Abstract
Gastro-esophageal adenocarcinomas (GEA) represent a severe global health burden and despite improvements in the multimodality treatment of these malignancies the prognosis of patients remains poor. HER2 overexpression/amplification has been the first predictive biomarker approved in clinical practice to guide patient selection for targeted treatment with trastuzumab in advanced gastric and gastro-esophageal junction cancers. More recently, immunotherapy has been approved for the treatment of GEA and PD-L1 expression is now a biomarker required for the administration of pembrolizumab in these diseases. Significant progress has been made in recent years in dissecting the genomic makeup of GEA in order to identify distinct molecular subtypes linked to distinct patterns of molecular alterations. GEA have been found to be highly heterogeneous malignances, representing a challenge for biomarkers discovery and targeted treatment development. The current review focuses on an overview of established and novel promising biomarkers in GEA, covering recent molecular classifications from TCGA and ACRG. Main elements of molecular heterogeneity are discussed, as well as emerging mechanisms of primary and secondary resistance to HER2 targeted treatment and recent biomarker-driven trials. Future perspectives on the role of epigenetics, miRNA/lncRNA and liquid biopsy, and patient-derived xenograft models as a new platform for molecular-targeted drug discovery in GEA are presented. Our knowledge on the genomic landscape of GEA continues to evolve, uncovering the high heterogeneity and deep complexity of these tumors. The availability of new technologies and the identification of promising novel biomarker will be critical to optimize targeted treatment development in a setting where therapeutic options are currently lacking. Nevertheless, clinical validation of novel biomarkers and treatment strategies still represents an issue.
Keywords: Gastro-esophageal cancer, Molecular biomarkers, HER-2, The Cancer Genome Atlas (TCGA), Asian Cancer Research Group (ACRG), Genomic profiling, Epigenomics, Immunotherapy, Liquid biopsy
Background
Gastric and esophageal adenocarcinomas, collectively referred to as gastro-esophageal adenocarcinomas (GEA), represents a severe global health issue. Gastric cancer (GC), in fact, ranks fifth among the most common malignancy in the world, and is the third leading cause of cancer-related death in both sexes worldwide [1]. Esophageal cancer (EC) on the other hand has a lower incident, ranking eighth among the most common cancers, but the overall mortality is fairly high (ratio of mortality to incidence of 0.88) [1]. Both malignancies are more frequent in males than in females and their incidence and mortality rates vary according to geographical regions, under the influence of several factors such as ethnicity, diet and infectious agents (i.e. Helicobacter pylori, Epstein-Barr Virus for GC); with the highest rates occurring in Eastern Asia. Although incidence of distal GC is declining over the past decades, incidence of upper third GC, junctional (GEJ) and lower third of the esophagus adenocarcinoma (EAC) are relatively increasing [2]. Despite recent improvements in the multidisciplinary and multimodality treatment, in fact, the overall prognosis for patients with GEA remains poor, with a global 5-year survival rate lower than 30% for GC and about 19% for EAC [3].
Moving from histo-pathological classifications, a great effort has been spent in recent years to define a genomic characterization of GEA, and to identify prognostic and predictive molecular biomarkers in order to better understand and represent the wide heterogeneity of these malignancies, and guide the development of effective targeted therapies. Major steps forward have been made for GC, with the identification first of HER2 overexpression and HER2/neu (ERBB2) amplification as predictive biomarkers for trastuzumab (Herceptin®; Genentech, San Francisco, California) efficacy in the metastatic setting, and more recently with the introduction of two novel genomic classifications by The Cancer Genome Atlas (TCGA) Research Network [4] and the Asian Cancer Research Group (ACRG) [5]. Thanks to this progress, different molecular subtypes of GC underlying different pathogenesis, genetic mechanisms and potentially druggable targets have been identified and novel therapeutic strategies are under development. Recently, based on microsatellite instability (MSI) and PD-L1 status as biomarkers, immunotherapy has been now integrated in the treatment of GEA. Nevertheless, the need to validate and implement promising molecular biomarkers in clinical practice is still critical in order to improve treatment selection and patients outcomes.
The present review focus on summarizing the recent developments, current trends and future perspectives on molecular biomarkers in gastro-esophageal cancer.
Molecular biomarkers in gastro-esophageal cancer: where are we coming from
Gastric cancer
Before the era of molecular biomarkers, GC has been classified by Lauren according to histological criteria identifying two different entities: the intestinal type and the diffuse type, plus a less common indeterminate type, with different phenotypes underlying different pathogenesis and prognosis [6, 7]. Although highly heterogeneous in treatment response, no predictive biomarker was available to guide therapeutic decisions for GCs before the discovery of HER2 overexpression/ERBB2 amplification and the introduction of targeted anti-HER2 treatment with trastuzumab.
HER2 is a receptor tyrosine kinase (RTK) belonging to the family of epidermal growth factor receptor (EGFR) coded by the proto-oncogene ERBB2, which plays an important role in cell differentiation, survival and proliferation [8]. The amplification of ERBB2 leads to an overexpression of HER2 promoting cancer cells survival, growth, migration and proliferation through the activation of the RAS/RAF/mitogen-activated protein kinase (MAPK) and the phosphatidylinositol-3 kinase/protein kinase-B/mammalian target of rapamycin (PI3K/AKT/mTOR) signalling pathways. The incidence of HER2 overexpression in GC ranges from 9 to 38% in most studies, depending on tumor location and histology [9–13], with higher frequencies in GEJ tumors and in intestinal type tumors [14–17]. The correlation between HER2 overexpression and tumor clinico-pathological features, however, is still debated, as some evidence suggests an association with cancer stage, tumor size, local invasion and nodal metastasis, not confirmed by other available data. The possible prognostic role of HER2 in GC is controversial as well. Some studies, in fact, have shown an association between HER2 overexpression and a worse prognosis, while others did not confirm a significant difference between HER2-positive and negative tumors [9, 11, 18–20]. In 2010, the international phase III randomized trastuzumab for gastric cancer (ToGA) trial, for the first time showed a significant overall survival (OS) improvement from the administration of trastuzumab, an anti-HER2 monoclonal antibody, in combination with platinum-based chemotherapy compared to chemotherapy alone in patients with HER2-positive advanced GEA (combining GC and GEJ tumors) [21]. In a post hoc exploratory analysis patients with the highest level of HER2 expression, measured as immunohistochemistry (IHC) 2+ and fluorescent in situ hybridization (FISH)+ or IHC 3+, derived the greatest benefit from trastuzumab compared to patients with low levels of HER2 expression via IHC despite a positive FISH for ERBB2 amplification (IHC 0 or 1 and FISH positive). Based on the results of this trial trastuzumab in combination with platinum-based chemotherapy has been approved for the first-line treatment of GEA with HER2 overexpression or ERBB2 amplification, and testing for HER2 status is recommended before starting treatment in all patients with advanced GEA who are candidates for HER2-targeted therapy [22]. Of note, recently the College of American Pathologists, American Society for Clinical Pathology, and American Society of Clinical Oncology have released official guidelines with recommendations for optimal HER2 testing and clinical decision-making in patients with GEA [23]. Results from ongoing trials investigating the activity of trastuzumab as well as a double-blockade strategy with trastuzumab plus pertuzumab, in combination with chemotherapy, in the neoadjuvant/perioperative setting (i.e. locally advanced gastric or GEJ HER2-positive tumors: NCT01196390, NCT02205047, NCT02581462), will potentially lead to further testing and treatment indications.
The anti-vascular endothelial growth factor receptor 2 (VEGFR-2) ramucirumab (Cyramza®, Eli Lilly and Company) is the second targeted agent which has been approved for the treatment of GC and GEJ tumors [24, 25]. To date, similar to other cancer types, no predictive biomarkers are available for anti-VEGFR treatment in GEA [26]. Of note, however, plasma levels of VEGF-A and Angiopoietin-2 (Ang-2), two well-known key drivers of tumor angiogenesis, alongside tumor neuropilin-1 expression, have been respectively reported as promising predictive and prognostic biomarkers in patients treated with bevacizumab in the phase III AVAGAST trial, investigating the addition of bevacizumab to chemotherapy in advanced GC. Interestingly, preplanned subgroup analyses showed a regional variability in these findings, possibly reflecting an underlying heterogeneity which may account, at least partially, for outcome differences observed in this trial between Asian and non-Asian patients [27–29]. Indeed, GC has the highest incidence in Eastern Asian countries (i.e. China, Japan, and Korea), however, Asian countries have consistently reported superior GC outcomes. The underlying reasons remain mostly unclear, possibly involving a complex interaction of ethnicity, epidemiological and biological factors, molecular heterogeneity and healthcare environment variability.
On the other hand, promising predictive molecular biomarkers for targeted treatments, such as EGFR and mesenchymal-epithelial transition factor receptor (MET) amplification, failed to prove their role in GC. EGFR is found to be amplificated in about 33% of GC, 30–60% of GEJ adenocarcinomas and 8–31% of distal EAC [30, 31], and has been evaluated as a potential target for treatment in several trials. Despite a strong rationale, anti-EGFRs, either monoclonal antibodies cetuximab and panitumumab, or small TKIs such as gefitinib and erlotinib, did not show any benefit in GEA [32, 33]. Of note, however, enrollment in these trials were not selected according to EGFR expression, thus results of an ongoing phase III trial investigating the anti-EGFR nimotuzumab as second-line treatment in EGFR IHC 2+ or 3+ recurrent or metastatic GC are awaited (NCT03400592). The prognostic impact of EGFR amplification remains controversial, as some authors have suggested a negative prognostic value [34], which has not been confirmed in other series. MET, the receptor of hepatocellular growth factor (HGF), plays a key role in several physiologic processes involving cell proliferation, survival and differentiation through the activation of multiple pathways including PI3K–AKT and RAS–MAPK signaling cascades [35]. Mutations or aberrant MET activation are associated with the development of several cancer types including GC. MET protein over-expression is present in up to 50% of advanced GC, and MET amplification can be found in up to 20% of GC [36], characterizing a more aggressive disease with poor prognosis [37]. Despite encouraging results in small phase II trials, MET-targeted inhibition was tested in phase III trials in MET-positive GEA with negative results [38, 39].
More recently, modern high through-put molecular technologies such as next generation sequencing (NGS) exploiting whole genome sequencing and providing more comprehensive and accurate tools for genome analysis, have become available. The use of these techniques has allowed the identification of several candidate genes mutations in known cancer-related genes in GC, such as TP53, PTEN, ARID1A, APC, CTNNB1, CDH1, PI3KCA and KMT2C [40, 41]. Moving from these data, a large effort was dedicated to defining distinctive molecular subtypes, based on genomic profiling, in order to dissect the complex heterogeneity of this disease and aid the development of novel biomarkers and targeted treatment to improve patients outcome. The TCGA and ACRG classifications, developed to address this issue, will be discussed in detail in the next sections alongside subtypes-related novel biomarkers and targeted therapies.
Esophageal cancer
No molecular biomarker is currently approved in clinical practice for EAC excepting HER2 in GEJ cancers. Recently, however, multiple studies have explored the genomic profiling of EAC highlighting the presence of mutations in several cancer-related genes and distinctive gene signatures with could potentially translate in the development of novel biomarkers for targeted treatment. A study from Dulak et al. analyzed the genomic profile of 149 EACs using whole-exome sequencing. Main genes identified as mutated in this tumor series were TP53 (72%), ELMO1 (25%), DOCK2 (12%), CDKN2A (12%), ARID1A (9%), SMAD4 (8%) and PIK3CA (6%). Additionally, amplifications of several oncogenes such as KRAS (21%), HER2 (19%), EGFR (16%), CND1 (10%) and MET (6%) were identified, as well as loss of SMAD4 (34%), CDKN2A (32%) and ARID1A (10%) [42]. Another study compared the gene signature of esophageal squamous cell carcinoma and EAC, highlighting a higher prevalence of HER2 and EGFR amplification, TGF-β signaling activation and RAS/MEK/MAPK pathway activation in EAC [43]. On the other hand, PI3K/AKT/MTOR signaling, fibroblast growth factor (FGF) signaling, epigenetic regulation pathways and the NOTCH signaling pathway showed a lower frequency in EAC. Additionally, TP53 and CDKN2A were highly altered in both tumor types. Finally, based on data from the International Cancer Genome Consortium project, Secrier et al. proposed a classification with potential therapeutic relevance based on a whole-genome sequence analysis of 129 EAC samples [44]. Results of the analysis showed a wide tumor heterogeneity with high prevalence of copy number alterations and frequent large-scale rearrangements. Based on their mutational signature the authors were able to identify three distinct molecular subtypes: a dominant T>G mutational pattern associated with a high mutational load and neoantigen burden (mutagenic, 53%), a C>A/T dominant mutational pattern with evidence of an aging imprint (29%) and a DNA damage repair (DDR) impaired pattern characterized by a BRCA-like enriched signature with prevalent defects in the homologous recombination pathway (18%). Co-amplification of RTKs and/or downstream mitogenic pathways was common (i.e. a simultaneous amplification of ERBB2 and MET), underlining a rationale for dual targeted inhibition for the treatment of these tumors which proved to be effective in in vitro experiments by the same authors. Additionally, in in vitro models, the DDR-impaired subgroup appeared to be sensitive to DNA damage repair-targeted treatment, such as the combination of PARP inhibitors with DNA-damaging agents. WEE1/CHK1 and G2/M-phase checkpoint regulators, were also identified as potential targets in this study.
