Abstract
Patients with a history of drug abuse and right sided endocarditis are prone to develop septic pulmonary emboli. Pneumothorax is a rare complication of septic pulmonary emboli reported in the literature, likely due to the rupture of thin-walled septic cavitary lesions resembling pneumatoceles into the pleural space. Only seven cases (including our case) of pneumothorax from septic pulmonary emboli due to right sided endocarditis have been described in the literature. Our patient is the first reported case of recurrent bilateral pneumothorax due to septic pulmonary emboli and tricuspid valve endocarditis.
Keywords: Septic pulmonary embolism, endocarditis, pneumothorax
Introduction
Pneumothorax (PTX) has been described as a rare complication of septic pulmonary emboli (SPE), most commonly seen in intravenous drug abusers with right sided endocarditis.1–6 PTX should be strongly and emergently considered as an etiology of sudden onset dyspnea or chest pain in a patient with SPE. To the best of our knowledge, this is the first case of recurrent bilateral PTX described in the literature as a complication from septic emboli to lungs from tricuspid valve endocarditis.
Case presentation
A 33-year-old cachectic female with past medical history of untreated hepatitis C infection and intravenous drug abuse (IVDA) was admitted for higher level of care from an outside hospital with acute respiratory failure requiring mechanical ventilation, methicillin sensitive Staphylococcus aureus (MSSA) bacteremia, and tricuspid valve (TV) endocarditis complicated by development on 10th day of spontaneous right sided PTX with chest tube placement. Vital signs on admission revealed a temperature of 100.9 F, pulse of 113/min, respiratory rate of 18/min, blood pressure of 109/65 mmHg, and pulse oximetry of 100% on FiO2 of 40%. Physical examination was consistent with coarse breath sounds bilaterally in anterior lung fields and presence of 3/6 systolic murmur best heard in the right lower sternal border. Her chest tube was in place with resolution of PTX. Labs on admission showed hemoglobin of 8.2 gm/dL, white blood cell count of 10,000/mL, platelet count of 52,000/mm3, BUN of 21 mg/dL, creatinine of 0.48 mg/dL, sodium of 138 mEq/L, potassium of 3.6 mEq/L, and normal coagulation parameters. She had persistent MSSA bacteremia on multiple blood cultures even with aggressive antibiotic treatment. Her pleural fluid cultures did not isolate any organism. Initial transthoracic echocardiography (TTE) demonstrated a large, mobile, prolapsing 3.5 × 1.5 cm2 vegetation on the anterior leaflet of TV with moderate tricuspid regurgitation. Computed tomography (CT) chest showed bilateral septic emboli to lungs and cavitary lesions, small bilateral pleural effusions, and bibasilar infiltrates. She was placed on empiric antibiotics and cardiothoracic surgery (CTS) was consulted for valve replacement surgery. Her intensive care unit (ICU) course was complicated by septic shock, acute renal failure, and urinary tract infection (UTI). Subsequently, she developed sudden onset respiratory distress and was found to have a new right sided PTX. A second chest tube was placed on the right to evacuate the PTX. CTS deemed that patient was not a suitable candidate for valve surgery due to continued IVDA and very poor nutritional status. During the course of her ICU stay, she kept developing recurrent noniatrogenic pneumothoraces, bilaterally requiring the placement of a total of three chest tubes on the right and two on the left for decompression. Figures 1–5 show the chest X-ray (CXR) findings,while Figure 6 shows the CT findings. The family decided to pursue comfort care measures due to her grim prognosis and she died post terminal extubation. Autopsy was not performed as the family refused to give consent.
Figure 1.
