Abstract
Objective
To evaluate patient engagement with, and the feasibility of, a novel, culturally adapted physiotherapy pain management approach.
Design
A participant-blinded and assessor-blinded pilot randomised controlled trial.
Setting
Outpatient physiotherapy departments at two public hospitals and one district pain clinic.
Participants
Adults (n=48) with chronic musculoskeletal pain (daily pain >3 months), who self-identified as Mandaean, Assyrian or Vietnamese, were randomised to one of two physiotherapy treatment conditions.
Interventions
24 participants underwent combined group and individualised treatment described as ‘culturally adapted physiotherapy’, while 24 underwent evidence-informed ‘usual physiotherapy care’. Both treatment arms consisted of up to 10 sessions over a 3-month period.
Outcome measures
Patient engagement was measured via participant attendance, adherence and satisfaction data. Secondary outcomes included clinical measures of pain severity, interference and suffering, physical function and negative emotional state.
Results
96% of participants undergoing culturally adapted physiotherapy completed treatment, compared with 58% of the usual physiotherapy group. For the culturally adapted group attendance (87%±18%) and adherence (68%±32%) were higher relative to usual care (68%±32% and 55%±43%). Satisfaction was similar for the culturally adapted (82.7%±13.4%) and usual care (79.3±17.3) groups. For secondary outcomes, a significant between-group effect for pain-related suffering in favour of the culturally adapted group was observed with a medium effect size (partial η2 0.086, mean 3.56, 95% CI 0.11 to 7), while results for pain severity, interference, physical function and negative emotional state were similar.
Conclusions
Aligning treatment with the beliefs and values of culturally and linguistically diverse communities enhances patient engagement with physiotherapy. These results support the feasibility of a larger, multisite trial to determine if improved engagement with culturally adapted physiotherapy translates to improved clinical outcomes.
Trial registration number
ACTRN12616000857404; Pre-results.
Keywords: cultural diversity, chronic pain, physical therapy speciality, cultural competency
Strengths and limitations of this study.
This was a randomised, assessor-blinded and participant-blinded controlled trial.
It provides evidence of feasibility of culturally adapted physiotherapy approaches for pain management as explored with three culturally and linguistically diverse communities.
Observed recruitment rates, follow-up rates and preliminary data can inform a future fully powered randomised controlled trial.
As a pilot study, analyses of clinical outcomes are exploratory.
Introduction
Patient engagement is paramount for the delivery of efficient and effective healthcare, reflecting a patients’ relationship with the health encounter, such that they participate (attends and adheres) and recognise value in their treatment (satisfaction and treatment completion).1 2 Research that has evaluated interventions and models of care to enhance patient engagement has provided evidence of success.2 Whether this is true for culturally and linguistically diverse (CALD) communities remains uncertain.1 This is problematic because healthcare must be responsive to the comparatively poorer health status observed in many CALD communities.3 Further, strategies promoting engagement tailored to the needs of CALD communities is vital, particularly given that many countries around the world are now culturally plural societies.
Culturally adapted approaches have been suggested to be an effective strategy to enhance patient engagement and reduce health disparities in CALD communities.1 4 Such approaches speak to more equitable health outcomes for diverse cultures by minimising the risk of a model that results in more favourable outcomes for the dominant, hegemonic culture.4 Systematic reviews and meta-analyses support the use of culturally adapted treatment for mental health conditions, chronic disease management, cancer screening and health promotion.4–8 For example, meta-analyses of mental health interventions demonstrated small to large pooled effect sizes in favour of culturally adapted treatments, compared with usual care.5 6 9 Despite evidence supporting the use of culturally adaptive approaches, research is still lacking for many prominent, debilitating conditions, including for chronic pain.10 As such, suboptimal health outcomes continue to be observed in patients from CALD communities with chronic pain.
