Abstract
Background:
Patients with a neck of femur fracture have a high mortality rate. National outcomes have improved significantly as the management of this patient group is prioritized. In 2016, however, 4398 (6.7%) patients died within 30 days of admission.
Objective:
To investigate whether palliative care could be integrated early in the care plan for high-risk patients.
Methods:
All cases of inpatient mortality following neck of femur fracture at North Bristol Major Trauma Centre over a 24-month period were reviewed. A comprehensive assessment of care was performed from the emergency department until death. All investigations, interventions, and management decisions were recorded. A consensus decision regarding expected mortality was made for each case at a multidisciplinary meeting which included surgical, orthogeriatric, nursing, and anesthetic team input.
Results:
A total of 1033 patients were admitted following a neck of femur fracture. There were 74 inpatient deaths, and 82% were considered predictable at our multidisciplinary meeting. The mean length of stay was 18 days (range: 0-85, median 14). In 42% of cases, mortality was considered predictable on admission, and 40% were considered predictable following acute deterioration. These patients received on average 28 blood tests (range: 4-114) and 6.8 X-rays and computed tomographies (range: 2-20). Of this, 66% received end-of-life care; mean duration 2.3 days (range: 0-17).
Conclusions:
Mortality rates remain high in a subset of patients. This study demonstrates that intensive investigation and medical management frequently continues until death, including in patients with predictably poor outcomes. Early palliative care input has been integrated successfully into patient management in other specialties. We demonstrate that it is feasible to identify patients with hip fracture who may benefit from this expertise.
Keywords: geriatric trauma, systems of care, trauma surgery, geriatric nursing, geriatric medicine, physical medicine and rehabilitation
Introduction
Neck of femur (NOF) fractures present an ever-increasing health-care challenge. They are the commonest serious injury in older people and the commonest cause of accidental death.1 The total health and social service bill in the United Kingdom is over 1 billion pounds annually.1 Across the United Kingdom, the mean length of stay is 21.6 days.1 Following the introduction of robust management pathways and best practice tariff for patients with NOF fractures, mortality rates have declined; however, the mean 30-day mortality remains 6.7%.1 The percentage of the population aged 65 years and older is set to increase from 18% in 2016 to over 24% in 2046.2 Combined with an expanding population, this represents an increasing burden to our health-care services.
Palliative care has become recognized as an independent specialty; the World Health Organization formally defined the term in 1989.3 Since then, it has grown substantially with the aim of providing physical, emotional, spiritual, and social support.3 Care provided to both patients with cancer and other chronic disease leads to positive outcomes.4-6 Early integration of palliative care is associated with improved continuity and coordination of care, greater quality of life, improved symptom control, and a reduction in health-care costs.4,5 Carers may also benefit from the additional expertise.7 Temel and colleagues demonstrated a significantly lower rate of depression coupled with a survival benefit in patients with metastatic small-cell lung cancer.6 Bakitas et al demonstrated improved mood and quality of life following the integration of a palliative care program for patients with a variety of cancers.8 Patients with nononcological disease may also benefit from the early integration; a reduction in symptom burden has been demonstrated in patients with refractory breathlessness.9 In the trauma ICU environment, care plans and “Do-not-attempt-resuscitation” orders were initiated earlier, resulting in a reduced length of stay without an increase in mortality.10 Several of the palliative interventions described in the literature can be delivered by trained individuals under the supervision of specialist palliative care physicians.6,9,10 This distinction is important when considering the financial implications of any initiatives.
The aim of this study was to investigate treatment escalation plans and end-of-life management of inpatients with NOF fractures at a major trauma center. Focus was placed on the duration of medical therapy, the involvement of palliative care teams, and the timing of end-of-life management plans. An assessment of the predictability of inpatient mortality was performed.
Method
Study Design
All patients admitted to a major trauma center with an NOF fracture from January 2015 until December 2016 were included in this observational study. This included all inpatient falls that resulted in an NOF fracture. All cases of inpatient mortality were highlighted, and each month a comprehensive review was performed of patient care from prehospital management until death.
Data Collection
Data were gathered from ambulance charts, emergency department documentation, hospital notes, anesthetic charts, bedside documentation and observations, death certificates, and coroners’ reports. Our pathology and radiology system was interrogated for all investigations requested during the inpatient stay.