The emerging scenario for EAC is thus characterized by genomic instability with complex rearrangements leading to a significant degree of heterogeneity between patients. Although promising, however, data on genomic profiling and potential genetic biomarkers in EAC still need further validation.
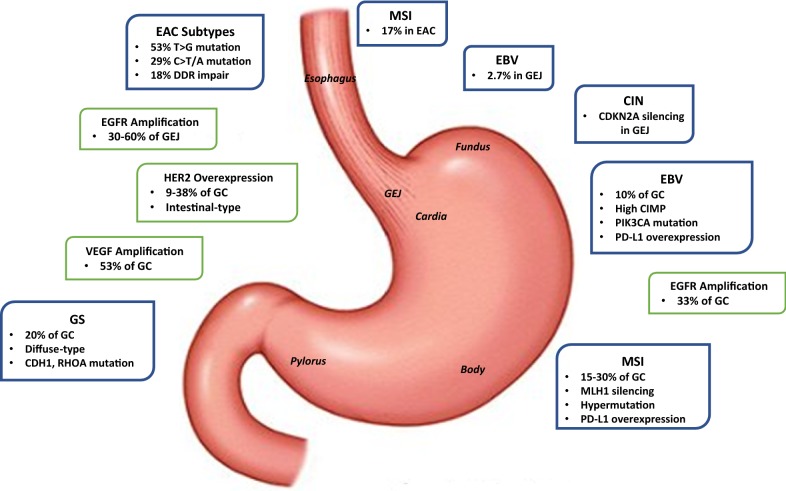
Main biomarkers and trials of targeted therapies in GEA are summarized in Table 1. A schematic representation of main biomarkers and molecular characteristics according to tumor location and genomic subtype (further discussed in the next sections) are illustrated in Fig. 1.
Table 1.
Main biomarkers and trials of targeted therapies in gastric and esophageal adenocarcinoma
| Target | Biomarker | Targeted agent | Study (treatment line) | Regimen | Primary endpoint | Positive study Y/N | Refs. |
|---|---|---|---|---|---|---|---|
| HER2 | HER2 amplification/ overexpression | ||||||
| Trastuzumab | ToGA (1st) | Trastuzumab + CX vs CX | OS | Y | [21] | ||
| Lapatinib | TRIO-013/LOGiC (1st) | Lapatinib + XELOX vs XELOX | OS | N | [95] | ||
| Lapatinib | TyTAN (2nd) | Lapatinib + paclitaxel vs paclitaxel | OS | N | [95] | ||
| T-DM1 | GATSBY (2nd) | T-DM1 vs taxane | OS | N | [97] | ||
| Pertuzumab | JACOB (1st) | Pertuzumab + trastuzumab + CF vs trastuzumab + CF | OS | N | [98] | ||
| VEGF-A and VEGFR-2 | – | ||||||
| Bevacizumab | AVAGAST (1st) | Bevacizumab + CX vs CX | OS | N | [29] | ||
| Ramucirumab | REGARD (2nd) | Ramucirumab vs placebo | OS | Y | [24] | ||
| Ramucirumab | RAINBOW (2nd) | Paclitaxel + ramucirumab vs Paclitaxel | OS | Y | [25] | ||
| EGFR | EGFR amplification | ||||||
| Cetuximab | EXPAND (1st) | Cetuximab + CX vs CX | PFS | N | [32] | ||
| Panitumumab | REAL-3 (1st) | Paniumumab + EOX vs EOX | OS | N | [33] | ||
| MET and HGF | MET amplification | ||||||
| Rilotumumab | RILOMET-1 (1st) | Rilotumumab + ECX vs ECX | OS | N | [38] | ||
| Onartuzumab | METGastric (1st) | Onartuzumab + FOLFOX vs FOLFOX | OS | N | [39] | ||
| FGFR2 | FGFR2 polysomy/gene amplification | ||||||
| AZD4547 | SHINE (2nd) | AZD4547 vs paclitaxel | PFS | N | [73] | ||
| PD-1 | – | ||||||
| Nivolumab | ATTRACTION-2 (ONO-4538-12) (≥ 3rd) | Nivolumab vs placebo | OS | Y | [81] | ||
| PD-L1 expression | |||||||
| Pembrolizumab | KEYNOTE-059 (≥ 3rd cohort 1; 1st cohort 2 and 3) | Pembrolizumab (cohort 1); Pembrolizumab + CF (cohort 2); Pembrolizumab (cohort 3) | ORR (cohort 1 and 3) | Y | [80] | ||
| Pembrolizumab | KEYNOTE-028 (after failure on standard therapy or if standard therapy not appropriate) | Pembrolizumab | ORR | Y | [82] | ||
| PD-L1 | – | ||||||
| Avelumab | JAVELIN Gastric 300 (3rd) | Avelumab + BSC vs CT | OS | N | [87] |
BSC best supportive care, CF cisplatin + fluoropyrimidine, CT chemotherapy, CX cisplatin + capecitabine, EGFR epidermal growth factor receptor, EOX epirubicin + oxaliplatin + capecitabine, FGFR fibroblast growth factor receptor, FOLFOX 5-fluorouracil + leucovorin + oxaliplatin, HGF hepatocyte growth factor, ORR overall response rate, OS overall survival, PD-1 programmed cell death protein 1, PD-L1 programmed death-ligand 1, PFS progression-free survival, VEGF vascular endothelial growth factor, VEGFR vascular endothelial growth factor receptor, XELOX capecitabine + oxaliplatin
Fig. 1.
Schematic representation of main biomarkers and molecular characteristics according to tumor location and genomic subtype
TCGA gastric cancer subtypes
In 2014, the TCGA network used six genomic and molecular platforms to comprehensively characterize 295 gastric tumors into four molecular subtypes: Epstein-Barr virus (EBV)-positive tumors (9%), microsatellite instable (MSI) tumors (22%), genomically stable (GS) tumors (20%), and tumors with chromosomal instability (CIN) (50%) [4]. Their goal was to develop a robust molecular classification of GC and to identify aberrant pathways and candidate drivers of unique classes of GC. Later, Sohn et al. [45]. conducted a follow-up study to investigate the clinical significance of TCGA subtypes. They discovered that the EBV subtype was associated with the best prognosis, and GS subtype was associated with the worst prognosis. Furthermore, patients with MSI and CIN subtypes had poorer overall survival than those with EBV subtype, but better overall survival than those with GS subtype. Sohn et al. also evaluated differences in response to chemotherapy between the four TCGA subtypes, and discovered that patients with the CIN subtype derived the greatest benefit from adjuvant chemotherapy, whereas those with the GS subtype derived the least benefit from adjuvant chemotherapy. Hence, the TCGA subtypes offer useful biomarkers for development of targeted therapies for GC patients with different prognostic outcomes and responses to chemotherapy. The four TCGA subtypes are described in detail below.
EBV-positive
Epstein-Barr virus is a DNA virus infecting over 90% of the global population, and is currently categorized as a group-1 carcinogen associated with many cancers, including nasopharyngeal carcinomas, Burkitt’s lymphoma and Hodgkin’s lymphomas [46]. EBV was first discovered in GC in 1990, with an annual incidence of 75,000–90,000 cases per year [46]. EBV is not yet reported in esophageal adenocarcinomas; however, its prevalence in GC is approximately 10%, and in gastroesophageal junction cancers is reported to be 2.7% [47]. EBV-positive GC is more prevalent among males and younger patients [46]. Although several reports have concluded that EBV is predominantly found in proximal gastric regions [48], the TCGA cohort found EBV-positive GC to be localized to the gastric fundus or body [4]. Based on the TCGA data, EBV associated GCs have the best prognosis [45].
It is postulated that EBV enters gastric epithelia through the oropharynx and establishes a lifelong virus carrier state, called latent infection, where it persists as an episome within the nucleus and is propagated to daughter cells during cell division [46]. During latency, EBV induces extensive CpG island methylation, including both promoter and non-promoter islands of the human genome [49]. Unsupervised clustering of CpG methylation performed by TCGA revealed that all EBV-positive tumors exhibited extreme CpG island methylator phenotype (CIMP), which was distinct from that in the MSI subtype [4]. For instance, EBV-positive tumors have hypermethylation of the CDKN2A (p16) promoter, but lack MLH1 hypermethylation [4]. A comprehensive analysis of promoter methylation status of 51 gastric carcinoma cases was conducted by Shinozaki and colleagues [50], who subsequently classified GCs into three epigenotypes characterized by different sets of methylation genes: EBV-positive/extensively high-methylation, EBV-negative/high-methylation and EBV-negative/low-methylation. Methylated genes specific for the EBV-positive subtype included CXXC4, TIMP2 and PLXND1. COL9A2, EYA1 and ZNF365 were highly methylated in EBV-positive and EBV-negative/high-methylation subtypes, whereas AMPH, SORC33 and AJAP1 were frequently methylated in all epigenotypes. They discovered that EBV-positive GCs had approximately 270 genes which were uniquely methylated. Interestingly, MLH1 was frequently methylated (46%) in the EBV-negative/high-methylation phenotype, whereas none of the EBV associated GC cases showed MLH1 methylation. Similar results were observed in the TCGA analysis, where EBV-positive GCs lacked the MLH1 hypermethylation characteristic of MSI-associated CIMP.
In addition to hypermethylation, EBV-positive GCs also exhibit elevated levels of programmed death ligands 1 and 2 (PD-L1/2) [46]. PD-L1 is encoded by CD274 and PD-L2 is encoded by PDCD1LG2, both of which are immunosuppressant proteins inhibiting cytokine production and cytolytic activities of CD4 and CD8 T cells [51]. Therefore, inhibitors of PD-L1/2 are currently being evaluated as targets for augmenting immune response against cancer cells. Both these genes are located on chromosome 9p24.1, and were notably amplified in the EBV subtype of TCGA cohort [4]. Evaluation of mRNA by TCGA also showed increased expression of PD-L1 and PD-L2 in this subtype. This overexpression characterizes the immune signature of EBV-positive GCs, which is known to have a prominent lymphoid infiltration of the stroma and high density of tumor infiltrating lymphocytes (TILs), creating a balance between host immune evasion through PD-L1/2 overexpression, and host immune response [46]. Hence, EBV subtype is a promising candidate for anti-PD-1/PD-L1 therapy in gastroesophageal cancers.
Somatic mutations unique to EBV-positive GCs include activation of BMP (bone morphogenetic protein) signaling [52], amplification of JAK2, MET, ERBB2, non-silent PIK3CA mutations, and mutations in ARID1A and BCO [4]. TP53 mutations were rare in EBV subtype. Hence, EBV-positive GCs could be treated with drugs targeting the BMP/SMAD, JAK2, PIK3CA, MET and ERBB pathways. In the TCGA analysis, PIK3CA mutations were more dispersed in EBV-positive cancers, but localized in the kinase domain (exon 20) in EBV-negative cancers. TCGA investigators also reported that the two most marked features of EBV-positive cancers are diminished hypoxia-inducible factor 1α-related activity and diminished ERBB receptor signaling [52]. Furthermore, the EBV-miRNA cluster is postulated to promote cancer cell resistance to hypoxia and poor nutrient supply along with invasiveness [53]. Hence, angiogenesis inhibitors might also prove to be useful in this subtype.
Microsatellite instability
Approximately 15–30% of GC [54], and 17% of GEJ cancer patients [55] have MSI. The MSI phenotype results from mutations in repetitive sequences due to a defective DNA mismatch repair (MMR) system [54]. This can occur in the context of hereditary syndromes, such as Lynch syndrome, with germline mutations in MLH1, MSH2, MSH6 or PMS2, or it can occur sporadically through somatic mutations in MMR genes [54]. Epigenetic silencing of MLH1 by promoter hypermethylation is the main mechanism leading to MMR deficiency in both sporadic and familial MSI GC cases.
In the TCGA cohort, most MSI patients were female (56%), and were of advanced age (median age 72) [4]. Furthermore, patients with MSI had poorer overall survival than the EBV subtype, but better than the GS subtype [45]. A German study conducted by Mathiak et al. examined 452 GC patients, and discovered that MSI was significantly more prevalent in elderly patients, distal stomach, and was associated with a significantly lower number of lymph node metastases with a significantly better overall and tumor-specific survival [56].
Similar to the EBV subtype, MSI also displays overexpression of PD-L1 [57]. Strong immunogenicity associated with MSI GC has shown improved treatment responses to PD-1 inhibitors among this subtype [58]. Hence, PD-1 inhibitors, such as pembrolizumab, are now approved for use in metastatic MSI GC s and novel immunotherapy options continue to be investigated in MSI. However, treatment benefits and prognosis may be stage dependent. For instance, the CLASSIC trial investigated 592 GC patients, and discovered that MSI status correlated with favorable prognosis in patients with stage II and III GC, but did not show benefits from adjuvant chemotherapy [59].