Chronic pain disorders contribute to considerable societal burden and personal suffering.11 Many physiotherapy interventions for chronic pain, particularly exercise-based approaches, are safe and effective.12 13 Current evidence-based recommendations suggest that exercise, when combined with cognitive–behavioural and psychosocial treatments, reduces pain, improves quality of life and reduces long-term disability.12 14 However, the efficacy of these approaches has been established in populations speaking the same language, with few studies including CALD and migrant communities.10 The limited research inclusive of CALD communities suggests limited efficacy for pain, quality of life and psychological health outcomes.10 Such uncertainty supports investigation of sociocultural factors that could influence implementation of pain management approaches within CALD communities.15
Successful management of chronic pain requires a strong therapeutic alliance and patient acceptance of, and engagement with, treatment concepts.16 17 Unfortunately, engagement with activity-based treatments is often suboptimal in CALD communities, evidenced by lower attendance, reduced acceptance and premature drop-out from treatment.10 18 Discordant expectations, low patient–provider alliance, cultural–spiritual factors and communication problems have been cited as contributors to suboptimal engagement for CALD communities.19 20 This is perhaps not surprising in the context of intercultural encounters where there is evidence of healthcare provider ethnocentrism, implicit and explicit bias towards patients from CALD backgrounds.21–23 Since engagement with treatment underpins improved patient outcomes,24 it is imperative that strategies are implemented to optimise engagement by CALD populations for costly and debilitating conditions, such as chronic pain.
Thus, the aim of this pilot study was to determine the feasibility, patient engagement and trends of clinical effectiveness of a culturally adapted physiotherapy assessment and treatment approach compared with evidence-informed ‘usual physiotherapy care’. Thus, the research questions for this pilot randomised trial were:
Is a 12-week culturally adapted treatment approach superior to ‘usual physiotherapy care’, in terms of patient engagement (adherence, attendance and satisfaction)?
Is it feasible to deliver and evaluate culturally adapted physiotherapy assessment and treatment approaches across three CALD communities using a randomised controlled trial (RCT) design?
Methods
Design
This was a prospective, multicentre pilot RCT with concealed allocation, and participant and assessor blinding, using a patient sample with chronic pain drawn from three CALD communities (Mandaean, Assyrian and Vietnamese). The trial was conducted across two hospital-based physiotherapy departments and one district pain clinic, between July 2016 and June 2017. A study protocol with eligibility criteria and intervention descriptions was published previously.22 The study was registered with the Australian and New Zealand Clinical Trials Registry (ACTRN12616000857404).
Participants and recruitment
This pilot RCT was the culmination of 3 years of engagement with local Assyrian, Mandaean and Vietnamese communities, facilitated by the multicultural health unit in South-West Sydney Local Health District. Bilingual community educators and multicultural health workers informed the development of the intervention in earlier qualitative phases15 and guided processes in this RCT, ensuring the research team were cognisant of the communities needs and vulnerabilities.
Following consultation with multicultural representatives, it was evident that a broad recruitment strategy was required to be inclusive. This included: (1) recognising the complexity of chronic pain in each community by not excluding participants based on pain location (such as only including low back pain) or psychological comorbidity; (2) considering patients from multiple countries of birth (Iraq, Iran, Syria, Turkey, Jordan and Vietnam) and anyone speaking Arabic, Assyrian or Vietnamese as potentially eligible, especially where data on ethnocultural identification were not available. Ethnocultural identification was then established according to self-identification by the participant at the screening assessment. A total of 94 participants were assessed for eligibility by a physiotherapist not involved in the delivery of interventions and who was bilingual or used the services of an accredited health language interpreter. While a multicultural community representative was not present during recruitment, participants were offered the opportunity to consult community representatives and family members before consenting to participation. This resulted in 48 participants randomised into the study. Inclusion criteria were: adult (≥18 years), non-specific musculoskeletal pain, daily pain of greater than 3 months’ duration, self-identification as a member of the Mandaean, Assyrian or Vietnamese ethnocultural communities, and ability to provide written informed consent in their own language or English. Exclusion criteria were: specific diagnoses necessitating other treatment (ie, complex regional pain syndrome), surgery within the last 3 months and assistance for mobility other than a walking stick, to ensure safety during a group or home-based exercise programme.
