Abstract
We argue that research on political behavior, including political participation, public opinion, policy responsiveness, and political inequality will be strengthened by studying the role of health. We then provide evidence that health matters for voter turnout and partisanship. Using the General Social Survey (GSS) and The National Longitudinal Study of Adolescent Health (Add Health), we find that people who report poor health are less likely to vote and identify with the Republican Party. Moreover, the effects of health on voter turnout and partisanship appear to have both developmental and contemporaneous components. Taken together, our findings suggest that health inequalities may have significant political consequences.
This article has two central goals. The first one is to argue that research on political behavior, including political participation, public opinion, political inequality and policy responsiveness will be strengthened by studying the role of health. Theorizing about how health is related to political behavior is a formidable task since it requires integrating literatures from political science, sociology, psychology, and public health to generate new theories that link health conditions and risk behaviors to political behavior. In addition, empirically testing hypotheses requires innovative research designs since existing surveys (e.g., the National Election Survey or the Behavioral Risk Factor Surveillance Survey) often do not have extensive measures on health outcomes and political behavior.
The second goal is to provide evidence, albeit preliminary, that health matters for voter turnout and partisanship. The evidence we gather supports the argument that even if the relationship is not overwhelming, it is not weaker than that found between political behavior and more commonly studied individual characteristics. In addition, as we argue below, incorporating health into our studies may illuminate the link between important covariates, such as educational attainment, and political behavior since it often originates in early childhood prior to political socialization (Palloni 2005). Health is also pivotal to the aging experience (Ferraro 2006); integrating health into our studies of political behavior may help clarify the relationship between aging, political participation (e.g., Shields et al. 1998), and political preferences. Health may also be a potential mechanism by which biology influences political behavior since it is genetically transmitted (National Research Council 2000) and related to biomarkers, such as cortisol the biomarker of the stress response (Hajat et al. 2010), and personality factors, such as conscientiousness (Rhodes and Smith 2006), that impact political participation and preferences (Mondak 2010).
We are certainly not the first to consider the impact of physical health on political behavior. Schur and colleagues, for instance, have several articles documenting that individuals with disabilities are less likely to register and vote (Schur and Kruse 2000; Schur and Kruse 2002; Schur et al. 2002), tend to identify with the Democratic Party, and favor a greater government role in healthcare (Schur and Adya 2012). These studies are important first steps, although we argue that systematic comparative research on the impact of health on political behavior is in its infancy (but, see Mattila et al. 2013). As we suggest below, scholars would benefit from conceptualizing health as a multidimensional concept beyond physical disability.
The macro-implications of our findings are twofold. First, our results suggest that health inequalities may have significant political consequences. Compared to the unhealthy, if healthy people are more likely to turnout and have systematically different policy preferences or predispositions, as we suggest, then electoral results and the policies that are enacted may have a “health bias.” Second, health policies aimed at improving the health of the nation, such as universal healthcare, may contribute to a more politically active and engaged society. Policymakers interested in increasing the turnout of the electorate, particularly among the disadvantaged, should consider interventions aimed at decreasing or eliminating health disparities.
WHAT IS HEALTH?
Health is a multidimensional concept that encompasses both physical and mental aspects of well-being with various origins, trajectories, and consequences, making it difficult to conceptualize and measure. For instance, physical aspects of health include viral and bacterial infections that may impair early growth; exposure to and contraction of illnesses that may be acute, such as the common cold, or chronic, such as asthma; and repeated exposures to illnesses, which may have interactive effects across the lifespan (Palloni 2005). Physical disabilities and limitations, including hearing and vision impairments, as well as physical frailty, general fitness levels, and nutritional intake also constitute health. Mental aspects of health include not just extreme mental or cognitive impairments, but also depression, dysfunctional behavioral styles, levels of energy and alertness, the adoption of motivations and aspirations, personality disorders, and assessments of self-esteem (Palloni 2005). Health conditions may originate in utero as a response to the hormonal environment or toxins, develop in early childhood or adolescence (e.g., youth diabetes), have temporary effects (e.g., the flu), persist across the lifespan (e.g., disability), or change throughout the lifecycle (e.g., obesity). Finally, exposure to detrimental conditions may depend on external factors, such as maternal behavior during pregnancy, environments experienced at home or work, peer groups in schools, and doctors and caretakers at health facilities.
We define health as an enduring self-concept of general well-being, as opposed to a spontaneous health assessment (Boardman 2006). Empirically, we use self-rated health status (SRHS) which asks respondents “in general, how is your health?” with five allowable responses of excellent, very good, good, fair, and poor.1 While not uncontroversial (see Huisman and Deeg 2010), SRHS is a valid indicator of health because it is related to objective measures of mortality (Jylha 2009) as well health conditions such as coronary heart disease, cancer, and physical functioning (Bjorner et al. 2005). SRHS is also related to health service use (Angel and Gronfein 1988) and is a better predictor of mortality than physican-rated health (Markides et al. 1993). Some even claim that “an individual’s health status cannot be assessed without” SRHS and that this single item captures “an irreplaceable dimension of health status” (Idler and Benyamini 1997 34).
Conceptually, our definition of health is broader than others, such as disability or mental capacity, making it more relevant to a range of political processes. First, unlike disability or mental capacity, our definition of health originates in early childhood (Palloni 2005); consequently adolescent health is an important pre-adult force that may impact trajectories of participation and preferences that persist across the lifespan. Second, our conception of health status is transmitted across generations (National Research Council 2000) lending itself to studying the cycle of political inequality that persists across generations due to genetic, environmental, and societal factors. Third, our definition of health is related to health trajectories across the lifespan (Ferraro 2006), often reflecting how an individual’s health is changing. As a consequence, SRHS is a useful concept to explore changes in political behavior that occurs across the lifecycle as people age and have life experiences.
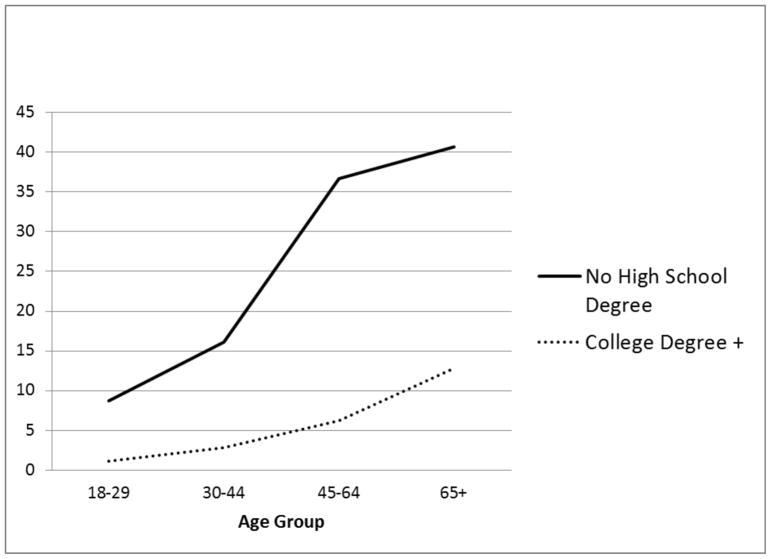
Most importantly, our definition of health is highly correlated with macro-social forces, such as socioeconomic status, poverty, race, family structure, and neighborhood characteristics (Palloni 2005) that likely matter for political behavior and public opinion. In fact, much of the public health literature has worked to understand and explain the link between health and socioeconomic status, also known as the “health gradient” (e.g., Lantz et al. 1998). Figure 1 shows an example of the health gradient by plotting the percentage of individuals with poor or fair SRHS across age and educational attainment using the 2011 National Health Interview Survey.2 As shown in Figure 1, health disparities across educational attainment exist in young adulthood and widen across the life course so that at age 65+ those without a high school degree are about 3 times as likely to report being in poor or fair health compared to those with a college degree or higher.3 This pattern is consistent with data from at least the 1970s (Elo and Preston 1996) and exists across various measures of health including nutritional status (Miller and Korenman 1994), diet (Dubois and Girard 2001), cardiovascular disease (Marmot et al. 1991), and mortality rates (Palloni 2005). The health gradient is present regardless of how socioeconomic status is measured, for instance, using maternal education, maternal income, or permanent income (Palloni 2005) and is evident in childhood, by some accounts as early as infancy (Braveman et al. 2010).