The successful response to immunotherapy in MSI patients may be related to increased tumor mutational burden associated with this subtype [57]. MSI is characterized by elevated mutation rates, including mutations of genes encoding targetable oncogenic signaling proteins [60]. MSI GCs have been shown to harbor more mutations in genes that act as tumor suppressors or oncogenes [61]. TCGA HotNet analysis of genes mutated within MSI tumors revealed common alterations in major histocompatibility complex class I genes, including beta-2 microglobulin (B2M) and HLA-B [4]. B2 M mutations result in loss of expression of HLA class 1 complexes, which benefits hypermutated tumors by reducing antigen presentation to the immune system [62]. Targetable amplifications were not identified in MSI, however, mutations in PIK3CA, ERBB3, ERBB2, ARID1A, and EGFR were noted [4]. Integrated exome sequencing by Liu and colleagues [63] revealed that MSI GCs have frequent mutations in TP53, ACVR2A, PTEN, PIK3CA, KRAS, ERBB2, ZBTB1, TRAPPC2L, GPR39, GPR85, and CHRM3. Interestingly, BRAF V600E mutations were not observed in MSI GCs, which is commonly seen in MSI colorectal cancer [4].
Genomically stable
When the TCGA classified tumors based on the number of somatic copy-number alterations, one of the classifications was genomically stable (GS) subtype. The GS subtype is characterized by low mutation rates and low copy-number alterations [4]. It is diagnosed at a younger age (median age 59), and has an enrichment of the diffuse histological subtype of GC [4]. As diffuse-type GC are known to be aggressive and invasive, their rapid tumor progression may result in a diagnosis at an early age and may not provide enough time to accumulate mutations [64]. Prognostically, GS subtype is associated with the worst overall survival and recurrence-free survival among the four TCGA subtypes. It has also been shown to be resistant to adjuvant chemotherapy [45].
The clinical outcomes observed in GS could be a result of the molecular landscape of this subtype. For instance, NUPR1 is an activated transcription regulator in GS subtype, and recent studies have demonstrated that it enhances chemo-resistance in multiple cancers [45]. From the TCGA data, CDH1 (Cadherin 1, encoding E-cadherin) was found to be mutated in 11% of all GCs, with 37% of all GS GC having a CDH1 mutation [4]. Genomically stable subtype also had frequent mutations in ARID1A, CLDN18, CDH1, and RHOA (Ras homolog family member A). ARID1A is a tumor suppressor encoding a subunit for switch-sucrose nonfermentable (Swi-SNF) box, and is crucial for chromatin remodeling [65]. Loss of expression of ARID1A has widespread implications in tumor development, and is associated with lymphatic invasion, MSI, and poor prognosis [64]. Therefore, ARID1A could be useful for targeted treatment potentials. RHOA also plays significant roles in cell migration, adhesion, cell survival, cell division, gene expression and vesicle trafficking, thereby guiding tumor cell biology [66]. However, the prognostic impact of RHOA in GC is currently unknown [67]. CLDN18-ARHGAP fusions were found in 15% of GS subtype, and were mutually exclusive from RHOA mutations [64].
Clustering mutations based on pathways in the GS subtype reveals interesting findings. It was discovered that there is elevated expression of mitotic network components such as AURKA/B and E2F, targets of MYC activation, FOXM1 and PLK1 signaling and DNA damage response pathways across all subtypes, but to a lesser degree in GS tumors [4]. However, the GS subtype exhibited elevated expression of cell adhesion pathways, including the B1/B3 integrins, syndecan-1 mediated signaling, and angiogenesis-related pathways [4]. These unique patterns of mutations in the GS subtype offer new candidate therapeutic targets, which warrant further investigation.
Chromosomal instability
Chromosomal instability GCs are classified based on degree of aneuploidy, comprising approximately 50% of GC [4]. CIN is characterized by highly variable chromosomal copy numbers, without exhibiting high mutation rates. CIN subtype tumors are frequent at the gastroesophageal junction/cardia, correlate with the Lauren intestinal histologic variant, show marked aneuploidy, and harbor focal amplifications of RTKs, in addition to recurrent TP53 mutations and RTK–RAS activation [4]. Molecular characterization has identified CIN gastric subtype to be similar to esophageal adenocarcinoma, comprising one large subgroup [68]. As the prognosis of CIN is similar to that of MSI subtype, it is worthwhile to explore targeted treatments in this subtype based on its unique molecular profile [45].
As TP53 mutations cause chromosomal instability, it is consistent with the finding from TCGA that CIN GCs have an enrichment of TP53 mutations and recurrent chromosomal amplifications and deletions. RTKs amplification is a signature of CIN GC. Frequent amplifications have been found in the genomic regions of RTK–RAS, which harbors EGFR, ERBB2, ERBB3, MET, VEGFA, and KRAS [4]. Hence, it is worthwhile to explore the benefits of the HER2 monoclonal antibody, trastuzumab, in CIN tumors harboring ERBB2 amplification. Furthermore, VEGF-A inhibitors could also be used in this subgroup, as recurrent amplification of VEGFA was notable in the TCGA cohort. Other amplified genes in CIN include oncogenic transcription factors, such as MYC, GATA4, and GATA6, and cell cycle regulators including CCNE1, CCND1, and CDK6 [4]. Hence, cyclin-dependent kinase inhibitors could also be promising in CIN. Chromosomal deletions have also been found in CIN, in genomic regions containing FHIT (Fragile histidine triad), WWOX (WW domain containing oxidoreductase), STK3 (Serine/threonine kinase 3), CDH1, CTNNA1 (Catenin alpha 1), PARD3 (Par-3 family cell polarity regulator), and RB1 (retinoblastoma 1) [64].
Amplification of fibroblast growth factor receptor 2 (FGFR2) is also frequent in CIN GCs [4], and is of considerable interest due to clinical trials investigating FGFR inhibitors. FGFR is a tyrosine kinase receptor, which binds to FGF and triggers cell growth, proliferation, differentiation, migration and survival [69]. FGFR amplification in GC is associated with poor prognosis and lymphatic invasion [70]. In EGJ adenocarcinoma, however, FGFR2 expression, but not amplification, is associated with poor survival [71]. The FGFR pathway has been of interest to researchers, leading to several FGFR inhibitors currently under investigation in preclinical and clinical trials, with tolerable safety profiles to date. FGFR inhibitors have been shown to enhance tumor sensitivity to conventional chemotherapeutic drugs such as 5-fluorouracil, irinotecan, paclitaxel, and etoposide [72]. Recent pharmaceutical development has led to highly selective FGFR inhibitors, including drugs such as AZD4547, which, despite encouraging preliminary results, unfortunately failed to improve progression free survival (PFS) versus chemotherapy as second-line treatment in GC with FGFR2 amplification/polysomy [73]. Of note, the authors highlighted a considerable intra-tumor heterogeneity for FGFR2 amplification and poor concordance between FGFR2 amplification/polysomy and FGFR2 expression, suggesting the need for alternative biomarker testing. Another phase II study (NCT02699606) examining selective FGFR inhibitor, erdafitinib, is also ongoing with preliminary results still pending. In addition to highly selective FGFR inhibitors, clinical trials using multi-kinase inhibitors with pan-FGFR inhibition are ongoing [72]. Among these, dovitinib (TKI258) is currently being investigated in several phase I and II clinical trials (NCT01791387, NCT01719549, NCT02268435) including patients with FGFR2 amplification and GC [69]. Overall, FGFR2 amplification in gastroesophageal cancers presents an exciting opportunity for testing these novel drugs, thereby, improving patient prognosis and future outlooks for these patients.
ACRG molecular subtypes
On May, 2015, the ACRG published a molecular classification of GC [5], which is based on a large sample size (300 cases) and integrated molecular data from whole-genome sequencing, gene expression profiling, genome-wide copy number microarrays and targeted gene sequencing. By the integration of the data analysis, ACRG classified GC into four distinct molecular subtypes, which are associated with distinct genomic alterations, survival outcome and recurrence patterns after surgery [74]. Importantly, they confirmed the presence of the proposed molecular subtypes in previously published GC cohorts: the TCGA gastric cohort [75] and the gastric cancer Project’08 Singapore cohort [76], which suggested that the ACRG molecular subtypes could be reproduced in other GC cohorts.
Asian Cancer Research Group gene expression signatures defined four molecular subtypes of GC, which were different from the TCGA subtypes: MSI (N = 68), epithelial-to-mesenchymal transition (microsatellite stable (MSS)/EMT, N = 46), MSS/TP53 positive (N = 79) and MSS/TP53 negative (N = 107). MSI tumors typically have an intestinal-type by Lauren classification (> 60% of subjects) and show MLH1 loss of RNA expression and an elevated DNA methylation signature, occurred predominantly in the antrum (75%), and > 50% of subjects were diagnosed at an early stage (I/II); MSS/EMT tumors typically have a diffuse-type by Lauren classification at stage III/IV, include a large set of signet ring cell carcinomas, and show CDH1 loss of expression, occurred at a significantly younger age; EBV infection occurred more frequently in the MSS/TP53+ group. In addition, the authors observed that the MSI subtype had the best prognosis, followed by MSS/TP53+ and MSS/TP53−, with the MSS/EMT subtype showing the worst prognosis of the four (log-rank, P = 0.0004). The MSS/EMT group had a higher chance of recurrence compared to the MSI group (63% versus 23%). When they looked at the first site of recurrence, they observed a higher percentage of subjects with peritoneal seeding in the MSS/EMT GC subtype and liver-limited metastasis in the MSI and MSS/TP53− subtypes, which may have a huge impact on the clinical practice.
Regarding the somatic mutations associated with each ACRG group, the authors observed that the MSI subtype, similar to TCGA, was associated with the presence of hypermutation, with mutations in ARID1A (44.2%), the PI3K-PTEN-mTOR pathway (42%), KRAS (23.3%) and ALK (16.3%). The EMT subtype had a lower number of mutation events when compared to the other MSS groups. The MSS/TP53− subtype showed the highest prevalence of TP53 mutations (60%), with a low frequency of other mutations, as well as focal amplification of ERBB2, EGFR, CCNE1, CCND1 whereas the MSS/TP53+ subtype showed a relatively higher prevalence (compared to MSS/TP53−) of mutations in APC, ARID1A, KRAS, PIK3CA and SMAD4. Of note, ERBB2 amplification was seen in 17.4% of MSS/TP53− tumors, compared to MSS/TP53+ (3.0%), MSI (0.0%) and MSS/EMT (0.0%, P = 0.0001). These findings implied that the subtype of MSS/TP53− maybe suitable for approved HER2-targeting agent, such as trastuzumab [21].
The authors compared the ACRG subtypes with the TCGA genomic subtypes. When applied to both ACRG and TCGA data sets, they observed similarities among MSI tumors in both data sets, and they showed that the TCGA GS, EBV+ and CIN subtypes were enriched in ACRG MSS/EMT, MSS/TP53+ and MSS/TP53− subtypes, respectively. Furthermore, the authors observed that the tumors classified as the TCGA CIN subtype were present across all ACRG subtypes in the TCGA data set, while tumors classified as the GS subtype in the TCGA set were present across all ACRG subtypes in the ACRG data set. Nevertheless, the ACRG researchers saw a substantially lower percentage of Lauren’s diffuse-subtype cases in the TCGA cohort (24% in TCGA versus 45% in ACRG) with the majority (57%) of Lauren’s diffuse-subtype cases present in the TCGA GS group but only 27% cases present in the ACRG MSS/EMT subtype. In addition, although CDH1 mutations were highly prevalent in the TCGA GS subtype (37%), they were infrequent in the ACRG MSS/EMT subtype (2.8%), suggesting that the TCGA GS type is not equivalent to the ACRG MSS/EMT subtype. Such findings suggest that the TCGA and ACRG classification systems are related but distinct [77].
Biomarkers in gastro-esophageal cancer: where are we going
Main promising biomarkers and future directions in the field discussed in the following sections are summarized in Table 2.
Table 2.
Promising future biomarkers
| Biomarker | Description | Potential value | Refs. |
|---|---|---|---|
| HER2 loss | Loss of HER2 overexpression after anti-HER2 treatment | Predictive: secondary resistance to anti-HER2 agents | [102] |
| EGFR, MET, KRAS, ERBB3, CCNE1, CDK6, CCND1, FGFR2 and PIK3CA alterations, loss of PTEN | Secondary driver alterations (mutations/amplification) co-occurrent with HER2 amplification in GEA | Predictive: primary resistance to anti-HER2 Potential target for combined blockade |
[98–101] |
| MYC, EGFR, FGFR2 and MET amplifications | Acquired alterations under anti-HER2 treatment pressure | Predictive: secondary resistance to anti-HER2 agents Potential target for novel treatment strategies |
[103, 104] |
| Liquid biopsy | Mutational analysis of circulating tumor DNA | Molecular profiling and identification of predictive mutations for targeted treatments at baseline Dynamic monitoring of treatment response/disease progression Early detection of secondary resistance |
[111–117] |
| DNA methylation | Aberrant promoter DNA methylation in target genes | Diagnostic value Negative prognostic value Possible predictive value and role as novel treatment target |
[118–120] |
| miRNA | Micro RNA: short noncoding single-stranded RNA molecules, with post-transcriptional regulatory functions | Diagnostic and prognostic value Possible predictive value and role as novel treatment target |
[124–129] |
| lncRNA | Long noncoding RNA: noncoding single-stranded RNA molecules, > 200 nucleotides, involved in cancer development and metastases | Possible diagnostic and prognostic value Possible predictive value and role as novel treatment target |
[125, 130–132] |
| PDX models | Patient-derived xenograft animal models with defined molecular signatures | Predictive: preclinical studies with targeted drugs | [133, 134] |
Microsatellite instability and PD-L1 status: immunotherapy in GEA
Over the last year the groundbreaking success of immunotherapy with checkpoint inhibitors has opened a new era in the treatment of MSI-H tumors, including GEA.
