Abstract
Background
It is well documented that patients with knee osteoarthritis (KOA) suffer from reduced physical function and that function of the affected knee is improved after knee joint replacement (KJR). However, it remains uncertain whether patients with KOA are less physically active than healthy people and whether patients increase their level of physical activity after surgery to a level comparable with that of healthy people. The aim of this study was to examine whether patients with KOA are less physically active than healthy participants and whether patients who have undergone KJR show an increased activity and achieve the same level of physical activity as healthy participants 5 years postoperatively.
Methods
Fifty-four patients with KOA (29 women; mean age 62 ± 8.6; mean body mass index (BMI) 27 ± 5), 52 patients who had KJR due to KOA 5 years earlier (26 women; mean age 66 ± 7.2; mean BMI 30 ± 5) and 171 healthy participants (76 women, mean age 64 ± 9.7, mean BMI 26 ± 5) were included in this cross-sectional study. The level of physical activity was measured over a mean period of 5.5 days with a triaxial accelerometer mounted on the thigh. Number of daily steps, number of daily short walking bouts of <10 s duration and number of daily transfers from sitting to standing position were recorded. Data were analysed using two sample t tests and were adjusted for age, gender and BMI.
Results
Patients with KOA did not differ significantly from healthy participants regarding daily steps (+321, p = 0.50) or daily transfers from sitting to standing (+1.9, p = 0.52) but performed significantly less daily short walking bouts <10 s (−11.9, p = 0.02). Patients after KJR did not differ significantly from healthy participants regarding daily steps (−281, p = 0.60) of transfers from sitting to standing position (−3.2, p = 0.32) but performed significantly less daily short walking bouts <10 s (−21.7, p = 0.001).
Conclusion
Patients with KOA and KJR showed no significant reduction in number of daily step counts and transfers from sitting to standing position when compared with matched healthy controls. However, the number of short walking bouts was reduced in patients with KOA and by twice as much in patients with KJR. This indicates that KOA and treatment with KJR hardly affect health-related general activity but do affect specific physical activity behaviour potentially indicative of KOA or post-KJR functional limitations.
The translational potential of this article
Activity monitoring with an accelerometer-based method gives insights into health-related general activity levels such as total daily steps and specific parameters such as short walking bouts, which may serve as an objective outcome measure in clinical practice.
Keywords: Accelerometry, Activity monitoring, Knee osteoarthritis, Knee replacement, Physical activity
Introduction
Knee osteoarthritis (KOA) results in pain, stiffness and limitation of movement [1]. High age and overweight are among the most predominant factors in developing KOA [2]. Knee joint replacement (KJR) may be required in end-stage KOA and is known to reduce pain, increase functional ability [2], [3], [4] and improve patients' quality of life [2], [4], [5], [6].
Increased physical activity (PA) is a desired outcome after KJR surgery, and in the early recovery phase, PA seems to be associated with reduced length of hospitalisation [7]. PA is also an important component in the preventive treatment and rehabilitation of patients with KOA. Physical exercise has been shown to relieve pain and stiffness of the knee joint and improve the objectively assessed function [8] and can therefore postpone KJR surgery. Furthermore, PA is well known to decrease the risk of a broad range of lifestyle diseases [9]. Unfortunately, physical inactivity is highly prevalent among patients with KOA [9], [10] contributing to forming a vicious circle; inactivity is a risk factor for KOA, and KOA itself causes more inactivity, which aggravates the symptoms further.
It is well documented that patients with KOA have reduced physical function and that function of the affected knee is improved after KJR. These patients will thus have the potential to lead a more active lifestyle [2], [4]. However, it is uncertain whether patients with KOA are actually less physically active than healthy people, and if so, to which extent, and whether patients increase their level of PA after surgery to a level comparable with that of healthy people [5], [6], [9], [10]. If not, this could be due to adapting to an inactive lifestyle or fear of overloading the operated knee [11].
The literature shows disagreement on whether patients are more physically active during the years after KJR surgery. A selection of studies measuring PA using objective measures suggests that patients only achieve minor increases in their level of PA [5], [6], [9], [10]. In a systematic review, Paxton et al compared the results of 18 studies regarding this issue and found inconclusive results on whether patients increased or decreased their level of PA [9]. The studies showing an increase in the level of PA were primarily based on self-reported data. Self-reported data can be biased as they are affected by pain experience and expectation to own abilities and are thus less suitable for outcome assessment [3]. This is especially true for self-reported data on PA where a review of the most popular instruments showed that none of the reviewed studies used adequate measurement properties; accelerometry was thus recommended for valid assessment [12].
