Abstract
Retears of the rotator cuff, following operative repair, is not an uncommon event. Various factors have been shown to influence recurrence including the technique of repair. Multiple techniques have been performed with varying results and complications. The repair technique significantly affects the rate and pattern of retears. Although risk of retears with double row and suture bridge techniques is relatively low, medial cuff failure is a potential complication which poses significant challenges when revision repair is undertaken. Modifications in surgical techniques in, both, double row and suture bridge repairs can help decrease the risk of medial cuff failure. Thorough analysis of retear rates and patterns reported, and their relation with the repair technique, provides new insights about the pathogenesis of rotator cuff retears, their future prevention and appropriate management.
Key words: Recurrent cuff tears, medial cuff failure, revision rotator cuff repair, retear rates, retear patterns
Introduction
Tears of the rotator cuff are a common pathological entity of the shoulder, and are present in 20.7% of the general population.1 Various approaches and techniques have been described to repair a torn rotator cuff. Despite advancements in surgical technique, retear of a previously repaired rotator cuff tendon is a fairly common complication. Although functional outcomes do not always correlate with the structural integrity after repair,2 several studies reported superior outcomes in intact tendons compared to retorn ones.3,4 Repair of a recurrent rotator cuff tear (RRCT) is more difficult owing to shorter tendons and excess implant at the footprint. Multiple patient factors and operative techniques affect the rate and pattern of rotator cuff retears. The aim of this article is to review the rates, patterns, and management of rotator cuff retears, and how these factors are affected by different methods of primary repair.
Tendon to bone healing
Animal studies have shown that regeneration of the structure and composition of the normal tendon-bone interface is never achieved after repair of the torn rotator cuff tendon.5 Healing begins with formation of a fibrovascular tissue which acts as a scaffold for gradual bone ingrowth. Finally, collagen fiber continuity is re-established.6 Several genetic factors and inflammatory mediators play important roles during the healing process. Growth factors can potentially be administered to promote tendon healing after repair. In a rat model, addition of transforming growth factor-beta 3 (TGF-β3) to calcium-phosphate matrix improved strength of repair at 4 weeks postoperatively compared to calcium-phosphate matrix alone.7 Similarly, application of fibroblast growth factor-2 to rotator cuff defects reconstructed with acellular dermal matrix in rats accelerated remodeling and improved biomechanical strength.8 In a sheep model, application of bone morphogenetic protein-12 showed increased formation of new bone and fibrocartilage at the tendon bone interface on magnetic resonance imaging (MRI) and histologic examinations. Additionally, biomechanical testing showed increased load-to-failure.9
The effect of platelet-rich fibrin matrix (PRFM) on the structural integrity of rotator cuff tendons after repair is controversial. Barber et al.10 demonstrated lower retear rates on MRI with the addition of PRFM. On the other hand, it has been shown, in two randomized controlled trials, that PRFM is not beneficial for rotator cuff tendon healing after repair.11,12
Diagnosis of a rotator cuff tear after surgical repair does not always imply failure of healing. It can theoretically be secondary to early mechanical failure due to an unsound repair, biologic failure of healing despite a good repair or recurrent tear after successful healing of the initial tear. Miller et al.13 reported 9 retears, 7 of which were diagnosed during the first 3 months postoperatively, which reflects mechanical failure of repair rather than biological failure of tendon to bone healing. Iannotti et al.,14 in a multi-institutional study, had only one out of 19 retears diagnosed later than 6 months postoperatively.
Factors affecting retear rates
A large number of factors affect the rate of RRCT. Increasing patient age has been shown in multiple studies to have a negative impact on tendon healing. The risk of retear progressively increases with increasing age.15 Boileau et al.16 reported significantly lower rates of healing over the age of 65 years. Preoperative images and intraoperative arthroscopic findings can provide clues on the risk of retear. Retears are more likely with larger tears, higher degree of tendon retraction, shorter tendons and more severe fatty degeneration.15,17-19 The initial tear size is reported to be the most significant factor that affects tendon healing. The relative risk of retear increases 2.29 times with every 1 cm increase in tear size.15 Fatty degeneration is a powerful prognostic factor. More severe fatty degeneration has been associated with significantly higher retear rates.18 Liem et al. demonstrated higher retear rates with Goutallier stage 2 compared to stages 0 and 1.20 Length of tendon available for repair can also have a direct effect on success, with tendons of lengths more than 15 mm and less fatty infiltration showing better results.19 Radiologically, recent studies showed that high critical shoulder angle or short acromiohumeral interval increase the risk of retear17,21 (Figure 1). Quality of tendon and bone can also significantly influence healing. Bone mineral density was found to be an independent predictor of rotator cuff healing after repair.22 Finally, comorbidities of smoking and diabetes have detrimental effects on tendon healing.23 Neyton et al.24 reported significantly higher retear rates in smokers compared to nonsmokers (Table 1).
Figure 1.
