Abstract
Background
Using twice-yearly campaigns such as Child Health Days to deliver vitamin A supplements has been a key strategy over the last 2 decades, and was an important component in helping reach the Millennium Development Goals in child health. As countries move to strengthen their routine health services under the Sustainable Development Goals, efforts are underway to shift supplementation from campaign to routine delivery.
Objective
The aim of this study was to compare cost, coverage, and user satisfaction between twice-yearly campaigns and routine delivery of vitamin A supplements in Senegal.
Methods
Information was collected on cost, coverage, and user satisfaction with both types of delivery, using administrative data, interviews at various levels in the health system, and focus group discussions with caregivers. Both qualitative and quantitative information were obtained, for 2 regions using routine delivery and 2 regions using campaign delivery.
Results
Routine delivery receives fewer dedicated resources. Coverage is lower, especially of children >12 mo of age. Districts undertake outreach (“mini-campaigns”) to try to improve coverage in regions using routine delivery, in effect using a hybrid approach. Some mothers prefer the administration of supplements at a health facility as it is perceived as more hygienic and involving professional health workers, but others, especially those living further away, prefer house-to-house delivery which was the norm for the campaign mode.
Conclusions
Advance planning for the shift to routine delivery is important in maintaining coverage, as is strengthening the primary health care system by having an appropriate ratio of salaried workers to population. When the system relies heavily on volunteers, and the small incentive payments to volunteers are discontinued, coverage suffers. Routine delivery also relies on good record-keeping and hence literacy. Community understanding of, and support for, supplementation are even more important for routine than for campaign delivery.
Keywords: cost, coverage, health systems, nutrition, child health, community mobilization, vitamin A supplements, Child Health Days
Introduction
Deficiency of vitamin A in diets in low- and middle-income countries remains widespread, and is known to increase child morbidity and mortality due to infectious diseases such as diarrhea, pneumonia, and measles. Using high-dose supplementation in children aged 6–59 mo has been shown to reduce mortality and morbidity (1, 2) and has led to a WHO guideline that children aged 6–59 mo should receive supplements every 4–6 mo (3).
Given the limitations in coverage of primary health care systems in many countries, delivery of vitamin A supplements has frequently been one component of mass campaigns such as ChildHealth Days, which deliver a package of services such as deworming, immunization, and nutritional screening. Child Health Days in sub-Saharan Africa have been shown to be both modest in cost per child and cost-effective (4, 5). At the same time, the reliance on external aid for budgeting and limited national capacity for micro-planning and implementation mean that the long-term goal is to phase out campaign-style distribution and shift to using routine health services (6).
A few countries are now piloting this transition for vitamin A supplementation. Senegal and Ethiopia for example have ≥3 y of experience of transition for selected geographic areas. Tanzania has adopted a different strategy by transitioning from a national program to one with more local responsibility and funding, and with greater decentralization of health services.
There is considerable interest in the cost and coverage of service delivery through alternative platforms, as well as the implications for equity and maintenance of coverage of the most vulnerable groups. Previous economic studies have examined, for example, the transition from outreach to clinic-based services for family planning in urban Bangladesh (7), and grouping several previously vertical interventions against HIV, diarrhea, and malaria in Kenya (8). To date there have been no published evaluations of the shift of delivery of vitamin A supplements that we could identify, and this paper fills that gap.
The objective of this study was to compare cost, coverage, and user perceptions of distribution of vitamin A using 2 modalities, namely campaign and routine, to inform those countries considering switching modality. Although the original intention had been to compare the cost-effectiveness of the 2 modalities, early in the fieldwork it became obvious that this was not feasible without considerably more time and resources than were available. The study went ahead with the narrower scope, and may provide useful information for a future cost-effectiveness study.
In Senegal, large-scale supplementation with vitamin A has occurred since 1999 as part of an essential child survival package, run as a government program with support from partners such as Helen Keller International, UNICEF, United States Agency for International Development (USAID), and Nutrition International. Initially, supplementation was included with the polio vaccination campaign, which evolved to become Supplementation Days (Journées Locales de Supplémentation) and, since 2013, twice-yearly Child Survival Days [Journées de Survie de l'Enfant (JSE)] (9). Through the JSE campaign, a package of interventions is offered 2 times/y, including deworming, growth monitoring, screening and referral for severe malnutrition, screening and treatment for diarrhea, catch-up for vaccination, and civil registration for children aged <5 y. Coverage of these interventions has been high: national coverage of vitamin A supplements in the December 2015 campaign in 9 regions was 98% (10). Coverage in July–December 2015 in the 5 regions using routine delivery was 54% (11). But the financial and human resource cost of maintaining the campaigns is somewhat burdensome and leadership has been mainly provided by external partners.
Starting in 2013, the government moved to integrate vitamin A supplementation into the routine health services. This was piloted in 1 of the 14 regions of the country, again with partner support over the transition period, and 3 more regions were added in 2014 and 1 in 2015. The transition occurred first in the more densely populated regions, including those in which the 3 largest cities, Dakar, Thiès, and Saint Louis, are situated. The transition has been slowest in the least densely populated, arid regions in the east of the country. The present evaluation occurred in August–September 2016 at a time when 3 additional regions were transitioning to using routine health services instead of mass campaigns.
The health services in Senegal are organized through 14 regions, with each region further subdivided into health districts. Each district has ≥1 health center, which is often the district hospital. The chief medical officer at the district level supervises the work in the various health posts within the district, each of which is headed by a head nurse who is usually male. The head nurse in turn supervises the activities of the health huts which serve the local communities. The work of the salaried staff at the level of hospitals, health centers, and health posts is supported by volunteer community health workers (agents de santé communautaires, or ASCs) and community mobilizers (relais). The ASCs provide all health services at the health huts, supported by the relais. A separate cadre of personnel provides assistance with deliveries at hospitals, health centers, health posts, and health huts.