Figure 1.
Percentage with Poor or Fair Self-Rated Health, by Education and Age, NHIS 2011
Given the strong and positive relationship between health and socioeconomic status, public health scholars, the Centers for Disease Control, and the World Health Organization now characterize health as having strong social determinants. Health is not just shaped by individual behavior or exposure to risk, but also the conditions in which people are born, grow, live, work, and age (Marmot and Wilkinson 2009). Consequently, a research paradigm has emerged exploring health disparities across race and ethnicity (e.g., Morenoff and Lynch 2004), gender (e.g., Sen and Ostlin 2007), and neighborhood characteristics (e.g., Diez-Roux 2001), among other things.
The fact that health is socially patterned, much like political voice and power (Schlozman, Verba, and Brady 2012), has implications for the study of political behavior and political inequality more broadly. At the very least, health may be part of the individual political disadvantage that scholars traditionally measure through socioeconomic status (Brady et al. 1995). For instance, health may be related to politically relevant resources simply because of socioeconomic status. In our analyses below, however, we find that while socioeconomic status remains an important determinant of voting (1) poor health has a deleterious effect on adult and youth voter turnout; (2) this effect is direct and unmediated by socioeconomic status; and (3) this effect has both contemporaneous and developmental components, suggesting that poor health contributes to a cycle of political or civic disadvantage that is transmitted across generations. Hence, it appears from our analyses that the relationship between health and voter turnout is not spurious due to socioeconomic status. In the next section, we suggest potential theoretical pathways that link health to political participation and report our empirical results from analyses using the General Social Survey (GSS) and The National Longitudinal Study of Adolescent Health (Add Health).
CONCEPTUALLY LINKING HEALTH TO POLITICAL PARTICIPATION
How might health influence political participation? We offer four potential theoretical pathways linking health to political participation drawing from the extensive literature on the individual determinants of political participation.4 These pathways include resources, motivation, social support, and mobilization.
Resources
A large body of research suggests that varying levels of participation are due to individual differences in politically relevant resources, such as civic skills, time, money, and political knowledge, which are highly correlated with socioeconomic status (Verba et al. 1995). Education is arguably the most important and consistently documented resource that encourages political participation, both among youths (Plutzer 2002) and adults (Verba et al. 1995). After decades of research, however, political scientists question whether education has a direct, causal impact on participation or whether pre-adult forces, such as cognitive ability or personality traits, account for the positive relationship between education and political participation in adulthood (e.g., Kam and Palmer 2008).
Interestingly, many of the same pre-adult factors that may account for the spurious relationship between educational attainment and political participation correlate highly with childhood health. Large bodies of research show that child health is related to early cognitive ability, which is strongly correlated with adult cognitive performance and eventual socioeconomic status (e.g., O’Brien Caughy 1996). Michael (2004) shows that birth weight is positively associated with cognitive test scores, even in the presence of controls for parental resources. Cognitive ability also predicts higher educational attainment (Pallas 2000) and may be associated with increased political interest (Cacioppo et al. 1996).
We also know a great deal about the relationship between health and the Big Five—openness to experience, conscientiousness, extraversion, agreeableness, and neuroticism—with many finding that these traits are related to risk-taking behaviors, which impact health. Adults who are score high on the openness to experience trait are more likely to drink alcohol, drink and drive, and smoke (Booth-Kewley and Vickers 1994). On the other hand, people who score high on the conscientious dimension tend to be risk adverse, which translates into a healthy lifestyle (Booth-Kewley and Vickers 1994) with increased physical activity (Rhodes and Smith 2006) and fitness (Hogan 1989). Many of these same traits are related to the acquisition of higher education (e.g., Wagerman and Funder 2007) and political action (Mondak 2010).
Besides illuminating the causal link between education and participation, health may directly impact other politically relevant resources, like time, money, and civic skills. It takes time to manage chronic disease, such as diabetes or depression, time that may alternatively be used to learn about political affairs. Similarly, being diagnosed with a disease constitutes the kind of major life event that may discourage political participation by directing attention to personal matters and away from political ones (Stoker and Jennings 1995).5 The financial burdens of poor health, such as medical expenses to cover doctor visits, medication and treatments, as well as the temporary or permanent loss of employment that typically accompanies poor health (e.g., Havemen et al. 1994), decreases the probability of campaign contributions. Health conditions that limit physical mobility, a resource often overlooked by political scientists, may be particularly detrimental to political participation (e.g., Schur and Kruse 2000), although research has shown that absentee ballots (Alvarez et al. 2012) or improved street conditions (Clarke et al. 2010) can help overcome some of these physical limitations. Finally, health conditions, such as depression (Fassati et al. 1999) or dementia (Irastorza et al. 2011), impair cognitive abilities and executive functioning that likely affects the civic skills required for participation.
Motivation
Even if one has the resources conducive to political participation, motivation is necessary to transform those resources into action (Han 2009). Motivation refers to the psychological factors, such as political interest, political efficacy, and the belief that political participation is a civic obligation, required to participate in politics (Schlozman et al. 2012). The most obvious way that health impacts the motivation to participate is through mental health conditions, such as anxiety or depression, that are related to low levels of subjective well-being (Ainsworth 2000) that likely spillover to affect politically relevant psychological factors and decrease participation (Ojeda 2013). Often times, psychological factors that may hinder participation are prevalent in people with poor physical health. For instance, patients with coronary heart disease (CHD) are likely to have symptoms of depression or anxiety (Meyer et al. 2010). This suggests that physical health conditions, not just mental health conditions, may be relevant for motiving political behavior. Finally, there is a large literature suggesting that people with certain health conditions are subject to stigma and discrimination. Obese people, for instance, are assumed to be impulsive with a lack of personal control (Teachman et al. 2001), which leads to discrimination in the workforce (Roehling 1999), school (Latner and Stunkard 2001), medical facilities (Teachman and Brownell 2001), and day-to-day interactions (Carr and Friedman 2005). People with disabilities are also likely to experience discrimination (Yuker 1988). Institutional discrimination, studied mostly from the experiences of African Americans, reduces feelings of internal and external efficacy (Gimpel et al. 2003) that may inhibit political participation.
Social Networks
Supportive social networks formed from family and friends, in school, at workplaces, and through voluntary or religious associations, play a large role in fostering political activity (Zuckerman 2005). Through these interactions, people learn about politics and obtain information that can supplement and replace the resources needed for political participation (McClurg 2003). Conversely, people who are isolated miss out on the opportunities to learn about politics from others (Verba et al. 1995). Feelings of social isolation are strongly associated with human physical health (Cacioppo and Hawkley 2003), such as cardiovascular and inflammation-related diseases (Caspi et al. 2006) and disability (Louis Harris and Associates 1998), as well as aspects of mental health, such as depression (Rubin and Coplan 2004). Most important, health is negatively related to labor force participation (McDonough and Amick III 2001); hence, people of poor health are likely to experience temporary or permanent loss of employment, which impacts participation via the loss of workplace social networks.