Management was separated into prehospital, emergency department, preoperative, surgical, and postoperative care. Table 1 illustrates the data recorded for each patient. Focus was placed on the involvement of palliative care, including ceiling of care decisions and the timing of end-of-life support. These data were combined with the information submitted by the Trust to the National Hip Fracture Database.
Table 1.
Data Collection.
| Care Period | Data Collected |
|---|---|
| Prehospital | Current residence, general health, mobility, events leading to injury, prehospital analgesia |
| Emergency department | Time in the emergency department, analgesia, fluid prescription, medical problems identified and treated, admission ward |
| Preoperative | ASA Score, preoperative carbohydrate drink, preoperative orthogeriatric review, anesthetic reviews on the ward, anesthetic management, delays, nutritional status, waiting time in theater, preoperative bloods including hemoglobin and lactate |
| Operative | Grade of anesthetist, anesthetic type, grade of surgeon, operation, duration of surgery, time in recovery, complications, further interventions |
| Postoperative | Arrival time to the ward, initial observations, time to medical review, time to orthogeriatric review, postoperative medical problems, actions, outcomes of actions, postoperative blood results, end-of-life management, cause of death |
Abbreviation: ASA, American Society of Anesthesiologists.
Morbidity and Mortality Meeting
Each patient was discussed at a monthly morbidity and mortality meeting. This was attended by a minimum of 1 consultant from each of the orthopedic, orthogeriatric, anesthetic, and emergency department teams, in addition to the lead ward nurse, junior doctors, and orthogeriatric nurses. The management of each patient was reviewed, and an assessment was made of whether death was anticipated. This was classified as anticipated following admission, anticipated following acute medical deterioration, and not anticipated.
Data Analysis
All data were anonymized and placed on a secure trust database. Means, medians, and standard deviations were calculated for numerical data. The χ2 test was performed on nonparametric categorical data. An unpaired Student t test was used to compare the abbreviated mental test score (AMTS) score between the 2 groups.11 The length of time prior to death that patients were placed on end-of-life care was recorded. A Nottingham Hip Fracture Score (NHFS) was calculated retrospectively for all patients.12
Results
Patient Admissions With an NOF Fracture
A total of 1033 patients received management for an NOF fracture during the study period. Of this, 60% were intracapsular fractures. Twelve patients presented following falls in hospital. There were 74 inpatient deaths across the 24 months. Six of these patients did not receive an operation, as they were considered to be too unwell. Patients in the mortality group were more likely to be male (P = .017) with a lower AMTS on admission (P ≤ .0001), illustrated in Table 2. Patients who died in hospital had on average a higher American Society of Anesthesiologists (ASA) grade (P ≤ .0001) and were more likely to be admitted from a residential home (P ≤ .0001).
Table 2.
Comparison Between the Mortality Group and All Patients Admitted With a NOF Fracture.
| Patient characteristics | All Patients | Mortality Group |
|---|---|---|
| % female | 70% | 58% |
| Mean age | 83 (61-105) | 86 (68-101) |
| Mean AMTS on admission | 7.4 (0-10) | 4.9 (0-10) |
| % from nursing/residential home | 18% | 31% |
| ASA Score 3 or more | 72% | 88% |
| Delay >36 hours until surgery | 18% | 15% |
| Mobilized the day following surgery | 77% | 70% |
Abbreviations: AMTS, abbreviated mental test score; ASA, American Society of Anesthesiologists; NOF, neck of femur.
Mortality Group
In the mortality group, the mean preoperative hemoglobin was 114.4 g/L (range: 78-185). Patients spent on average 4.7 hours in the Emergency Department (range: 2-9), and the mean duration of surgery was 1.7 hours (range: 0.8-3.75). The primary surgeon was a registrar in 61% of patients, a consultant in 16%, and a junior trainee in 23%. These trainees are at least 1 year following medical school but not yet on an orthopedic training program. Patients commonly had multiple postoperative medical issues (Table 3).
Table 3.
Postoperative Medical Problems.
| Acute kidney injury | 32% | Fast AF | 11% |
| Delirium/agitation | 23% | Anemia (Hb < 80 g/dL) | 20% |
| Respiratory tract infection | 50% | Hypotension | 24% |
| Electrolyte abnormalities | 22% | Congestive heart failure and pulmonary oedema | 16% |
Abbreviations: AF, atrial fibrillation; Hb, hemoglobin.