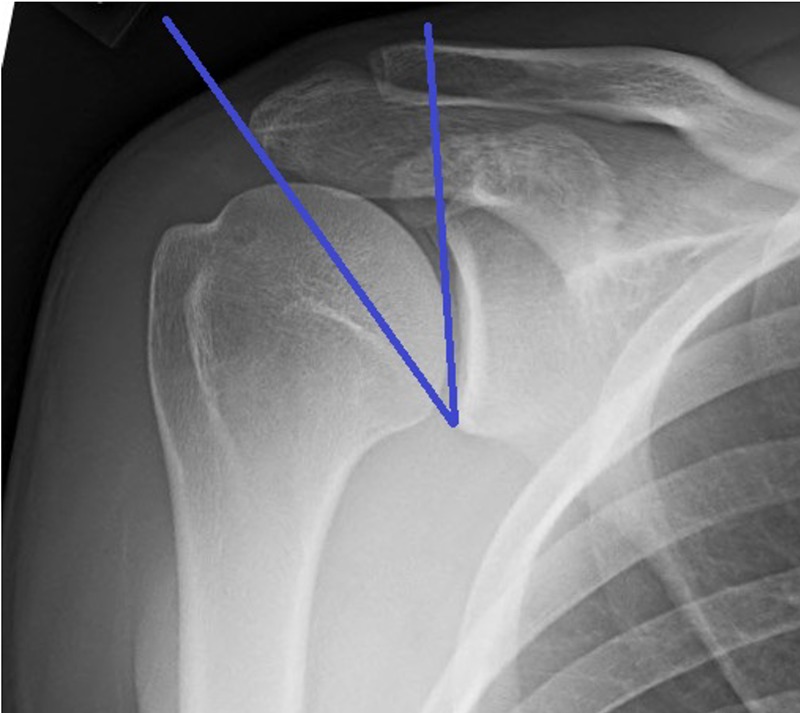
Critical shoulder angle: angle between the glenoid and lateral border of the acromion.
Table 1.
Preoperative factors affecting rotator cuff retear rates.
Effect of repair technique on rotator cuff retear
The effect of suture position and configuration on retear rates and patterns has been of particular concern. In SR repair, stitches should be positioned just medial to the rotator cable to decrease risk of cutout of the tendon.25 Passing sutures lateral or through the cable should be avoided. Double row (DR) repair provide better biomechanical properties compared to single row (SR) in terms of mechanical strength, gap formation, footprint coverage and tendon to bone contact that theoretically leads to improved healing response.26,27 The suture bridge (SB) technique can increase footprint coverage and mean pressurized contact area even more, with higher ultimate-to-load failure and less gap formation when compared to a DR technique (Figure 2).28,29 Also, inserting lateral row anchors away from the top of the greater tuberosity (more lateral) in SB technique potentially leaves more space on the footprint for the tendon to heal. Passing sutures through the lateral edge of the tendon, in DR technique, can be worrisome especially in chronic degenerative tears, whereas bridging sutures over the edge of the tendon, in SB technique, flattens and stabilizes the lateral edge and prevents the tear from catching on impinging structures. 28,30 Moreover tension mismatch during humeral rotation is less likely with SB owing to the interconnection between anchors.29
Figure 2.
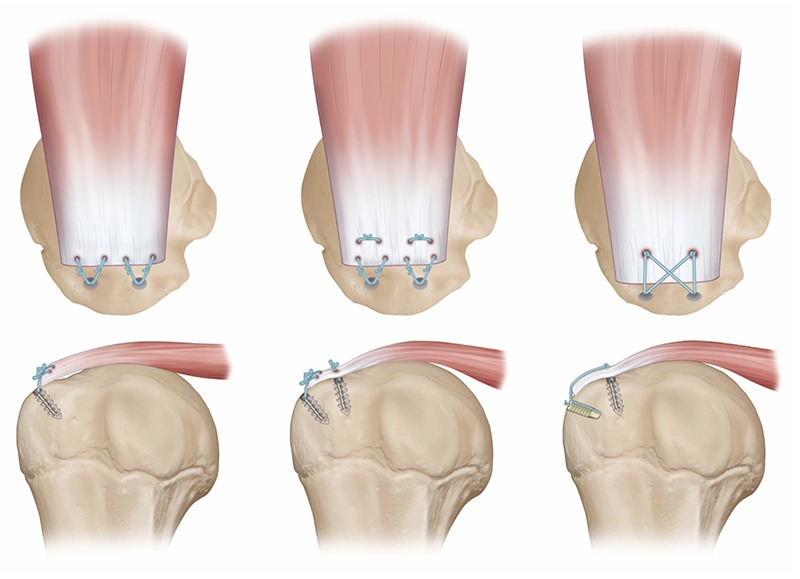
Techniques of rotator cuff repair (Single row, double row, suture bridge).
Suture bridge technique, however, is not without drawbacks. Although contact pressure might be beneficial for healing, it can reduce blood flow to the rotator cuff tendon.31 Stress concentration and increased risk of retears around the medial anchors have been great concerns since the introduction of DR and SB techniques. A few studies have demonstrated significantly higher rates of medial cuff failure after DR and SB techniques (Table 2).32-35 Therefore, it is clear that no technique is optimum in all situations, and the rate and pattern of retear varies according to the initial repair technique.
Table 2.
Rotator cuff retear patterns according to repair technique.
| Authors, year | N. retears | Type | SR (%) | SB (%) | K-SB (%) |
|---|---|---|---|---|---|
| Kim et al., 201441 | 65 | Type 1 | 15 (71.4) | 9 (40.9) | 12 (54.5) |
| Type 2 | 5 (23.8) | 13 (59.0) | 9 (40.9) | ||
| Type 3 | 1 (4.7) | 1 (4.5) | |||
| Lee et al., 201335 | 30 | Type 1 | 10 (33.3) | ||
| Type 2 | 20 (66.7) | ||||
| Cho et al., 201140 | 29 | Type 1 | 12 (41.4) | ||
| Type 2 | 17 (58.6) | ||||
| Cho et al., 201034 | 46 | Type 1 | 14 (73.7) | 7 (25.9) | |
| Type 2 | 5 (26.3) | 20 (74.1) |
SR: single row, DR: double row, SB: suture bridge, K-SB: knotless suture bridge. Type 1: retear at the tendon-bone interface, type 2: medial cuff failure, type 3: unclassified.. Studies included in the table are those reporting both repair technique and retear type, with total number of retears more than 20.