Activity monitoring by an accelerometer-based method is an objective method and is applicable to monitor patients' levels of PA and daily and weekly patterns of PA behaviour [13]. In addition, the method provides a number of parameters tracking the patients' progression in physical performance and daily use of physical capacity, such as number of transfers from sitting to standing and number of walking bouts, which are otherwise solely examined at clinical controls by physical performance tests. This may provide disease- or treatment-specific aspects of outcome and thus serves as a remote monitor of patient function in a translational application.
The aim of this study was to examine whether patients with KOA are less physically active than healthy participants, using selected variables from an accelerometer-based method and then to examine whether patients who have undergone KJR achieve the same level of physical activity as healthy participants 5 years postoperatively.
Materials and methods
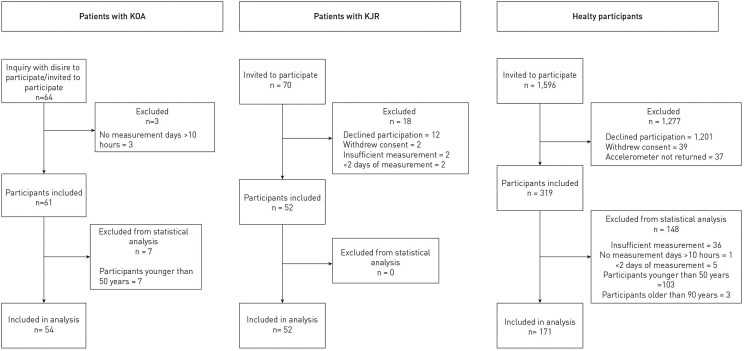
This cross-sectional study included data from three different data collections, among patients in Germany, the Netherlands and healthy participants in Denmark (Figure 1).
Figure 1.
Flow chart of the inclusion of patients in the studies in Germany, the Netherlands and Denmark.
Data on the patients with KOA were collected as part of a German study from Münster University Hospital between February 2016 and February 2017. The patients were recruited through newspaper advertisements and referrals from their doctor or orthopaedic surgeon. The patients were included if they were diagnosed with clinical KOA according to the American College of Rheumatology guidelines and reported pain for 4 or more days of the week for more than 3 months. Nineteen of a 54-patient cohort had unilateral knee symptoms (35.2%), whereas 35 had bilateral symptoms (64.8%). Patients who suffered from medical conditions, other than KOA, that could affect the functional test performance were excluded.
Data on the patients with KJR were collected as part of a Dutch study from Atrium Medical Center, Heerlen between October 2014 and May 2015. Patients were referred to the study through their doctor or orthopaedic surgeon. All patients had primary, unilateral total or unicompartmental knee replacement surgery for KOA 5 years before inclusion. Forty of a 52-patient cohort had unilateral KJR (77%), whereas 12 were bilaterally operated (23%). Patients who suffered from medical conditions that could affect the functional test performance were excluded.
Data on the healthy participants were collected as reference material on PA from Danish people. The study was performed at Aarhus University Hospital in Denmark between April 2014 and April 2016. The participants were randomly selected from the Danish Civil Registration System and were invited to participate by letter.