Mobilization
People are more likely to participate in politics when asked to do so, whether this request comes from face-to-face interactions with someone they know (Brady et al. 1999; Lim 2008), through shared membership in a voluntary association (McAdam and Paulsen 1993), or from campaign activists during an election (Rosenstone and Hansen 1993). We have already discussed the reasons why people of poor health may be less likely to be mobilized through social interactions above, so in this section we concentrate on organized mobilization from external sources. Practically, people of poor health may be particularly hard to reach if most of their time is spent in out-patient or in-patient treatment centers, hospitals, or other medical facilities. Residential mobility, one of the largest predictors of being contacted by a political organization (Rosenstone and Hansen 1993), is also strongly associated with poor health in mature adults (Larsen et al. 2004), suggesting that people of poor health are geographically difficult to locate.
In other cases, the personal experience of a serious health condition may encourage bouts of activism through an association committed to a particular disease or condition. The disability rights movement, for instance, provided an opportunity for persons with disabilities to turn personal struggles into political action (Schur 1998) and resulted in the passage of the Americans with Disabilities Act in 1990.6 Anecdotal evidence abounds with stories of celebrities turning their own personal struggles into political advocacy, for instance, Michael J. Fox after being diagnosed with Parkinson’s disease, Magic Johnson after being diagnosed with AIDS, and Christopher Reeves, after suffering a spinal cord injury.
To summarize, there are multiple theoretical pathways linking health to various forms of political participation. Health may impact the resources and motivation necessary for political action as well as social networks and mobilization. The relationship between health and political participation is no doubt complex, varied across the lifespan, and difficult to disentangle. Nonetheless, we take a first step at understanding the complex relationships described above by looking at the impact of health on voter turnout using two data sources, the GSS and Add Health, as we describe below.
The Impact of Health on Voter Turnout using the General Social Survey
To analyze the effects of health on turnout among the general population, we use the General Social Survey (GSS). The GSS conducted 24 nationally representative surveys between 1972 and 2010 that included both the turnout and health measures.7 The sample consists of 39,345 respondents with about 1,500 respondents interviewed for each year. Response rates range from 70–82%.8 Fifty-two percent of the respondents are female. In terms of race, 81% of the respondents are white, 12% black, and 6% of another race.9 Twenty-three percent of the respondents have no high school degree, 53% have a high school degree, 5% have some college education, and 18% have a college degree. The majority of respondents report being married (64%) at the time of the survey. Finally, the average age is 46 years. Descriptive information on all variables is included in Table A1 in the Appendix.
Measures
The dependent variable is a measure of voter turnout in the most recent presidential election. There is an over reporting of voting since many people incorrectly report voting, either due to social desirability or memory failure (e.g., Burden 2000). Statistically, classical measurement error in the dependent variable is of little consequence to our analyses and conclusions. Regression coefficients remain unbiased and standard errors remain valid, but will be larger than in the absence of error (Wooldridge 2012). In our sample, 62% report voting in the most recent election.
Health is measured using SRHS with answers including excellent, good, fair, or poor. We measure health linearly with higher values indicating better health.10 Five percent of our sample report being in poor health at the time of the survey, 18% report being in fair health, 45% report being in good health, and 32% report being in excellent health. There is a moderate correlation between self-rated health and age (r=−.24), with 31% of those in poor health being 65 years of age or older.
We include other covariates in the analyses that are important for voter turnout. We include indicator variables of the highest degree earned, with no high school degree as the omitted category with the general expectation that highly educated people are more likely to participate (Brady et al. 1995). Race is included as binary variables (white, black, and other) with the white category as the omitted category. An indicator variable is included for gender (1=female, 0=male) as well as marital status (1=married, 0 otherwise) since married persons are more likely to turnout (Stoker & Jennings 1995). We include age centered at the mean (46 years of age) to ease statistical interpretation.11 We also include partisan strength (1=strong partisan, 0 otherwise), religious attendance (0=never, 1=less than once a year, 2=once a year, 3=several times a year, 4=once a month, 5=2–3 times a month, 6=nearly every week, 7=every week, and 8=more than once a week), and newspaper readership (0=never, 1=less than once a week, 2=once a week, 3=few times a week, 4=everyday); all of these things are positively related to voter turnout (Brady et al. 1995). Finally, to account for temporal trends in voter turnout, we include year and year squared.12
We use logistic regression to explore the effect that health has on voter turnout. In the first model, we regress SRHS and control variables on voter turnout. In the second model, we interact SRHS with age to explore the differential impacts of health on turnout across age. In both models, we report the estimated changes in the predicted probabilities when the variable changes from its minimum to maximum value, keeping all other variables constant at the mean. We employ weights for household size and the oversampling of African Americans (Marsden 2012).
Results
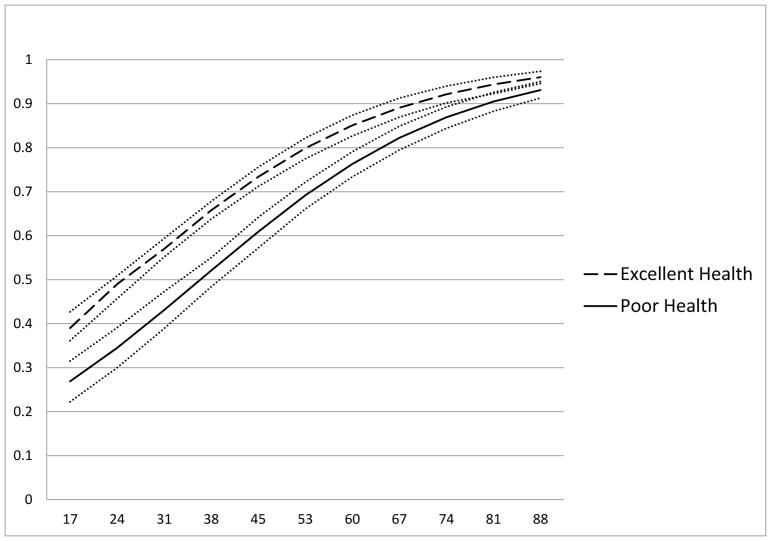
Table 1 presents the results of regressing SRHS on voter turnout in the most recent election using the cumulative GSS. As shown in Model 1 in Table 1, better health increases the probability of voting in the most recent presidential election. Specifically, the model predicts that increasing health from poor to excellent increases the probability of voting by 12%. While education and age have stronger impacts on turnout, health is similar to the effects of race, marital status, partisan strength, religious attendance, and newspaper readership. Results in Model 2 in Table 1 indicate that health has a positive impact on voting across age groups, although the effect is stronger as age increases. To visualize how health interacts with age to influence voter turnout, we plot the predicted probabilities of voter turnout across age for those in poor and excellent health in Figure 2. Figure 2 shows that the turnout gap between those of poor and excellent health widens as age increases, then slowly narrows in old age.
Table 1.
Logistic Regression Predicting Turnout in Presidential Elections with SRHS using the GSS 1972–2010 (N=19,807)
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| Δ probability min to max | Δ probability min to max | |||
| SRHS | .17*** (.03) |
12% | .19*** (.04) |
13% |
| Age (centered at 46) | .04*** (.002) |
54% | .03*** (.004) |
40% |
| Age* Self-Rated Health | .01*** (.002) |
29% | ||
| High School Degree | .96*** (.07) |
21% | .94*** (.07) |
20% |
| Some College | 1.35*** (.18) |
22% | 1.33*** (.18) |
22% |
| College Degree or Higher | 1.91*** (.09) |
32% | 1.90*** (.89) |
31% |
| Female | .03 (.05) |
1% | .03 (.04) |
1% |
| Black | −.28** (.09) |
−6% | −.28** (.09) |
−6% |
| Other | −1.04*** (.13) |
−25% | −1.05*** (.13) |
−25% |
| Married | .44*** (.05) |
10% | .41*** (.05) |
9% |
| Strong Partisan | .92*** (.08) |
18% | .93*** (.08) |
18% |
| Religious Attendance | .10*** (.01) |
17% | .10*** (.01) |
17% |
| Newspaper Readership | .19*** (.02) |
17% | .19*** (.02) |
17% |
| Year | −.03** (.01) |
−14% | −.03** (.01) |
−15% |
| Year-squared | .001* (.001) |
13% | .001* (.001) |
12% |
| Constant | −1.75*** (.13) |
−1.71*** (.13) |
||
Note: Standard Errors in parentheses. Significance levels:
p<0.01,
p<0.05,
p<0.1 with a two-tailed test.