Effect on retear rates
The incidence of RRCT varies greatly. A systematic reviewed by Duquin et al.36 evaluated retear rates after different repair techniques. They analyzed the results according to the size of the initial tear to less the 1 cm, 1-3 cm, less than 3 cm, 3-5 cm, more than 3 cm and more than 5 cm. Retear rates were significantly lower for DR compared to SR in all tears more than 1 cm. Hein and colleagues,37 in a more recent systematic review, followed similar methods to evaluate retear rates after arthroscopic SR, DR and SB techniques. The overall retear rates were 26%, 21% and 21% respectively. Their study included 2048 rotator cuff retears. They reported significantly less retear rates after DR than SR techniques in all tear sizes except those between 3 and 5 cm. Retears after SB technique were also significantly less in all tear sizes except those less than 1 cm and between 3 and 5 cm. Our explanation to these results is that tears between 3 and 5 cm that are repaired arthroscopically might be small enough to get back to the footprint but large enough to be over-tensioned, in case they are anatomically repaired without adequate release. This potentially affects retear rates in DR and SB techniques more than it does in SR. Smaller tears are usually not much retracted and inadequate release may not have a significant negative impact, whereas in larger tears, adequate release is necessary, and not optional, in order to be able to get the tendon back to the footprint. In other words, tears between 3 and 5 cm might be the most vulnerable to repair with excessive tension. Recently, Sobhy et al.,38 in a systematic review of level I randomized controlled trials comparing SR and DR repairs, showed significantly higher partialthickness retear rates after SR compared to DR. However, the higher number of fullthickness retears after SR was not statistically significant. Despite the decreased overall retear rates with DR and SB compared to SR techniques, the opposite seems to be true in case of short tendons. Kim et al.39 observed retear rates after repair of larger than medium-sized tears (more than the entire supraspinatus). Retear rate was significantly higher with SB than SR in patients with remnant tendons less than 10 mm in length.
Effect on retear patterns
Cho et al.40 classified retear patterns as type 1 which is failure at the tendon-bone interface (Figure 3A), and type 2 which is medial cuff failure with remnant cuff remaining attached to the greater tuberosity (Figure 3B). Kim et al.41 added type 3 for unclassified patterns. Despite the decreased risk of overall retear rates with the introduction of DR and SB techniques, type 2 retears have evolved and have become more frequent than type 1.32-35,40-43
Figure 3.
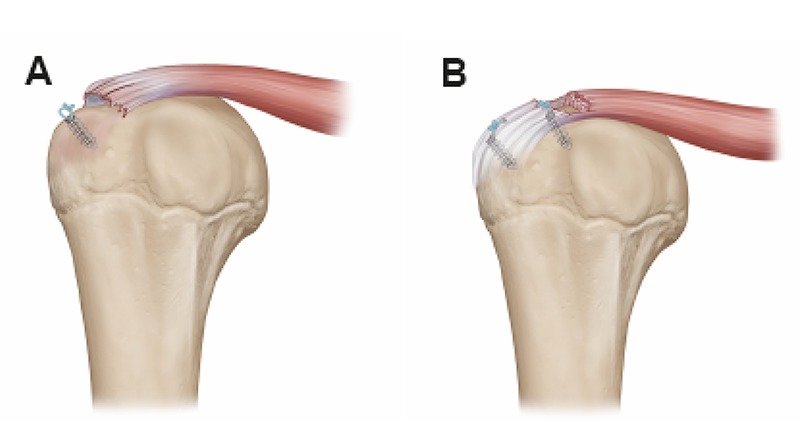
A) Type 1 rotator cuff retear; retear at the tendon-bone interface. B) Type 2 rotator cuff retear; medial cuff failure.
Medial cuff failure was not reported until Trantalis et al.32 recognized 5 cases of medial cuff failure after DR repair. Potential causes postulated for this retear pattern were (1) transferring the tension-bearing row more medial, (2) use of braided suture materials that are ultimately stronger than the diseased tendon and (3) oblique passage of instruments through the tendon which puts more tension on the medial cuff, creates larger holes in the tendon during passage, and compromises the overall integrity of the tendon. Hayashida et al.42 reported 7 type 2 out of a total of 13 retears after DR repair. Similarly, when reviewing the retear patterns after SB repair (Table 2), studies suggest that rotator cuff tears repaired with SB technique demonstrated type 2 retears in more than half of the retorn rotator cuffs.34,35,40,41 Two studies, each included more than 45 total retears, directly compared retear patterns according to repair technique.34,41 Both comparative studies showed significantly higher rates of type 2 retears in the SB than in the SR groups (Table 2).
The musculotendinous junction
The musculotendinous junction (MTJ), in particular, is a vulnerable point. Cho et al.34 reported 20 type 2 retears out of 27 total retears (74%) after SB repair, in which type 2 retears were mainly at the MTJ. Placing medial row sutures through the MTJ diminishes the holding strength and increases risk of failure compared to sutures placed through the tendon, 5 mm or 10 mm lateral to the MTJ.44,45 This is particularly important in chronic degenerative tears that often demonstrate tendon tissue loss and in revision cases. However, in patients with muscle atrophy and/or fatty degeneration, retears occur more often at the footprint because the tendon proper becomes mechanically weaker than the MTJ.34,40
Prevention of medial cuff failure
Despite the relative increase in type 2 retears with SB technique, Neyton et al.,24 in a study performed on 107 patients treated with SB technique, reported 10 type 1 retears and only one type 2 retear (Table 2). They explained their results with technical modifications that reduced the risk of type 2 retears. In their study, no more than 2 medial row anchors were used, with only one suture on each anchor. Medial row mattress sutures were not over-tensioned. These modifications decreased the amount of mattress sutures and limited the harmful compression that could form zones of necrosis across the footprint. They also penetrated the tendon 5 mm, or more, lateral to the MTJ.
