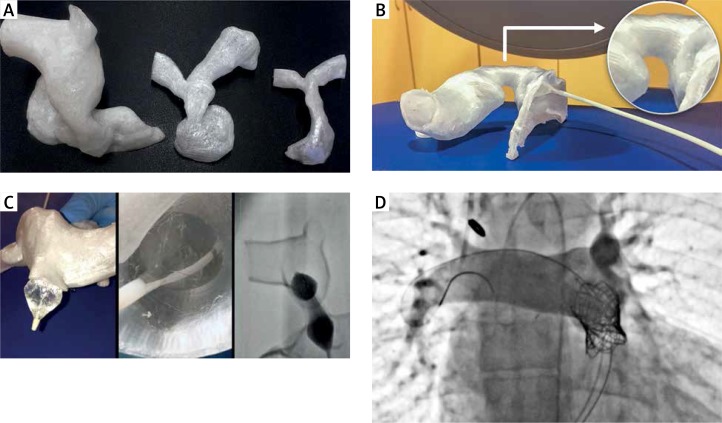
The complexity and the variability of homograft anatomy of post-TOF patients (Figure 1 A) makes every Melody valve implantation procedure a distinct challenge [2]. For that reason, we prepared a 3D model of the region of interest encompassing the right ventricular outflow tract (RVOT), homograft and pulmonary branches. The imaging modality was MRI 1.5T, contrast enhanced TWIST sequence on 1.9 mm slice thickness. For post-processing we used commonly available software including Osirix, Meshmixer, Meshlab and a printer dedicated Z-suite slicer to prepare the print. The model was printed with the fused deposition modelling (FDM) technique using Zortax desktop 3D printer available at our department. The image analysis and post-processing took 3 h, printing time was 7 h. Next the model was taken to the cath-lab for simulation (Figures 1 B–C) to better plan the procedure and shorten the total procedure time, fluoroscopy time and failure rate similarly to the experience of others [3].
Figure 1.
A – Variability of RVOT – homograft – pulmonary branches region illustrated by three 3D printed models of (from left to right) 34-year-old, 12-year-old and 8-year-old subjects, top-down presentation. B – Model of the treated patient in the cath-lab, right lateral presentation best showing the narrowing of the homograft. C – Procedure simulation using the model – outside, inside and fluoroscopy view. D – Image documenting excellent procedure outcome: proper placement of the Melody valve and no regurgitation
The Melody valve implantation on a patient, preceded by double pre-stenting using 20 atm pressure, was carried out uneventfully on the next day (Figure 1 D). The procedure outcome was assessed to be excellent with good device position and stability, no stent fractures, negligible gradient, and no pulmonary valve incompetence. In the opinion of the interventionist the model precisely reflected the complex anatomy, helping to choose the landing zone, but lacked the elastic properties of the real tissue.
The issue of elasticity could have been addressed by outsourcing the printing of the model to use other techniques, but the material would need to be carefully chosen as some, although elastic, have a low breaking point, thus ruling out their use in simulating dilatation of significant vascular stenosis. Additionally, the higher costs and longer processing time would need to be taken into account.
We conclude that with the advances in software and printing techniques, the 3D printed heart models are a useful addition to daily practice. They may become rapidly available if an in-house facility is established and personnel are trained. The currently available technique has shortcomings, such as reliably reproducing tissue elasticity, that need to be addressed by future research.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Luo H, Meyer-Szary J, Wang Z, Sabiniewicz R, Liu Y. Three-dimensional printing in cardiology: current applications and future challenges. Cardiol J. 2017;24:436–44. doi: 10.5603/CJ.a2017.0056. [DOI] [PubMed] [Google Scholar]
- 2.Schievano S, Migliavacca F, Coats L, et al. Percutaneous pulmonary valve implantation based on rapid prototyping of right ventricular out ow tract and pulmonary trunk from MR data. Radiology. 2007;242:490–7. doi: 10.1148/radiol.2422051994. [DOI] [PubMed] [Google Scholar]
- 3.Biglino G, Capelli C, Taylor AM, Schievano S. 3D Printing Cardiovascular Anatomy: A Single-Centre Experience. 2016. [cited 2017 Nov 14]; Available from: http://www.intechopen.com/books/new-trends-in-3d-printing/3d-printing-cardiovascular-anatomy-a-single-centre-experience.