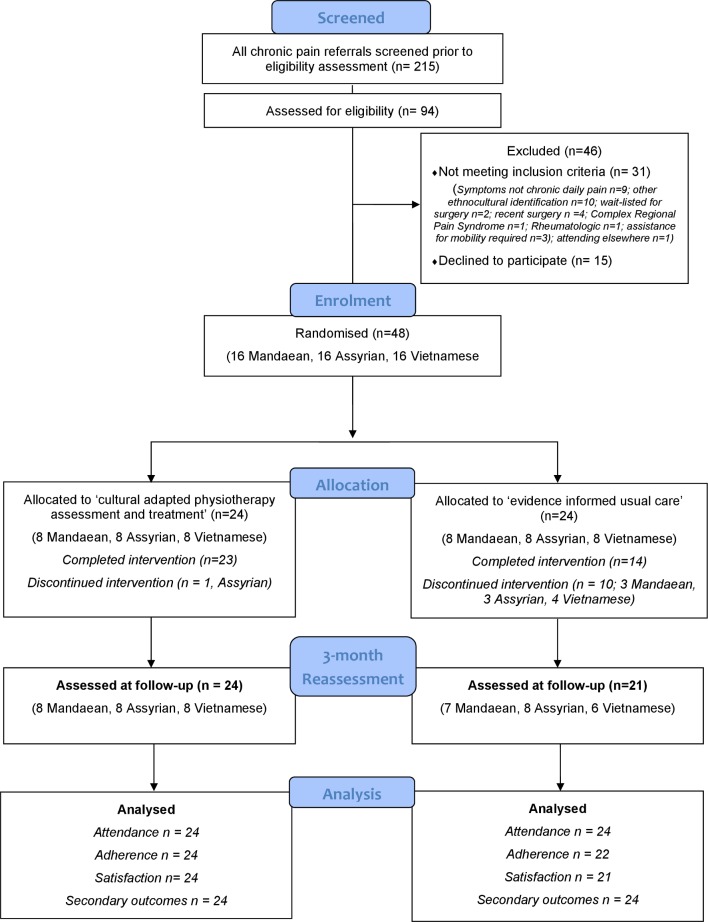
Sixteen participants from each community were allocated randomly to the experimental or control group after baseline assessment (figure 1). Group allocation was determined by a computer-generated sequence with a 1:1 allocation ratio, with each ethnocultural community randomised separately. An independent person prepared sealed opaque envelopes containing the intervention arm, labelled with a participant number according to their entrance sequences. These envelopes were managed securely by a central administrative officer responsible for randomising participants and arranging relevant appointments once a participant had been consented. Participants were blind to treatment allocation and were told the trial was comparing two physiotherapy approaches for chronic pain and it was unknown which was more effective. Thus, participants were unaware that they were receiving culturally adapted treatment approaches for the experimental groups. The success of blinding was assessed at the 3-month reassessment with the question; ‘Do you think your physiotherapist has been trained in culturally responsive treatments for chronic pain?’.
Figure 1.
Flow diagram of the study following consolidated standards of reporting trial guidelines.
Intervention
Participants from intervention and control groups attended for a maximum of 10 sessions of physiotherapy over a 3-month treatment period. A maximum of ‘10’ sessions was selected to enable the treating physiotherapist to tailor interventions to the individual needs of participants, and was consistent with the average number of physiotherapy sessions reported in clinical trials for the management of chronic pain.13 14 All participants were given a home exercise programme designed by their physiotherapist, and they were provided with translated log-books to facilitate recording of exercise adherence. A professional health interpreter was available for all treatment sessions (group and individual), if required, in accordance with best practice.
Culturally adapted physiotherapy assessment and treatment
Participants received a combination of group and individual physiotherapy sessions, adapted to reflect the ethnocultural beliefs and values of the community to which the participant identified. Three ethnocultural-specific group programmes were designed by the research team, informed by qualitative research involving each community and guided by two adaptation frameworks.15 25 Sessions were delivered once per week for 6 weeks, included a combination of education and exercise, and were conducted in groups of eight participants from the same ethnocultural community. Sessions were run by a physiotherapist at a local community facility, and facilitated by a bilingual educator in the language of participants. In addition, group sessions were supplemented by up to four individual sessions tailored to the participant according to the culturally informed initial assessment to ensure consistency with the dose of the control group. Components of the cultural adaptation for each ethnocultural community have been previously published and a summary is presented in online supplementary appendix 1.25
bmjopen-2018-021999supp001.pdf (109.9KB, pdf)
Evidence-informed ‘usual physiotherapy care’
Participants allocated to this condition attended physiotherapy in the outpatient department where they were referred, for treatment informed by evidence-based recommendations for chronic pain. All treating physiotherapists underwent a training session to familiarise them with evidence-based management of chronic pain. Treatment adherence to these guidelines was monitored by review of therapist treatment logs. Treating physiotherapists used their clinical judgement to guide the specifics of treatment according to principles of patient-centred care.26 Following the initial assessment, physiotherapists worked with patients to select the treatment mode (individual or group based), frequency and dose (to a maximum of 10 sessions) tailored to the patient’s needs and goals, consistent with best available evidence.13 27 It is of note that a substantial proportion of research examining the impact of interventions on chronic pain had excluded patients from CALD backgrounds.10
Outcomes
Trained assessors, not involved in the recruitment or treatment of participants and unaware of group assignment, performed assessments according to standardised instructions at baseline (month 0) and (3-month reassessment). Success of assessor blinding was determined with the question; ‘Did you know to which treatment arm the participant belonged?’ If an assessor responded ‘yes’, they were asked to nominate; ‘to which group’.