Accelerometer-based activity monitoring
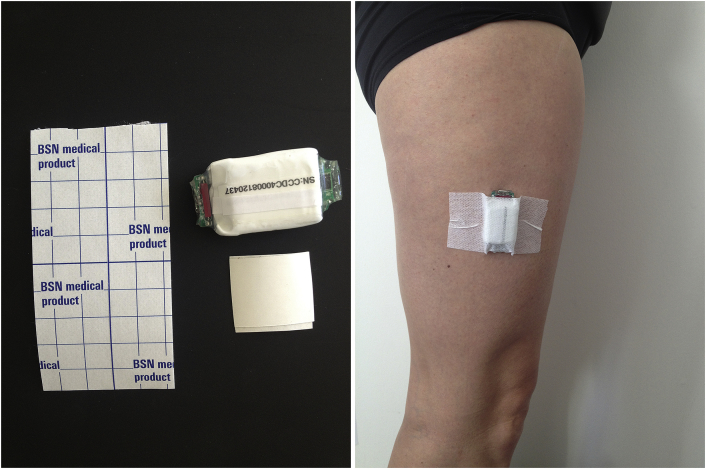
In all three groups of participants, data on the level of PA were collected using a triaxial accelerometer of comparable configurations (X16-mini, GCdataconcepts, USA and AX3, Axivity Ltd., Newcastle, UK) and similar settings mounted on the lateral thigh using adhesive tape (Figure 2). The accelerometer measures accelerations in three dimensions at 100 Hz and stores data on an on-board memory chip for signal postprocessing. The participants wore the accelerometer over a mean of 5.5 consecutive days (Table 1). The accelerometers were not worn at night or during water-based activities, such as swimming or bathing.
Figure 2.
Example of an accelerometer placed on the thigh by adhesive tape.
Table 1.
Characteristics of the three groups; patients with KOA, patients who had KJR 5 years earlier and healthy participants.
| Patients with knee osteoarthritis n = 54 | Patients with knee joint replacement n = 52 | Healthy subjects n = 171 | |
|---|---|---|---|
| Agemean (sd) | 62 (8.6) | 66 (7.2) | 64 (9.7) |
| Gendern (%) | |||
| Female | 29 (54 %) | 26 (50 %) | 76 (44 %) |
| Male | 25 (46 %) | 26 (50 %) | 95 (56 %) |
| BMImean (sd) | 27.4 (4.9) | 29.5 (4.6) | 26.3 (4.8) |
| KOOSmean (sd) | |||
| KOOS-ADL | 63.63 (22.0) | ||
| KOOS-Sport/rec | 35.51 (26.06) | ||
| KOOS-PS | 33.32 (14.19) | ||
| Number of measurement daysmean (sd) | 6.6 (1.1) | 3.8 (0.5) | 6.1 (1.4) |
BMI = body mass index; KJR = knee joint replacement; KOA = knee osteoarthritis; KOOS = Knee injury and Osteoarthritis Outcome Score; SD = standard deviation.
The stored acceleration signal was postprocessed using a previously described algorithm [MATLAB (Mathworks, Natick, MA, USA)] [14], validated for healthy participants and orthopaedic patients with pathology of the lower extremities. One specific feature of the algorithm is that it calibrates through manual selection of a representative period of level walking, which works as an individual reference for distinguishing walking from resting or nonwalking activities (e.g., cycling). This way, participants with a wide range of functionally limited walking ability can reliably be measured including the healthy participants and patients with KOA and KJR of this study. On this basis, overall activities can be classified [14]. For this study, number of daily steps, number of daily short walking bouts of <10 s duration and number of daily transfers from sitting to standing position were calculated. These three parameters were chosen because they were expected to be sensitive for discriminating between high and low level of PA.
Following published consensus, participants with measurement days less than 10 h [15] and participants with less than 2 days of recorded measurements were excluded. Participants younger than 50 years and older than 90 years were also excluded to achieve a comparable range of age in the three groups.
Furthermore, information on age, gender and body mass index (BMI) of the participants was registered, along with Knee injury and Osteoarthritis Outcome Score (KOOS) or KOOS Physical Function Shortform (KOOS-PS) of the patients.
Accelerometer-based activity monitoring has shown high sensibility and retest reliability, and the algorithms used in this study have been previously validated [3], [13], [16], [17], [18], [19], [20].
Statistical analysis
The levels of PA in patients with KOA and patients treated with KJR were compared with the healthy participants separately with two sample t tests. Furthermore, multiple linear regressions were performed to adjust for possible confounding effects by age, gender and BMI. The assumptions of normal distribution were substantiated by histograms and probability plots. A test for interaction between each of the three selected confounders and each of the groups of participants was included in the regression model, but no such interactions were found. Probability values < 0.05 were considered statistically significant. Statistical analyses were performed with STATA IC, version 14.2 (StataCorp, College Station, TX).
Results
The healthy participants from Denmark were comparable with the patients from Germany and the Netherlands regarding common and potential PA-related characteristics such as age, gender ratio and BMI (Table 1).