Based on the positive results of the KEYNOTE-059 trial, the anti-PD-1 monoclonal antibody pembrolizumab (Keytruda®, Merck & Co., Inc.) has been approved by the Food and Drug Administration (FDA) for the treatment of patients with programmed cell death-ligand 1 (PD-L1)-positive (> 1%) advanced GC or GEJ adenocarcinoma [78, 79]. A pre-planned analysis of the study, in fact, showed a significantly higher response rate in PD-L1-positive tumors when compared to PD-L1 negative ones.
More recently the Japanese Ministry of Health, Labor and Welfare (MHLW) approved nivolumab (Opdivo®, Bristol-Myers Squibb), another anti-PD-1 monoclonal IgG4 antibody, for the treatment of unresectable advanced or recurrent GC progressing after chemotherapy. The approval was based on positive results of the phase III ATTRACTION-2 (ONO-4538-12) trial, enrolling 493 Asian patients with advanced or recurrent gastric or GEJ cancer refractory to at least two previous chemotherapy. This study showed a significant reduction in patients’ risk of death and an increased overall survival (OS) rate at 12 months from nivolumab when compared to placebo [80]. Notably, no predictive biomarker has been required for this indication.
Data on immunotherapy in esophageal cancer are available as well. In the multicohort phase Ib KEYNOTE-028 trial, in fact, pembrolizumab as single agent has been tested also in a series of PD-L1-positive esophageal cancer after failure of standard chemotherapy (including both squamous cell carcinomas and EAC). Promising results showed an overall response rate of 30.4 and 52.2% in squamous cell carcinoma and EAC, respectively, with a 12-month progression free rate of 21.7%, in an heavily pretreated patient population [81].
On the other hand, anti-CTLA-4 agents monotherapy (i.e. ipilimumab and tremelimumab) showed higher toxicity and lower efficacy than anti-PD-1 in EGA [82, 83]. Combined therapy with anti-CTLA-4 antibodies and anti-PD-1, however, have been tested with encouraging results and is currently the object of further investigation (NCT02872116).
Additionally, pembrolizumab is currently under investigation in several different settings. The phase III KEYNOTE-06 compared pembrolizumab versus paclitaxel as second-line treatment in patients with advanced GC [84]; recently released updates from this study showed no significant benefit in this setting. The ongoing phase III KEYNOTE-062 is testing pembrolizumab as a monotherapy and in combination with chemotherapy in the first-line treatment of PD-L1–positive advanced GC or GEJ cancer, while the phase III KEYNOTE-585 is evaluating the combination of pembrolizumab with chemotherapy in the neoadjuvant and adjuvant settings.
Another strategy under study for immunotherapy in GEA is targeting PD-L1. Avelumab, a fully human anti-PD-L1 IgG1 antibody, has been investigated as a first-line maintenance or second-line treatment in patients with advanced GC or GEJ cancer with promising results (NCT01772004) [85]. Unfortunately, it was recently announced that the phase III JAVELIN Gastric 300 trial (NCT02625623), investigating avelumab as a third-line treatment advanced GC and GEJ adenocarcinoma, unselected for PD-L1 expression, failed to meet its primary endpoint (OS) [86]. Results of the phase III JAVELIN Gastric 100 trial evaluating avelumab as first-line maintenance therapy following induction chemotherapy in gastric or GEJ cancer are awaited.
The relevance of testing for MSI-H/dMMR status or PD-L1 expression, thus, has become crucial in GEA since eligible patients can now receive immunotherapy as a standard treatment. Of note, based on recent molecular subtypes, EBV-positive and MSI-H GCs emerge as the best candidates for immunotherapy based on the increased PD-L1 expression associated with these subtypes and the high tumor mutational load in MSI-H GEA, which has been shown to correlate with a greater benefit from anti-PD-1/PD-L1 blockade [87]. Nevertheless, new strategies and novel therapeutic targets are needed to increase treatment options for GEA patients. A promising novel biomarker, V-domain Ig suppressor of T-cell activation (VISTA), also known as PD1 homolog (PD1H), has been recently analyzed in GC. VISTA expression was present in 8.8% out of 464 analyzed samples, and was associated with clinical and molecular features such as Lauren phenotype, tumor localization, EBV infection, KRAS and PIK3CA mutational status and PD-L1 expression [88]. A combined blockade of VISTA and PD-1 might thus be a promising treatment option in these patients,
Several additional clinical trials investigating the efficacy of immune checkpoint inhibitors in GEA, in different settings and exploring different treatment strategies and combinations with other agents, are ongoing and can be found reviewed in dedicated papers [89–93].
Beyond HER2: primary and acquired resistance to trastuzumab
As aforementioned, trastuzumab in combination with chemotherapy has been the first targeted therapeutic to demonstrate a survival improvement in patients with advanced HER2-positive GEA. However, not all HER2-positive patients respond to trastuzumab and most patients eventually develop an acquired resistance to this drug during treatment. Furthermore, alternative targeted anti-HER2 strategies, conversely from other tumor types (i.e. HER2-positive breast cancer) failed to show significant benefit in the treatment of GEA. For instance, both lapatinib, an oral tyrosine kinase inhibitor (TKI) dual inhibitor of HER2 and EGFR, and trastuzumab-emtansine (T-DM1), an antibody-drug conjugate of trastuzumab and emtansine a microtubule inhibitor, failed to show a significant survival improvement in addition to chemotherapy compared to chemotherapy alone in this setting [94–96]. Other agents such as pertuzumab and afitinib are currently being evaluated in a phase III (NCT01358877, NCT01774786) and a phase II (NCT01522768) clinical trial, respectively, in the second-line setting following first-line trastuzumab therapy, after the addition of pertuzumab to trastuzumab plus chemotherapy in the first-line setting failed to demonstrate a significant survival benefit [97]. Although the exact mechanisms underlying primary and acquired resistance to HER2 targeted therapy are still under study, intra-tumor heterogeneity and the activations of downstream signaling pathways including several RTKs seem to be involved in tumor escape from HER2-blockade.
As highlighted in previous sections, recent genomic studies have disclosed the high degree of complexity of GEA genomic landscape underlining the challenges of biomarker assessment in these tumors. Several secondary alterations in key cancer genes have been reported to occur frequently in HER2-positive GEA. Among these EGFR, MET, ERBB3, CCNE1, CDK6, CCND1, and PIK3CA [98]. Notably the co-occurrence of these alterations has been showed to confer resistance to HER2-targeted treatment in vitro, which can be reversed by combined blockade of HER2 and secondary driver mutations, thus suggesting a promising rationale for combined targeted therapies to overcome primary HER2 resistance in HER2 positive tumors. Indeed, in a small case series, a patient with a co-amplification of HER2 and MET was treated with a combination of trastuzumab, crizotinib, and paclitaxel and experienced near-complete disease response [99], and combined targeted blockade warrants further investigations. Additionally, loss of PTEN expression and low HER2 amplification index have been correlated with primary resistance to first-line trastuzumab-based therapy and poor prognosis in a study involving 129 HER2 positive GC [100].
More recently Pietrantonio et al. reported the results of a study investigating biomarkers of primary resistance to trastuzumab in HER2-positive metastatic GC (the AMNESIA study). A panel of candidate genomic alterations including EGFR, MET, KRAS, PI3K and PTEN mutations and EGFR, MET, and KRAS amplifications was tested in 37 patients treated with trastuzumab (17 responders and 20 patients with primary resistance). AMESIA panel alterations were significantly more frequent in resistant patients and in HER2 IHC 2+ compared to HER2 IHC 3+ tumors. The absence of any alteration was correlated with longer median PFS and OS and the predictive accuracy of the combined evaluation of the AMNESIA panel and HER2 IHC was 84% [101]. These promising results, however, need further prospective validation.
In another previous study, the same author explored the possible mechanisms of anti-HER2 acquired resistance in GEA. In a small series of 22 matched pre-treatment and post-progression samples from patients receiving chemotherapy and trastuzumab for advanced HER2‐positive (IHC 3+ or 2+ with ISH amplification) GEA, HER2 loss was identified a mechanism of resistance in 32% of cases. Notably, the chance of HER2 loss was not associated with any baseline clinico-pathological features except initial IHC score 2+ versus 3+ [102]. Loss of HER2 overexpression might partially explain the failure of second-line anti-HER2 treatment strategies in initially HER2-positive tumors.
Additionally, molecular alterations emerging upon tumor progression after trastuzumab treatment have been observed in several candidate genes such as TP53 (92%), EGFR (13%), cell-cycle mediators, i.e. cyclin-dependent kinases (42%) and in the PI3K/AKT/mTOR axis (21%) [103]. Similarly, a recently reported biomarker analysis from a phase II study evaluating the efficacy of lapatinib in combination with chemotherapy as first-line treatment in HER-2-positive GC showed the emergence of genomic aberrations such as MYC, EGFR, FGFR2 and MET amplifications at disease progression [104].
None of these biomarkers, however, are currently implemented in clinical practice, and additional evidence is necessary to optimize patient selection and personalize treatment strategies based on the definition of key mechanisms of resistance to targeted treatment and development of effective alternative targeted therapies for refractory disease, including combined targeted blockade of concomitant or emerging secondary driver alterations.
Molecular heterogeneity between primary tumor and metastatic disease: possible role of liquid biopsy
Intra-tumor heterogeneity has been shown to be extremely relevant in GEA. Indeed, HER2 expression has been found to range widely with variable percentages of tumor cells staining positive in the same samples, and variable concordance rates between biopsy and paired surgical resections have been reported [105, 106], as well as previously discussed changes in HER2 expression related to targeted treatment (HER2 loss). Additionally, recent results of a large-scale profiling study in GC confirmed a high grade of tumor heterogeneity in EBV-positivity and PIK3CA mutations, suggesting caution in the extrapolation of tumor genomic profiling from the analyses of single tissue biopsies [107]. Discordance in HER2 expression between primary tumor (PT) and metastatic lesions (MLs) has been reported as well [108, 109], possibly due to a clonal selection during tumor progression or to intra-tumor heterogeneity of HER2. These data underline the issue of possible limitations in molecular testing in GEA due to single specimen analyses which might not be representative of the whole tumor genetic landscape.
More recently two works highlighted a deeper level of genomic heterogeneity between PTs and MLs in GEA through the use of targeted NGS and whole-exon sequencing techniques [110, 111]. Of note, Pectasides and colleagues sequenced paired primary GEA and MLs across multiple cohorts, finding remarkable levels of discordance in genomic alterations, including potentially clinically relevant alterations, reaching up to 60% for the amplification profile of genes such as HER2, EGFR, KRAS and CDK4/6. Their study included a pilot analysis of cell-free DNA (cfDNA) which showed both concordance and discordance with matched PT and MLs results, as sequencing of cfDNA was able to identify in some cases alterations (i.e. genomic amplifications) not observed in the PTs, but at the same time failed in other cases to show the presence of known alterations involving genes such as HER2 and FGFR found in PTs. Additionally, profiling of paired PTs, MLs, and cfDNA from patients enrolled in the PANGEA (Personalized Antibodies for Gastroesophageal Adenocarcinoma) trial (NCT02213289) highlighted a recurrent discrepancy of genomic biomarkers between PTs and untreated metastases, which led to treatment reassignment in about one-third of patients. In case of discordant PT and MLs, cfDNA displayed an 87.5% concordance rate with MLs for targetable alterations, suggesting the potential role of cfDNA testing to enhance targeted treatment selection [111].
Indeed, several studies have underlined the promising role of ctDNA testing (commonly referred to as ‘liquid biopsy’) as a less invasive and more comprehensive method to pharmacogenomic profiling and dynamic molecular monitoring in several cancer types, including GEA. Notably, a study from Gao et al. demonstrated that the mutational profile of ctDNA in a series of 30 GC patients was able to reflect the sum of somatic mutations present in multiple paired tissue samples while the concordance with a single tumor sample was low, highlighting once again the issue of tumor heterogeneity in GEA and the potential of ctDNA to at least partially overcome it [112]. Additionally, in this study HER2 amplification in ctDNA were showed to be highly concordant with HER2 amplification in tumor tissue. Furthermore, Wang and colleagues recently reported positive data on the use of ctDNA to evaluate HER2 copy number levels as a minimally-invasive biomarker to predict and monitor trastuzumab efficacy in advanced GC [113]. Main evidence on liquid biopsy in GC are reviewed in dedicated papers [114–116]. Of note, recent evidence suggests a prognostic value as well as a role in monitoring treatment response and risk of recurrence, for ctDNA in early stage esophageal cancers [117].
Although validation and further investigations are critical, altogether these data support the role of liquid biopsy as a promising technique for genomic profiling, targeted treatment selection and monitoring of treatment response as well as early detection of secondary resistance mechanisms in GEA, which warrants further development for future clinical applications.
Emerging role of epigenomics and miRNA in GEA
Epigenetic changes, including DNA methylation, histone modifications and non-coding RNAs, are a common event in cancer and contribute to both carcinogenesis and disease progression. Aberrant DNA methylation is one of the most studied epigenetic alteration in cancer and it has been proposed as a potential biomarker both for tumor diagnosis, prognosis and treatment response in several cancer types.