Age is mean centered. Weights are employed to account for the complex survey design.
Figure 2.
Predicted Probabilities of Voting Across Age and SRHS
The results in Table 1 and Figure 2 suggest that poor health dampens voter turnout among the general population, however, the cross-sectional nature of the data as well as the fact that voting is asked retrospectively are two limitations that may cause doubt in our findings. Furthermore, analyses from the GSS cannot separate the developmental effects of health on turnout from the contemporaneous effects. Consequently, we use panel data on young citizens to explore the potential developmental effects of health on voter turnout in the next section.
The Impact of Health on Youth Voter Turnout using Add-Health
The National Longitudinal Study of Adolescent Health (Add Health) is a longitudinal study of a nationally representative sample of 7th–12th grade students surveyed in 1994–1995 (W1) with follow-up surveys conducted in 1996 (W2), 2001/2002 (W3), and 2007/2008 (W4). Add Health asks numerous questions to respondents and parents regarding a number of topics including health-related behaviors, attitudes, relationships, civic activities, and political participation. We use data from W1 and W3 since the voter turnout measure is only available for W3. There were 14,138 individuals eligible to vote by W3 who also had survey weights available and did not have missing data on self-reported health or education. The sample is 49% female, 68% white, 16% African American, and 12% Hispanic. Average age is 22 years with a range from 18 to 26. Fifty two percent attended college, while 33% completed schooling by graduating high school. These rates are mirrored by the respondents’ mothers’ levels of education, with 52% attending college and 34% stopping at high school graduation. For descriptive statistics on all variables, see Table A1 in the Appendix.
Measures
The dependent variable is voter turnout in the 2000 presidential election asked in W3. Forty three percent of the sample reported voting in the 2000 election. Like the GSS, we measure health using a SRHS question with five allowable responses of excellent (32% W3, 28%W1) very good (41% W3, 40% W1) good (22% W3, 25% W1), fair (4% W3, 6% W1), and poor (<1% in W3 and W1). We measure SRHS so that higher values represent better health. 13 Since health may have both developmental and contemporaneous effects, we measure SRHS in W1 and W3. SRHS in W1 is our measure of adolescent health, while the SRHS in W3 measures contemporaneous health.
We control for other variables that impact youth voter turnout including respondent gender (1=female), race (black, Hispanic, and other; white is omitted), income at W3, employment at W3, age at W3, education at W3 (no high school degree is omitted), and religious attendance (Plutzer 2002). We also include a dummy variable to indicate whether the respondent had missing family data. Finally, to account for the role that the home environment has on later political participation (Plutzer 2002), we include mother’s level of educational attainment (no high school degree is omitted) 14 and family income at W1.15 We model turnout using logistic regression as a function of SRHS and parental and respondent controls. Robust standard errors, clustered by state, are included to correct for non-independence across observations within states and estimates are also weighted to account for the complex survey design. Results are shown in Table 2.
Table 2.
Logistic Regression Predicting Turnout in Presidential Elections with SRHS using Add-Health (N=12,540)
| Δ probability min to max | ||
|---|---|---|
|
|
||
| SRHS (W1) | .07* (.04) |
7% |
| SRHS (W3) | .10** (.03) |
9% |
| High School Grad (W3) | .49*** (.09) |
12% |
| College Grad (W3) | 1.20*** (.09) |
28% |
| Employment (W3) | .03 (.05) |
1% |
| Income (W3) | .000002 (.000002) |
28% |
| Age (W3) | .08*** (.02) |
20% |
| Female | −.05 (.05) |
−1% |
| Hispanic | −.36** (.13) |
−9% |
| Black | .49** (.15) |
12% |
| Other Race | −.72*** (.13) |
−16% |
| Religious Attendance (W3) | .14*** (.02) |
20% |
| Mother High School Grad | .15* (.08) |
4% |
| Mother College Grad | .41*** (.09) |
10% |
| Family Income (W1) | .004*** (.001) |
58% |
| Missing Family Information | −.13** (.06) |
−3% |
| Constant | −4.27*** (.47) |
|
Note: Robust standard errors in parentheses. Estimates are weighted to account for the complex survey design.
p<0.01,
p<0.05,
p<0.1
Results
As shown in Table 2, both adolescent and contemporaneous health positively impact youth voter turnout. Keeping all other variables constant at their mean values, the model estimates that an adolescent who is in excellent health has a probability of turning out five years later that is 7 percentage points higher than an adolescent who is in poor health. The magnitude of the effect of adolescent health on youth voter turnout is more than the effect of maternal high school degree, which is about 4 percentage points, keeping all variables constant. Table 2 also shows that youths in excellent health at the time of the 2000 election have a probability of turning out that is about 9 points higher than young adults who report being in poor health. The contemporaneous effect of health is equal in magnitude to the effect of having a mother with a college degree versus a mother who dropped out of high school. In short, health status has both developmental and contemporary components that impact voter turnout and rivals other important factors, like parental educational attainment.
The results in Tables 1 and 2 suggest that (1) poor health decreases turnout among all age groups, but particularly among older age groups; (2) poor health in adolescence decreases voter turnout years later, suggesting that health has both contemporary and developmental effects; and (3) the effect of health on voter turnout is direct and unmediated by socioeconomic status. While identifying the correlates of political participation is an important endeavor in its own right, the implications of such research are amplified if non-participants have different political preferences than the politically active. In short, differential participation rates coupled with differential preferences increases the risk of non-responsiveness. In the next section, we show that not only is health related to voter turnout, but it is also related to partisanship suggesting that health inequalities in participation may have significant political consequences.
CONCEPTUALLY LINKING HEALTH TO PARTISANSHIP
How might health influence partisanship?16 While classic research on the origins of partisanship suggests that family socialization plays a large role (Campbell et al. 1960), we also know that partisanship can shift in response to political issues, events, and candidates (Franklin 1984). Thus, it is likely that the impact of health on partisanship has both developmental and contemporaneous effects. We briefly discuss both below.
Developmental Components
Studies of political socialization show that partisanship begins to form in childhood and early adolescence (Jennings and Niemi 1974) with parents being particularly influential. For instance, Beck et al. (2008) find that in families where both parents share a party affiliation, nearly three fourths of offspring adopt the same party (Chapter 7). Conversely, only about one tenth of offspring rebelled politically against their parents and identified with the opposing party (Beck et al. 2008). Like partisanship, parental health is highly correlated with offspring health (National Research Council 2000), yet a large portion of the intergenerational transmission of health, like political activity, is linked to socioeconomic status. For instance, Case et al. (2002) find that children from lower-income households with chronic health conditions have worse health than do children from higher-income households. They also find that poor health has cumulative impacts on socioeconomic status that persist across the lifespan.
