Abstract
Objectives
The purpose of this study was to validate T2* mapping as an objective, noninvasive method for the prediction of acetabular cartilage damage.
Methods
This is the second step in the validation of T2*. In a previous study, we established a quantitative predictive model for identifying and grading acetabular cartilage damage. In this study, the model was applied to a second cohort of 27 consecutive hips to validate the model. A clinical 3.0-T imaging protocol with T2* mapping was used. Acetabular regions of interest (ROI) were identified on magnetic resonance and graded using the previously established model. Each ROI was then graded in a blinded fashion by arthroscopy. Accurate surgical location of ROIs was facilitated with a 2-dimensional map projection of the acetabulum. A total of 459 ROIs were studied.
Results
When T2* mapping and arthroscopic assessment were compared, 82% of ROIs were within 1 Beck group (of a total 6 possible) and 32% of ROIs were classified identically. Disease prediction based on receiver operating characteristic curve analysis demonstrated a sensitivity of 0.713 and a specificity of 0.804. Model stability evaluation required no significant changes to the predictive model produced in the initial study.
Conclusions
These results validate that T2* mapping provides statistically comparable information regarding acetabular cartilage when compared to arthroscopy. In contrast to arthroscopy, T2* mapping is quantitative, noninvasive, and can be used in follow-up. Unlike research quantitative magnetic resonance protocols, T2* takes little time and does not require a contrast agent. This may facilitate its use in the clinical sphere.
Keywords: T2*, quantitative cartilage imaging, hip
Despite intense interest in cartilage preservation surgery, there is no clinically available method that objectively measures the state of a patient’s articular cartilage. As a result, today’s clinician has no objective, quantitative way to assess a patient’s suitability for cartilage preservation surgery. Current clinical practice is based on radiography, a qualitative technology not significantly changed for over a century.1 Similarly, once a procedure has been performed, the clinician or clinical researcher cannot quantitatively measure whether the intervention has positively or negatively affected the patient’s articular cartilage—or if indeed it has affected the patient’s articular cartilage at all. The data presented here suggest that this issue may be addressed with the use of T2* mapping, a quantitative sequence that can be performed in a short amount of time on clinical 3-T scanners without the use of contrast.2
While other medical specialties such as cardiology and neurology have validated clinical magnetic resonance imaging (MRI) sequences that are applicable to their specialty-specific questions, orthopedic surgery largely has not and no sequence has been validated for acetabular cartilage.3-6 Instead, quantitative cartilage imaging of the hip has been limited to research protocols introduced in the 1990s that have not been adopted by the clinical community in part because of concerns with cost, reliability, and the safety of intravenous contrast.7,8 The absence of an accessible, objective measure of cartilage quality has likely affected cartilage preservation research and patient care.
T2* mapping may have the ability to change this. It can be performed using existing clinical scanners, requires no intravenous contrast, requires only a few additional minutes of scan time, and is known to provide a reproducible, quantitative biochemical evaluation of articular cartilage.9 Though T2* would appear ideally suited for clinical use, it has not been clinically validated and therefore cannot be used.
The purpose of this study was to further the goal of clinically validating T2*. In a previous publication, we presented the first step in validating T2*, presenting evidence that T2* values could be used to accurately predict the state of acetabular hyaline cartilage.10 This was done by comparing the results of T2* to a diagnostic arthroscopy gold standard. That study reported on a single cohort with which T2* thresholds were both statistically identified and then retroactively applied to the same cohort. As such, it did not represent validation of the technique, only the initial step toward doing so. In this communication, we now report on the second step, validation of these thresholds by reproducing the results on a second, independent cohort of patients with femoroacetabular impingement. We further suggest that T2* may represent, in concert with patient-reported outcome scores, a future standard for reporting the long-term clinical outcomes of attempts at preserving hip cartilage via surgical procedures.