Promoter DNA methylation of several tumor suppressor genes has been reported in pre-malignant stages of GC, suggesting a potential role for early cancer detection of these biomarkers, which have been identified either in blood, gastric juice or stool samples (reviewed in [118]). On the other hand, promoter hypermethylation of several genes has been associated with worse prognosis in GC (reviewed in [119]). Notably, both Helicobacter pylori and EBV infections are associated with increased levels of DNA methylation, and, as previously discussed, EBV-positive tumors exhibit extreme CIMP signature involving hypermethylation of numerous target genes. In EAC, abnormal DNA methylation has been extensively researched as a tool for stratifying Barrett’s esophagus patients’ risk to develop cancer. Aberrant methylation in several genes, in fact, such as CDKN2A and APC, has been reported as part of the neoplastic progression from Barret’s esophagus to EAC [120]). Similar with GC, promoter methylation of multiple genes has been associated with poor prognosis in EAC. Future research will further address the promising diagnostic and prognostic value of aberrant DNA methylation in GEA and its possible implication in treatment response as well as its potential role as a treatment target in these malignancies.
In recent years, miRNAs have emerged as critical regulators in the oncogenesis pathways and have been proposed as useful novel diagnostic and prognostic biomarkers in multiple cancer types [121, 122]. These small noncoding RNA fragments regulate target genes expression by binding to their 3′UTR region and impairing translation, hence modulating a broad range of biological processes comprising cellular signaling, metabolism, apoptosis, proliferation and differentiation, acting either as oncogenes or as tumor suppressors [123]. Their role as a biomarker represents an expanding field of research in GEA [124–127]. Several miRNAs have been identified and implicated in GC and EAC diagnosis and prognosis and many others are currently under investigation [128, 129]. A predictive role of miRNAs in treatment response has been proposed as well. Although available data still need validation, the possible clinical application of miRNAs as biomarkers or as a potential target of treatment in GEA deserves further investigation.
In addition to miRNA, long noncoding RNAs (lncRNAs), are recently becoming one of the next frontier of cancer research. Recent findings, in fact, suggest that they play an important role in carcinogenesis and metastasis and numerous lncRNAs have been found to be altered in GEA, thus supporting a strong rational for their potential role as biomarkers in these malignancies [125, 130–132].
Patient-derived xenograft models
Patient-derived xenograft (PDX) models represent a novel approach with the potential to enhance biomarker discovery and preclinical testing of personalized treatment options, providing a platform which replicates tumor molecular and biological features as well as tumor microenvironment in the animal model.
Patient-derived xenograft models have been successfully created for GC and explored in several studies. Notably, PDX models of tumors harboring alterations in HER-2, MET and FGFR2 signaling pathways have been proven useful for targeted drugs screening and evaluation, highlighting preliminary evidence of activity of the combination of targeted anti-MET and anti-FGFR2 treatment in tumors with co-occurrent amplifications of these genes [133]. More recently, tumor molecular profiling of PDX models has been used to guide treatment selection and test the efficacy of selected targeted drugs while exploring possible candidate response biomarkers [134]. The authors of this study were able to identify definite molecular signature in different PDX models with corresponding individual histopathological and molecular features. Main recurrent genomic alterations involved the MAPK, ErbB, VEGF, mTOR, and cell cycle signaling pathways. Several potential drug targets were selected and activity of targeted blockade (i.e. anti-MET volitinib, anti-EGFR monoclonal antibody BK011 and cetuximab, afatinib, apatinib and the CDK1/2/9 inhibitor AZD5438), was demonstrated in corresponding models. These preliminary results should be validated in larger studies with PDX models or in clinical trials, nevertheless current evidence supports future perspectives on a wider use of PDX models with defined molecular signatures in preclinical studies with targeted drugs.
Conclusions
As our knowledge on the genomic landscape of GEA continues to evolve, uncovering the high heterogeneity and deep complexity of these tumors, current efforts are centered upon establishing the clinical relevance of novel molecular subtypes and validate novel biomarker-driven targeted treatment approaches.
The availability of new technologies and the identification of promising novel biomarker with the potential to overcome tumor heterogeneity and provide a dynamic monitoring of tumor molecular evolution under treatment pressure will be crucial to optimize drug development and clinical investigation in a setting where therapeutic options are currently lacking.
Several promising biomarkers are under study and growing evidence is accumulating on mechanisms of primary and acquired resistance to treatment, nevertheless further validation is necessary before translating available evidence into clinical practice.
Authors’ contributions
FB and MN drafted the manuscript with the aid of AP. HJL supervised the manuscript. All authors directly provided their contribution. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
Heinz-Josef Lenz has received clinical trial financial support from Merck Serono and Roche and honoraria for advisory board membership and lectures from Bayer, Boehringer Ingelheim, Genentech, Merck Serono and Roche.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
This manuscript was partly supported in part by the National Cancer Institute (Grant Number P30CA014089), the Gloria Borges WunderGlo Foundation-The Wunder Project, the Dhont Family Foundation, the San Pedro Peninsula Cancer Guild, the Daniel Butler Research Fund, and the Call to Cure Research Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- ACRG
Asian Cancer Research Group
- AKT
AKT8 virus oncogene cellular homolog
- Ang-2
angiopoietin-2
- B2M
beta-2-microglobulin
- BMP
bone morphogenetic protein
- BRAF
v-Raf murine sarcoma viral oncogene homolog B1
- CDH1
cadherin 1
- CIN
chromosomal instability
- CIMP
CpG island methylation phenotype
- cfDNA
circulating free DNA
- ctDNA
circulating tumor DNA
- CTLA-4
cytotoxic T lymphocyte-associated protein 4
- CTNNA1
catenin alpha 1
- EAC
esophageal adenocarcinoma
- EBV
Epstein-Barr virus
- EC
esophagus carcinoma
- EGFR
epidermal growth factor receptor
- ERK
extracellular signal-regulated kinase
- FDA
Food and Drug Administration
- FGFR2
fibroblast growth factor receptor 2
- FHIT
fragile histidine triad
- FISH
fluorescent in situ hybridization
- GEA
gastro-esophageal adenocarcinomas
- GEJ
gastro-esophageal junction
- GC
gastric cancer
- GS
genomically stable
- HER2/neu
human epidermal growth factor receptor 2
- IHC
immunohistochemical staining
- KRAS
Kirsten rat sarcoma viral oncogene homolog
- lncRNA
long noncoding RNA
- MAPK
mitogen-activated protein kinase
- MEK
mitogen-activated protein kinase kinase
- MET
tyrosine-protein kinase Met
- MHLW
Japanese Ministry of Health, Labor and Welfare
- miRNA
micro RNA
- MMR
mismatch repair
- MSI
microsatellite instability
- MSS
microsatellite stable
- mTOR
mammalian target of rapamycin
- NGS
next generation sequencing
- OS
overall survival
- PARD3
Par-3 family cell polarity regulator
- PD-1
programmed cell death protein 1
- PD1H
PD1 homolog
- PD-L1
programmed death-ligand 1
- PDX
patient-derived xenograft
- PFS
progression free survival
- PIK3CA
phosphatidylinositol 3-kinase catalytic subunit alpha
- PTEN
phosphatase and tensin homolog
- RAF
v-Raf murine sarcoma viral oncogene homolog
- RAS
rat sarcoma viral oncogene homolog
- RB1
retinoblastoma 1
- RET
REarranged during transfection
- ROHA
Ras homolog family member A
- RTK
receptor tyrosine kinase
- STK3
serine/threonine kinase 3
- TCGA
The Cancer Genome Atlas
- T-DM1
trastuzumab-emtansine
- TILs
tumor infiltrating lymphocytes
- TKI
tyrosine kinase inhibitor
- VEGF
vascular endothelial growth factor
- VEGFR
VEGF receptor
- VISTA
V-domain Ig suppressor of T cell activation
- WWOX
WW domain containing oxidoreductase)
Contributor Information
Francesca Battaglin, Phone: +1-323-865-0584, Email: fbattagl@usc.edu.
Madiha Naseem, Email: naseem@usc.edu.
Alberto Puccini, Email: albertopuccini91@gmail.com.
Heinz-Josef Lenz, Email: lenz@med.usc.edu.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, Feuer EJ. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013;119(6):1149–1158. doi: 10.1002/cncr.27834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Cancer Institute Surveillance, Epidemiology, and End Results Program. https://seer.cancer.gov/. Accessed 16 Apr 2018.
- 4.Bass AJ, Thorsson V, Shmulevich I, Reynolds SM, Miller M, Bernard B, Hinoue T, Laird PW, Curtis C, Shen H, et al. Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513(7517):202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cristescu R, Lee J, Nebozhyn M, Kim KM, Ting JC, Wong SS, Liu J, Yue YG, Wang J, Yu K, et al. Molecular analysis of gastric cancer identifies subtypes associated with distinct clinical outcomes. Nat Med. 2015;21(5):449–456. doi: 10.1038/nm.3850. [DOI] [PubMed] [Google Scholar]
- 6.Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta pathologica et microbiologica Scandinavica. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 7.Petrelli F, Berenato R, Turati L, Mennitto A, Steccanella F, Caporale M, Dallera P, de Braud F, Pezzica E, Di Bartolomeo M, et al. Prognostic value of diffuse versus intestinal histotype in patients with gastric cancer: a systematic review and meta-analysis. J Gastrointest Oncol. 2017;8(1):148–163. doi: 10.21037/jgo.2017.01.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Normanno N, Bianco C, Strizzi L, Mancino M, Maiello MR, Luca AD, Caponigro F, Salomon DS. The ErbB receptors and their ligands in cancer: an overview. Curr Drug Targets. 2005;6(3):243–257. doi: 10.2174/1389450053765879. [DOI] [PubMed] [Google Scholar]
- 9.Gravalos C, Jimeno A. HER2 in gastric cancer: a new prognostic factor and a novel therapeutic target. Ann Oncol. 2008;19(9):1523–1529. doi: 10.1093/annonc/mdn169. [DOI] [PubMed] [Google Scholar]
- 10.Okines AFC, Cunningham D. Trastuzumab in gastric cancer. Eur J Cancer. 2010;46(11):1949–1959. doi: 10.1016/j.ejca.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Okines AFC, Thompson LC, Cunningham D, Wotherspoon A, Reis-Filho JS, Langley RE, Waddell TS, Noor D, Eltahir Z, Wong R, et al. Effect of HER2 on prognosis and benefit from peri-operative chemotherapy in early oesophago-gastric adenocarcinoma in the MAGIC trial. Ann Oncol. 2013;24(5):1253–1261. doi: 10.1093/annonc/mds622. [DOI] [PubMed] [Google Scholar]
- 12.Barros-Silva JD, Leitao D, Afonso L, Vieira J, Dinis-Ribeiro M, Fragoso M, Bento MJ, Santos L, Ferreira P, Rego S, et al. Association of ERBB2 gene status with histopathological parameters and disease-specific survival in gastric carcinoma patients. Br J Cancer. 2009;100(3):487–493. doi: 10.1038/sj.bjc.6604885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Press MF, Ellis CE, Gagnon RC, Grob TJ, Buyse M, Villalobos I, Liang Z, Wu S, Bang Y-J, Qin S-K, et al. HER2 status in advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma for entry to the TRIO-013/LOGiC trial of lapatinib. Mol Cancer Ther. 2017;16(1):228–238. doi: 10.1158/1535-7163.MCT-15-0887. [DOI] [PubMed] [Google Scholar]
- 14.Boers JE, Meeuwissen H, Methorst N. HER2 status in gastro-oesophageal adenocarcinomas assessed by two rabbit monoclonal antibodies (SP3 and 4B5) and two in situ hybridization methods (FISH and SISH) Histopathology. 2011;58(3):383–394. doi: 10.1111/j.1365-2559.2011.03760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunz PL, Mojtahed A, Fisher GA, Ford JM, Chang DT, Balise RR, Bangs CD, Cherry AM, Pai RK. HER2 expression in gastric and gastroesophageal junction adenocarcinoma in a US population: clinicopathologic analysis with proposed approach to HER2 assessment. Appl Immunohistochem Mol Morphol. 2012;20(1):13–24. doi: 10.1097/PAI.0b013e31821c821c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Cutsem E, Bang YJ, Feng-Yi F, Xu JM, Lee KW, Jiao SC, Chong JL, Lopez-Sanchez RI, Price T, Gladkov O, et al. HER2 screening data from ToGA: targeting HER2 in gastric and gastroesophageal junction cancer. Gastric Cancer. 2015;18(3):476–484. doi: 10.1007/s10120-014-0402-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim WH, Gomez-Izquierdo L, Vilardell F, Chu KM, Soucy G, Dos Santos LV, Monges G, Viale G, Brito MJ, Osborne S, et al. HER2 status in gastric and gastroesophageal junction cancer: results of the large, multinational HER-EAGLE study. Appl Immunohistochem Mol Morphol AIMM. 2018;26(4):239–245. doi: 10.1097/PAI.0000000000000423. [DOI] [PubMed] [Google Scholar]
- 18.Fisher SB, Fisher KE, Squires MH, Patel SH, Kooby DA, El-Rayes BF, Cardona K, Russell MC, Staley CA, Farris AB, et al. HER2 in resected gastric cancer: is there prognostic value? J Surg Oncol. 2014;109(2):61–66. doi: 10.1002/jso.23456. [DOI] [PubMed] [Google Scholar]
- 19.Begnami MD, Fukuda E, Fregnani JH, Nonogaki S, Montagnini AL, da Costa WL, Jr, Soares FA. Prognostic implications of altered human epidermal growth factor receptors (HERs) in gastric carcinomas: HER2 and HER3 are predictors of poor outcome. J Clin Oncol. 2011;29(22):3030–3036. doi: 10.1200/JCO.2010.33.6313. [DOI] [PubMed] [Google Scholar]
- 20.Janjigian YY, Werner D, Pauligk C, Steinmetz K, Kelsen DP, Jäger E, Altmannsberger HM, Robinson E, Tafe LJ, Tang LH, et al. Prognosis of metastatic gastric and gastroesophageal junction cancer by HER2 status: a European and USA international collaborative analysis. Ann Oncol. 2012;23(10):2656–2662. doi: 10.1093/annonc/mds104. [DOI] [PubMed] [Google Scholar]
- 21.Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, Lordick F, Ohtsu A, Omuro Y, Satoh T, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet (London, England) 2010;376(9742):687–697. doi: 10.1016/S0140-6736(10)61121-X. [DOI] [PubMed] [Google Scholar]
- 22.National Comprehensive Cancer Network. Clinical practice guidelines in oncology. Gastric Cancer. https://www.nccn.org/professionals/physician_gls/PDF/gastric.pdf. Accessed 16 April 2018.