Data to assess feasibility were collected throughout the trial period regarding recruitment rates, treatment withdrawals, therapist fidelity to evidence-based guidelines, success of participant and assessor blinding, and trial drop-outs. Primary outcome measures were: measures of patient engagement, defined by attendance, and adherence to, and satisfaction with treatment. Attendance was measured as the proportion of sessions attended, relative to the number of sessions scheduled. Adherence was calculated as a percentage of the average number of home exercise sessions completed each week, relative to the number of sessions prescribed, determined from participant log-books or self-report (where the participant was unable or did not complete the log-book).28 Patient satisfaction with treatment was evaluated using the Client Satisfaction Questionnaire (CSQ-8),29 which evaluates satisfaction with treatment generally, and was selected because it has been validated in Arabic and Vietnamese.
Secondary outcomes included core measures recommended by the Initiative on Methods, Measurement and Pain Assessment in Clinical Trials.30 This included measures for pain severity and interference (Brief Pain Inventory: BPI),31 pain-related suffering (Pictorial Representation of Illness and Self Measure: PRISM),32 physical function (6 min walk test: 6MWT, and 1 min sit to stand test: STS test)33 34 and severity of symptoms for Depression, Anxiety and Stress (DASS-21).35 The reliability and validity of these measures, including for Arabic and Vietnamese translations, have been reported previously and were documented in the trial protocol.25
Patient involvement
The research questions were developed following qualitative enquiry into the experience of chronic pain among CALD communities.15 Specifically, challenges raised by participants accessing and participating in pain management in South-West Sydney were incorporated in the study design. As such, participant engagement was considered a primary outcome measure. While patients were not involved in the recruitment and conduct of the study, all participants were given the opportunity to attend a feedback session following trial completion, held in local community venues.
Sample size and statistical analysis
A total sample of 48 participants was deemed appropriate to allow the piloting of a novel culturally adapted programme with three communities (eight participants per programme), while ensuring equal numbers in both treatment arms (24 culturally adapted and 24 usual care) and allowing for the detection of medium to large effects (effect sizes of 0.5–0.8), should they exist.36 37
Descriptive statistics were used to report the characteristics of participants, including means and SDs for continuous variables, and frequencies and proportions (%) for categorical variables. Primary outcome measures (attendance, adherence and satisfaction) were evaluated using descriptive statistics and Mann-Whitney U tests, because data were not normally distributed and transformations did not achieve normality. Effect sizes for non-parametric tests were reported using r and interpreted as large (0.5), medium (0.3) and small (0.1).38
Exploratory examination for group differences in secondary outcome measures was undertaken using a repeated-measures analysis of variance (ANOVA), with the treatment condition (usual care/culturally adapted intervention) as the between-group factor and time of assessment (preintervention or reassessment) as the repeated, within-group factor. One-way repeated measures ANOVAs compared within-group main effects at each time point. Effect sizes were classified as small, medium or large (partial ƞ2 0.01, 0.06, 0.14, respectively).39 If the assumptions of ANOVA were violated, data were transformed to achieve a normal distribution40 before repeating the ANOVA. Intention-to treat analyses were performed for all participants and missing data were addressed by carrying the last data point forward.41 Analyses were performed using the SPSS, V.24.
Results
Feasibility and treatment characteristics
Forty-eight participants, 16 from each ethnocultural community, were randomised within 4 months (figure 1). For the culturally adapted treatment arm, all group sessions were delivered by the physiotherapist who developed the culturally adapted treatment protocols, according to the session manual and verified by review of the therapist log-book. On average, three individual sessions were recommended to supplement the six group sessions (range 1–4). One participant discontinued treatment prematurely, citing illness. For the usual care arm, 14 participants completed the treatment they were allocated. Ten participants withdrew from treatment citing reasons that included illness (n=1), treatment not helping (n=4), lack of time (n=1) and changed mind/sought care elsewhere (n=4). Treating physiotherapists in the usual care arm used both group and individual modes of delivery for 8/24 participants, while individual therapy alone was recommended for 16 participants. Fidelity was evaluated from logbooks completed by each therapist as the percentage of core treatment components included. The components included pain education, goal setting, activity pacing, active coping strategies, flare-up management and a tailored home exercise programme. For the 14 participants who completed treatment, there was 100% therapist fidelity to six core treatment components while for the other participants, an average of four of the six core components were included prior to drop-out, with flare up management and active coping strategies the most commonly omitted elements. Therapist fidelity to evidence-based principles was confirmed for all participants, except for the two participants who withdrew following their initial assessment.