Other strategies have been performed to decrease the stress concentration on medial row anchors, and thereby decrease the risk of medial strangulation and necrosis. Knotless suture bridge technique (K-SB) showed lower, but statistically insignificant, type 2 retears compared to conventional SB technique.41 Similarly, Tanaka and colleagues have demonstrated rotator cuff repair with absorbable sutures in the medial row anchors provided lower type 2 retears than what was previously reported by the same institution.42,46
Treatment options for medial cuff failure
Medial cuff failure poses significant revision challenges, owing to the shorter tendon remaining. Every possible effort should be undertaken to achieve adequate release of the tendon. Excessive tension to attach the torn tendon to the anatomic footprint can lead to failure of the repair and should be avoided.47,48 When tension-free repair is not possible, partial repair,49 interposition graft50 or medialization51 can be performed. Kim et al.51 demonstrated that a medialized repair is a simple and reliable procedure with good clinical results. Range of abduction is not compromised with medialization as long as medial advancement is not more than 10 mm.51,52
Treatment of rotator cuff retears
There is insufficient data in literature to formulate a clear algorithm for the appropriate management of re-torn rotator cuffs after arthroscopic repair.53 Several treatment options have been proposed, and the choice of treatment should be individualized for each patient.
Nonoperative management
Functional outcome has been correlated to rotator cuff integrity after repair.16 However, structural failure does not always lead to clinical failure54. Satisfactory clinical outcomes have been reported after longterm follow up of patients with re-torn rotator cuffs.54,55 In addition to favorable functional outcome, small retears could potentially heal.54
Revision rotator cuff repair
Functional and clinical outcomes are generally satisfactory after revision rotator cuff repair,56-58 but still inferior to primary repair, with twice the risk of failure.59 Shorter tendons and excess implant at the footprint render repair of RRCT more challenging. In cases with short tendons where one cannot pass the medial row sutures away from the MTJ, Barber recommended performing SR rather than a DR or a SB technique.60 Shamsudin et al.59 reported similar short-term clinical outcomes in revision and primary rotator cuff repair. However, structural failure at 2 years was twice as likely in revision rotator cuff repair. Appropriate patient selection can significantly affect results.57,61 Young active patients, with tendons that display good quality and adequate length, and those with traumatic retears are typical candidates for revision surgery. Poor prognostic factors include female sex and poor preoperative range of motion.57 Rotator cuff repair is not recommended in patients with disrupted deltoid origin and those who have had more than one prior cuff repair.62
Tendon augmentation grafts
Multiple natural and synthetic grafts have been used, demonstrating mixed results, to augment repair of massive rotator cuff tears. Barber et al.50 in a randomized controlled trial demonstrated higher healing rates and better ASES and constant scores with augmentation of repair using GraftJacket acellular human dermal matrix (Wright Medical Technology, Arlington, TN) compared to repair alone. Similarly, in a retrospective study on 152 patients with massive rotator cuff tears treated by open repair, augmentation of repair with synthetic polypropylene patch (Repol Angimesh, ANGIOLOGICA BM Srl, Pavia, Italy) showed lower retear rate and better UCLA scores, elevation in the scapular plane and abduction strength.63 Xenografts, however, do not seem to be as efficient. A randomized controlled trial compared augmentation of repair with porcine small intestine mucosa to repair without augmentation failed to show significant differences in functional outcomes or healing rates.64 Favorable healing rates have also been reported with polyester ligament synthetic graft,65 as well as biceps tendon66 and fascia lata autografts.67 The latter studies, however, are retrospective studies with less number of patients.
Superior capsular reconstruction
Superior capsular reconstruction is also a potential treatment option for revision procedures. Mihata et al.68 reported favorable outcomes after arthroscopic superior capsular reconstruction using fascia lata for patients with irreparable cuff tears, with significant improvement in ASES scores. Dermal allograft is another option for capsular reconstruction with less morbidity and shorter operative time. A recent multicenter study performed on 59 patients with irreparable cuff tears showed promising results after arthroscopic superior capsular reconstruction with dermal allograft.69 Added cost, however, is a limitation of dermal allograft compared to fascia lata.
Salvage procedures
Tendon transfer can be a treatment option for irreparable cuff tears without arthritis, particularly in young patients in which arthoplasty is not preferred. The location of the tear significantly influence the surgeon’s choice of the donor tendon. For posterosuperior tears, good outcomes have been reported with both Latissimus dorsi (LD) and lower trapezius as donor tendons.70,71 Lower trapezius is a biomechanically better option because the direction of pull of the lower trapezius is more in line with the native rotator cuff than that of LD. For anterosuperior tears, pectoralis major transfer has been traditionally performed providing improvement in functional outcomes and reducing pain.72,73 However, poor outcomes have been reported in patients with anterior subluxation of the humeral head.74 Latissimus dorsi transfer to the subscapularis insertion is another option that provides a more anatomic transfer owing to the more posterior origin of LD compared to pectoralis major. Latissimus dorsi is more in line with the origin of the subscapularis, therefore more effectively bringing back the humeral head to the center around the glenoid.75 Elhassan et al.75 described the feasibility of the latter procedure with or without teres major transfer.
Insertion of a biodegradable spacer (balloon) arthroscopically into the subacromial space is a simple procedure that can relieve pain and improve shoulder function. Satisfactory short term outcomes that are comparable to other salvage procedures have been reported.76 This procedure is advantageous over other salvage procedure in being less invasive with minimal morbidity. Long term results, however, are not yet available in literature.