- 23.Bartley AN, Washington MK, Ventura CB, Ismaila N, Colasacco C, Benson AB, 3rd, Carrato A, Gulley ML, Jain D, Kakar S, et al. HER2 testing and clinical decision making in gastroesophageal adenocarcinoma: guideline from the College of American Pathologists, American Society for Clinical Pathology, and American Society of Clinical Oncology. Arch Pathol Lab Med. 2016;140(12):1345–1363. doi: 10.5858/arpa.2016-0331-CP. [DOI] [PubMed] [Google Scholar]
- 24.Fuchs CS, Tomasek J, Yong CJ, Dumitru F, Passalacqua R, Goswami C, Safran H, Dos Santos LV, Aprile G, Ferry DR, et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet (London, England) 2014;383(9911):31–39. doi: 10.1016/S0140-6736(13)61719-5. [DOI] [PubMed] [Google Scholar]
- 25.Wilke H, Muro K, Van Cutsem E, Oh SC, Bodoky G, Shimada Y, Hironaka S, Sugimoto N, Lipatov O, Kim TY, et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 2014;15(11):1224–1235. doi: 10.1016/S1470-2045(14)70420-6. [DOI] [PubMed] [Google Scholar]
- 26.Fuchs CS, Tabernero J, Tomášek J, Chau I, Melichar B, Safran H, Tehfe MA, Filip D, Topuzov E, Schlittler L, et al. Biomarker analyses in REGARD gastric/GEJ carcinoma patients treated with VEGFR2-targeted antibody ramucirumab. Br J Cancer. 2016;115(8):974–982. doi: 10.1038/bjc.2016.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Cutsem E, de Haas S, Kang YK, Ohtsu A, Tebbutt NC, Ming XuJ, Peng Yong W, Langer B, Delmar P, Scherer SJ, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a biomarker evaluation from the AVAGAST randomized phase III trial. J Clin Oncol. 2012;30(17):2119–2127. doi: 10.1200/JCO.2011.39.9824. [DOI] [PubMed] [Google Scholar]
- 28.Hacker UT, Escalona-Espinosa L, Consalvo N, Goede V, Schiffmann L, Scherer SJ, Hedge P, Van Cutsem E, Coutelle O, Buning H. Evaluation of Angiopoietin-2 as a biomarker in gastric cancer: results from the randomised phase III AVAGAST trial. Br J Cancer. 2016;114(8):855–862. doi: 10.1038/bjc.2016.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohtsu A, Shah MA, Van Cutsem E, Rha SY, Sawaki A, Park SR, Lim HY, Yamada Y, Wu J, Langer B, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J Clin Oncol. 2011;29(30):3968–3976. doi: 10.1200/JCO.2011.36.2236. [DOI] [PubMed] [Google Scholar]
- 30.Wang KL, Wu TT, Choi IS, Wang H, Resetkova E, Correa AM, Hofstetter WL, Swisher SG, Ajani JA, Rashid A, et al. Expression of epidermal growth factor receptor in esophageal and esophagogastric junction adenocarcinomas: association with poor outcome. Cancer. 2007;109(4):658–667. doi: 10.1002/cncr.22445. [DOI] [PubMed] [Google Scholar]
- 31.Lieto E, Ferraraccio F, Orditura M, Castellano P, Mura AL, Pinto M, Zamboli A, De Vita F, Galizia G. Expression of vascular endothelial growth factor (VEGF) and epidermal growth factor receptor (EGFR) is an independent prognostic indicator of worse outcome in gastric cancer patients. Ann Surg Oncol. 2008;15(1):69–79. doi: 10.1245/s10434-007-9596-0. [DOI] [PubMed] [Google Scholar]
- 32.Lordick F, Kang YK, Chung HC, Salman P, Oh SC, Bodoky G, Kurteva G, Volovat C, Moiseyenko VM, Gorbunova V, et al. Capecitabine and cisplatin with or without cetuximab for patients with previously untreated advanced gastric cancer (EXPAND): a randomised, open-label phase 3 trial. Lancet Oncol. 2013;14(6):490–499. doi: 10.1016/S1470-2045(13)70102-5. [DOI] [PubMed] [Google Scholar]
- 33.Waddell T, Chau I, Cunningham D, Gonzalez D, Okines AF, Okines C, Wotherspoon A, Saffery C, Middleton G, Wadsley J, et al. Epirubicin, oxaliplatin, and capecitabine with or without panitumumab for patients with previously untreated advanced oesophagogastric cancer (REAL3): a randomised, open-label phase 3 trial. Lancet Oncol. 2013;14(6):481–489. doi: 10.1016/S1470-2045(13)70096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim MA, Lee HS, Lee HE, Jeon YK, Yang HK, Kim WH. EGFR in gastric carcinomas: prognostic significance of protein overexpression and high gene copy number. Histopathology. 2008;52(6):738–746. doi: 10.1111/j.1365-2559.2008.03021.x. [DOI] [PubMed] [Google Scholar]
- 35.Gherardi E, Birchmeier W, Birchmeier C, Vande Woude G. Targeting MET in cancer: rationale and progress. Nat Rev Cancer. 2012;12(2):89–103. doi: 10.1038/nrc3205. [DOI] [PubMed] [Google Scholar]
- 36.Lennerz JK, Kwak EL, Ackerman A, Michael M, Fox SB, Bergethon K, Lauwers GY, Christensen JG, Wilner KD, Haber DA, et al. MET amplification identifies a small and aggressive subgroup of esophagogastric adenocarcinoma with evidence of responsiveness to crizotinib. J Clin Oncol. 2011;29(36):4803–4810. doi: 10.1200/JCO.2011.35.4928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Panarese I, De Vita F, Ronchi A, Romano M, Alfano R, Di Martino N, Zito Marino F, Ferraraccio F, Franco R. Predictive biomarkers along gastric cancer pathogenetic pathways. Expert Rev Anticancer Ther. 2017;17(5):417–425. doi: 10.1080/14737140.2017.1301207. [DOI] [PubMed] [Google Scholar]
- 38.Cunningham D, Tebbutt NC, Davidenko I, Murad AM, Al-Batran S-E, Ilson DH, Tjulandin S, Gotovkin E, Karaszewska B, Bondarenko I, et al. Phase III, randomized, double-blind, multicenter, placebo (P)-controlled trial of rilotumumab (R) plus epirubicin, cisplatin and capecitabine (ECX) as first-line therapy in patients (pts) with advanced MET-positive (pos) gastric or gastroesophageal junction (G/GEJ) cancer: RILOMET-1 study. J Clin Oncol. 2015;33(15_suppl):4000. [Google Scholar]
- 39.Shah MA, Bang YJ, Lordick F, Tabernero J, Chen M, Hack SP, Phan SC, Shames DS, Cunningham D. METGastric: a phase III study of onartuzumab plus mFOLFOX6 in patients with metastatic HER2-negative (HER2-) and MET-positive (MET+) adenocarcinoma of the stomach or gastroesophageal junction (GEC) J Clin Oncol. 2015;33(15_suppl):4012. [Google Scholar]
- 40.Wang K, Yuen ST, Xu J, Lee SP, Yan HH, Shi ST, Siu HC, Deng S, Chu KM, Law S, et al. Whole-genome sequencing and comprehensive molecular profiling identify new driver mutations in gastric cancer. Nat Genet. 2014;46(6):573–582. doi: 10.1038/ng.2983. [DOI] [PubMed] [Google Scholar]
- 41.Zang ZJ, Cutcutache I, Poon SL, Zhang SL, McPherson JR, Tao J, Rajasegaran V, Heng HL, Deng N, Gan A, et al. Exome sequencing of gastric adenocarcinoma identifies recurrent somatic mutations in cell adhesion and chromatin remodeling genes. Nat Genet. 2012;44(5):570–574. doi: 10.1038/ng.2246. [DOI] [PubMed] [Google Scholar]
- 42.Dulak AM, Stojanov P, Peng S, Lawrence MS, Fox C, Stewart C, Bandla S, Imamura Y, Schumacher SE, Shefler E, et al. Exome and whole-genome sequencing of esophageal adenocarcinoma identifies recurrent driver events and mutational complexity. Nat Genet. 2013;45(5):478–486. doi: 10.1038/ng.2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang K, Johnson A, Ali SM, Klempner SJ, Bekaii-Saab T, Vacirca JL, Khaira D, Yelensky R, Chmielecki J, Elvin JA, et al. Comprehensive genomic profiling of advanced esophageal squamous cell carcinomas and esophageal adenocarcinomas reveals similarities and differences. Oncologist. 2015;20(10):1132–1139. doi: 10.1634/theoncologist.2015-0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Secrier M, Li X, de Silva N, Eldridge MD, Contino G, Bornschein J, MacRae S, Grehan N, O’Donovan M, Miremadi A, et al. Mutational signatures in esophageal adenocarcinoma define etiologically distinct subgroups with therapeutic relevance. Nat Genet. 2016;48(10):1131–1141. doi: 10.1038/ng.3659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sohn BH, Hwang JE, Jang HJ, Lee HS, Oh SC, Shim JJ, Lee KW, Kim EH, Yim SY, Lee SH, et al. Clinical significance of four molecular subtypes of gastric cancer identified by the cancer genome atlas project. Clin Cancer Res. 2017;23(15):4441–4449. doi: 10.1158/1078-0432.CCR-16-2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Naseem M, Barzi A, Brezden-Masley C, Puccini A, Berger MD, Tokunaga R, Battaglin F, Soni S, McSkane M, Zhang W, et al. Outlooks on Epstein-Barr virus associated gastric cancer. Cancer Treat Rev. 2018;66:15–22. doi: 10.1016/j.ctrv.2018.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Genitsch V, Novotny A, Seiler CA, Kroll D, Walch A, Langer R. Epstein-barr virus in gastro-esophageal adenocarcinomas—single center experiences in the context of current literature. Front Oncol. 2015;5:73. doi: 10.3389/fonc.2015.00073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Camargo MC, Murphy G, Koriyama C, Pfeiffer RM, Kim WH, Herrera-Goepfert R, Corvalan AH, Carrascal E, Abdirad A, Anwar M, et al. Determinants of Epstein-Barr virus-positive gastric cancer: an international pooled analysis. Br J Cancer. 2011;105(1):38–43. doi: 10.1038/bjc.2011.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chang MS, Uozaki H, Chong JM, Ushiku T, Sakuma K, Ishikawa S, Hino R, Barua RR, Iwasaki Y, Arai K, et al. CpG island methylation status in gastric carcinoma with and without infection of Epstein-Barr virus. Clin Cancer Res. 2006;12(10):2995–3002. doi: 10.1158/1078-0432.CCR-05-1601. [DOI] [PubMed] [Google Scholar]
- 50.Shinozaki-Ushiku A, Kunita A, Fukayama M. Update on Epstein-Barr virus and gastric cancer. Int J Oncol. 2015;46(4):1421–1434. doi: 10.3892/ijo.2015.2856. [DOI] [PubMed] [Google Scholar]