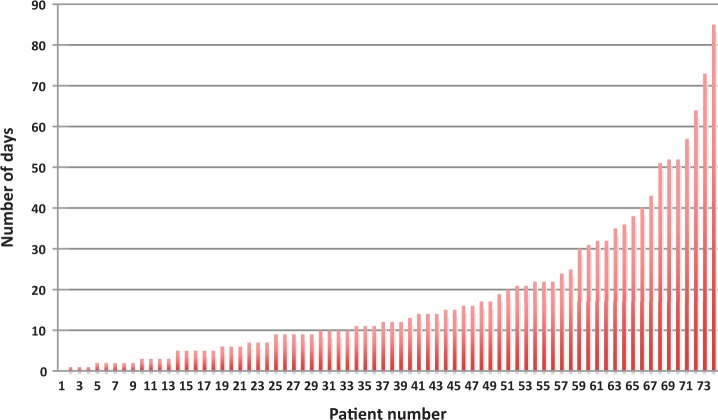
During admission, patients received on average 28 blood tests (range: 4-114, median 22), 6 X-rays (range: 2-16, median 5), and 1 computed tomography (CT) scan (range: 0-7, median 0). Patients were managed on end-of-life care plans for a mean of 2.3 days (range: 0-17 days, median 1 day). In 25 patients, full medical management was continued on the ward up until death. Two patients received cardiopulmonary resuscitation. The mean time from admission until death was 18 days (range: 1-85, median 12 days) as shown in Figure 1.
Figure 1.
Number of days from admission until death.
A retrospective NHFS was calculated. The mean 30-day mortality risk on admission was 13% (range: 4.4%-45%, median 11%). Figure 2 demonstrates the number of patients who received end-of-life care relative to their NHFS on admission.
Figure 2.
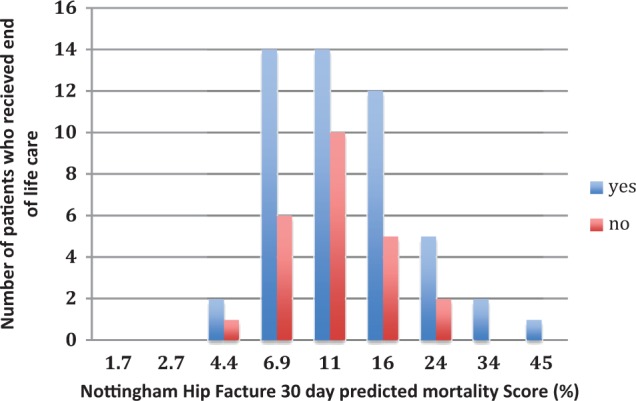
Proportion of patients receiving end-of-life care, relative to their predicted mortality on admission.
A respiratory tract infection was the primary cause of death in 34 cases. In 6 patients, the cause of death was acute cardiac ischemia and pulmonary embolism in 3 cases. Following case discussion at our departmental multidisciplinary team (MDT) meeting, death was considered predictable in 82% of patients and in 43% of death was deemed predictable on admission.
Discussion
This study demonstrates that end-of-life care is initiated for a mean duration of 2.3 days, prior to death in patients with an NOF fracture. In 34% of patients, medical management and ward-based interventions were continued until death. Our MDT assessment revealed that in many cases, inpatient mortality may have been predictable on or shortly after admission. Despite this, patients received up to 114 blood tests and between 2 and 16 X-rays and CT scans. This may cause both significant distress to patients and have substantial financial implications without positively affecting outcome.
The expectation that surgery will “fix” the problem and improve patients’ outcomes can make discussions surrounding prognosis difficult.10 Furthermore, work performed in a surgical intensive care unit demonstrated wide variation in the satisfaction of nurses, surgeons, and physicians with communication related to prognosis.13
Medical interventions may be continued until the late stages in certain conditions. Mitchell and colleagues compared the management decisions for 2492 nursing home patients with advanced dementia to those with terminal cancer.14 Of this, 1.1% of patients with advanced dementia were predicted to die within 6 months; however, the proportion reached 71%. These patients were more likely to die with a feeding tube compared to those with terminal cancer (25% vs 5.2%), they were more likely to undergo laboratory tests (49.2% vs 32.3%) and receive intravenous therapy (10.1% vs 7.1%). In patients with severe Alzheimer disease and a fever, thorough investigation and antibiotic therapy may not result in improved outcomes compared to symptom management only. Fabiszewski et al demonstrated no difference in survival between those who received a series of laboratory tests and imaging followed by targeted antibiotic therapy (n = 37) compared to symptom management and intensive nursing care only (n = 38).15 However, in less severe cases, antibiotics provided a significant survival benefit.