Reverse total shoulder arthroplasty (RTSA) can be considered a true salvage procedure in patients with RRCTs. Indications for RTSA in rotator cuff disease are cuff tear arthropathy and chronic pseudoparalysis with a massive rotator cuff tear with or without arthritis.77-79 Persistent pseudoparalysis, irreparable tears of the rotator cuff, and glenohumeral arthritis after rotator cuff repair are best managed with RTSA.80-82 Reverse total shoulder arthroplasty has been proven to be more cost effective than revision rotator cuff repair in patients with pseudoparalysis without arthritis.83 Excellent results can be achieved with proper patient selection. Good deltoid function is necessary for the success of RTSA. Bacle et al.84 reported 93% prosthetic survival rate after 10-year follow-up, using revision as the end point. RTSA is not recommended, after rotator cuff repair, in a painful shoulder with greater than 90 degrees of preoperative active anterior elevation77,81 (Table 3).
Table 3.
Factors influencing the decision to perform reverse total shoulder arthroplasty for recurrent rotator cuff tears.
| RTSA recommended | RTSA not recommended |
|---|---|
| Good deltoid function | Poor deltoid function |
| Persistent pseudoparalysis | Axillary nerve injury |
| Irreparable rotator cuff tears | Painful shoulder with good active anterior elevation |
| Rotator cuff arthropathy |
RTSA: reverse total shoulder arthroplasty.
Conclusions
Repair technique significantly affects rotator cuff retear rate and pattern after arthroscopic repair. Medial cuff failure is gaining more attention in clinical practice and the literature. Although DR and SB techniques decrease the overall rates of retears, the increased risk of medial cuff failure theoretically poses significant revision challenges. Therefore, retear patterns, in addition to retear rates, should be considered when evaluating the outcomes of different techniques of repair. Studies with long term follow up are needed to demonstrate which outcomes are better; less retears that are mostly type 2, or more retears that are predominantly type 1.
Funding Statement
Funding: none.
References
- 1.Yamamoto A, Takagishi K, Osawa T, et al. Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 2010;19:116-20. [DOI] [PubMed] [Google Scholar]
- 2.Voigt C, Bosse C, Vosshenrich R, et al. Arthroscopic supraspinatus tendon repair with suture-bridging technique. Am J Sports Med 2010;38:983-91. [DOI] [PubMed] [Google Scholar]
- 3.Park JY, Lhee SH, Oh KS, et al. Clinical and ultrasonographic outcomes of arthroscopic suture bridge repair for massive rotator cuff tear. Arthroscopy 2013;29:280-9. [DOI] [PubMed] [Google Scholar]
- 4.Yang J, Robbins M, Reilly J, et al. The clinical effect of a rotator cuff retear: a meta-analysis of arthroscopic singlerow and double-row repairs. Am J Sports Med 2017;45:733-741. [DOI] [PubMed] [Google Scholar]
- 5.Angeline ME, Rodeo SA. Biologics in the Management of Rotator Cuff Surgery. Clin Sports Med 2012;31:645-63. [DOI] [PubMed] [Google Scholar]
- 6.St Pierre P, Olson EJ, Elliott JJ, et al. Tendon-healing to cortical bone compared with healing to a cancellous trough. A biomechanical and histological evaluation in goats. J Bone Joint Surg Am 1995;77:1858-66. [DOI] [PubMed] [Google Scholar]
- 7.Kovacevic D, Fox AJ, Bedi A, et al. Calcium-Phosphate Matrix With or Without TGF-β3 Improves Tendon- Bone Healing After Rotator Cuff Repair. Am J Sports Med 2011;39:811-9. [DOI] [PubMed] [Google Scholar]
- 8.Ide J, Kikukawa K, Hirose J, et al. The effects of fibroblast growth factor-2 on rotator cuff reconstruction with acellular dermal matrix grafts. Arthroscopy 2009;25:608-16. [DOI] [PubMed] [Google Scholar]
- 9.Kovacevic D, Rodeo SA. Biological Augmentation of Rotator Cuff Tendon Repair. Clin Orthop Relat Res 2008;466:622-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barber FA, Hrnack SA, Snyder SJ, Hapa O. Rotator Cuff Repair Healing Influenced by Platelet-Rich Plasma Construct Augmentation. Arthroscopy 2011;27:1029-35. [DOI] [PubMed] [Google Scholar]
- 11.Rodeo SA, Delos D, Williams RJ, et al. The Effect of Platelet-Rich Fibrin Matrix on Rotator Cuff Tendon Healing. Am J Sports Med 2012;40:1234-41. [DOI] [PubMed] [Google Scholar]
- 12.Castricini R, Longo UG, De Benedetto M, et al. Platelet-Rich Plasma Augmentation for Arthroscopic Rotator Cuff Repair. Am J Sports Med 2011;39:258-65. [DOI] [PubMed] [Google Scholar]
- 13.Miller BS, Downie BK, Kohen RB, et al. When Do Rotator Cuff Repairs Fail? Serial Ultrasound Examination After Arthroscopic Repair of Large and Massive Rotator Cuff Tears. Am J Sports Med 2011;39:2064-70. [DOI] [PubMed] [Google Scholar]