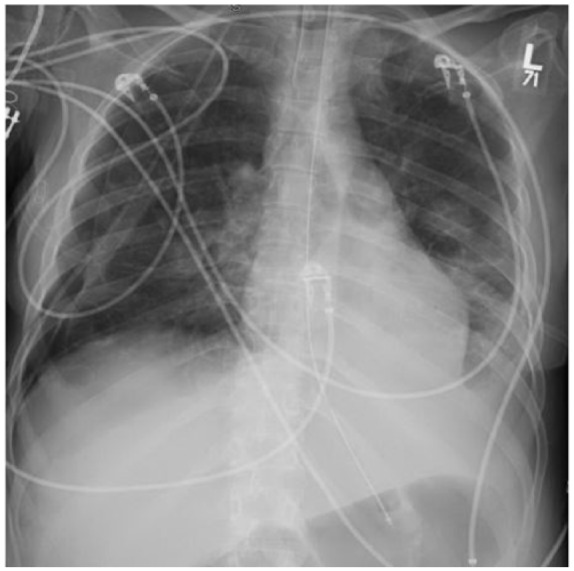
CXR showing right sided chest tube and resolution of pneumothorax.
Figure 2.
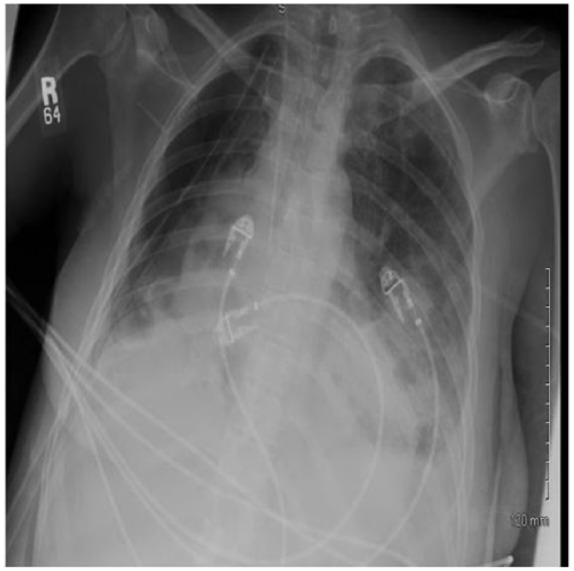
CXR with new right spontaneous PTX.
Figure 3.

CXR showing second right chest tube (pig tail) in place for decompression of PTX.
Figure 4.

CXR showing new left PTX.
Figure 5.
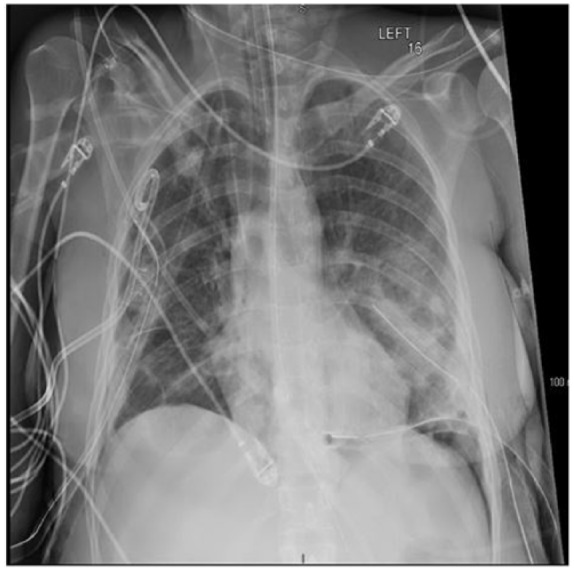
CXR showing three chest tubes on the right and two on the left.
Figure 6.