Consequently, there are a variety of theoretical pathways linking adolescent health to partisanship years later. One pathway involves the simultaneous transmission of health and party affiliation from parent to child. If parents of poor health are likely to identify with a certain party, offspring may adopt a similar party through parental nurturing and also be likely to have similar health conditions and outcomes in adulthood. Another pathway involves personality. Personality traits, which tend to form early (McCrae and Costa 2008) and exhibit stability in adulthood (Caspi 2000), are also related to health (Rhodes and Smith 2008) and partisanship (Mondak 2010). For instance, Mondak (2010) finds that people who are high on the agreeableness trait are also likely to identify with the Democratic Party. High levels of agreeableness are associated with less risky behaviors in youth (Markey et al. 2006). Adults who scored high on this dimension are less likely to smoke (Malouff et al. 2006) and have lower rates of alcoholism, depression, and arrest (Laursen et al. 2002). Thus, personality traits may simultaneously influence health and partisanship years later. Finally, it may be that adolescent health is related to different experiences that ultimately influence opinions regarding the determinants of health, tapping into broader political debates regarding individual versus social responsibility and likely impact partisan attachments. For instance, Robert and Booske (2011) find that healthy people are less likely to believe that social factors, such as affordable health care, play a role in determining health; they are also less likely to think that social policy, such as reducing poverty and improving education, are effective at improving public health. In short, people in poor health, probably as a result of their own experiences, are more likely to recognize the social determinants of health, leading to higher support of government intervention and a higher likelihood of identifying with the Democratic Party.
Contemporaneous Effects
Besides having developmental components, the impact of health on partisanship also likely has contemporaneous effects and varies as individuals react to elite rhetoric, the behavior of party leaders, and the political agenda (Brooks and Manza 1997). While there are a variety of issues that make health relevant to political attitudes, the longest running debate regarding health policy concerns universal health insurance, which is “the oldest story in American health politics” (Hacker and Skocpol 1997 315).
While on and off the political agenda since at least the Progressive Era, the modern era of health care reform begins with President Truman’s failed attempt at universal health care which gave birth to a pro-reform coalition consisting of Democrats, liberals, healthcare officials, and allies in organized labor that ushered in the Social Security Amendments signed by President Johnson in 1965 (Hacker and Skocpol 1997). The Health Security plan sponsored by President Clinton during 1993 and 1994 brought health care reform back into the political spotlight and echoed much of the political optimism surrounding Truman’s plan fifty years earlier. In the end, Republican leadership, backed by a coalition of small businesses, commercial insurance companies, members of the Christian Coalition, and other right-wing advocacy groups (Skocpol 1997) defeated the Health Security plan, causing many to claim that even modest incremental solutions towards expanded health care were lost. In 2010, President Obama signed the Affordable Care Act (ACA) into law ushering in a new era of health care reform. Although seen as a political victory, political challenges await as opponents at the state and national levels seek to undermine the law through judicial and administrative action (Skocpol 2013).
The brief history of healthcare reform summarized above provides insights about the contemporaneous role of health on partisanship. Given that Democrats have traditionally supported an expansive role of government to improve the health of the nation, the expectation is that people who are most in need of those improvements (e.g., those in poor health) will be most likely to support the Democratic Party, particularly in recent years as healthcare reform has gained national prominence in political debates.
The Effect of Health on Partisanship
We estimate the effect of health on party identification using both the GSS and Add Health data. The advantage of the GSS is that we can estimate the impact of health on partisanship among the general population while Add-Health allows us to test whether the effect of health on partisanship has both developmental and contemporaneous components, as suggested above.
For the analyses using the GSS, respondents are asked “Generally speaking, do you usually think of yourself as a Republican, Democrat, Independent, or what?” Responses are recoded into a binary variable with a positive response indicating identification with the Republican Party. In our sample, 26% of adults identified with the Republican Party. For Add-Health, students are asked in W3 “With which party do you identify” to which 14% identified with the Republican Party. Similar to the analyses above, we measure the linear effect of health in both surveys using SRHS; the difference between the two is that we measure both developmental SRHS (at W1) and contemporaneous SRHS (at W3) in the Add-Health data, whereas in the GSS we only have contemporaneous measures.17
We control for the “usual suspects” that have been shown to influence party identification (e.g., Beck et al. 2008) including education, race, gender, age, and religious attendance measured identically to the previous analyses. We also include marital status in the GSS analyses and year and year squared to account for temporal trends in partisanship. In the Add Health analyses, we include various indicators of the home environment, including maternal education at W1 and family income at W1. Logistic regression with survey weights is used for both analyses; in addition, robust standard errors, clustered by state, are included to correct for non-independence across observations within states in Add Health. We also report the estimated changes in the predicted probabilities when the variable changes from its minimum to maximum value, keeping all other variables constant at the mean. Results are shown in Table 3.
Table 3.
Logistic Regression Predicting Republican Party Identification with SRHS, using the GSS and Add-Health
| GSS (N=38,286)
|
Add-Health (N=12,540)
|
||||
|---|---|---|---|---|---|
| Δ probability min to max | Δ probability min to max | ||||
| SRHS | .18*** (.02) |
9% | SRHS (W1) | .11** (.05) |
4% |
| SRHS (W3) | .09* (.04) |
2% | |||
| Age (centerd at 46) | .07*** (.001) |
9% | Age (W3) | .07*** (.02) |
6% |
| High School Degree | .27*** (.05) |
5% | High School Grad (W3) | .45*** (.12) |
4% |
| Some College | .42*** (.08) |
8% | |||
| College Degree or Higher | .45*** (.06) |
9% | College Grad (W3) | .86*** (.13) |
6% |
| Black | −1.89** (.09) |
−23% | Black | −2.33*** (.26) |
−11% |
| Other | −.91*** (.11) |
−13% | Other | −1.66*** (.22) |
−7% |
| Female | −.16*** (.03) |
−3% | Female | −.33*** (.06) |
−3% |
| Hispanic | −.92*** (.24) |
−5% | |||
| Employment (W3) | −.04 (.09) |
||||
| Income (W3) | .0000001 (.00003) |
||||
| Family Income (W1) | .001 (.001) |
||||
| Mom High School Grad | .001 (.22) |
||||
| Mom College Grad | .19 | ||||
| Married | (.10)** (.04) |
2% | (.21) | ||
| Religious Attendance | .10*** (.01) |
15% | Religious Attendance (W3) | .30*** (.02) |
18% |
| Year | .07*** (.01) |
27% | |||
| Year-squared | −.002*** (.0004) |
−19% | |||
| Missing Family Information | −.09** (.09) |
−1% | |||
| Constant | −2.24*** (.08) |
Constant | −5.19*** (.54) |
||
Note: Standard Errors in parentheses. Significance levels:
p<0.01,
p<0.05,
p<0.1 with a two-tailed test.
Age is mean centered. Weights are employed to account for the complex survey design. Robust standard errors are reported for analyses using Add-Health.
As shown in Table 3, better self-rated health increases the likelihood of identifying with the Republican Party among adults and in youths. Specifically, using the GSS, the model predicts that the probability of identifying with the Republican Party is 9 percentage points higher for people in excellent health compared to respondents who report being in poor health, keeping all other variables constant. To be fair, other variables matter more. For instance, the strongest predictor of Republican identification is race (blacks have probabilities that are 23 points lower than whites). However, health continues to have an effect on party identification, even after accounting for these other important covariates, and this effect rivals other important covariates, such as having a college degree or being older.18
Similar results are obtained using Add Health. As shown in Table 3, SRHS has both developmental and contemporaneous effects on youth partisanship. Specifically, the model predicts that adolescents who report being in excellent health are 4 percentage points more likely to identify with the Republican Party years later compared with those who report being in poor health. The model also predicts that young adults who are in excellent health at the time of the survey are 2 percentage points more likely to identify with the Republican Party. Similar to the analyses using the GSS, race remains an important factor in partisan attachments; black youths are 11 percentage points less likely to identify with the Republican Party compared to whites.
In sum, there is empirical support that health status matters for party identification both among adults and youths. Moreover, the results suggest that the effects of health on partisanship have both developmental and contemporaneous effects, holds up in the presence of traditional controls, and rivals other more studied covariates, such as education and gender.