- 14.Iannotti JP, Deutsch A, Green A, et al. Time to Failure After Rotator Cuff Repair: A Prospective Imaging Study. J Bone Jt Surg 2013;95:965-71. [DOI] [PubMed] [Google Scholar]
- 15.Nho SJ, Brown BS, Lyman S, et al. Prospective analysis of arthroscopic rotator cuff repair: Prognostic factors affecting clinical and ultrasound outcome. J Shoulder Elbow Surg 2009;18:13-20. [DOI] [PubMed] [Google Scholar]
- 16.Boileau P, Brassart N, Watkinson DJ, et al. Arthroscopic Repair of Full- Thickness Tears of the Supraspinatus: Does the Tendon Really Heal? J Bone Joint Surg 2005;87:1229. [DOI] [PubMed] [Google Scholar]
- 17.Shin YK, Ryu KN, Park JS, et al. Predictive Factors of Retear in Patients With Repaired Rotator Cuff Tear on Shoulder MRI. Am J Roentgenol 2018;210:134-41. [DOI] [PubMed] [Google Scholar]
- 18.Yi JW, Cho NS, Cho SH, Rhee YG. Arthroscopic Suture Bridge Repair Technique for Full Thickness Rotator Cuff Tear. Clin Orthop Surg 2010;2:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer DC, Wieser K, Farshad M, Gerber C. Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med 2012;40:2242-7. [DOI] [PubMed] [Google Scholar]
- 20.Liem D, Lichtenberg S, Magosch P, Habermeyer P. Magnetic Resonance Imaging of Arthroscopic Supraspinatus Tendon Repair. J Bone Jt Surg. 2007;89:1770-6. [DOI] [PubMed] [Google Scholar]
- 21.Garcia GH, Liu JN, Degen RM, et al. Higher critical shoulder angle increases the risk of retear after rotator cuff repair. J Shoulder Elbow Surg 2017;26:241-5. [DOI] [PubMed] [Google Scholar]
- 22.Chung SW, Oh JH, Gong HS, et al. Factors Affecting Rotator Cuff Healing After Arthroscopic Repair. Am J Sports Med 2011;39:2099-107. [DOI] [PubMed] [Google Scholar]
- 23.Abtahi AM, Granger EK, Tashjian RZ. Factors affecting healing after arthroscopic rotator cuff repair. World J Orthop 2015;6:211-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Neyton L, Godenèche A, Nové-Josserand L, et al. Arthroscopic suturebridge repair for small to medium size supraspinatus tear: healing rate and retear pattern. Arthroscopy 2013;29:10-7. [DOI] [PubMed] [Google Scholar]
- 25.Wieser K, Rahm S, Farshad M, et al. Stitch positioning influences the suture hold in supraspinatus tendon repair. Knee Surg Sports Traumatol Arthrosc 2013;21:1587-92. [DOI] [PubMed] [Google Scholar]
- 26.Mazzocca AD, Millett PJ, Guanche CA, et al. Arthroscopic Single-Row Versus Double-Row Suture Anchor Rotator Cuff Repair. Am J Sports Med 2005;33:1861-8. [DOI] [PubMed] [Google Scholar]
- 27.Kim DH, ElAttrache NS, Tibone JE, et al. Biomechanical Comparison of a Single-Row Versus Double-Row Suture Anchor Technique for Rotator Cuff Repair. Am J Sports Med 2006;34:407-14. [DOI] [PubMed] [Google Scholar]
- 28.Park MC, El Attrache NS, Tibone JE, et al. Part I: Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg 2007;16:461-8. [DOI] [PubMed] [Google Scholar]
- 29.Park MC, Tibone JE, ElAttrache NS, et al. Part II: Biomechanical assessment for a footprint-restoring transosseousequivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg 2007;16:469-76. [DOI] [PubMed] [Google Scholar]
- 30.Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy 1994;10:4-19. [DOI] [PubMed] [Google Scholar]
- 31.Christoforetti JJ, Krupp RJ, Singleton SB, et al. Arthroscopic suture bridge transosseus equivalent fixation of rotator cuff tendon preserves intratendinous blood flow at the time of initial fixation. J Shoulder Elbow Surg 2012;21:523-30. [DOI] [PubMed] [Google Scholar]
- 32.Trantalis JN, Boorman RS, Pletsch K, Lo IKY. Medial Rotator Cuff Failure After Arthroscopic Double-Row Rotator Cuff Repair. Arthroscopy 2008;24:727-31. [DOI] [PubMed] [Google Scholar]
- 33.Yamakado K, Katsuo S, Mizuno K, et al. Medial-Row Failure After Arthroscopic Double-Row Rotator Cuff Repair. Arthroscopy 2010;26:430-5. [DOI] [PubMed] [Google Scholar]
- 34.Cho NS, Yi JW, Lee BG, Rhee YG. Retear Patterns After Arthroscopic Rotator Cuff Repair: Single-row Versus Suture Bridge Technique. Am J Sports Med 2010;38:664-71. [DOI] [PubMed] [Google Scholar]
- 35.Lee KW, Seo DW, Bae KW, Choy WS. Clinical and Radiological Evaluation after Arthroscopic Rotator Cuff Repair Using Suture Bridge Technique. Clin Orthop Surg 2013;5:306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Duquin TR, Buyea C, Bisson LJ. Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med 2010;38:835-41. [DOI] [PubMed] [Google Scholar]
- 37.Hein J, Reilly JM, Chae J, et al. Retear Rates After Arthroscopic Single-Row, Double-Row, and Suture Bridge Rotator Cuff Repair at a Minimum of 1 Year of Imaging Follow-up: A Systematic Review. Arthroscopy 2015;31:2274-81. [DOI] [PubMed] [Google Scholar]