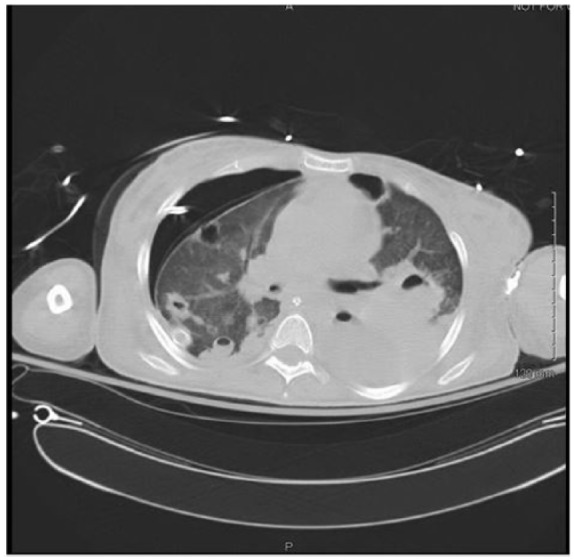
CT findings.
Discussion
Illicit drug use has emerged as a common worldwide health problem, affecting about 5% of the world’s adult population and accounting for 0.5%–1.3% of all causes of mortality in 15–64-year-old adults.7 Patients addicted to illicit drugs are susceptible to develop a multitude of infectious and noninfectious pulmonary complications like aspiration pneumonia, pulmonary edema ( cardiogenic and noncardiogenic), pulmonary infections, hemorrhage, fibrosis, hypersensitivity pneumonitis, PTX, and so on.5 Etiology for PTX in intravenous drug users include jugular or subclavian vein in correct self-injection causing pleural trauma, pneumocystis jirovecci pneumonia, military tuberculosis, interstitial, and bullous lung diseases and SPE.1 The common causes of SPE include IVDA, right sided infective endocarditis (IE; TV and pulmonic valve), septic thrombophlebitis, suppurative angina, periodontal abscess, purulent infections of skin and soft tissue, infected intravascular catheters, pacemakers, and pelvic thrombophlebitis.6 In a systemic review by Ye et al.,6 26% patients with SPE had a history of drug abuse, 12.5% had intravascular indwelling catheters, and 12% had IE. SPE can cause lung consolidation mimicking bronchopneumonia, thin-walled cavitary lesions simulating pneumatoceles, necrotic lung infarcts, lung abscess, bronchopleural fistula, empyema, pleural effusion, fatal pulmonary hemorrhage, and infrequently PTX.6
PTX due to SPE from right sided endocarditis was first described in the literature by Aguado et al.1 in 1990, where a patient with h/o iv heroin abuse and MSSA TV endocarditis developed bilateral PTX requiring bilateral tube thoracostomy. PTX or hydro PTX is usually caused by rupture/progression of subpleural septic cavitary lesions, abscess, or empyema into the pleural cavity.
So far, seven cases (including our case) have been reported in the literature where patients with right sided endocarditis developed spontaneous PTX from SPE, three of them bilateral.1–4,8 Table 1 lists all the reported cases. All except one had a history of IVDA. The median age of presentation is 25 years ( range 19–78 years). Most of the reported cases are males (six out of seven) with sudden onset shortness of breath being the most common symptom. The PTX usually developed between days 1 and 15 with the median being 6 days. Our patient developed recurrent bilateral PTX, first episode on day 10. Of all the cases of IE, Staphylococcus aureus was the most common bacteria isolated in blood cultures with five out of seven cases growing MSSA. Five out of seven cases survived and no information was available for one patient. Our patient expired in the ICU. Two patients underwent valve replacement. All patients reported in the literature were treated with chest tube drainage. The poor outcome in our patient can be explained by multiple factors including large sized vegetation, persistent bacteremia, recurrent pneumothoraces, and inability to undergo surgery. Persistent bacteremia and positive pressure ventilation predisposed her to develop recurrent pneumothoraces. Our case is unique in several ways compared to previous cases. It is the first reported case in females due to drug abuse and IE; the patient developed recurrent bilateral hydro pneumothoraces (five times total) and was associated with poor outcomes (death).
Table 1.