Blinded reassessment data were available for 45 participants, with 3 participants (usual care group) withdrawing from the trial and declining final assessment for similar reasons: ‘treatment has not helped me’, ‘treatment has not done anything to help my leg pain at all’ and ‘treatment has been a waste of time’. As such, the last data point for each was carried forward for all outcomes except satisfaction, for which an initial data point was not available. Success rates for assessor blinding was 91%, while 44% of participants correctly answered the blinding question regarding their therapists’ cultural responsiveness. No participant experienced an adverse event due to participation in the trial.
Demographic and baseline symptom characteristics of participants are displayed in table 1. There were no significant differences between the groups for baseline characteristics.
Table 1.
Participant baseline demographic and symptom characteristics
| Culturally adapted (n=24) |
Usual care (n=24) |
|
| Age (years) | 55 (10.0) | 54 (10.9) |
| Sex, (n) male:female | 5:19 | 4:20 |
| Length of time in Australia, years | 15.5 (12.9) | 14.0 (10.1) |
| Migration circumstances | ||
| Voluntary migrant, n (%) | 6 (25) | 8 (33) |
| Refugee, n (%) | 18 (75) | 16 (67) |
| Marital status—married, n (%) | 16 (67) | 18 (75) |
| Level of education | ||
| No school or primary, n (%) | 9 (38) | 7 (29) |
| Secondary, n (%) | 13 (54) | 13 (54) |
| Tertiary, n (%) | 2 (8) | 4 (17) |
| Duration of pain (years) | 10.0 (7.9) | 8.5 (7.3) |
| Work status | ||
| Full-time or part-time work, n (%) | 1 (4) | 2 (8.3) |
| Unemployed due to pain, n (%) | 18 (75) | 18 (75) |
| Retired, n (%) | 2 (8) | 2 (8.3) |
| Other, n (%) | 3 (13) | 2 (8.3) |
| Receiving pension or benefit, n (%) | 23 (96) | 22 (92) |
| Mean classes of pain medication*/5 | 2.08 (0.78) | 2.08 (0.72) |
| BPI (pain severity)/10 | 7.3 (1.8) | 7.4 (1.3) |
| BPI (pain interference)/10 | 7.7 (1.6) | 7.1 (1.3) |
| DASS subscores/42 | ||
| Depression | 27.6 (12.2) | 26.0 (9.8) |
| Anxiety | 23.9 (12.4) | 23.5 (10.2) |
| Stress | 26.8 (11.4) | 28.8 (8.3) |
| Pain suffering (PRISM)/27 | 3.4 (5.0) | 5.2 (6.4) |
| 6MWT | 266.8 (142.3) | 265.3 (108.7) |
| 1 min STS test | 9.6 (6.5) | 9.4 (6.9) |
Data are presented as mean (±SD) unless otherwise indicated.
*Classes included simple analgesics, compound analgesics, anti-inflammatory, anticonvulsant and opioids.
1 min STS test, 1 min sit to stand test; BPI, Brief Pain Inventory; DASS, Depression Anxiety and Stress Scale; 6MWT, 6 min walk test; PRISM, Pictorial Representation of Illness and Self Measure Separation.
Primary outcomes
Attendance
Overall mean (±SD) attendance at physiotherapy was 8.0±3.1 visits. The culturally adapted treatment group attended a higher number of scheduled sessions compared with ‘usual physiotherapy care’ (mean difference=4.0 sessions, 95% CI 2.6 to 5.3). There was an 87% (±18) attendance rate in the culturally adapted programme, compared with 68% (±32) in the usual care group with a medium between group effect size (U=170, r=0.36).
Home exercise adherence
Home exercise adherence data were available for all participants in the culturally adapted programme (n=24) and 22 participants from the usual care group. Data were absent for two participants who dropped out after their initial visit. Overall, adherence varied from 0% to 100%. The average number of home exercises prescribed was similar for the culturally adapted (n=7, range 2–10) and usual care group (n=6, range 3–11). Overall, the culturally adapted group had a higher adherence rate (88%±15%) relative to usual physiotherapy care (55%±43%), consistent with a moderate between group effect size (U=145, r=0.39).