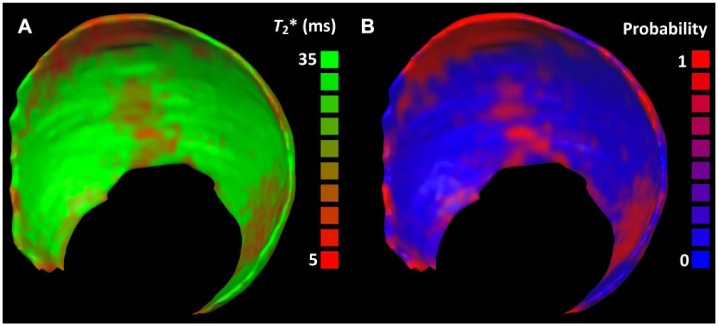
Following our previously published protocol, 27 consecutive patients who met the following criteria were recruited: the patient had undergone our routine, clinical 3-T MRI arthrogram protocol which includes an additional five minutes of scan time for T2* mapping and who then proceeded to arthroscopic hip surgery. Exclusion criteria were (1) Tönnis grade 2 or higher on radiographs; (2) patients with hip dysplasia, osteonecrosis, Perthes, or protrusio deformity; (3) patients who had undergone previous ipsilateral hip surgery; and (4) patients who presented with an appropriate, diagnostic MRI performed at an outside institution. Using our routine MRI, a standardized set of acetabular regions of interest (ROIs) were identified in our study patients and the corresponding T2* values were placed on a map projection of the patient’s acetabulum ( Fig. 1 ). Aided by this map projection, but blinded to the T2* value, each individual ROI was then identified arthroscopically, examined by the surgeon with a smooth probe, and then graded on a common 6-grade descriptor of cartilage changes specific to the acetabulum.11
Figure 1.
T2* relaxation time map showing areas of poor acetabular cartilage quality in red (A) and the respective probability map of disease (B).
The arthroscopic grading of each ROI was then used as the gold standard with which to evaluate how these regions of interest were graded using T2*. Statistical analysis to compare the 2 data sets was developed by an independent, biomedical statistician using the same methods as in the previous study. For each voxel, we produced a predicted Beck value by first applying our predictive model to the voxel’s T2* value and the patient’s sex and weight. This yielded a predicted probability for each Beck category. The category with the highest predicted probability was taken to be the voxel’s predicted Beck score. We used a parametric bootstrapping procedure to obtain smooth estimates of the receiver operating characteristic curve (ROC) and 95% pointwise confidence band. These statistical methods were then submitted for review by the statistical community and published in the peer-reviewed biomedical statistical literature.12 The study was approved by an institutional review board.
In total, 459 ROIs were graded for cartilage quality by both a surgical examination and with T2* mapping. When the 2 techniques were compared for agreement, 32% of ROIs were graded identically, and 82% of ROIs were graded within ±1 grade. Disease prediction based on ROC analysis demonstrated a sensitivity of 0.713 and a specificity of 0.804 ( Fig. 2 ). Model stability evaluation required no significant changes to the predictive model produced in the initial study.
Figure 2.
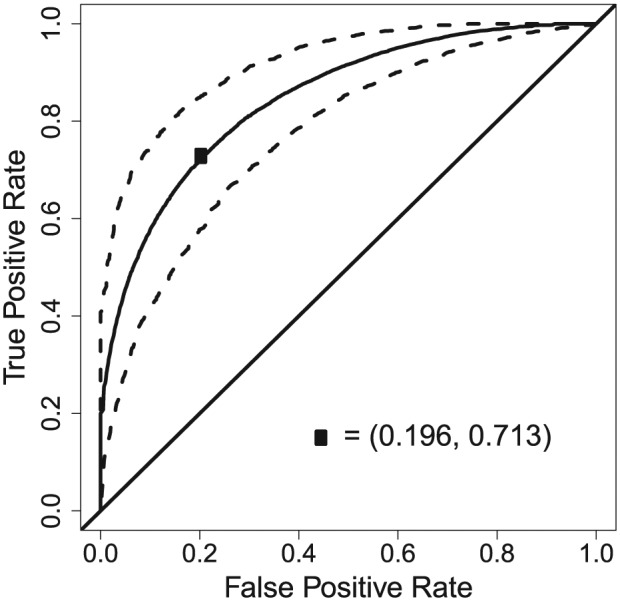
Receiver operating characteristics curve for the dichotomized outcome.
The results of this second cohort of patients validates the findings of our first cohort, verifying that T2* mapping provides information that is statistically comparable to the information gained from diagnostic arthroscopy. In contrast to a surgical gold standard, we suggest that T2* is convenient, inexpensive, allows for repeated evaluation of the joint over time, and poses no additional risk to the patient. Because it can be performed pre-operatively, T2* mapping may be useful in identifying both who may benefit from a surgical intervention the most and also the least, avoiding both the undertreatment of a painful condition while identifying instances when the risks of surgery are unwarranted.