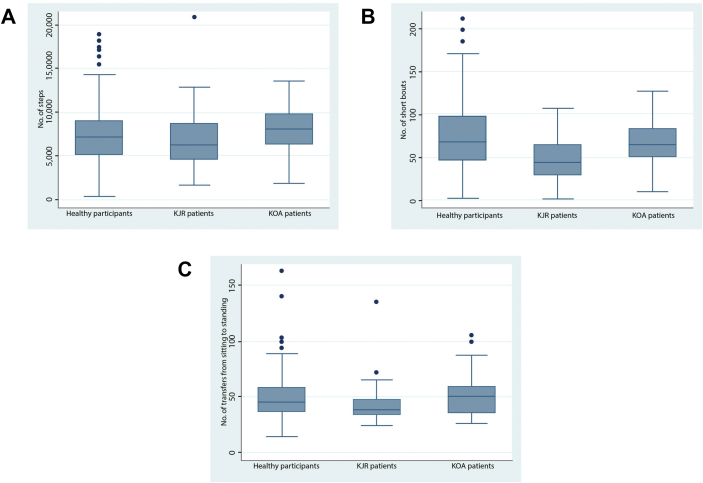
The number of daily steps, short walking bouts and transfers from sitting to standing position is shown in Figure 3A–C. Healthy participants performed an average of 7477 steps per day (SD: 3388), whereas the corresponding number was 7964 steps (SD: 2332) for patients with KOA and 6702 steps per day (SD: 3203) for patients with KJR (Figure 3A).
Figure 3.
(A) Distribution of number of steps per day in the three groups. (B) Distribution of number of short walking bouts per day in the three groups. (C) Distribution of number of transfers from sitting to standing position per day in the three groups: patients with KOA, patients who had KJR 5 years earlier and 171 healthy participants.
On average, healthy participants had 73.9 short walking bouts (SD: 36.9); patients with KOA had 64.8 short walking bouts (SD: 25.2), whereas patients with KJR had 48.7 short walking bouts (SD: 25.9) (Figure 3B).
Healthy participants had an average of 50 transfers from sitting to standing position per day (SD: 21.0), patients with KOA an average of 52 transfers (SD: 18.7) and patients with KJR an average of 43 transfers per day (SD: 16.8) (Figure 3C).
The patients with KOA and the healthy participants were comparable on number of steps and number of transfers; patients with KOA performed significantly fewer short walking bouts (−11.9, −16%) than healthy participants (p = 0.02). No interactions with the three possible confounders were found (Table 2).
Table 2.
Comparison of average number of short walking bouts, number of steps and number of transfers from sitting to standing position per day between healthy participants and patients with KOA.
| Unadjusted estimate |
Adjusted estimatea |
Adjusted estimateb |
|||||
|---|---|---|---|---|---|---|---|
| Coefficient (95 % CI) | p-value | Coefficient (95 % CI) | p-value | Coefficient (95 % CI) | p-value | ||
| No. of steps | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KOA | −487 (−1,298;324) | 0.34 | 273 (−658;1,205) | 0.56 | 321 (−618;1,260) | 0.50 | |
| No. of short walking bouts | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KOA | −9.07 (−0.27;−17.86) | 0.04 | −12.23 (−22.05;−2.41) | 0.02 | −11.92 (−21.82;−2.03) | 0.02 | |
| No. of transfers | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KOA | −1.70 (−8.02;4.62) | 0.60 | 0.74 (−5.48;6.95) | 0.82 | 1.98 (−4.07;8.02) | 0.52 | |
BMI = body mass index; CI = confidence interval; KOA = knee osteoarthritis.
Adjusted for gender and age.
Adjusted for gender, age and BMI.
Patients with KJR and healthy participants were comparable on the number of daily steps and number of transfers, but the number of short walking bouts was significantly lower among patients with KJR (−21.7, −29%) than among healthy participants, when adjusted for gender, age and BMI (p = 0.001). No interactions with the three possible confounders were found in the analyses of steps and short bouts; the BMI seemingly correlated with number of transfers from sitting to standing position. Adjustment for this confounding factor eliminated the significant difference between healthy participants and patients with KJR before adjustment (Table 3).
Table 3.