The organization of supplementation is obviously different in the 2 service modalities. In the campaign modality, the Division of Food, Nutrition and Child Survival in the Ministry of Health oversees the program and supervises the regional teams. The regional teams in turn supervise the teams at the district level, who train and supervise the nurses who direct the health posts. The health posts in turn organize and train the fieldwork teams comprised of ASCs who implement campaign activities throughout the district over a period of ∼4 d once every 6 mo, delivering the package of services to households. The package includes vitamin A supplements, which are administered to children between the ages of 6 and 59 mo. Although service delivery is primarily through unpaid community workers, the salaried health staff train and supervise the volunteers and maintain records. There are also per diems for staff and small incentive payments to the volunteers, as well as costs of necessary materials, transport, and social mobilization and communication. The costs of campaigns, originally borne by partner organizations, have proven difficult for the government to take over.
Delivery of supplements occurs through many points of contact when delivered through routine health services. When children visit the health hut or the health post for routine immunizations, monthly growth monitoring, quarterly screening for malnutrition, or for treatment of illnesses, they may also receive vitamin A supplements as part of a package of preventive services. This is supposed to be noted in the registers as well as on the child's immunization card which is held by the mother. Various methods are used to reach those children who do not visit health facilities within a specific 6-mo period. These methods include mobilizing the community to attend the health hut or an outreach site and, in some localities, undertaking house-to-house visits targeting those children who were missed, in “mini-campaigns”. Experience in Ethiopia, which is undergoing a similar transition in method of distribution of vitamin A, suggests that hybrid methods are likely more important in localities where the population is more dispersed, and for older children who on the one hand are too heavy for the mother to carry, but who on the other hand are still too young to walk a long distance to the health hut. The initial experience in Ethiopia was that coverage levels for vitamin A supplementation dropped with the transition in service, particularly for older children (12). Partner agencies have provided transitional support to Senegal for additional supervision by salaried health workers, in an effort to maintain coverage.
Data on coverage for the JSE campaigns are collected in the field, registering the number of children supplemented by age, but not child names. These data are collected at the health posts and forwarded on and collated at the district, regional, and national levels. The biannual campaigns are supposed to occur in June and December, and coverage is calculated as the number supplemented divided by the number of eligible children, i.e., those in the relevant age groups. Coverage data for campaigns can exceed 100%, because the same child is supplemented twice, because of temporary migration, or because children outside the eligible age range are supplemented.
Data on coverage of supplementation through routine services are also maintained, including the name of the child. Data are reported by “semester”, i.e., January–June and July–December, to correspond to the campaign coverage in other regions.
Methods
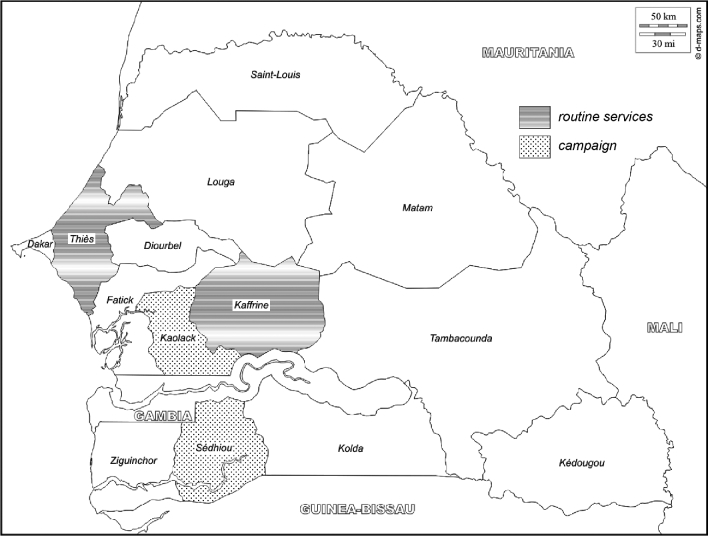
Quantitative data were collected in 4 of the 14 regions of the country, 2 closer to Dakar with higher population density, Thiès and Kaolack, and 2 a little further away with lower population density, Kaffrine and Sédhiou (see map in Figure 1), for the period 1 July 2015 to 30 June 2016. Qualitative data were collected in 2 regions, Thiès and Kaolack. Thiès and Kaffrine use routine delivery and achieved coverage rates of 90% and 44%, respectively, in July–December 2015. Kaffrine had switched to routine delivery in 2013, and Thiès in 2014. Kaolack and Sédhiou use campaign delivery and achieved coverage rates of 113% and 30% respectively in the December 2015 campaign (10, 11). Choice of the survey regions was undertaken in conjunction with the Ministry of Health with the aim of providing as broad a range of experience as possible within the budget and timeline constraints of the research funding partner. Fieldwork was undertaken by 4 teams each of 2 individuals: 2 quantitative teams and 2 qualitative. In addition, there was 1 supervisor of the quantitative and 1 of the qualitative fieldwork. The fieldwork was conducted over a 2-wk period in August–September 2016. Fieldwork in the regions was supplemented with 7 interviews of key informants involved in the vitamin A program at the national level, either in government or in an international partner. These interviews took place later in September 2016.
FIGURE 1.
Map of Senegal showing regions surveyed, by mode of distribution of vitamin A supplements (as of December 2015). Source: authors’ adaptation using an outline available freely from http://d-maps.com/carte.php?num_car=4915&lang=en.
Research ethics approval was obtained from the Centre National d'Ethiques pour la Recherche en Santé, of the Division of Research Planning and Statistics of the Ministry of Health and Social Action, Senegal, file number SEN 16/42, and all those interviewed gave free and informed written consent. Only adults were interviewed.