The evidence to support more timely involvement of palliative care teams is increasing; however, there are several barriers that must be overcome. The provision of care has traditionally been considered as 2 independent entities along a spectrum where life-prolonging therapy is prioritized, until the initiation of care to optimize comfort and minimize suffering.16 Student exposure to palliative interventions during medical school is limited, and many clinicians believe it represents end-of-life support, focused on symptom control, following the cessation of active treatment.17,18 Clinicians may be reluctant to recommend palliative care input while active care is ongoing due to concerns about reducing hope or increasing fear.19,20 According to the National Institute of Clinical Excellence (NICE), palliative care is “the active holistic care of patients with advanced, progressive illness…many aspects of palliative care are also applicable earlier in the course of the illness in conjunction with other treatments.”21 Dalal and colleagues demonstrated an increase in palliative care referrals following a change in the name from “palliative” to “supportive” care, and a “supportive care model” has been proposed to encourage a more holistic approach to frail older patients.22,23 In the context of patients with cancer, NICE considers supportive care to represent an “umbrella term” for the broad variety of resources and care required.21
The current 1 year net survival for men of stage 2 lung cancer is 72.7%.24 Even with the significant improvements in hip fracture care, 1 year survival rates remain between 70% and 80% and are comparable to early stages of lung cancer where palliative care programs are well established.1,24 The NICE guidelines recommend early surgery and prompt mobilization; however, end-of-life management is not implicitly included.25 We were unable to find evidence of targeted palliative care plans for patients with NOF fracture in the literature.
Determining an accurate prognosis can be particularly difficult in nonmalignant disease.4 This can lead to reduced involvement of palliative care teams, despite high symptom burdens.26 Chronic conditions such as heart failure and chronic obstructive pulmonary disease often result in acute exacerbations on a background of chronic decline.18,19 In contrast, patients with Parkinson disease may face a slow deterioration without a clear trigger for palliative intervention.27 Trauma in older patients is particularly challenging due to the abrupt stepdown in function.28 On admission, patients and their relatives are provided with large volumes of information in a short period of time, prior to early surgery. On an acute trauma ward, palliative care discussions may not be prioritized, and junior medical staff may lack the confidence and education to conduct these independently.
Although risk stratification scores exist, patients admitted with an NOF fracture frequently have unpredictable outcomes due to the medical complexity typically seen in this population. The retrospective NHFS performed on our study group revealed a mean 30-day mortality risk of 13%. Encouragingly, in this study, patients with the highest NHFS did receive end-of-life care. Marufu and colleagues performed a systematic review of perioperative risk scoring models to predict morbidity and mortality in patients with fragility hip fractures.29 Twenty-five scoring systems were identified, 4 of which had been validated outside the original institution. More recently, McGreevy et al demonstrated the “Palliative Performance Scale” is a useful predictor of mortality and poor functional outcome in elderly trauma patients.30 Prediction models may also focus on the risk of in-hospital mortality only.31 In our study, the mortality group were more likely to be male, admitted from institutional care, with a lower AMTS and a higher ASA grade.
Given the high number of prognostic scoring systems currently available, our aim is to highlight the importance of suitable planning for end-of-life care by applying the available systems to prevent patients receiving unnecessary investigations and interventions. Resources are limited and a routine review of all patients with a fragility hip fracture by a palliative care physician may be unrealistic. To maximize patient benefit within the current resource constraints, palliative care could be integrated on admission in 1 of 2 ways. Patients deemed to be higher risk using one or more prediction tools, such as the externally validated NHFS or the Palliative Performance Scale, could be selected for further palliative assessment.12,32 Alternatively, several studies have described interventions initiated in all patients at the time of admission or diagnosis.6,9,10 This may include a routine patient and family discussion around the goals of care, likely prognosis, and patient preferences.10 Interventions could occur before or after surgery depending on several factors including the patient’s acute condition, the time available prior to surgery, the time of admission, and the presence of family members.