Comparison of average number of short walking bouts, number of steps and number of transfers from sitting to standing position per day between healthy participants and patients with KJR.
| Unadjusted estimate |
Adjusted estimatea |
Adjusted estimateb |
|||||
|---|---|---|---|---|---|---|---|
| Coefficient (95 % CI) | p-value | Coefficient (95 % CI) | p-value | Coefficient (95 % CI) | p-value | ||
| No. of steps | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KJR | −775 (−1,820;269) | 0.15 | −539 (−1,547;470) | 0.29 | −281 (−1,328;765) | 0.60 | |
| No. of short walking bouts | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KJR | −25.2 (−36.0;−14.4) | 0.001 | −23.1 (−33.2;−13.0) | 0.001 | −21,7 (−32.2;−11.3) | 0.001 | |
| No. of transfers | Healthy subjects | Reference | — | Reference | — | Reference | — |
| Patients with KJR | −7.45 (−13.74;−1.16) | 0.02 | −6.62 (−12.83;−0.41) | 0.04 | −3.18 (−9.43;3.08) | 0.32 | |
BMI = body mass index; CI = confidence interval; KJR = knee joint replacement.
Adjusted for gender and age.
Adjusted for gender, age, and BMI.
Discussion
The aim of this study was to examine whether patients with KOA have decreased levels of PA compared with a matched group of healthy participants. Furthermore, whether patients who have had KJR achieve the same level of PA as healthy participants 5 years postoperatively. The level of PA was measured with selected variables by an accelerometer-based method.
Patients with KOA and healthy participants were comparable on the measures of number of total daily steps and transfers from sitting to standing position. However, when looking at a specific PA behaviour such as the number of short walking bouts per day, patients with KOA turned out to have significantly fewer short walking bouts than healthy participants, indicating a difference in physical capacity.
Furthermore, the analyses showed that the patients with KJR were comparable with healthy participants concerning number of daily steps and transfers from sitting to standing position. Patients with KJR, however, had significantly fewer short walking bouts than healthy participants, again indicating a difference in physical capacity.
These results indicate that the short walking bouts are a sensitive measure to discriminate between patients and healthy participants.
Both patients with KOA and KJR had fewer short walking bouts than healthy participants, which suggests that both groups are affected by their knee conditions. One rationale behind this diverging PA behaviour could be that the affected patients avoid the short walking bouts because of pain, stiffness or reduced strength; they prefer to stay sedentary or gather the short walking trips to fewer but longer walking bouts or avoid walking all together. It may seem contradicting that there is a difference in the number of short walking bouts, but not in the number of transfers from sitting to standing position because steps often follow a transfer. An explanation could be that patients with knee-related disabilities do not avoid getting up but avoid activities that demand standing and walking few steps for a period of time, such as gardening, cooking and cleaning.
Verlaan et al [21] compared patients with end-stage KOA with healthy participants in a cross-sectional study and found that the patients performed both fewer short (<1 min and <5 min) and long (>5 min) walking bouts than healthy participants. These results are in accordance with the findings in the present study suggesting that patients with KOA avoid not only the short walking bouts of a few seconds duration but also the longer bouts lasting several minutes. Moreover, Verlaan et al found that patients with KOA generally spend less time walking and more time sitting than healthy participants.
In a review by Paxton et al [9] comparing the results of 18 studies, results regarding level of PA in patients with KJR compared with patients with KOA awaiting surgery were conflicting. Among the studies with accelerometer-based activity monitoring, an equal number of patients showed an increase, stagnation or a decrease in PA after surgery. Most of the studies reported lower level of PA measured on a selection of parameters, e.g., number of steps, among patients with KJR compared with healthy participants; this is in accordance with the results of the present study. The review and the results of the present study do not provide any clear conclusion to whether patients who have had KJR surgery actually become more physically active than before the surgery even though they gain better function and have less pain.
Limitations
Activity measurement using an accelerometer is an objective and a validated method with a high degree of intertester reliability [14], [22]. From the data collected using the accelerometer, a large number of relevant parameters can be extracted. As such, the method allows for a far more detailed and precise mapping of a participant's PA behaviour than would ever be possible to obtain by self-reported measures. In this study, we only selected three PA variables, though of different nature: a general PA level and health-related parameter such as daily steps, account of a specific event demanding and potentially painful for patients with KOA and KJR such as transfers from sitting to standing position and a parameter expressing PA behaviour in a more qualitative than quantitative way expressed by number of short walking bouts.