Quantitative methods
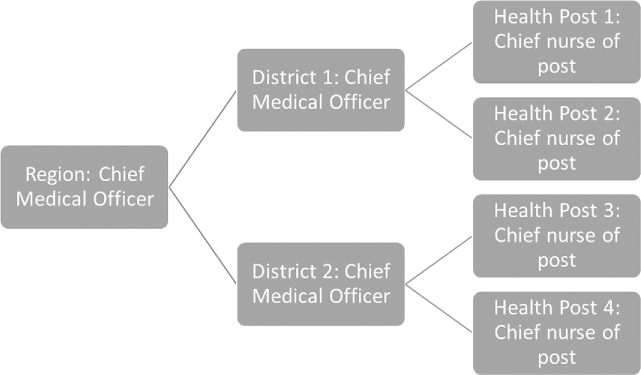
A total of 44 quantitative interviews were undertaken, covering 4 regions. Within each region, 1 higher-coverage and 1 more average-coverage district were identified, and within each district 1 higher-coverage and 1 more average-coverage health post, and 1 health hut associated with each health post (Figure 2). Higher-coverage was defined as being within the upper tertile of the distribution of coverage within the region or district, and average-coverage as within the middle tertile. The choice of specific districts and health posts took into account logistical considerations and advice from knowledgeable local informants. Interviews were undertaken in person by a team of 2 interviewers, with the exception that the Chief Medical Officers of the Region were sent an email questionnaire. Responses were received from all 44 targeted individuals or their designates.
FIGURE 2.
Quantitative interviews undertaken in each of 4 regions. When the designated individual was not available for interview, his/her deputy was interviewed if available.
The quantitative questionnaire was developed drawing on experience from a previous study in Ethiopia (12) but considerably adapted for the Senegalese context. The adaptations were made during a 3-d workshop involving 5 of the 7 authors. The main aim of the quantitative questionnaires was to estimate costs, using a bottom-up “ingredients” approach. This required collecting information on financial expenditures from those who held this information, as well as estimating the time requirements for personnel involved in vitamin A supplementation, either directly or as supervisors or administrators. Information was also collected on coverage at the local level to supplement information available nationally, to obtain both more recent and more disaggregated information than is available nationally.
Questionnaires were customized by the respondent's role within the health system, and by routine or campaign modality, such that in all there were 8 variants of the questionnaire. Each questionnaire consisted of 6 sections: identification of the facility and role of the respondent; the context, namely population served by the facility and staff complement; information about personnel involved in distribution of vitamin A and the training they received; financial resources dedicated to vitamin A distribution; supervision; and coverage attained. Original questionnaires along with the quantitative fieldwork report are available (in French) from the corresponding author.
Fieldwork staff were experienced individuals selected by the lead quantitative author, either with a university degree in a relevant discipline such as sociology, or with training in health, for example as a nurse or midwife. One day of training was provided which incorporated pretesting and any necessary refinement of the instruments. The supervisor accompanied the teams in the field and verified the data quality daily such that there was immediate follow-up of any errors and omissions. Data for the quantitative interviews were recorded using tablets, using the software CSPro (Census and Survey Processing System: https://www.census.gov/data/software/cspro.html), and analyzed using Microsoft Excel (Redmond, WA).
Qualitative methods
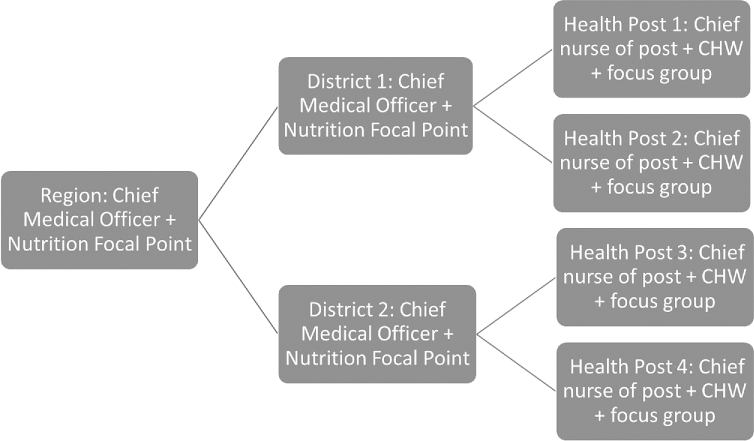
A total of 27 qualitative interviews were undertaken in Thiès and Kaolack, 2 of the same 4 regions, covering the regional health headquarters, 2 districts/region, and 2 health posts/district (Figure 3). One chief medical officer at the regional level was not available, so 27 interviews were undertaken in total rather than the intended 28. Ten individuals were interviewed on separate occasions by each of the quantitative and qualitative teams. These individuals were the Chief Medical Officer of 2 of the regions, the Chief Medical Officer of 4 of the districts, and the Chief Nurse of 4 of the health posts. In addition to the interviews at regional and district level, 7 national-level qualitative interviews were undertaken by the lead qualitative researcher with individuals working in government, nongovernment organizations, and 1 United Nations agency supporting vitamin A supplementation.
FIGURE 3.
Qualitative interviews undertaken in each of 2 regions. When the designated individual was not available for interview, his/her deputy was interviewed if available. CHW, community health worker.
Eight focus groups of child caregivers were also conducted, 2 in each of the 4 districts studied in the qualitative research. One focus group in each district was conducted close to a health post, and the other near to a health hut about 7 km away from a health post. Each focus group consisted of mothers and grandmothers of children <5 y of age who were communicative and respected community members, identified in conjunction with knowledgeable local informants. The focus groups had between 8 and 12 participants, and discussions lasted ≤90 min.
The qualitative instruments were developed locally based on the research objectives, and elaborated at the same 3-d workshop involving the authors. Topics explored in interviews included description of implementation of the campaign or routine approach and the respondent's role in vitamin A supplementation, perceptions of the advantages and disadvantages of the delivery modality being used locally, perceived obstacles to switching from campaign to routine delivery, and specific ways in which delivery might be improved.
Topics explored in focus groups included knowledge about vitamin A, experience with supplementation, perceptions concerning the local delivery modality, the preferred approach, and recommendations on how to strengthen local vitamin A activities. Focus groups were used for caregivers since this was expected to make them feel more comfortable in responding, whereas health workers were interviewed individually in order to cause less disruption in the work environment, and with the expectation that health workers are more familiar than are caregivers with one-on-one interviews.