CONCLUSION
In May 2013, while crediting the recent success of immigration reform in Congress to the Hispanic vote that went heavily against Republicans in 2012, Gail Collins quipped
“if somebody came up with a dramatic poll showing that all the people with diabetes, asthma, and chronic back problems had voted against Mitt Romney, there would no longer be a problem getting funding for health care reform.”
Our results suggest exactly that; we find that people of poor health are not only less likely to participate in politics, but that they also have different partisan attachments. In short, health appears to be highly relevant to political behavior and the broader political system. This result may surprise some political scientists who have focused on the sociological divisions of political power based on class and other demographic factors. Yet, public health scholars have long recognized the fundamental links between health, class, and demographic characteristics, such as gender and race and ethnicity. The empirical evidence presented in this paper suggests that political scientists should consider how health outcomes are related to individual political behavior and how that relationship translates into relevant political divisions that impact electoral outcomes and eventual public policy.
To that end, our results suggest that the health inequalities that we find in political voice may have significant political consequences. If healthy people have systematically different policy preferences than the unhealthy and are more likely to turnout, then electoral results and the policies that are enacted may have a “health bias.” The health policies offered and enacted by the government may favor the healthy and not be suitable for those in poor health, much like disparities in political voice across income levels influence the enactment of public policies from which the poor are most likely to benefit (Hill and Leighley 1992). Hence, one avenue for future research is to explore the policy implications of these political inequalities, perhaps by comparing policies in states where the participation gap between those in excellent and poor health is relatively small to states with large inequalities in participation across health.
Additional empirical analyses about the relationship between health outcomes, risk behaviors, political participation, and public opinion would help further determine the relevance of health to political behavior. Scholars may benefit from looking at how aggregate participation or opinions vary across health status to determine if and on which issues health matters most. Research designs that parse out the mechanism that links health to political behavior, for instance through political rhetoric and elite framing or through individual characteristics are particularly beneficial. Moreover, which indicators of population health e.g., obesity rates, smoking rates, disease-incidence, or SRHS, matter most for aggregate patterns of political participation? Cross-national comparative studies of political participation would be particularly helpful in answering these questions
In addition, our results imply that health policies aimed at improving the health of the nation, such as universal healthcare, may contribute to a more politically active and engaged society. Increasing the political participation of the unhealthy is a formidable task for policy advocates, particularly since our results suggest the effects of health on voter turnout originate in adolescence and persist into young adulthood. Nonetheless, policies aimed at making registration and voting easier (Alvarez et al. 2010) or improving the built environment (Clarke et al. 2011), for instance by reducing traffic, increasing residential security, or improving street conditions, may help. Finally, there are institutions, such as community colleges, that at their core attempt to “level the playing field” across levels of disadvantage (Pacheco and Plutzer 2007). These same institutions may have large impacts on the political participation of youths who are unhealthy.
Nonetheless, there is still much to learn about the impact that health has on political participation and public opinion with implications to our understandings of policy responsiveness and political inequality. Indeed, our primary goal is to theoretically and empirically show that health is an important explanatory factor of political behavior in hopes that other scholars will follow suit. The effects of adolescent and adult health on voter turnout and partisanship are not overwhelming, but they do exist and are highly correlated with arguably the most studied covariate, educational attainment, which makes health all the more relevant to political science research.
Supplementary Material
Footnotes
The General Social Survey has four allowable responses including excellent, good, fair, and poor while Add-Health has five response categories.
The National Health Interview Survey is collected by the National Center for Health Statistics, which is part of the Centers for Disease Control and Prevention, and has tracked health topics annually since 1957. The NHIS is a large-scale household interview survey of a statistically representative sample of the US civilian non-institutionalized population. For more information go to the website located at http://www.cdc.gov/nchs/nhis/about_nhis.htm.
Estimates in Figure 1 are weighted to account for the complex survey design.
We define political participation much like other scholars as activities directed at government (Schlozman et al. 2012). In particular, political participation includes such acts as donating money, campaigning, voting, displaying yard signs, yet excludes political discussion and creative participation.
While beyond the scope of this paper, having a family member recently diagnosed with a chronic medical condition may also impact political participation of otherwise healthy respondents.
Having a family member diagnosed with a serious health condition may induce otherwise health family members to become politically active on their behalf. The Susan G. Komen organization, for instance, was started by Nancy G. Brinker after her sister, Susan, died from breast cancer (http://ww5.komen.org/AboutUs/AboutUs.html).
Specifically, data is available for the following years: 1972, 1973, 1974, 1976, 1977, 1980, 1982, 1984, 1985, 1987, 1988, 1990, 1991, 1993, 1994, 1996, 1998, 2000, 2002, 2004, 2006, 2008, and 2010.
General Social Survey website. http://www3.norc.org/NR/rdonlyres/2E75FB22-4D36-474F-AA28-97D9A2C04B6C/1966/GSSResponsePeriodandFieldPeriod1.pdf. Accessed July 27, 2010.
The GSS did not start asking about Hispanic ethnicity until 2000. We use the three category race variable since it is available in all surveys.
Analyses are nearly identical when health is measured as a categorical variable.
In additional analyses, we also included the GSS WORDSUM score as a measure of vocabulary ability to account for the cognitive skills needed for turning out. While this variable was statistically significant, it did not change our substantive conclusions regarding the influence of health on turnout. We choose not to include this variable because it was asked in a subset of the GSS surveys and would decrease our sample size substantially.
Analyses are nearly identical when including fixed effects of year.
Results are nearly identical when SRHS is measured as a categorical variable as opposed to linearly.
The parental survey targeted the mother or female mother figure. Only in cases where none were available did a father/father figure complete the parental survey. In most cases, the parental civic engagement variable measures maternal civic engagement.
In results available upon request, we also included a measure of parent civic engagement at W1, which asks whether the parent is a member of a civic or social organization. The inclusion of this variable drops the number of cases by 2,000 and causes the coefficient on the SRHS at W1 to fail to reach statistical significance. When values on the parental civic engagement variable are mean-imputed, the coefficient on SRHS at W1 is statistically significant (B=.067* with a two-tailed test).
We acknowledge that health may impact political attitudes beyond partisanship including ideology, opinions about the saliency of issues, feelings towards political candidates, and views towards specific policies including healthcare reform, abortion, the death penalty, welfare, and others. It is beyond the scope of the paper to look at these different types of attitudes, although we encourage others to do so.
Results are nearly identical when we measure SRHS categorically instead of linearly.
We find that the effect of health on partisanship declines as age increases as the interaction between age and SRHS is negative and statistically significant (B=−.003*). Nonetheless, health appears to influence partisanship at all age levels.
Contributor Information
Julianna Pacheco, Assistant Professor of Political Science, University of Iowa.
Jason Fletcher, Associate Professor of Public Affairs, University of Wisconsin-Madison.