Should surgery be performed in very high-risk patients that are not expected to survive their hospital admission? Limited work exists in this area. A recent systematic review demonstrated very few studies comparing operative and nonoperative management.33 The available work focuses on mortality and not quality of life or health-care costs. Six patients in our mortality group did not receive a procedure following a consensus decision from the MDT. Due to their medical condition on admission, they were considered to have a very low chance of surviving surgery and received symptom management only.
Further work is necessary to explore the opinions of patients and members of the MDT regarding early palliative care interventions in patients with fragility hip fractures, to aid design of the most appropriate interventions.
Limitations
This work was carried out in a single hospital, and patient populations in other regions may vary; however, this regional major trauma center has an established orthogeriatric team and over 500 annual admissions for patients with an NOF fracture. The work is retrospective, and so informal care discussions with patients and their relatives may not be included; however, clinicians are encouraged to document all care escalation decisions and a comprehensive review of patient documentation followed by a multidisciplinary discussion has been carried out. These discussions were performed after death, and so potential bias is substantial; however, they highlight that patients may demonstrate several predictors of deterioration.
Conclusion
Over one-third of patients with NOF fracture in this study received full active medical care until death despite clear, early indicators that they were unlikely to survive the current inpatient episode. End-of-life care planning was frequently delayed until death was imminent, and patients received large numbers of investigations. Admission to hospital with an NOF fracture continues to be associated with high mortality rates, and although palliative care programs have been successfully integrated into the management of a broad range of conditions with demonstrated efficacy, they do not appear to have been considered for hip fractures. Early palliative care involvement may improve quality of life and reduce the frequency of interventions and acute hospital stay for the frailest patients.
Footnotes
Authors’ Note: The authors are happy to provide further data from this work on request.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Royal College of Physicians. National Hip Fracture Database annual report 2017. 2017. http://www.nhfd.co.uk/. Accessed September 19, 2017.
- 2. Office for National Statistics. Overview of the UK population: July 2017. 2017. https://www.rcplondon.ac.uk/projects/outputs/national-hip-fracture-database-annual-report-2017. Accessed July 28, 2017.
- 3. Clark D. From margins to centre: a review of the history of palliative care in cancer. Lancet Oncol. 2007;8(5):430–438. [DOI] [PubMed] [Google Scholar]
- 4. Siouta N, van Beek K, Preston N, et al. Towards integration of palliative care in patients with chronic heart failure and chronic obstructive pulmonary disease: a systematic review of European guidelines and pathways. BMC Palliat Care. 2016;15:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Aldridge MD, Hasselaar J, Garralda E, et al. Education, implementation and policy barriers to greater integration of palliative care: a literature review. Palliat Med. 2016;30(3):224–239. [DOI] [PubMed] [Google Scholar]
- 6. Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small cell lung cancer. N Engl J Med. 2010;363(8):733–742. [DOI] [PubMed] [Google Scholar]
- 7. Hannon B, Swami N, Rodin G, Pope A, Zimmermann C. Experiences of patients and caregivers with early palliative care: a qualitative study. Palliat Med. 2017;31(1):72–81. [DOI] [PubMed] [Google Scholar]
- 8. Bakitas M, Lyons KD, Hegel MT, et al. The project ENABLE II randomised controlled trial to improve palliative care in patients with advanced cancer. JAMA. 2009;302(7):741–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med. 2014;2(12):979–987. [DOI] [PubMed] [Google Scholar]
- 10. Mosenthal AC, Murphy PA, Barker LK, Lavery R, Retano A, Livingston DH. Changing the culture around end-of-life care in the trauma intensive care unit. J Trauma. 2008;64(6):1587–1593. [DOI] [PubMed] [Google Scholar]
- 11. Hodkinson HM. Evaluation of a mental test score for assessment of mental impairment in the elderly. Age Ageing. 1972;1(4):233–238. [DOI] [PubMed] [Google Scholar]
- 12. Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101(4):511–517. [DOI] [PubMed] [Google Scholar]