The 4 field research staff had relevant degrees and previous experience in undertaking qualitative studies. They spent 3 d in training and in pretesting and fine-tuning the instruments. Interviews of health sector workers occurred in a private space at the work site where interruptions would not occur. Focus groups took place in a neutral place in the community where interruptions would not occur.
The qualitative interviews and focus group discussions were digitally recorded with the permission of the participants. Interviews were conducted in French or Wolof, depending on the preference of the respondent, whereas focus groups were carried out in Wolof. Audio recordings were transcribed and, if needed, translated into French. The qualitative instruments (in French) and the report on the qualitative fieldwork are available from the corresponding author.
Qualitative analysis was undertaken by the lead qualitative researcher, LSB, using well-accepted methodological principles (13). Transcripts were coded using ATLAS.ti software (http://www.atlasti.com) and reviewed to develop different coding systems for campaign and routine delivery, and for health personnel interviews and focus groups of caregivers. Content analysis was used to identify trends of concepts in and across individual codes. The combination of data and methodologic and environmental triangulation allowed the analysis of data across different research methods, namely in-depth interviews and focus group discussions, and across and between respondents living in different research sites.
In the course of the fieldwork it was discovered that 1 of the regions, Kaolack, which had been using campaign delivery up to the end of 2015, was in the process of transitioning to routine services for distribution of vitamin A. Accordingly for Kaolack, data on vitamin A implementation activities and financing were collected only for July–December 2015, and data for January–June 2016 were excluded, whereas for the other regions both periods were covered.
Financial data are recorded in thousands of 2016 Francs of the Financial Community of Africa [Francs Communauté Financière d'Afrique (FCFA)]. As of October 2016, 1 US$ was worth ∼584 FCFA (14). Financial data were provided by knowledgeable individuals at each level with access to financial records. Imputation of economic costs for health personnel, volunteers, and vehicles was undertaken based on information on quantities from the quantitative survey, and unit costs at national level based on information from a single knowledgeable informant; these are summarized in Table 1. Volunteers’ time was valued at the very modest rate received from specific projects or from their community.
TABLE 1.
Unit cost estimates of health system resources, used for cost calculations1
| Resource | Cost per day,2 FCFA |
|---|---|
| Health personnel, region level | 34 |
| Chief Medical Officer of district | 34 |
| Chief Nurse, health post | 8.2 |
| Agent de Santé Communautaire | 0.45 |
| Relais (during campaigns only) | 3 |
| Car (including fuel) | 30 |
| Motorcycle (including fuel) | 10 |
| Cart | 5 |
Assumes people work 22 d/mo. Source: KN. FCFA, Franc of the Financial Community of Africa (Franc Communauté Financière d'Afrique).
In thousands.
There are additional in-kind costs at national level for the campaigns, since these involve a substantial time commitment by government personnel and personnel in international partner agencies. These costs were too difficult to ascertain, and likely are relatively modest on a per-child basis. We also do not include the procurement costs of supplies, which are also relatively modest compared to the other costs. A study for Somalia (15) found that vitamin A capsules and deworming tablets added ∼0.05 US$/child in Somalia, in 2009 prices.
Results
Coverage
The campaign modality has been generally successful in maintaining a high level of coverage. The average coverage of children 6–59 mo across the 9 regions delivering vitamin A supplements through the campaigns in December 2015 was 98%, with very little difference between the age groups of 6–11 mo of age and 12–59 mo of age (10). Seven of the 9 regions using campaign delivery achieved coverage ranging from 99–113%, although coverage in the remaining 2 regions in the southwest of the country was lower at 77% and 30%, respectively. The 2 regions selected for our survey, Kaolack and Sédhiou, had the highest and lowest coverage, respectively, of all 9 campaign regions in December 2015.
National data on coverage of children aged 6–59 mo through the routine delivery system for July–December 2015 present a somewhat concerning picture (11). Coverage of children aged 6–59 mo was on average only 54% in the 5 regions using routine delivery compared to the average of 98% achieved in the campaign regions. The difference was particularly large for children aged 12–59 mo, namely 36% for routine compared to 98% for campaign, but also significant for children aged 6–11 mo, namely 79% for routine compared to 100% for campaign. Although 1 region, Thiès, undertaking routine delivery close to the capital, reported achieving 90% coverage of children aged 6–59 mo, the other 4 regions achieved coverage only in the 40–50% range. Coverage in Kaffrine, which was also included in our survey, was 44%.
The transition between delivery modes impacts coverage. Kaolack was using campaign delivery for the period July–December 2015, and achieved 113% coverage of children aged 6–59 mo. Coverage levels were identical at 113% for children aged 6–11 mo and children aged 12–59 mo. In the next 6-mo period, January–June 2016, as the switch to routine delivery began, coverage dropped to 33% for children aged 6–59 mo. The drop was to 87% for children aged 6–11 mo, and to 26% for children aged 12–59 mo (16). It is expected that coverage will improve as familiarity with the new system improves. There is also considerable variation across districts and health posts (Table 2) for both delivery modalities.
TABLE 2.
Coverage of children aged 6–59 mo with vitamin A, July–December 2015, by region and modality1
| Region | Coverage, % | District | Coverage, % | Health posts | Coverage, % |
|---|---|---|---|---|---|
| Delivery modality: Campaign (JSE) | |||||
| Kaolack | 113 | Nioro | 116 | Post #1 | 136 |
| Post #2 | 97 | ||||
| Guinguineo | 110 | Post #1 | 140 | ||
| Post #2 | 102 | ||||
| Sédhiou | 30 | Bounkiling | 34 | Post #1 | 158 |
| Post #2 | 90 | ||||
| Sédhiou | 29 | Post #1 | 123 | ||
| Post #2 | 97 | ||||
| Delivery modality: Routine | |||||
| Thiès | 90 | Khombole | 38 | Post #1 | 53 |
| Post #2 | 37 | ||||
| Joal | 247 | Post #1 | 94 | ||
| Post #2 | 36 | ||||
| Kaffrine | 44 | Kaffrine | 59 | Post #1 | 53 |
| Post #2 | 33 | ||||
| Birkelane | 32 | Post #1 | 42 | ||
| Post #2 | 38 | ||||
Source: Quantitative survey responses, based on health unit records. JSE, Journées de Survie de l'Enfant (Child Survival Days).