References
- Alvarez Michael R, Levin Ines, Andrew Sinclair J. Making Voting Easier: Convenience Voting in the 2008 Presidential Election. Political Research Quarterly. 2012;65:248–262. [Google Scholar]
- Ainsworth Patricia. Understanding Depression. University Press of Mississippi; 2000. [Google Scholar]
- Angel Ronald, Gronfein William. The Use of Subjective Information in Statistical Models. American Sociological Review. 1988;53:464–473. [Google Scholar]
- Beck, Lewis Michael S, Jacoby William G, Norpoth Helmut, Weisberg Herbert F. The American Voter Revisited. Ann Arbor, MI: University of Michigan Press; 2008. [Google Scholar]
- Belli Robert F, Traugott Micheal W, Young Margaret, McGonagle Katherine A. Reducing Vote Overreporting in Surveys: Social Desirability, Memory Failure, and Source Monitoring. Public Opinion Quarterly. 1999;63(1):90–108. [Google Scholar]
- Boardman Jason D. Self-Rated Health among U.S. Adolescents. Journal of Adolescent Health. 2006;38(4):401–408. doi: 10.1016/j.jadohealth.2005.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth-Kewley Stephanie, Vickers Ross R. Associations between Major Domains of Personality and Health Behavior. Journal of Personality. 1994;62:281–98. doi: 10.1111/j.1467-6494.1994.tb00298.x. [DOI] [PubMed] [Google Scholar]
- Bjorner Jakob B, Fayers PM, Idler EL. Self-rated health. In: Fayers Peter, Hays Ron., editors. Assessing Quality of Life. Oxford University Press; 2005. [Google Scholar]
- Brady Henry E, Schlozman Kay Lehman, Verba Sidney. Prospecting for Participants: Rational Expectations and the Recruitment of Political Activists. American Political Science Review. 1999;93(1):153–68. [Google Scholar]
- Braveman Paula, Cubbin Catherine, Egerter Susan, Williams David R, Pamuk Elsie. Socioeconomic Disparities in Health in the United States: What the Patterns Tell Us. American Journal of Public Health. 2010;100(S1):S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks Clem, Manza Jeff. Social Cleavages and Political Alignments: US Presidential Elections, 1960–1992. American Sociological Review. 1997;62(6):937–946. [Google Scholar]
- Burden Barry C. Voter Turnout and the National Election Studies. Political Analysis. 2000;8(4):3890–398. [Google Scholar]
- Cacioppo John T, Petty Richard E, Feinstein Jeffrey A, Blair W, Jarvis G. Dispositional Differences in Cognitive Motivation: The Life and Times of Individuals Varying in Need for Cognition. Psychological Bulletin. 1996;119:197–253. [Google Scholar]
- Cacioppo John T, Hawkley Louise C. Social isolation and health, with an emphasis on underlying mechanisms. Perspectives in biology and medicine. 2003;46(3):S39–S52. [PubMed] [Google Scholar]
- Campbell Angus, Converse Philip E, Miller Warren E, Stokes Donald E. The American Voter. University of Chicago Press; 1960. [Google Scholar]
- Carr Deborah, Friedman Michael A. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. Journal of Health and Social Behavior. 2005;46(3):244–259. doi: 10.1177/002214650504600303. [DOI] [PubMed] [Google Scholar]
- Anne Case, Lubotsky Darren, Paxson Christina. Economic status and health in childhood: The origins of the gradient. American Economic Review. 2002;92:1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Caspi Avshalom, Harrington HonaLee, Moffitt Terrie E, Milne Barry J, Poulton Richie. Socially isolated children 20 years later: risk of cardiovascular disease. Archives of pediatrics & adolescent medicine. 2006;160(8):805. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Clarke Philippa J, Ailshire Jennifer A, Nieuwenhuijens Els R, de Kleijn-de Vrankrijker Marijke W. Participation Among Adults With Disability: The Role of the Urban Environment. Social Science & Medicine. 2011;72(10):1674–1684. doi: 10.1016/j.socscimed.2011.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins Gail. Somebody Did Something. [Accessed July 22, 2013];New York Times Op-Ed. 2013 May 22; http://www.nytimes.com/2013/05/23/opinion/collins-somebody-did-something.html?ref=opinion.
- Diez Roux Ana V. Investigating neighborhood and area effects on health. American journal of public health. 2001;91(11):1783–1789. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubois L, Girard M. Social Position and Nutrition: A Gradient Relationship in Canada and the USA. European Journal of Clinical Nutrition. 2001;55(5):366–373. doi: 10.1038/sj.ejcn.1601165. [DOI] [PubMed] [Google Scholar]
- Elo Irma T, Preston Samuel H. Educational Differentials in Mortality: United States 1979–85. Social Science and Medicine. 1996;42(1):47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Ferraro Keneth F. Health and aging. Handbook of aging and the social sciences. 2006;6:238–256. [Google Scholar]
- Fossati Philippe, Amar Gilles, Raoux Nadine, Ergis Anne M, Allilaire Jean F. Executive Functioning and Verbal Memory in Young Patients with Unipolar Depression and Schizophrenia. Psychiatry Research. 1999;89(3):171–87. doi: 10.1016/s0165-1781(99)00110-9. [DOI] [PubMed] [Google Scholar]
- Franklin CE. Issue Preferences, Socialization, and the Evolution of Party Identification. American Journal of Political Science. 1984;28:459–78. [Google Scholar]
- Gimpel James G, Celeste Lay J, Schuknecht Jason E. Cultivating democracy: Civic environments and political socialization in America. Brookings Institution Press; 2003. [Google Scholar]
- Hacker Jacob, Skocpol Theda. The New Politics of US Health Policy. Journal of Health Politics, Policy and Law. 1997;22(2):316–338. doi: 10.1215/03616878-22-2-315. [DOI] [PubMed] [Google Scholar]
- Han Hahrie. Moved to Action: Motivation, Participation and Inequality in American Politics. Stanford, CA: Stanford University Press; 2009. [Google Scholar]
- Hajat Anjum, Diez-Roux Ana, Franklin Tracy G, Seeman Teresa, Shrager Sandi, Ranjit Nalini, Castro Cecilia, Watson Karol, Sanchez Brisa, Kirschbaum Clemens. Socioeconomic and race/ethnic differences in Daily Salivary Cortisol Profiles: The Multi-Ethnic Study of Atherosclerosis. Psychoneuroendocrinology. 2010;35(5):932–943. doi: 10.1016/j.psyneuen.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haveman Robert, Wolfe Barbara, Kreider Brent, Stone Mark. Market work, wages, and men’s health. Journal of Health Economics. 1994;13(2):163–182. doi: 10.1016/0167-6296(94)90022-1. [DOI] [PubMed] [Google Scholar]
- Hogan Joyce. Personality Correlates of Physical Fitness. Journal of Personality and Social Psychology. 1989;56:284–88. doi: 10.1037//0022-3514.56.2.284. [DOI] [PubMed] [Google Scholar]
- Huisman Martijn, Deeg Dorly JH. A commentary on Marja Jylhä’s “What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine. 2010;70(5):652–654. doi: 10.1016/j.socscimed.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Idler Ellen L, Benyamini Yael. Self-Rated Health and Mortality: A Review of Twenty-Seven Community Studies. Journal of Health and Social Behavior. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Irastorza Luis Javier, Corujo Pablo, Bañuelos Pilar. Capacity to Vote in Persons with Dementia and the Elderly. International Journal of Alzheimer’s Disease. 2011 doi: 10.4061/2011/941041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings M Kent, Niemi Richard G. The political character of adolescence: The influence of families and schools. Princeton, NJ: Princeton University Press; 1974. [Google Scholar]
- Jylhä Marja. What is Self-Rated Health and Why does it Predict Mortality? Towards a Unified Conceptual Model. Social Science & Medicine. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kam Cindy D, Palmer Carl L. Reconsidering the Effects of Education on Political Participation. The Journal of Politics. 2008;70(3):612–631. [Google Scholar]
- Lantz Paula M, House James S, Lepkowski James M, Williams David R, Mero Richard P, Chen Jieming. Socioeconomic factors health behaviors and mortality: Results from a nationally representative prospective study of US adults. Journal of American Medical Association. 1998;279:1703–1708. doi: 10.1001/jama.279.21.1703. [DOI] [PubMed] [Google Scholar]