- 38.Sobhy MH, Khater AH, Hassan MR, El Shazly O. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol 2018. doi:10.1007/s00590-018-2145-7. [DOI] [PubMed] [Google Scholar]
- 39.Kim YK, Moon SH, Cho SH. Treatment Outcomes of Single- Versus Double- Row Repair for Larger Than Medium- Sized Rotator Cuff Tears. Am J Sports Med 2013;41:2270-7. [DOI] [PubMed] [Google Scholar]
- 40.Cho NS, Lee BG, Rhee YG. Arthroscopic Rotator Cuff Repair Using a Suture Bridge Technique: Is the Repair Integrity Actually Maintained. Am J Sports Med 2011;39:2108-16. [DOI] [PubMed] [Google Scholar]
- 41.Kim KC, Shin HD, Cha SM, Park JY. Comparisons of Retear Patterns for 3 Arthroscopic Rotator Cuff Repair Methods. Am J Sports Med 2014;42:558-65. [DOI] [PubMed] [Google Scholar]
- 42.Hayashida K, Tanaka M, Koizumi K, Kakiuchi M. Characteristic retear patterns assessed by magnetic resonance imaging after arthroscopic double-row rotator cuff repair. Arthroscopy 2012;28:458-64. [DOI] [PubMed] [Google Scholar]
- 43.Gerhardt C, Hug K, Pauly S, et al. Arthroscopic Single-Row Modified Mason-Allen Repair Versus Double- Row Suture Bridge Reconstruction for Supraspinatus Tendon Tears. Am J Sports Med 2012;40:2777-85. [DOI] [PubMed] [Google Scholar]
- 44.Virk MS, Bruce B, Hussey KE, et al. Biomechanical Performance of Medial Row Suture Placement Relative to the Musculotendinous Junction in Transosseous Equivalent Suture Bridge Double-Row Rotator Cuff Repair. Arthroscopy 2017;33:242-50. [DOI] [PubMed] [Google Scholar]
- 45.Kullar RS, Reagan JM, Kolz CW, et al. Suture placement near the musculotendinous junction in the supraspinatus: implications for rotator cuff repair. Am J Sports Med 2015;43:57-62. [DOI] [PubMed] [Google Scholar]
- 46.Tanaka M, Hayashida K, Kobayashi A, Kakiuchi M. Arthroscopic Rotator Cuff Repair With Absorbable Sutures in the Medial-Row Anchors. Arthroscopy 2015;31:2099-105. [DOI] [PubMed] [Google Scholar]
- 47.Hersche O, Gerber C. Passive tension in the supraspinatus musculotendinous unit after long-standing rupture of its tendon: a preliminary report. J Shoulder Elbow Surg 1998;7:393-6. [DOI] [PubMed] [Google Scholar]
- 48.Reilly P, Bull AMJ, Amis AA, et al. Passive tension and gap formation of rotator cuff repairs. J Shoulder Elbow Surg 2018;13:664-7. [DOI] [PubMed] [Google Scholar]
- 49.Duralde XA, Bair B. Massive rotator cuff tears: The result of partial rotator cuff repair. J Shoulder Elbow Surg 2005;14:121-7. [DOI] [PubMed] [Google Scholar]
- 50.Barber FA, Burns JP, Deutsch A, et al. A prospective, randomized evaluation of acellular human dermal matrix augmentation for arthroscopic rotator cuff repair. Arthroscopy 2012;28:8-15. [DOI] [PubMed] [Google Scholar]
- 51.Kim YK, Jung KH, Won JS, Cho SH. Medialized repair for retracted rotator cuff tears. J Shoulder Elbow Surg 2017;26:1432-40. [DOI] [PubMed] [Google Scholar]
- 52.Yamamoto N, Itoi E, Tuoheti Y, et al. Glenohumeral joint motion after medial shift of the attachment site of the supraspinatus tendon: a cadaveric study. J Shoulder Elbow Surg 2007;16:373-8. [DOI] [PubMed] [Google Scholar]
- 53.Lädermann A, Denard PJ, Burkhart SS. Management of failed rotator cuff repair: a systematic review. J ISAKOS Jt Disord Orthop Sport Med 2016;1:32-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jost B, Zumstein M, Pfirrmann CWA, Gerber C. Long-Term Outcome After Structural Failure of Rotator Cuff Repairs. J Bone Jt Surg 2006;88:472. [DOI] [PubMed] [Google Scholar]
- 55.Paxton ES, Teefey SA, Dahiya N, et al. Clinical and radiographic outcomes of failed repairs of large or massive rotator cuff tears: minimum ten-year followup. J Bone Joint Surg Am 2013;95:627-32. [DOI] [PubMed] [Google Scholar]
- 56.Keener JD, Wei AS, Kim HM, et al. Revision Arthroscopic Rotator Cuff Repair: Repair Integrity and Clinical Outcome. J Bone Joint Surg Am 2010;92:590-8. [DOI] [PubMed] [Google Scholar]
- 57.Lädermann A, Denard PJ, Burkhart SS. Midterm outcome of arthroscopic revision repair of massive and nonmassive rotator cuff tears. Arthroscopy 2011;27:1620-7. [DOI] [PubMed] [Google Scholar]
- 58.Chuang MJ, Jancosko J, Nottage WM. Clinical outcomes of single-row arthroscopic revision rotator cuff repair. Orthopedics 2014;37:e692-8. [DOI] [PubMed] [Google Scholar]
- 59.Shamsudin A, Lam PH, Peters K, et al. Revision Versus Primary Arthroscopic Rotator Cuff Repair. Am J Sports Med 2015;43:557-64. [DOI] [PubMed] [Google Scholar]
- 60.Barber FA. Editorial Commentary: Musculotendinous Junction Mattress Sutures Are Inefficient. Arthroscopy 2017;33:251-3. [DOI] [PubMed] [Google Scholar]