Comments from the qualitative data helped to illuminate some of the reasons for the changes observed in coverage. Caregivers of children liked some aspects of the shift to routine delivery. One mother commented:
“With this new system our children are supplemented appropriately, hygienically and the work is done by qualified and professional people. During campaigns, supplementation was not done professionally.”
But other mothers pointed out some disadvantages to routine delivery:
“The campaign is the best approach because when we go to the health hut there are often a lot of people and we can get impatient and return home and try to come back another day.”
“They went door to door for distribution during the campaign. This suits us because we have work to do at home and it is not always easy for us to travel outside the household.”
One of the national-level interviewees commented about another advantage of campaign delivery:
“For the JSE, what is important is the fact that we have an intervention package. This is an added value of JSE. We attempt to touch those living farthest away, because the JSE reaches everybody. It promotes equity.”
Budget and implementation
The shift from campaign to routine coverage was accompanied by a significant difference in the budget available per district for vitamin A distribution (Table 3). The median in the previous 6 mo was just over 5,000,000 FCFA or 8707 US$/district in campaign regions, compared to just over 200,000 FCFA or 342 US$/district in routine regions. The drop at the level of the region was of a similar order of magnitude. Although it was anticipated that local health committees might step in to partially offset the drop in partner funding, only 1 of the 4 districts concerned reported receiving local funds.
TABLE 3.
Comparison between campaign and routine delivery activities, at district and health post levels1
| Activity | Campaign (4 study districts) | Routine (4 study districts) |
|---|---|---|
| Date of last training | Within last 6 mo | 2016 (1) and 2013 (other 3) |
| Training budget/district,2 FCFA | 978 (range: 418–7295) | Not specified |
| Median number of days of training/district | 1 (nutrition for JSE) | 2 (but not only on nutrition) |
| Method used for distribution (8 health posts reported) | House to house only (7); house to | House to house only (3); house to |
| house + fixed point (1) | house + fixed point (3); no outreach (2) | |
| Number of days to verify data at district level | 5 (range: 1–15) | 11 (range: 1–18) |
| Budget for vitamin A distribution during previous campaign or previous 6 mo of routine services,2 district FCFA | 5085 (range: 4426–5568) | 213 (range: 0–600) |
Data are medians (and ranges) for 4 districts using each modality, except where stated otherwise. Source: quantitative survey: information from Chief Nurse at health post and Chief Medical Officer at district level. FCFA, Franc of the Financial Community of Africa (Franc Communauté Financière d'Afrique); JSE, Journées de Survie de l'Enfant (Child Survival Days).
In thousands.
The budget decrease was also reflected, among other ways, in less frequent training on vitamin A in the routine system. In campaign districts, it is standard to have 1-d refresher training on the components of JSE every 6 mo; in routine districts, training on vitamin A is meant to be one component of overall training. Three of the 4 routine districts mentioned that the last training on vitamin A had been 3 y previously (Table 3); this was also confirmed by the Chief Medical Officers at the region level.
Similarly, the JSE campaigns are accompanied by specific communications efforts to increase awareness just before each campaign begins, whereas routine delivery does not have such communication or social mobilization activities. One person working in the health sector noted:
“….some mothers do not bring their children for vaccinations, and also children older than 1 year and who have completed their vaccinations are lost from view. Despite awareness-raising activities, some mothers do not understand the importance of vitamin A…. Due to the lack of understanding about the importance of vitamin A, and also because the population was used to the campaign approach involving supplementation in each household compound, mothers don't understand the routine approach and think vitamin A capsules are only given during campaigns.”
Others pointed out that routine delivery imposes a heavy burden on health systems with very limited data and information capabilities. An interviewee at the national level commented:
“Efforts are needed to improve the quality of work at the community level, especially regarding recording and transmission of data.”
Interviewees noted that the existing child immunization and health cards do not have enough space to record vitamin A supplementation ≤5 y of age. Keeping records in separate registers in health huts and health posts as well as field notes creates issues of possible double-counting, whereby the same child is counted twice in coverage statistics, whereas on the other hand some children may be supplemented too frequently.
Costs
Some further understanding can be obtained by analyzing the cost per child covered with vitamin A using campaign delivery (Table 4). Although it was originally intended to analyze the cost per child covered using routine delivery as well in order to compare the cost-effectiveness of the 2 approaches, the time and scope of this study made this impractical. Many modalities to deliver services to children are involved in the routine system, for example the health post and health hut, house-to-house visits, and outreach sites. Each modality is employed with varying frequency depending on need, and in most cases vitamin A supplementation occurs jointly with other services. Similarly, training and supervision for vitamin A delivery occurs jointly with training and supervision for other health interventions. One-time retrospective questionnaires of personnel were not adequate to track the time devoted specifically to vitamin A.
TABLE 4.