We also suggest that current alternatives to the surgical gold standard—radiographs and nonquantitative MRI—are too frequently unreliable in the clinical sphere and inadequate as investigative tools. Radiographs are graded on a 0 to 3 Tönnis scale, a scale that has been shown to have poor intrarater reliability; nonquantitative MRI—graded most often with a subjective mild, moderate, severe descriptor—provides different but not necessarily better information than plain radiographs.13-15
By validating a safe, convenient, and inexpensive method of reliably quantifying acetabular cartilage the results of this study also offer a significant advancement toward the goal of routine, objective assessment of the results surgical hip interventions. Today, the end-points for evaluating and reporting the results of joint preservation surgery rely largely on secondary measures of outcome such as pain or conversion to arthroplasty, a limitation imposed by the lack of a practical source of objective cartilage data. While we strongly agree that the result of a surgical procedure from the patient’s perspective is paramount and that data from patient reported outcomes are essential, we also believe that this in no way absolves the surgeon from the obligation to know a procedure’s anatomic consequences. Specifically, in the case of young adult hip surgery, we believe that a procedure described as joint preserving should be so described based on more than simply not being an arthroplasty. Seen in this light, the real value in T2*’s ability to reliably quantify articular cartilage may lie in an ability to evaluate the efficacy of the current generation of orthopedic hip procedures and thus to objectively discern their long-term effects on the growing population of young patients that are undergoing them. The reliability of T2* in quantitatively evaluating articular cartilage is likely not limited to the hip. Further efforts to understand and use this powerful tool are warranted.
Data from this study can be accessed by contacting the corresponding author.
Footnotes
Authors’ Note: This work was performed at The University of Minnesota–Twin Cities.
Acknowledgments and Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Academy of Finland Grant 285909 and Departmental Funding from the Departments of Orthopaedic Surgery and Radiology, University of Minnesota.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: Ethical approval to report this case was obtained from University of Minnesota Institutional Review Board
Informed Consent: Written informed consent was obtained for anonymized patient information to be published in this article.
References
- 1. Nissi MJ, Mortazavi S, Hughes J, Morgan P, Ellermann J. T2* relaxation time of acetabular and femoral cartilage with and without intraarticular gadopentetate dimeglumine in patients with femoroacetabular impingement. AJR Am J Roentgenol. 2015;204(6):W695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shanks SC. Radiology in the twenties. Br J Radiol. 1973;46(550):766-7. [DOI] [PubMed] [Google Scholar]
- 3. Allen LM, Hasso AN, Handwerker J, Farid H. Sequence-specific MR imaging findings that are useful in dating ischemic stroke. Radiographics. 2012;32(5):1285-97. [DOI] [PubMed] [Google Scholar]
- 4. Ginat DT, Fong MW, Tuttle DJ, Hobbs SK, Vyas RC. Cardiac imaging: part 1, MR pulse sequences, imaging planes, and basic anatomy. AJR Am J Roentgenol. 2011;197(4):808-15. [DOI] [PubMed] [Google Scholar]
- 5. Pohost GM. The history of cardiovascular magnetic resonance. JACC Cardiovasc Imaging. 2008;1(5):672-678. [DOI] [PubMed] [Google Scholar]
- 6. Savoy RL. History and future directions of human brain mapping and functional neuroimaging. Acta Psychol. 2001;107(1):9-42. [DOI] [PubMed] [Google Scholar]
- 7. Adil B, Gray ML, Burstein D. Gd-DTPA2− as a measure of cartilage degradation. Magn Reson Med. 1996;36(5):665-73. [DOI] [PubMed] [Google Scholar]
- 8. Engen CN, Løken S, Årøen A, Ho C, Engebretsen L. No degeneration found in focal cartilage defects evaluated with dGEMRIC at 12-year follow-up. Acta Orthop. 2017;88(1):82-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chavhan GB, Babyn PS, Thomas B, Shroff MM, Haacke EM. Principles, techniques, and applications of T2*-based MR imaging and its special applications. RadioGraphics. 2009;29(5):1433-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ellermann J, Ziegler C, Nissi MJ, Goebel R, Hughes J, Benson M, et al. Acetabular cartilage assessment in patients with femoroacetabular impingement by using T2* mapping with arthroscopic verification. Radiology. 2014;271(2):512-23. [DOI] [PubMed] [Google Scholar]
- 11. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012-8. [DOI] [PubMed] [Google Scholar]
- 12. Henn LL, Hughes J, Iisakka E, Ellermann J, Mortazavi S, Ziegler C, et al. Disease severity classification using quantitative magnetic resonance imaging data of cartilage in femoroacetabular impingement. Stat Med. 2017;36(9):1491-505. doi: 10.1002/sim.7213. [DOI] [PubMed] [Google Scholar]
- 13. Carlisle JC, Zebala LP, Shia DS, Hunt D, Morgan PM, Prather H, et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop J. 2011;31:52-8. [PMC free article] [PubMed] [Google Scholar]
- 14. Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467(3):666-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Berlin, Germany: Springer; 1987. [Google Scholar]