- 61.Lo IK., Burkhart SS. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy 2004;20:250-67. [DOI] [PubMed] [Google Scholar]
- 62.Djurasovic M, Marra G, Arroyo JS, et al. Revision rotator cuff repair: factors influencing results. J Bone Joint Surg Am 2001;83A:1849-55. [DOI] [PubMed] [Google Scholar]
- 63.Ciampi P, Scotti C, Nonis A, et al. The Benefit of Synthetic Versus Biological Patch Augmentation in the Repair of Posterosuperior Massive Rotator Cuff Tears. Am J Sports Med 2014;42:1169-75. [DOI] [PubMed] [Google Scholar]
- 64.Iannotti JP, Codsi MJ, Kwon YW, et al. Porcine small intestine submucosa augmentation of surgical repair of chronic two-tendon rotator cuff tears. A randomized, controlled trial. J Bone Joint Surg Am 2006;88:1238-44. [DOI] [PubMed] [Google Scholar]
- 65.Nada AN, Debnath UK, Robinson DA, Jordan C. Treatment of massive rotatorcuff tears with a polyester ligament (Dacron) augmentation: clinical outcome. J Bone Jt Surg Br 2010;92:1397-402. [DOI] [PubMed] [Google Scholar]
- 66.Sano H, Mineta M, Kita A, Itoi E. Tendon patch grafting using the long head of the biceps for irreparable massive rotator cuff tears. J Orthop Sci 2010;15:310-6. [DOI] [PubMed] [Google Scholar]
- 67.Mori D, Funakoshi N, Yamashita F. Arthroscopic Surgery of Irreparable Large or Massive Rotator Cuff Tears With Low-Grade Fatty Degeneration of the Infraspinatus: Patch Autograft Procedure Versus Partial Repair Procedure. Arthroscopy 2013;29:1911-21. [DOI] [PubMed] [Google Scholar]
- 68.Mihata T, Lee TQ, Watanabe C, et al. Clinical Results of Arthroscopic Superior Capsule Reconstruction for Irreparable Rotator Cuff Tears. Arthroscopy 2013;29:459-70. [DOI] [PubMed] [Google Scholar]
- 69.Denard PJ, Brady PC, Adams CR, et al. Preliminary Results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy 2018;34:93-9. [DOI] [PubMed] [Google Scholar]
- 70.Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior- superior rotator cuff tear. J Shoulder Elbow Surg 2016;25:1346-53. [DOI] [PubMed] [Google Scholar]
- 71.Gerber C, Rahm SA, Catanzaro S, et al. Latissimus Dorsi Tendon Transfer for Treatment of Irreparable Posterosuperior Rotator Cuff Tears. J Bone Joint Surg Am 2013;95:1920-6. [DOI] [PubMed] [Google Scholar]
- 72.Gavriilidis I, Kircher J, Magosch P, et al. Pectoralis major transfer for the treatment of irreparable anterosuperior rotator cuff tears. Int Orthop 2010;34:689-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Resch H, Povacz P, Ritter E, Matschi W. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J Bone Joint Surg Am 2000;82:372-82. [DOI] [PubMed] [Google Scholar]
- 74.Elhassan B, Ozbaydar M, Massimini D, et al. Transfer of pectoralis major for the treatment of irreparable tears of subscapularis: does it work? J Bone Joint Surg Br 2008;90B:1059-65. [DOI] [PubMed] [Google Scholar]
- 75.Elhassan B, Christensen TJ, Wagner ER. Feasibility of latissimus and teres major transfer to reconstruct irreparable subscapularis tendon tear: an anatomic study. J Shoulder Elbow Surg 2014;23:492-9. [DOI] [PubMed] [Google Scholar]
- 76.Senekovic V, Poberaj B, Kovacic L, et al. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatol 2013;23:311-6. [DOI] [PubMed] [Google Scholar]
- 77.Drake GN, O’Connor DP, Edwards TB. Indications for Reverse Total Shoulder Arthroplasty in Rotator Cuff Disease. Clin Orthop Relat Res 2010;468:1526-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wall B, Nové-Josserand L, O’Connor DP, et al. Reverse Total Shoulder Arthroplasty: A Review of Results According to Etiology. J Bone Joint Surg 2007;89:1476. [DOI] [PubMed] [Google Scholar]
- 79.Neri BR, Chan KW, Kwon YW. Management of massive and irreparable rotator cuff tears. J Shoulder Elbow Surg 2009;18:808-18. [DOI] [PubMed] [Google Scholar]
- 80.Denard PJ, Lädermann A, Jiwani AZ, Burkhart SS. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy 2012;28:1214-9. [DOI] [PubMed] [Google Scholar]
- 81.Boileau P, Gonzalez JF, Chuinard C, et al. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg 2009;18:600-6. [DOI] [PubMed] [Google Scholar]
- 82.Sirveaux F, Favard L, Oudet D, et al. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 2004;86:388-95. [DOI] [PubMed] [Google Scholar]
- 83.Dornan GJ, Katthagen JC, Tahal DS, et al. Cost-Effectiveness of Arthroscopic Rotator Cuff Repair Versus Reverse Total Shoulder Arthroplasty for the Treatment of Massive Rotator Cuff Tears in Patients With Pseudoparalysis and Nonarthritic Shoulders. Arthroscopy 2017;33:716-25. [DOI] [PubMed] [Google Scholar]
- 84.Bacle G, Nové-Josserand L, Garaud P, Walch G. Long-Term Outcomes of Reverse Total Shoulder Arthroplasty. J Bone Joint Surg 2017;99:454-61. [DOI] [PubMed] [Google Scholar]