A limitation to this study is the different methods of recruitment in the three groups and differences in the background populations. The patients with KOA were partly invited to participate through newspaper advertisements, and it is possible that the participants are a selected group of resourceful patients highly motivated to regain physical function, with a higher level of PA than most patients with KOA. Furthermore, the stage of OA was not specified, and therefore, some patients may only have mild KOA with few symptoms. However, the similarity in the number of daily steps and number of daily transfers indicates that the three groups of participants are comparable. That underlines the difference in the number of short walking bouts as relevant.
The patients with KOA rated their knee function on the KOOS scale, whereas the patients with KJR rated their knee function on the KOOS-PS scale, the short form of the KOOS, which consists of four questions from the Activity of Daily Living subscale (ADL subscale) of KOOS and three questions from the sports/recreation subscale. The two scales are not directly comparable, but they have some overlap (Table 1).
Another limitation to this study is the small groups of both patients with KOA and KJR. A post hoc analysis showed power to be as low as 32% for analyses on the number of daily steps. Only the analysis of the short walking bouts had a sufficient power >80%.
The analyses were adjusted for gender, age and BMI because these three factors were considered to be the most obvious confounders. This adjustment does not eliminate residual confounding, and there are a number of other factors, such as personal habit, socio-economic status and daily need for activity, that may also affect levels of PA. For example, several studies have shown that the weather conditions influence levels of PA [23], [24], [25].
Conclusion
Patients with KOA and patients after KJR showed no significant reduction in the number of total daily steps, the main measure of overall PA, compared with matched healthy controls, nor did they perform significantly less transfers from sitting to standing position. However, the number of short walking bouts was reduced in patients with KOA and by twice as much in patients after KJR. This indicates that KOA and treatment with KJR hardly affect health-related general activity but affects specific behaviour, possibly due to pain, effort or functional limitations. Our results suggest that the number of short walking bouts measured by an accelerometer-based method can be used to discriminate between high and low PA capacity and could be more discriminative than general parameters such as the number of total daily steps.
The knowledge that disease or treatment of KOA may not affect general levels of PA but specific aspects of PA behaviour may be used in clinical practice to educate patients. Moreover, it can be used as an objective outcome measure of function.
Ethical board review statement
Ethical approval was obtained from the Ethik Komission der Ärztekammer Westfalen-Lippe und der Westfälischen Wilhelms-Universität (identifier 2015-475-f-S) and the METC Atrium-Orbis-Zuyd (Medisch Ethische Toetsings Commissie van Atrium, Orbis én van Zuyd Hogeschool), (identifier 10-N-72 and ABR-Nr. 33590).
All authors contributed to the design, acquisition and analysis of the data and/or drafting and revising the manuscript and approved the final manuscript.
Funding
This work has not received any funding.
Conflicts of interest
The authors declare that they have no conflicts of interest.