- 51.Garcia-Diaz A, Shin DS, Moreno BH, Saco J, Escuin-Ordinas H, Rodriguez GA, Zaretsky JM, Sun L, Hugo W, Wang XY, et al. Interferon receptor signaling pathways regulating PD-L1 and PD-L2 expression. Cell Rep. 2017;19(6):1189–1201. doi: 10.1016/j.celrep.2017.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gulley ML. Genomic assays for Epstein-Barr virus-positive gastric adenocarcinoma. Exp Mol Med. 2015;47:e134. doi: 10.1038/emm.2014.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pandya D, Mariani M, He SQ, Andreoli M, Spennato M, Dowell-Martino C, Fiedler P, Ferlini C. Epstein-Barr virus MicroRNA expression increases aggressiveness of solid malignancies. PLoS ONE. 2015;10(9):e0136058. doi: 10.1371/journal.pone.0136058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Velho S, Fernandes MS, Leite M, Figueiredo C, Seruca R. Causes and consequences of microsatellite instability in gastric carcinogenesis. World J Gastroenterol. 2014;20(44):16433–16442. doi: 10.3748/wjg.v20.i44.16433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zou L, Wu YY, Ma K, Fan YW, Dong DF, Geng NY, Li EX. Molecular classification of esophagogastric junction carcinoma correlated with prognosis. Oncotargets Ther. 2017;10:4765–4772. doi: 10.2147/OTT.S145912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mathiak M, Warneke VS, Behrens HM, Haag J, Boger C, Kruger S, Rocken C. Clinicopathologic characteristics of microsatellite instable gastric carcinomas revisited: urgent need for standardization. Appl Immunohistochem Mol Morphol. 2017;25(1):12–24. doi: 10.1097/PAI.0000000000000264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vranic S. Microsatellite instability status predicts response to anti-PD-1/PD-L1 therapy regardless the histotype: a comment on recent advances. Bosnian J Basic Med. 2017;17(3):274–275. doi: 10.17305/bjbms.2017.2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fuchs CS, Doi T, Jang RWJ, Muro K, Satoh T, Machado M, Sun W, Jalal SI, Shah MA, Metges JP, et al. KEYNOTE-059 cohort 1: efficacy and safety of pembrolizumab (pembro) monotherapy in patients with previously treated advanced gastric cancer. J Clin Oncol. 2017 doi: 10.1200/JCO.2017.35.15_suppl.4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Choi YY, Kim H, Yang HK, Kim WH, Kim YW, Kook MC, Park YK, Kim HH, Lee HS, Lee KH, et al. Clinical impact of microsatellite instability in patients with stage II and III gastric cancer: results from the CLASSIC trial. J Clin Oncol. 2017 doi: 10.1200/JCO.2017.35.15_suppl.4022. [DOI] [Google Scholar]
- 60.Corso G, Velho S, Paredes J, Pedrazzani C, Martins D, Milanezi F, Pascale V, Vindigni C, Pinheiro H, Leite M, et al. Oncogenic mutations in gastric cancer with microsatellite instability. Eur J Cancer. 2011;47(3):443–451. doi: 10.1016/j.ejca.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 61.Park J, Yoo HM, Jang W, Shin S, Kim M, Kim Y, Lee SW, Kim JG. Distribution of somatic mutations of cancer-related genes according to microsatellite instability status in Korean gastric cancer. Medicine. 2017;96(25):e7224. doi: 10.1097/MD.0000000000007224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gornalusse GG, Hirata RK, Funk SE, Riolobos L, Lopes VS, Manske G, Prunkard D, Colunga AG, Hanafi LA, Clegg DO, et al. HLA-E-expressing pluripotent stem cells escape allogeneic responses and lysis by NK cells. Nat Biotechnol. 2017;35(8):765–772. doi: 10.1038/nbt.3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liu JF, McCleland M, Stawiski EW, Gnad F, Mayba O, Haverty PM, Durinck S, Chen YJ, Klijn C, Jhunjhunwala S, et al. Integrated exome and transcriptome sequencing reveals ZAK isoform usage in gastric cancer. Nat Commun. 2014;5:3830. doi: 10.1038/ncomms4830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lim B, Kim JH, Kim M, Kim SY. Genomic and epigenomic heterogeneity in molecular subtypes of gastric cancer. World J Gastroenterol. 2016;22(3):1190–1201. doi: 10.3748/wjg.v22.i3.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Katona BW, Rustgi AK. Gastric cancer genomics: advances and future directions. Cell Mol Gastroenter. 2017;3(2):211–217. doi: 10.1016/j.jcmgh.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhou X, Zheng Y. Cell type-specific signaling function of RhoA GTPase: lessons from mouse gene targeting. J Biol Chem. 2013;288(51):36179–36188. doi: 10.1074/jbc.R113.515486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rocken C, Behrens HM, Boger C, Kruger S. Clinicopathological characteristics of RHOA mutations in a Central European gastric cancer cohort. J Clin Pathol. 2016;69(1):70–75. doi: 10.1136/jclinpath-2015-202980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kim J, Bowlby R, Mungall AJ, Robertson AG, Odze RD, Cherniack AD, Shih J, Pedamallu CS, Cibulskis C, Dunford A, et al. Integrated genomic characterization of oesophageal carcinoma. Nature. 2017;541(7636):169–175. doi: 10.1038/nature20805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Porta R, Borea R, Coelho A, Khan S, Araujo A, Reclusa P, Franchina T, Van Der Steen N, Van Dam P, Ferri J, et al. FGFR a promising druggable target in cancer: molecular biology and new drugs. Crit Rev Oncol Hemat. 2017;113:256–267. doi: 10.1016/j.critrevonc.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 70.Ahn S, Lee J, Hong M, Kim ST, Park SH, Choi MG, Lee JH, Sohn TS, Bae JM, Kim S, et al. FGFR2 in gastric cancer: protein overexpression predicts gene amplification and high H-index predicts poor survival. Modern Pathol. 2016;29(9):1095–1103. doi: 10.1038/modpathol.2016.96. [DOI] [PubMed] [Google Scholar]
- 71.Tokunaga R, Imamura Y, Nakamura K, Ishimoto T, Nakagawa S, Miyake K, Nakaji Y, Tsuda Y, Iwatsuki M, Baba Y, et al. Fibroblast growth factor receptor 2 expression, but not its genetic amplification, is associated with tumor growth and worse survival in esophagogastric junction adenocarcinoma. Oncotarget. 2016;7(15):19748–19761. doi: 10.18632/oncotarget.7782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chae YK, Ranganath K, Hammerman PS, Vaklavas C, Mohindra N, Kalyan A, Matsangou M, Costa R, Carneiro B, Villaflor VM, et al. Inhibition of the fibroblast growth factor receptor (FGFR) pathway: the current landscape and barriers to clinical application. Oncotarget. 2017;8(9):16052–16074. doi: 10.18632/oncotarget.14109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Van Cutsem E, Bang YJ, Mansoor W, Petty RD, Chao Y, Cunningham D, Ferry DR, Smith NR, Frewer P, Ratnayake J, et al. A randomized, open-label study of the efficacy and safety of AZD4547 monotherapy versus paclitaxel for the treatment of advanced gastric adenocarcinoma with FGFR2 polysomy or gene amplification. Ann Oncol. 2017;28(6):1316–1324. doi: 10.1093/annonc/mdx107. [DOI] [PubMed] [Google Scholar]
- 74.Yu Y. A new molecular classification of gastric cancer proposed by Asian Cancer Research Group (ACRG) Transl Gastrointest Cancer. 2016;5(1):55–57. [Google Scholar]
- 75.Cancer Genome Atlas Research N Comprehensive molecular characterization of gastric adenocarcinoma. Nature. 2014;513(7517):202–209. doi: 10.1038/nature13480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ooi CH, Ivanova T, Wu J, Lee M, Tan IB, Tao J, Ward L, Koo JH, Gopalakrishnan V, Zhu Y, et al. Oncogenic pathway combinations predict clinical prognosis in gastric cancer. PLoS Genet. 2009;5(10):e1000676. doi: 10.1371/journal.pgen.1000676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chia NY, Tan P. Molecular classification of gastric cancer. Ann Oncol. 2016;27(5):763–769. doi: 10.1093/annonc/mdw040. [DOI] [PubMed] [Google Scholar]
- 78.Fuchs CS, Doi T, Jang RWJ, Muro K, Satoh T, Machado M, Sun W, Jalal SI, Shah MA, Metges JP, et al. KEYNOTE-059 cohort 1: efficacy and safety of pembrolizumab (pembro) monotherapy in patients with previously treated advanced gastric cancer. J Clin Oncol. 2017 doi: 10.1200/JCO.2017.35.15_suppl.4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wainberg ZA, Jalal S, Muro K, Yoon HH, Garrido M, Golan T, Doi T, Catenacci DV, Geva R, Ku G, et al. LBA28_PRKEYNOTE-059 Update: efficacy and safety of pembrolizumab alone or in combination with chemotherapy in patients with advanced gastric or gastroesophageal (G/GEJ) cancer. Ann Oncol. 2017 doi: 10.1093/annonc/mdx440.020. [DOI] [Google Scholar]
- 80.Kang YK, Boku N, Satoh T, Ryu MH, Chao Y, Kato K, Chung HC, Chen JS, Muro K, Kang WK, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017 doi: 10.1016/S0140-6736(17)31827-5. [DOI] [PubMed] [Google Scholar]
- 81.Doi T, Piha-Paul SA, Jalal SI, Saraf S, Lunceford J, Koshiji M, Bennouna J. Safety and antitumor activity of the anti-programmed death-1 antibody pembrolizumab in patients with advanced esophageal carcinoma. J Clin Oncol. 2018;36(1):61–67. doi: 10.1200/JCO.2017.74.9846. [DOI] [PubMed] [Google Scholar]
- 82.Ralph C, Elkord E, Burt DJ, O’Dwyer JF, Austin EB, Stern PL, Hawkins RE, Thistlethwaite FC. Modulation of lymphocyte regulation for cancer therapy: a phase II trial of tremelimumab in advanced gastric and esophageal adenocarcinoma. Clin Cancer Res. 2010;16(5):1662–1672. doi: 10.1158/1078-0432.CCR-09-2870. [DOI] [PubMed] [Google Scholar]
- 83.Moehler MH, Cho JY, Kim YH, et al. A randomized, openlabel, two-arm phase II trial comparing the efficacy of sequential ipilimumab (ipi) versus best supportive care (BSC) following first-line (1L) chemotherapy in patients with unresectable, locally advanced/metastatic (A/M) gastric or gastro-esophageal junction (G/GEJ) cancer. J Clin Oncol. 2016 doi: 10.1200/JCO.2016.34.15_suppl.4011. [DOI] [Google Scholar]
- 84.Ohtsu A, Tabernero J, Bang YJ, Fuchs CS, Sun L, Wang Z, Csiki I, Koshiji M, Cutsem EV. Pembrolizumab (MK-3475) versus paclitaxel as second-line therapy for advanced gastric or gastroesophageal junction (GEJ) adenocarcinoma: Phase 3 KEYNOTE-061 study. J Clin Oncol. 2016 doi: 10.1200/jco.2016.34.4_suppl.tps183. [DOI] [Google Scholar]
- 85.Chung HC, Arkenau HT, Wyrwicz L, Oh DY, Lee KW, Infante JR, Lee SS, Lee J, Keilholz U, Mita AC, et al. Avelumab (MSB0010718C; anti-PD-L1) in patients with advanced gastric or gastroesophageal junction cancer from JAVELIN solid tumor phase Ib trial: analysis of safety and clinical activity. J Clin Oncol. 2016 doi: 10.1200/JCO.2016.34.15_suppl.4009. [DOI] [Google Scholar]
- 86.https://www.pfizer.com/news/press-release/press-release-detail/merck_kgaa_darmstadt_germany_and_pfizer_provide_update_on_phase_iii_javelin_gastric_300_study_in_patients_with_pre_treated_advanced_gastric_cancer. Accessed 16 Apr 2018.