Case reports of septic pulmonary emboli leading to spontaneous pneumothorax (PTX).
| Study/year | Age/sex of patient | Drug abuse/HIV/Hep status | Type of endocarditis | Survival | Complications | Pulmonary manifestations | Day when developed PTX |
|---|---|---|---|---|---|---|---|
| Aguado et al.,1 1990 | 19/male | Heroin (+), HIV (−), Hep B (−) | MSSA tricuspid valve endocarditis | Yes | Cardio respiratory arrest due to tension PTX | Bilateral PTX, b/l patchy infiltrates with cavitation, b/l pleural effusions | 6th Day |
| Corzo et al.,2 1992 Case 1 |
23/male | Heroin(+), HIV(+), Hep B(+) | MSSA tricuspid valve endocarditis | Yes | None | Bilateral hydropneumothoraces, small, multiple bilateral patchy infiltrates | 15th day |
| Corzo et al.,2 1992 Case 2 |
26/male | Heroin(+), HIV(+), Hep B(+) | Staphylococcus epidermidi tricuspid valve endocarditis | Yes | None | Right hydropneumothorax | 1st day |
| Sheu et al.,3 2006 | 23/male | Heroin(+), Hep C(+), HIV(−) | MSSA tricuspid valve endocarditis | Yes | Acute renal failure, septic shock, tricuspid valve replacement | Left PTX, bilateral nodular infiltrates, thin walled cavities | 7th day |
| Yang et al.,8 2012 | 78/male | None, source is infected hemodialysis catheter | MRSA tricuspid valve endocarditis | Not known | None | Left PTX, subpleural cavities, multiple nodular infiltrates | 3rd day |
| Swaminath et al.,4 2013 | 25/male | Positive, not specified | MSSA pulmonic valve endocarditis | Yes | Acute respiratory failure, septic shock, pulmonic valve replacement, coagulopathy | Left sided PTX, multifocal bilateral cavitary infiltrates | 1st day |
Conclusion
Spontaneous PTX is a rare but serious complication seen in patients with SPE and right sided endocarditis. Intensivists should have a strong suspicion for it in patients with right sided endocarditis presenting with sudden onset dyspnea or hemodynamic instability.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the deceased patient’s legally authorized representative (next of kin) for patient information (case report and image files) to be published in the journal.
ORCID iD: Sumit Kapoor  https://orcid.org/0000-0002-5683-3445
https://orcid.org/0000-0002-5683-3445
References
- 1. Aguado JM, Arjona R, Ugarte P. Septic pulmonary emboli. A rare cause of bilateral pneumothorax in drug abusers. Chest 1990; 98(5): 1302–1304. [DOI] [PubMed] [Google Scholar]
- 2. Corzo JE, Lozano de, León F, Gómez-Mateos J, et al. Pneumothorax secondary to septic pulmonary emboli in tricuspid endocarditis. Thorax 1992; 47(12): 1080–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sheu CC, Hwang JJ, Tsai JR, et al. Spontaneous pneumothorax as a complication of septic pulmonary embolism in an intravenous drug user: a case report. Kaohsiung J Med Sci 2006; 22(2): 89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Swaminath D, Yaqub Y, Narayanan R, et al. Isolated pulmonary valve endocarditis complicated with septic emboli to the lung causing pneumothorax, pneumonia, and sepsis in an intravenous drug abuser. J Investig Med High Impact Case Rep 2013; 1(4): 2324709613514566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wolff AJ, O’Donnell AE. Pulmonary effects of illicit drug use. Clin Chest Med 2004; 25(1): 203–216. [DOI] [PubMed] [Google Scholar]
- 6. Ye R, Zhao L, Wang C, et al. Clinical characteristics of septic pulmonary embolism in adults: a systematic review. Respir Med 2014; 108(1): 1–8. [DOI] [PubMed] [Google Scholar]
- 7. United Nations Office on Drugs and Crime. World drug report 2012, https://www.unodc.org
- 8. Yang SF, Yang WC, Lin CC. Infective endocarditis-related bilateral spontaneous pneumothorax in a haemodialysis patient. Acta Clin Belg 2012; 67(1): 51. [DOI] [PubMed] [Google Scholar]