- Larson Ann, Bell Martin, Young Anne Frances. Clarifying the relationships between health and residential mobility. Social Science & Medicine. 2004;59(10):2149–2160. doi: 10.1016/j.socscimed.2004.03.015. [DOI] [PubMed] [Google Scholar]
- Laursen B, Paulkkinen L, Adams R. The Antecedents and Correlates of Agreeableness in Adulthood. Developmental Psychology. 2002;38:591–603. doi: 10.1037//0012-1649.38.4.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latner JD, Stunkard AJ. The Stigmatization of Obese Children: 40 years and Counting. Obesity Research. 2001;11:452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- Lim C. Social Networks and Political Participation: How Do Networks Matter? Social Forces. 2008;87:961–82. [Google Scholar]
- Harris Louis, et al. 1998 N.O.D./Harris Survey of Americans with Disabilities. New York: Louis Harris and Associates; 1998. [Google Scholar]
- Malouff JM, Thorsteinsson EB, Schutte NS. The Five-Factor Model of Personality and Smoking: A Meta-Analysis. Journal of Drug Education. 2006;36:47–58. doi: 10.2190/9EP8-17P8-EKG7-66AD. [DOI] [PubMed] [Google Scholar]
- Markides Kyriakos S, Lee David J, Ray Laura A, Black Sandra A. Physicians’ ratings of health in middle and old age: a cautionary note. Journal of Gerontology. 1993;48(1):S24–S27. doi: 10.1093/geronj/48.1.s24. [DOI] [PubMed] [Google Scholar]
- Markey CN, Markey PM, Erikson AJ, Tinsley BJ. Children’s Behavioral Patterns, the Five-Factor Model of Personality, and Risk Behaviors. Personality and Individual Differences. 2006;41:1503–13. [Google Scholar]
- Marmot Michael, Wilkinson Richard., editors. Social determinants of health. Oxford University Press; 2009. [Google Scholar]
- Mattila Mikko, Soderlund Peter, Wass Hanna, Rapeli Lauri. Healthy voting: The Effect of Self-Reported Health on Turnout in 30 Countries. Electoral Studies. 2013 in press. [Google Scholar]
- McAdam D, Paulsen R. Specifying the Relationship Between Social Ties and Activism. American Journal of Sociology. 1993;99:640–67. [Google Scholar]
- McClurg Scott D. Social networks and political participation: The role of social interaction in explaining political participation. Political Research Quarterly. 2003;56(4):449–464. [Google Scholar]
- McCrae RR, Costa PTJR. The Five-Factor Theory of Personality. In: John OP, Robins RW, Pervin LA, editors. Handbook of Personality: Theory and Research. New York: Guilford; 2008. pp. 155–81. [Google Scholar]
- McDonough Peggy, Amick Benjamin C. The social context of health selection: a longitudinal study of health and employment. Social science & medicine. 2001;53(1):135–45. doi: 10.1016/s0277-9536(00)00318-x. [DOI] [PubMed] [Google Scholar]
- Meyer Thoas, Buss Ullrich, Herrmann-Lingen Christopher. Role of Cardiac Disease Severity in the Predictive Value of Anxiety for All-Cause Mortality. Psychosomatic Medicine. 2010;72(1):9–15. doi: 10.1097/PSY.0b013e3181c64fc0. [DOI] [PubMed] [Google Scholar]
- Michael RT. Family Influences on Children’s Verbal Ability. In: Kalil A, DeLeire T, editors. Family Investments in Children’s Potential: Resources and Parenting Behaviors that Promote Success. New Jersey: Lawrence Erlbaum Associates; 2004. pp. 49–83. [Google Scholar]
- Mondak Jeffery J. Personality and the Foundations of Political Behavior. Cambridge University Press; 2010. [Google Scholar]
- Morenoff Jeffrey D, Lynch John W. What makes a place healthy? Neighborhood influences on racial/ethnic disparities in health over the life course. Critical perspectives on racial and ethnic differences in health in late life. 2004:406–449. [Google Scholar]
- National Research Council. From Neurons to Neighborhoods. The Science of Early Childhood Development. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- O’Brien Caughy Margaret. Health and Environmental Effects on the Academic Readiness of School Age Children. Developmental Psychology. 1996;32:515–22. [Google Scholar]
- Ojeda Christopher. Mental Disability and Political Voice: The Effect of Depression on Political Participation and Trust. Working paper 2013 [Google Scholar]
- Pacheco Julianna Sandell, Plutzer Eric. Stay in School, Don’t Become a Parent: Teen Life Transitions and Cumulative Disadvantages for Voter Turnout. American Politics Research. 2007;35(1):32–56. [Google Scholar]
- Pallas Aaron M. The Effects of Schooling on Individual Lives. In: Hallinan Maureen T., editor. Handbook of the Sociology of Education. New York: Kluwer; 2000. pp. 499–525. [Google Scholar]
- Palloni Alberto. Reproducing Inequalities: Luck, Wallets, and the Enduring Effects of Childhood Health. Demography. 2005;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Plutzer Eric. Becoming a Habitual Voter: Inertia, Resources, and Growth in Young Adulthood. The American Political Science Review. 2002;96(1):41–56. [Google Scholar]
- Rhodes RE, Smith NEI. Personality Correlates of Physical Activity: A Review and Meta-Analysis. British Journal of Sports Medicine. 2006;40:958–65. doi: 10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert Stephanie A, Booske BC. US Opinions on Health Determinants and Social Policy as Health Policy. American Journal of Public Health. 2011;101(9):1655–1663. doi: 10.2105/AJPH.2011.300217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehling MV. Weight-Based Discrimination in Employment: Psychological and Legal Aspects. Personnel Psychology. 1999;52:969–1017. [Google Scholar]
- Rosenstone Steven J, Hansen John Mark. Mobilization, Participation, and Democracy in America. New York: Macmillan; 1993. [Google Scholar]
- Schlozman Kay Lehman, Verba Sidney, Brady Henry E. The Unheavenly Chorus. Princeton University Press; 2012. [Google Scholar]
- Schur Lisa, Adya Meera. Sidelined or Mainstreamed? Political Participation and Attitudes of People with Disabilities in the United States. Social Science Quarterly. 2012:1–29. [Google Scholar]
- Shields Todd G, Schriner Kay Flecher, Schriner Ken. The Disability Voice in American Politics: Political Participation of People with Disabilities in the 1994 Election. Journal of Disability Policy Studies 1998 [Google Scholar]
- Sen Gita, Östlin Piroska, George Asha. Final Report from the Women and Gender Equity Knowledge Network. 2007. Unequal, unfair, ineffective and inefficient. Gender inequity in health: why it exists and how we can change it. [Google Scholar]
- Skocpol Theda. Boomerang: Clinton’s Health Security Effort and the Turn Against Government in the US Politics. New York: Norton; 1997. [Google Scholar]
- Schur Lisa. Disability and the Psychology of Political Participation. Journal of Disability Policy Studies. 1998;9:3–31. [Google Scholar]
- Stoker Laura, Kent Jennings M. Life-cycle transitions and political participation: The case of marriage. American Political Science Review. 1995:421–433. [Google Scholar]
- Teachman B, Gapinski K, Brownell KD. Stigma of Obesity: Implicit Attitudes and Stereotypes. Social Psychology 2001 [Google Scholar]
- Teachman BA, Brownell KD. Implicit Anti-Fat Bias Among Health Professionals: Is Anyone Immune? International Journal of Obesity. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- Verba Sidney, Schlozman Kay Lehman, Brady Henry E. Voice and equality: Civic voluntarism in American politics. Harvard University Press; 1995. [Google Scholar]
- Wagerman Seth A, Funder David C. Acquaintance Reports of Personality and Academic Achievement: A Case of Conscientiousness. Journal of Research in Personality. 2007;41:221–9. [Google Scholar]
- Wooldridge JM. Introductory Econometrics. 4. New York: South-Western; 2012. [Google Scholar]
- Yuker Harold E., editor. Attitudes toward Persons with Disabilities. New York: Springer; 1988. [Google Scholar]
- Zuckerman Alan S., editor. The social logic of politics: Personal networks as contexts for political behavior. Temple University Press; 2005. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.