Estimated cost of most recent JSE campaign per 1000 children1
| Activity | Cost at level of region | Cost at level of district | Cost at level of health post/hut | Total (all levels) |
|---|---|---|---|---|
| Time of qualified personnel (preparation for JSE, supervision during JSE, verification of data) | 168.9 | 20.2 | 48.9 | 238.0 |
| Time of volunteers (Agents de Santé Communautaires) | 0 | 0* | 15.3 | 15.3 |
| Training (per diems etc.; excludes salary of trainees) | 0 | 19.5 | 39.1 | 58.6 |
| Supervision (per diems etc. for travel to supervise) | 120.0 | 13.0 | 24.7 | 157.7 |
| Motivation (bonuses mainly to volunteer personnel) | Combined with supervision cost | 126.4 | 66.7 | 193.1 |
| Transport | 6.0 | 20.4 | 21.5 | 47.9 |
| Communication | 5.0 | 0 | 0 | 5.0 |
| Other | 13.0 | 0 | 0 | 13.0 |
| Subtotal, government (in kind: personnel time, vehicle use) | 174.9 | 40.6 | 85.7 | 301.2 |
| Subtotal, partner (in cash) | 138.0 | 158.9 | 130.5 | 427.4 |
| Total | 312.9 | 199.5 | 216.2 | 728.5 |
Costs are in thousands (FCFA). Community volunteers may contribute also at district level, but their contribution in the field is greatest. Excludes cost of vitamin A capsules, deworming tablets, and other supplies. Excludes costs incurred at national level for meetings to organize campaigns and to monitor progress. Source: Quantitative interviews with Chief Medical Officers of regions and districts, and Chief Nurses at health posts; these individuals have access to the unit financial records. For unit costs see Table 1. FCFA, Franc of the Financial Community of Africa (Franc Communauté Financière d'Afrique); JSE, Journées de Survie de l'Enfant (Child Survival Days).
An examination of the costs of the campaign delivery is, however, instructive. We estimated the cost at each of the region, district, and health post or health hut levels by aggregating information from our interviews on the allocation of partner budgets, as well as the government in-kind contribution in terms of personnel and provision of vehicles.
Partner contributions accounted for 58.7% of campaign costs (Table 4). These were primarily for supervision, namely per diems for supervisors to travel to the field to supervise during the campaign, and small incentive payments (motivations) for the nonsalaried staff. Costs for social mobilization and transport were very small.
The in-kind contribution of the government amounted to 41.3% of the budget, consisting of time of the supervisors who are salaried staff, time of the community health volunteers, and use of government vehicles. Time of salaried staff was required to plan and organize the campaign, undertake the training, supervise the work in the field, and verify and report the data. Community health workers undertake the large majority of the actual distribution in the field, and volunteers mobilize the community.
Table 4 shows that the cost of a JSE campaign per child covered in Senegal is 728.6 FCFA, i.e., 1.25 US$, excluding supplies of vitamin A capsules and deworming tablets. The largest share of costs, 42.9%, is incurred at the regional level, with 27.4% at the district level and 29.7% at the level of the health post or health hut. Personnel time accounts for the major share of the budget: 34.5% of the total is for imputed costs of people's time, with in addition 48.1% for per diems for supervision and incentive payments; 8.0% is for training; and the balance is for transport, communications, and other unspecified uses.
It is not surprising that almost half of the campaign costs are in payments for supervision and motivation, in view of the very heavy workload on the frontline salaried health workers. In Senegal, there is about 1 health post/10,000 population, which should have 2 salaried, qualified health personnel. In practice, more remote areas may find it difficult to maintain this staff complement. In our sample of 16 health posts, the average health post served a population of 9714 (range 3500–25,098), employed 2.1 qualified personnel (range 1–4), oversaw the work of 2.6 health huts (range 1–6), and operated 2.6 outreach sites attached to the health post (range 0–8), and the head nurse at the post supervised on average 16.2 community volunteers, some at the health post but the majority elsewhere (range 6–32).
All types of respondents interviewed during the qualitative data collection made reference to the demanding workload for community health workers and volunteers. A mother who lived far from a health post commented about house-to-house delivery:
“The relais went door to door while walking. I can imagine that it was hard to walk under the sun going to all households in the villages. Most often they were well received in concessions. People were open and even offered them water to drink. But they could also meet people with difficult characters who gave them a hard time.”
And this was echoed by many of the relais working in a region which had made the switch to routine delivery, one of whom said:
“The number of personnel is insufficient; we are only 2 community actors for 3 villages. Imagine the workload and we get nothing at the end of the month…. It is important to look at compensation for relais, it is a big responsibility which many people are not willing to carry out. The relais must go long distances to supplement children without any remuneration. This discourages us from working, with remuneration we will be more effective.”
Discussion
Campaign delivery of vitamin A supplements as part of a package of services has been relatively inexpensive and cost-effective in Senegal. The cost estimates for the Child Health Day package delivered during the JSE campaign, at ∼1.25 US$/child excluding the cost of supplies, are similar to estimates for other African countries after taking account of inflation (4, 5, 17). Some previous studies present lower cost estimates than this as they consider the program to be incremental and do not impute salary costs for health workers (15, 18). Previous studies have estimated that vitamin A distribution accounts for ∼25% of the overall cost of the Child Health Day (5). There have not been other studies of the cost of vitamin A distribution when integrated into routine services. There is some evidence from other countries, however, on the coverage outcomes of the shift between campaign and routine distribution. Senegal, Tanzania, and Ethiopia have followed somewhat different paths in the evolution of their vitamin A supplementation programs.
Ethiopia developed a well–laid out plan, published in 2010 for a transition that began in 2014 (19), based on a very measured strategy for investing in the health system. Ethiopia aims to have 1 health post/5000 population, i.e., twice the ratio of health posts and salaried health workers that Senegal has. Ethiopia deliberately integrated outreach work into the workload of the Health Extension Workers, who receive a modest salary, and eliminated per diems and incentive payments. Ethiopia also aimed to recruit 1 health volunteer worker/25–30 households, and stated that the volunteers should not receive incentive payments. Ethiopia also clearly laid out different transition paths for different areas, such as pastoralist, agrarian, and urban, and identified criteria according to which communities would transition first to Community Health Days and then to routine delivery (9). One of the national interviewees succinctly pointed out the problems in Senegal, by comparison:
“I am concerned that routinization, as do other services, suffers from structural problems that are inherent in our health services.”