References
- 1.Schiphof D., de Klerk B.M., Koes B.W., Bierma-Zeinstra S. Good reliability, questionable validity of 25 different classification criteria of knee osteoarthritis: a systematic appraisal. J Clin Epidemiol. 2008 Dec;61(12):1205–1215. doi: 10.1016/j.jclinepi.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Carr A.J. Knee replacement. Lancet. 2012 March 6;379:1331–1340. doi: 10.1016/S0140-6736(11)60752-6. [DOI] [PubMed] [Google Scholar]
- 3.Bolink S. Inertial sensor motion analysis of gait, sit–stand transfers and step-up transfers: differentiating knee patients from healthy controls. Physiol Meas. 2012;33:1947–1958. doi: 10.1088/0967-3334/33/11/1947. [DOI] [PubMed] [Google Scholar]
- 4.Berghmans D. Functioning with knee osteoarthritis and one year after a TKA: are we able to predict functional recovery? Physiotherapy. 2015;101(1):140–141. WCPT Congress 2015. [Google Scholar]
- 5.De Groot I.B. Small increase of actual physical activity 6 months after total hip or knee arthroplasty. Clin Orthop Relat Res. 2008;466:2201–2208. doi: 10.1007/s11999-008-0315-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vissers M.M. Physical functioning four years after total hip and knee arthroplasty. Gait Posture. 2013;38:310–315. doi: 10.1016/j.gaitpost.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Schotanus M.G.M. Physical activity after outpatient surgery and enhanced recovery for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016:1–6. doi: 10.1007/s00167-016-4256-1. 04 August. [DOI] [PubMed] [Google Scholar]
- 8.Kahn T.L., Schwarzkopf R. Do total knee arthroplasty patients have a higher activity level compared to patients with osteoarthritis? Geriatr Orthop Surg. 2016;7(3):142–147. doi: 10.1177/2151458516654518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paxton R.J. Physical activity after total knee arthroplasty: a critical review. World J Orthop. 2015 September 18;6(8):614–622. doi: 10.5312/wjo.v6.i8.614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harding P. Do activity levels increase after total hip and knee arthroplasty? Clin Orthop Related Res. 2014;472:1502–1511. doi: 10.1007/s11999-013-3427-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brandes M. Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthr Care Res. 2011 March;63(3):328–334. doi: 10.1002/acr.20384. [DOI] [PubMed] [Google Scholar]
- 12.Terwee C.B. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthr Cartil. 2011 June;19(6):620–633. doi: 10.1016/j.joca.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Grimm B., Bolink S. Evaluating physical function and activity in elderly patient using wearable motion sensors. Effort Open Rev. 2016 May;1:112–120. doi: 10.1302/2058-5241.1.160022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipperts M. Clinical validation of a body-fixed 3D accelerometer and algorithm for activity monitoring in orthopaedic patients. J Orthop Transl. 2017;11:19–29. doi: 10.1016/j.jot.2017.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Troiano R.P. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 16.Kleijn L.L.A. Functional improvement after unicompartmental knee replacement: a follow-up study with a performance based knee test. Knee Surg Sports Traumatol Arthrosc. 2007;23:1187–1193. doi: 10.1007/s00167-007-0351-7. June; 15. [DOI] [PubMed] [Google Scholar]
- 17.Christiansen C.L. Measuring movement symmetry using tibial-mounted accelerometers for people recovering from total knee arthroplasty. Clin BioMech. 2015;30:732–737. doi: 10.1016/j.clinbiomech.2015.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Senden R. Acceleration-based motion analysis as a tool for rehabilitation – exploration in simulated functional knee limited walking conditions. Am J Phys Med Rehabil. 2011 March;90(3):226–232. doi: 10.1097/PHM.0b013e31820b151a. [DOI] [PubMed] [Google Scholar]
- 19.Laarhoven S.N. Validation of a novel activity monitor in impaired, slow-walking, crutch-supported patients. Ann Phys Rehabil Med. 2016;59:308–313. doi: 10.1016/j.rehab.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Senden R. The importance to including objective functional outcomes in the clinical follow up of total knee arthroplasty patients. Knee. 2011;18:306–311. doi: 10.1016/j.knee.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 21.Verlaan L., Bolink S.A.A.N., Van Laarhoven S.N., Lipperts M., Heyligers I.C., Grimm B. Accelerometer-based physical activity monitoring in patients with knee osteoarthritis: objective and ambulatory assessment of actual physical activity during daly lift circumstances. Open Biomed Eng J. 2015;9:157–163. doi: 10.2174/1874120701509010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tjur M. Validation and inter-tester reliability of a tri-axial accelerometer based classification of daily activities. Abstracts DOS Kongressen. 2014:217. 164, 2014 Oktober: 217. [Google Scholar]
- 23.Feinglass J. The effects of daily weather on accelerometer-measured physical activity among adults with arthritis. J Phys Activ Health. 2011 September;8(7):934–943. doi: 10.1123/jpah.8.7.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Timmermans E.J. The influence of weather conditions on outdoor physical activity among older people with and without osteoarthritis in 6 European countries. J Phys Activ Health. 2016;13:1385–1395. doi: 10.1123/jpah.2016-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins S.M. Quantity and quality of physical activity are influenced by outdoor temperature in people with knee osteoarthritis. Physiother Canada. 2013;65(3):248–254. doi: 10.3138/ptc.2012-39. [DOI] [PMC free article] [PubMed] [Google Scholar]