- 13. Aslakson RA, Wyskiel R, Shaeffer D, et al. Surgical intensive care unit clinician estimates of the adequacy of communication regarding patient prognosis. Crit Care. 2010;14(6):R218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mitchell SL, Kiely DK, Hamel MB. Dying with advanced dementia in the nursing home. Arch Intern Med. 2004;164(3):321–326. [DOI] [PubMed] [Google Scholar]
- 15. Fabiszewski KJ, Volicer B, Volicer L. Effect of antibiotic treatment on outcome of fevers in institutionalized Alzheimer patients. JAMA. 1990;263(23):3168–3172. [PubMed] [Google Scholar]
- 16. Morrison RS, Meier DE. Clinical practice. Palliative care. N Engl J Med. 2004;350(25):2582–2590. [DOI] [PubMed] [Google Scholar]
- 17. Von Roenn JH, Voltz R, Serrie A. Barriers and approaches to the successful integration of palliative care and oncology practice. J Natl Compr Canc New. 2013;11(suppl 1):S11–S16. [DOI] [PubMed] [Google Scholar]
- 18. Kavalieratos D, Mitchell EM, Carey TS, et al. “Not the ‘Grim Reaper Service’”: an assessment of provider knowledge, attitudes, and perceptions regarding palliative care referral barriers in heart failure. J Am Heart Assoc. 2014;3(1):e000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vermylen JH, Szmuilowicz E, Kalhan R. Palliative care in COPD: an unmet area for quality improvement. Int J Chronic Obstr. 2015;10:1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Greer JA, Jackson VA, Meier DE, Temel JS. Early integration of palliative care services with standard oncology care for patients with advanced cancer. CA Cancer J Clin. 2013;63(5):349–362. [DOI] [PubMed] [Google Scholar]
- 21. National Institute for Health and Clinical Excellence. Improving supportive and palliative care for adults with cancer (CSG4). 2004. https://www.nice.org.uk/guidance/csg4. Accessed July 26, 2017.
- 22. Dalal S, Palla S, Hui D, et al. Association between a name change from palliative to supportive care and the timing of palliative care referrals at a comprehensive cancer centre. Oncologist. 2011;16(1):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nicholson C, Morrow EM, Hicks A, Fitzpatrick J. Supportive care for older people with frailty in hospital: An integrative review. Int J Nurs Stud. 2016;66:60–71. [DOI] [PubMed] [Google Scholar]
- 24. Office for National Statistics. Cancer survival in England: adult, stage at diagnosis and childhood—patients followed up to 2016. 2017. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/cancersurvivalinengland/adultstageatdiagnosisandchildhoodpatientsfollowedupto2016. Accessed July 26, 2017.
- 25. National institute for Health and Care Excellence. Hip fracture: Management (CG124). 2017. https://www.nice.org.uk/guidance/cg124. Accessed 19/08/2017. [PubMed]
- 26. Ahmadi Z, Wysham NG, Lundström S, Janson C, Currow DC, Ekström M. End-of-life care in oxygen-dependent ILD compared with lung cancer: a national population-based study. Thorax. 2016;71(6):510–516. [DOI] [PubMed] [Google Scholar]
- 27. Siobhan F, Cashell A, Kernohan WG, et al. Interviews with Irish healthcare workers from different disciplines about palliative care for people with Parkinson’s disease: a definite role but uncertainty around terminology and timing. BMC Palliat Care. 2016;15:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Costa ML, Griffin XL, Achten J, et al. World Hip Trauma Evaluation [WHITE]: framework for embedded comprehensive cohort studies. BMJ Open. 2016;6(10):e011679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marufu TC, Mannings A, Moppett IK. Risk scoring models for predicting peri-operative morbidity and mortality in people with fragility hip fractures: qualitative systematic review. Injury. 2015;46(12):2325–2334. [DOI] [PubMed] [Google Scholar]
- 30. McGreevy CM, Bryczkowski S, Pentakota SR, Berlin A, Lamba S, Mosenthal AC. Unmet palliative care needs in elderly trauma patients: can the Palliative Performance Scale help close the gap? Am J Surg. 2017;213(4):778–784. [DOI] [PubMed] [Google Scholar]
- 31. Endo A, Bear HJ, Nagao M, Weaver MJ. Prediction model of in-hospital mortality after hip fracture surgery. J Orthop Trauma. 2018;32(1):34–38. [DOI] [PubMed] [Google Scholar]
- 32. Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative Performance Scale (PPS): a new tool. J Palliat Care. 1996;12(1):5–11. [PubMed] [Google Scholar]
- 33. van de Ree CLP, De Jongh MAC, Peeters CMM, de Munter L, Roukema JA, Gosens T. Hip fractures in elderly people: surgery or no surgery? a systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. 2017;8(3):173–180. [DOI] [PMC free article] [PubMed] [Google Scholar]