Tanzania, on the other hand, has experienced some of the same difficulties as Senegal. Tanzania adopted a policy of decentralization of health spending to district level (20), which can give greater local control, but also can create some difficulties in coordination of national programs. Most recently there have been supply interruptions of vitamin A capsules in some regions, which has led to unplanned gaps in distribution of capsules and the cancellation of expected campaign rounds. The result has been that in some regions, coverage of vitamin A distribution has slipped considerably, leading to potential increases in the prevalence of deficiency in children aged 6–59 mo (21).
Uganda also provides an interesting comparison, although the data are from operation of the campaign modality and not from a switch to routine services. Due to budget constraints, Uganda's Child Days Plus campaigns were consistently underfunded. The actual cost was 0.22 US$/child in 2010, but a study estimated that the full cost should have been 0.35 US$/child (4). The same study further estimated that two-thirds of the missing funding led to the work not being done, i.e., to lower coverage. The other third resulted in individuals doing the work they were supposed to, but not receiving the full value of allowances, such as per diems, to which they were entitled. The bulk of the underfunding occurred at the health facility level, i.e., on the frontline. Twenty-two percent of the underfunding was reflected in lower community outreach activities such as posters, community meetings, and public address systems, whereas 65% was reflected in limitations in operating facilities and outreach, i.e., providing fewer personnel and allowances to cover the outreach sites and travel. The end result was that coverage with vitamin A was only 58% (4), lower than in many other countries in the region (22). Although the program as operated was cost-effective, it could potentially have been equally cost-effective but saved more child lives if operating closer to planned funding levels and achieving higher coverage.
This has similarities to the case of Senegal. It is not surprising that coverage of vitamin A supplementation slipped when per diems for outreach for the head nurse were removed with the shift to routine, along with the motivation payments for the volunteers. Financial incentives can of course be replaced by nonfinancial ones, such as increased importance being placed upon the vitamin A supplementation in the performance assessments of health facilities. The community can also exert pressure, if households recognize the value of vitamin A supplementation, but both of these mechanisms require effort.
Vitamin A supplementation serves as an example of some of the issues arising in the transition from the Millennium Development Goals to the Sustainable Development Goals. Vitamin A supplementation was one of a series of vertical programs, based on scientific evidence, whose output was readily measurable, which became widely implemented 20 y ago during the Millennium Development Goal era. By 2012 supplementation had expanded to 70 countries and covered 70% of the eligible population in those countries (23). Three of the 4 African countries discussed here, namely Senegal, Uganda, and Tanzania, began mandatory fortification of cooking oil within the last decade. Fortification is one approach to greater sustainability for reducing vitamin A deficiency, although it does not immediately eliminate the need for supplementation, and does not necessarily reach poor and remote households. Although transitioning from vertical programs to routine health services is now on the agenda of many countries, our study points out some of the potential difficulties involved.
Our study has several limitations, including the geographically limited sample size, the exclusion of details of personnel costs incurred at national level, the methodology for imputing salary costs, and the reliance on self-reported financial and activity data for the costing. In lieu of more detailed data on the type of personnel involved in each activity at each administrative level, we used average salary data which may not be completely accurate. Service costs undoubtedly vary by district due to differences in population density among other factors; however, we had to assume that costs per child are similar across districts within the same region. We were not able to cost out vitamin A distribution using routine health services. We anticipate that it would be extremely difficult to do this, due to the joint delivery with other services. The choice of survey districts, health posts, and health huts was not random.
There are other factors that may affect coverage of campaign and routine services that we were not able to explore with our facility-based survey. Households located further from health facilities, which are poorer and where adults are less educated and live in locations where transport is less readily available, are likely to face reduced coverage with the shift to routine services. These tendencies are not easy to analyze from facility records, especially because in campaign distribution no child names are collected, only numbers of children. This question would be better addressed using household surveys.
In summary, it has proven difficult to maintain coverage when shifting from campaign to routine delivery of vitamin A supplements in Senegal. Vertical campaigns were used in the first place because of factors which have not completely disappeared, namely limited capacity to operate complex systems in a decentralized manner, dispersed and migratory populations, limitations on communications infrastructure, and relatively low levels of health worker literacy. Campaigns do not tend to strengthen the health system, and may even do the opposite, by disrupting routine activities and tasks and temporarily pulling out resources. It is therefore not surprising that the initial response to the shift to routine delivery is a drop in coverage. It remains to be seen whether countries can maintain adequate coverage of older children and children living further from health facilities.
It is particularly important to plan the transition, to educate the health workers and community mobilizers as to their new responsibilities, and to communicate the changed expectations to parents.
The Senegal example suggests that although financial costs can be cut by the shift to routine delivery, this may not necessarily improve cost-effectiveness. Senegal has not made the necessary investments to strengthen the capacity of health facilities, and hence to maintain coverage with vitamin A supplements. Simply pulling out the incentive payments and per diems but still requiring the outreach work to be done has been associated with poorer coverage.
Factors which help improve coverage irrespective of the mode of delivery include increased health worker literacy and ability to keep records, and community demand for services. Coverage is better if health workers can identify those children who have not been covered, if parents have a good understanding of the benefits that vitamin A brings for their children, and if there is buy-in from community leaders including religious leaders.
Finally, vitamin A supplementation in Senegal illustrates some of the broader issues involved in transitioning to a more sustainable approach via routine health services, and hence achieving the Sustainable Development Goal target of access to quality essential health care services.
Acknowledgments
We thank Balla Moussa Dedhiou, Country Director, Nutrition International Sahel Office for facilitating the study, and Papa Alioune Diop, Thiane Seck, Boubou Thiam, and Papa Ngore Sarr Sadio for their assistance with the qualitative fieldwork. The authors' responsibilities were as follows—AG and SH: designed the research; LSB, MD, BN, FN, and KN: conducted the research; SH and LSB: analyzed the data and wrote the paper; and all authors: read and approved the final manuscript.