- 87.Champiat S, Ferte C, Lebel-Binay S, Eggermont A, Soria JC. Exomics and immunogenics: bridging mutational load and immune checkpoints efficacy. Oncoimmunology. 2014;3(1):e27817. doi: 10.4161/onci.27817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Boger C, Behrens HM, Kruger S, Rocken C. The novel negative checkpoint regulator VISTA is expressed in gastric carcinoma and associated with PD-L1/PD-1: a future perspective for a combined gastric cancer therapy? Oncoimmunology. 2017;6(4):e1293215. doi: 10.1080/2162402X.2017.1293215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Murphy AG, Kelly RJ. The evolving role of checkpoint inhibitors in the management of gastroesophageal cancer. Hematol Oncol Clin North Am. 2017;31(3):485–498. doi: 10.1016/j.hoc.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 90.Tran PN, Sarkissian S, Chao J, Klempner SJ. PD-1 and PD-L1 as emerging therapeutic targets in gastric cancer: current evidence. Gastrointest Cancer. 2017;7:1–11. doi: 10.2147/GICTT.S113525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bonotto M, Garattini SK, Basile D, Ongaro E, Fanotto V, Cattaneo M, Cortiula F, Iacono D, Cardellino GG, Pella N, et al. Immunotherapy for gastric cancers: emerging role and future perspectives. Expert Rev Clin Pharmacol. 2017;10(6):609–619. doi: 10.1080/17512433.2017.1313113. [DOI] [PubMed] [Google Scholar]
- 92.Lordick F, Shitara K, Janjigian YY. New agents on the horizon in gastric cancer. Ann Oncol. 2017;28(8):1767–1775. doi: 10.1093/annonc/mdx051. [DOI] [PubMed] [Google Scholar]
- 93.Joshi SS, Maron SB, Catenacci DV. Pembrolizumab for treatment of advanced gastric and gastroesophageal junction adenocarcinoma. Future Oncol. 2017 doi: 10.2217/fon-2017-0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Satoh T, Xu RH, Chung HC, Sun GP, Doi T, Xu JM, Tsuji A, Omuro Y, Li J, Wang JW, et al. Lapatinib plus paclitaxel versus paclitaxel alone in the second-line treatment of HER2-amplified advanced gastric cancer in Asian populations: TyTAN—a randomized, phase III study. J Clin Oncol. 2014;32(19):2039–2049. doi: 10.1200/JCO.2013.53.6136. [DOI] [PubMed] [Google Scholar]
- 95.Hecht JR, Bang YJ, Qin SK, Chung HC, Xu JM, Park JO, Jeziorski K, Shparyk Y, Hoff PM, Sobrero A, et al. Lapatinib in combination with capecitabine plus oxaliplatin in human epidermal growth factor receptor 2-positive advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma: TRIO-013/LOGiC—a randomized phase III trial. J Clin Oncol. 2016;34(5):443–451. doi: 10.1200/JCO.2015.62.6598. [DOI] [PubMed] [Google Scholar]
- 96.Thuss-Patience PC, Shah MA, Ohtsu A, Van Cutsem E, Ajani JA, Castro H, Mansoor W, Chung HC, Bodoky G, Shitara K, et al. Trastuzumab emtansine versus taxane use for previously treated HER2-positive locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma (GATSBY): an international randomised, open-label, adaptive, phase 2/3 study. Lancet Oncol. 2017;18(5):640–653. doi: 10.1016/S1470-2045(17)30111-0. [DOI] [PubMed] [Google Scholar]
- 97.Tabernero J, Hoff PM, Shen L, Ohtsu A, Shah MA, Cheng K, Song C, Wu H, Eng-Wong J, Kang YK. 616OPertuzumab (P)+ trastuzumab (H)+ chemotherapy (CT) for HER2-positive metastatic gastric or gastro-oesophageal junction cancer (mGC/GEJC): final analysis of a Phase III study (JACOB) Ann Oncol. 2017 doi: 10.1093/annonc/mdx369. [DOI] [PubMed] [Google Scholar]
- 98.Kim J, Fox C, Peng S, Pusung M, Pectasides E, Matthee E, Hong YS, Do IG, Jang J, Thorner AR, et al. Preexisting oncogenic events impact trastuzumab sensitivity in ERBB2-amplified gastroesophageal adenocarcinoma. J Clin Investig. 2014;124(12):5145–5158. doi: 10.1172/JCI75200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kwak EL, Ahronian LG, Siravegna G, Mussolin B, Borger DR, Godfrey JT, Jessop NA, Clark JW, Blaszkowsky LS, Ryan DP, et al. Molecular heterogeneity and receptor coamplification drive resistance to targeted therapy in MET-amplified esophagogastric cancer. Cancer Discov. 2015;5(12):1271–1281. doi: 10.1158/2159-8290.CD-15-0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kim C, Lee C-K, Chon HJ, Kim JH, Park HS, Heo SJ, Kim HJ, Kim TS, Kwon WS, Chung HC, et al. PTEN loss and level of HER2 amplification is associated with trastuzumab resistance and prognosis in HER2-positive gastric cancer. Oncotarget. 2017;8(69):113494–113501. doi: 10.18632/oncotarget.23054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pietrantonio F, Fucà G, Morano F, Gloghini A, Corso S, Aprile G, Perrone F, De Vita F, Tamborini E, Tomasello G, et al. Biomarkers of primary resistance to trastuzumab in HER2-positive metastatic gastric cancer patients: the amnesia case-control study. Clin Cancer Res. 2018;24(5):1082–1089. doi: 10.1158/1078-0432.CCR-17-2781. [DOI] [PubMed] [Google Scholar]
- 102.Pietrantonio F, Caporale M, Morano F, Scartozzi M, Gloghini A, Vita FD, Giommoni E, Fornaro L, Aprile G, Melisi D, et al. HER2 loss in HER2-positive gastric or gastroesophageal cancer after trastuzumab therapy: implication for further clinical research. Int J Cancer. 2016;139(12):2859–2864. doi: 10.1002/ijc.30408. [DOI] [PubMed] [Google Scholar]
- 103.Janjigian YY, Sanchez-Vega F, Tuvy Y, et al. Emergence of RTK/RAS/PI3K pathway alterations in trastuzumab-refractory HER2-positive esophagogastric (EG) tumors. ASCO Meet Abstr. 2016;34:11608. [Google Scholar]
- 104.Kim ST, Banks KC, Pectasides E, Kim SY, Kim K, Lanman RB, Talasaz A, An J, Choi MG, Lee JH, et al. Impact of genomic alterations on lapatinib treatment outcome and cell-free genomic landscape during HER2 therapy in HER2+ gastric cancer patients. Ann Oncol. 2018 doi: 10.1093/annonc/mdy034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Grillo F, Fassan M, Sarocchi F, Fiocca R, Mastracci L. HER2 heterogeneity in gastric/gastroesophageal cancers: from benchside to practice. World J Gastroenterol. 2016;22(26):5879–5887. doi: 10.3748/wjg.v22.i26.5879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Fazlollahi L, Remotti HE, Iuga A, Yang H-M, Lagana SM, Sepulveda AR. HER2 heterogeneity in gastroesophageal cancer detected by testing biopsy and resection specimens. Arch Pathol Lab Med. 2018;142(4):516–522. doi: 10.5858/arpa.2017-0039-OA. [DOI] [PubMed] [Google Scholar]
- 107.Boger C, Kruger S, Behrens HM, Bock S, Haag J, Kalthoff H, Rocken C. Epstein-Barr virus-associated gastric cancer reveals intratumoral heterogeneity of PIK3CA mutations. Ann Oncol. 2017;28(5):1005–1014. doi: 10.1093/annonc/mdx047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Gumusay O, Benekli M, Ekinci O, Baykara M, Ozet A, Coskun U, Demirci U, Uner A, Dursun A, Atak EY, et al. Discordances in HER2 status between primary gastric cancer and corresponding metastatic sites. Jpn J Clin Oncol. 2015;45(5):416–421. doi: 10.1093/jjco/hyv020. [DOI] [PubMed] [Google Scholar]
- 109.Qiu Z, Sun W, Zhou C, Zhang J. HER2 expression variability between primary gastric cancers and corresponding lymph node metastases. Hepatogastroenterology. 2015;62(137):231–233. [PubMed] [Google Scholar]
- 110.Janjigian YY, Sanchez-Vega F, Jonsson P, Chatila WK, Hechtman JF, Ku GY, Riches JC, Tuvy Y, Kundra R, Bouvier N, et al. Genetic predictors of response to systemic therapy in esophagogastric cancer. Cancer Discov. 2018;8(1):49–58. doi: 10.1158/2159-8290.CD-17-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Pectasides E, Stachler MD, Derks S, Liu Y, Maron S, Islam M, Alpert L, Kwak H, Kindler H, Polite B, et al. Genomic heterogeneity as a barrier to precision medicine in gastroesophageal adenocarcinoma. Cancer Discov. 2018;8(1):37–48. doi: 10.1158/2159-8290.CD-17-0395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gao J, Wang H, Zang W, Li B, Rao G, Li L, Yu Y, Li Z, Dong B, Lu Z, et al. Circulating tumor DNA functions as an alternative for tissue to overcome tumor heterogeneity in advanced gastric cancer. Cancer Sci. 2017;108(9):1881–1887. doi: 10.1111/cas.13314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang H, Li B, Liu Z, Gong J, Shao L, Ren J, Niu Y, Bo S, Li Z, Lai Y, et al. HER2 copy number of circulating tumour DNA functions as a biomarker to predict and monitor trastuzumab efficacy in advanced gastric cancer. Eur J Cancer. 2018;88:92–100. doi: 10.1016/j.ejca.2017.10.032. [DOI] [PubMed] [Google Scholar]
- 114.Uchôa Guimarães CT, Ferreira Martins NN, da Silva Cristina, Oliveira K, Almeida CM, Pinheiro TM, Gigek CO, de Araújo Roberto, Cavallero S, Assumpção PP, Cardoso Smith MA, Burbano RR, et al. Liquid biopsy provides new insights into gastric cancer. Oncotarget. 2018;9(19):15144–15156. doi: 10.18632/oncotarget.24540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Creemers A, Krausz S, Strijker M, van der Wel MJ, Soer EC, Reinten RJ, Besselink MG, Wilmink JW, van de Vijver MJ, van Noesel CJM, et al. Clinical value of ctDNA in upper-GI cancers: a systematic review and meta-analysis. Biochimica et Biophysica Acta. 2017;1868(2):394–403. doi: 10.1016/j.bbcan.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 116.Lopez A, Harada K, Mizrak Kaya D, Dong X, Song S, Ajani JA. Liquid biopsies in gastrointestinal malignancies: when is the big day? Expert Rev Anticancer Ther. 2018;18(1):19–38. doi: 10.1080/14737140.2018.1403320. [DOI] [PubMed] [Google Scholar]
- 117.Azad TD, Chaudhuri A, Newman AM, Stehr H, Schroers-Martin J, Chabon JJ, Fang P, Qiao Y, Liao ZX, Komaki R, et al. Circulating tumor DNA analysis for outcome prediction in localized esophageal cancer. J Clin Oncol. 2017;35(15_suppl):4055. [Google Scholar]
- 118.Vedeld HM, Goel A, Lind GE. Epigenetic biomarkers in gastrointestinal cancers: the current state and clinical perspectives. Semin Cancer Biol. 2017 doi: 10.1016/j.semcancer.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Mi L, Ji X, Ji J. Prognostic biomarker in advanced gastric cancer. Transl Gastrointest Cancer. 2016;5(1):16–29. [Google Scholar]
- 120.Mallick R, Patnaik SK, Wani S, Bansal A. A systematic review of esophageal MicroRNA markers for diagnosis and monitoring of Barrett’s esophagus. Dig Dis Sci. 2016;61(4):1039–1050. doi: 10.1007/s10620-015-3959-3. [DOI] [PubMed] [Google Scholar]
- 121.Zhang S, Chen L, Jung EJ, Calin GA. Targeting microRNAs with small molecules: from dream to reality. Clin Pharmacol Ther. 2010;87(6):754–758. doi: 10.1038/clpt.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Shomron N. MicroRNAs and pharmacogenomics. Pharmacogenomics. 2010;11(5):629–632. doi: 10.2217/pgs.10.26. [DOI] [PubMed] [Google Scholar]
- 123.Pichler M, Calin GA. MicroRNAs in cancer: from developmental genes in worms to their clinical application in patients. Br J Cancer. 2015;113(4):569–573. doi: 10.1038/bjc.2015.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang K, Wu X, Wang J, Lopez J, Zhou W, Yang L, Wang SE, Raz DJ, Kim JY. Circulating miRNA profile in esophageal adenocarcinoma. Am J Cancer Res. 2016;6(11):2713–2721. [PMC free article] [PubMed] [Google Scholar]
- 125.Tan C, Qian X, Guan Z, Yang B, Ge Y, Wang F, Cai J. Potential biomarkers for esophageal cancer. SpringerPlus. 2016;5:467. doi: 10.1186/s40064-016-2119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Wu HH, Lin WC, Tsai KW. Advances in molecular biomarkers for gastric cancer: miRNAs as emerging novel cancer markers. Expert Rev Mol Med. 2014;16:e1. doi: 10.1017/erm.2013.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Liu H-S, Xiao H-S. MicroRNAs as potential biomarkers for gastric cancer. World J Gastroenterol WJG. 2014;20(34):12007–12017. doi: 10.3748/wjg.v20.i34.12007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Shirmohammadi K, Sohrabi S, Jafarzadeh Samani Z, Effatpanah H, Yadegarazari R, Saidijam M. Evaluation of altered expression of miR-9 and miR-106a as an early diagnostic approach in gastric cancer. J Gastrointest Oncol. 2018;9(1):46–51. doi: 10.21037/jgo.2017.11.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fassan M, Saraggi D, Balsamo L, Realdon S, Scarpa M, Castoro C, Coati I, Salmaso R, Farinati F, Guzzardo V, et al. Early miR-223 upregulation in gastroesophageal carcinogenesis. Am J Clin Pathol. 2017;147(3):301–308. doi: 10.1093/ajcp/aqx004. [DOI] [PubMed] [Google Scholar]
- 130.Song H, Sun W, Ye G, Ding X, Liu Z, Zhang S, Xia T, Xiao B, Xi Y, Guo J. Long non-coding RNA expression profile in human gastric cancer and its clinical significances. J Transl Med. 2013;11(1):225. doi: 10.1186/1479-5876-11-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yang Z, Guo X, Li G, Shi Y, Li L. Long noncoding RNAs as potential biomarkers in gastric cancer: opportunities and challenges. Cancer Lett. 2016;371(1):62–70. doi: 10.1016/j.canlet.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 132.Hao N-B, He Y-F, Li X-Q, Wang K, Wang R-L. The role of miRNA and lncRNA in gastric cancer. Oncotarget. 2017;8(46):81572–81582. doi: 10.18632/oncotarget.19197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Wang H, Lu J, Tang J, Chen S, He K, Jiang X, Jiang W, Teng L. Establishment of patient-derived gastric cancer xenografts: a useful tool for preclinical evaluation of targeted therapies involving alterations in HER-2, MET and FGFR2 signaling pathways. BMC Cancer. 2017;17:191. doi: 10.1186/s12885-017-3177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chen Z, Huang W, Tian T, Zang W, Wang J, Liu Z, Li Z, Lai Y, Jiang Z, Gao J, et al. Characterization and validation of potential therapeutic targets based on the molecular signature of patient-derived xenografts in gastric cancer. J Hematol Oncol. 2018;11:20. doi: 10.1186/s13045-018-0563-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.