Notes
Supported by Global Affairs Canada. Salaries of MD, BN, and AG were covered by Nutrition International.
SH, LSB, MD, BN, FN, KN, and AG, no conflicts of interest.
Abbreviations used:
- ASC
community health worker (agent de santé communautaire)
- FCFA
Franc of the Financial Community of Africa (Franc Communauté Financière d'Afrique)
- JSE
Child Survival Days (Journées de Survie de l'Enfant)
References
- 1. Beaton GH, Martorell R, Aronson KJ, Edmonston B, McCabe G, Ross AC, Harvey B. Effectiveness of Vitamin A supplementation in the control of young child morbidity and mortality in developing countries. Geneva: ACC/SCN, 1993. [cited 2017 June 30]. Available from: https://www.unscn.org/web/archives_resources/files/Policy_paper_No_13.pdf. [Google Scholar]
- 2. Imdad A, Herzer K, Mayo-Wilson E, Yakoob MY, Bhutta Z. Vitamin A supplementation for preventing morbidity and mortality in children from 6 months to 5 years of age. Cochrane Database Syst Rev 2010;12:CD008524. [DOI] [PubMed] [Google Scholar]
- 3. WHO. Guideline: vitamin A supplementation in infants and children 6–59 months of age. Geneva: World Health Organization, 2011. [cited 2017 Nov 15]. Available from: http://www.who.int/nutrition/publications/micronutrients/guidelines/vas_6to59_months/en/. [PubMed] [Google Scholar]
- 4. Fiedler J, Semakula R. An analysis of the cost of Uganda's Health Days Plus: do low costs indicate an efficient program or an underfinanced one? Food Nutr Bull 2014;35:92–104. [DOI] [PubMed] [Google Scholar]
- 5. Fiedler JL, Chuko T. The cost of Child Health Days: a case study of Ethiopia's Enhanced Outreach Strategy (EOS). Health Policy Plan 2008;23:222–33. [DOI] [PubMed] [Google Scholar]
- 6. UNICEF. Child Health Days. [cited 2017 Nov 14]. Available from: http://www.unicef.org/esaro/5479_child_health_days.html.
- 7. Routh S, Khuda B-E. An economic appraisal of alternative strategies for the delivery of MCH-FP services in urban Dhaka, Bangladesh. Int J Health Plann Manage 2000;15:115–32. [DOI] [PubMed] [Google Scholar]
- 8. Kahn JG, Muraguri N, Harris B, Lugada E, Clasen T, Grabowsky M, Mermin J, Shariff S. Integrated HIV testing, malaria, and diarrhea prevention campaign in Kenya: modeled health impact and cost-effectiveness. PLoS One 2012;7:e31316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ministère de la santé et de la prévention médicale. Programme national de supplémentation en vitamine A. Undated, unpublished.
- 10. Ministère de la santé et de la prévention médicale. Résultats journées supplémentation vitamine A – deuxième semestre 2015, unpublished.
- 11. Ministère de la santé et de la prévention médicale. Supplémentation en vitamine A de routine – deuxième semestre 2015, unpublished.
- 12. Gatobu S, Horton S, Kiflie Y, Abraham G, Birhanu N, Horton S, Greig A. Delivering vitamin A supplements to children aged 6 to 59 months: comparing delivery through mass campaign and through routine health services in Ethiopia. Food Nutr Bull 2017;38:564–73. [DOI] [PubMed] [Google Scholar]
- 13. Strauss AL, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Beverly Hills, CA: Sage, 1990. [Google Scholar]
- 14. XE. XE currency converter. [cited 2016 Oct 20]. Available from: http://www.xe.com/currencyconverter/convert/?From=XOF&To=USD.
- 15. Vijayaraghavan M, Wallace A, Mirza IR, Kamadjeu R, Nandy R, Durry E, Everard M. Economic evaluation of a Child Health Days strategy to deliver multiple maternal and child health interventions in Somalia. J Infect Dis 2012;205:S134–40. [DOI] [PubMed] [Google Scholar]
- 16. Ministère de la santé et de la prévention médicale. Données SVA semestre 1 2016. Dakar, unpublished 2016.
- 17. Neidecker-Gonzalez O, Nestel P, Bouis H. Estimating the global costs of vitamin A capsule supplementation: a review of the literature. Food Nutr Bull 2007;28:307–15. [DOI] [PubMed] [Google Scholar]
- 18. Ching P, Birmingham M, Goodman T, Sutter R, Loevinsohn B. Childhood mortality impact and costs of integrating vitamin A supplementation into immunization campaigns. Am J Public Health 2000;90:1526–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Federal Ministry of Health, Ethiopia. Integrating Enhanced Outreach Strategy (EOS) into Health Extension Programme (HEP) Ethiopia: a transitional plan. Final report. Addis Ababa, Ethiopia: Federal Ministry of Health, 2010. [Google Scholar]
- 20. Boex J, Fuller L, Malik A. Decentralized local health services in Tanzania. Washington (DC): Urban Institute, 2015. [cited 2016 Oct 20]. Available from: http://www.urban.org/sites/default/files/alfresco/publication-pdfs/2000215-Decentralized-Local-Health-Services-in-Tanzania.pdf. [Google Scholar]
- 21. MoHCDGEC, MoH, NBS, Office of the Chief Government Statistician, & ICF. Demographic and health survey and malaria indicator survey (TDHS-MIS) 2015-16. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF, 2016. Retrieved from: https://dhsprogram.com/pubs/pdf/FR321/FR321.pdf. [Google Scholar]
- 22. UNICEF. The state of the world's children, 2016 statistical tables; 2016. [cited 2016 Oct 21]. Available from: http://data.unicef.org/resources/state-worlds-children-2016-statistical-tables/.
- 23. Nutrition International. Why vitamin A: results; 2017. [cited 2017 June 30]. Available from: http://www.nutritionintl.org/what-we-do/by-micronutrient/micronutrientvitamin-a/.