Satisfaction
Satisfaction data were available for all participants who attended the 3-month blinded assessment (n=45). Overall, 93% of participants were satisfied with treatment, and 71% were highly satisfied, evaluated by a score of greater than 50% and 75%, respectively, for the CSQ-8. Satisfaction between the two groups did not differ. Mean CSQ-8 scores for the culturally adapted and usual physiotherapy care groups were 82.7 (±13.4) and 79.3 (±17.3).
Secondary outcomes
Culturally adapted treatment resulted in greater improvements in pain-related suffering than ‘usual physiotherapy care’, with a medium effect size observed (partial ƞ2 0.086) (table 2). A small effect size was observed for between-group difference in favour of the culturally adapted group for BPI pain interference (partial ƞ2 0.02) and 6MWT (partial ƞ2 0.053), while no effect was observed for BPI pain severity, STS test or the DASS-21 (table 2).
Table 2.
Between-group comparison
| ANOVA time x group | |||
| Between-group comparison of change scores culture–usual mean (95% CI) | F (1,46) value | Partial η2 | |
| BPI pain severity | −0.14 (−1.25 to 0.97)* | 0.063 | 0.001 |
| BPI pain interference† | −0.57 (−1.73 to 0.60)* | 0.962 | 0.020 |
| Pain-self separation† | 3.56 (0.11 to 7.0) | 4.322 | 0.086 |
| 6MWT (m) | 28.44 (−7.40 to 64.28) | 2.551 | 0.053 |
| STS test (reps) | 1.13 (−2.44 to 4.69) | 0.405 | 0.009 |
| DASS depression | −2.67 (−9.03 to 3.69)* | 0.712 | 0.015 |
| DASS anxiety | −2.0 (−8.28 to 4.28)* | 0.411 | 0.009 |
| DASS stress | 0.58 (−4.80 to 5.97)* | 0.048 | 0.001 |
*Minus score in favour of experimental group.
†Transformed data.
ANOVA, analysis of variance; BPI, Brief Pain Inventory; DASS, Depression, Anxiety and Stress Scale; 6MWT, 6 min walk test; STS, sit to stand test.
Sample size estimates
With respect to feasibility for a larger trial based on trial data, for power of 80%, alpha of 5% and a drop-out rate of 20%, a sample size of 124 in each group would be required to detect a clinically significant difference of 50 m for walking distance42 for the intervention group, based on the SD observed in our study of 128 m. This sample size would also be sufficient to identify between-group differences for the BPI Severity (2.2-point difference, SD 2.51) and interference subscales (2.2-point difference, SD 2.55), the PRISM suffering score (3.3 cm difference, SD 8.46) and the DASS total score (13-point difference, SD 31.88). A sample size of 300 would also allow for clinically important between-group differences to be detected for the 1 min STS test (3 repetition difference, SD 8.46).
Discussion
The culturally adapted programme was designed to target-specific language, cultural and access barriers faced by CALD communities that participate in pain management treatments. Results from this pilot study suggest there is an advantage in favour of a culturally adapted physiotherapy programme relative to usual physiotherapy care for addressing barriers to optimal patient engagement. The culturally adapted programmes were well received by all three communities, demonstrated by significantly higher patient engagement (attendance, completion of treatment and adherence) compared with the usual care group. While specific conclusions regarding the efficacy of treatment for clinical outcomes cannot be made, the moderate to small effect sizes observed for the secondary outcomes of pain-related suffering, pain interference and physical function warrant further investigation. Recent systematic reviews of multidisciplinary and exercise-based treatments for chronic pain have revealed pooled effect sizes that are small for function and disability, while pain and psychological health were associated with small effect sizes or no effect, depending on whether care was interdisciplinary or single disciplinary.43–45 In the context of such evidence, the results of this trial support further research into cultural adaptation to maximise the effect on pain and psychological outcomes.
Attendance and treatment retention is an important aspect of patient engagement essential to ensure positive outcomes from cognitive–behavioural and exercise treatments for chronic pain are realised.16 17 Despite this, drop-out from pain management programmes has been reported to be as high as 40%,46 while for exercise-based physiotherapy, drop-out rates of 30%–40% are common.47 48 In the current study, drop-out rates in the ‘usual physiotherapy care’ group (42%) were consistent with rates observed in the literature,18 47 48 while for the ‘culturally adapted’ group, drop-out was less (4%). Further, attendance at scheduled sessions was higher in the ‘culturally adapted’ group, and participants were willing to attend for a greater number of sessions. In combination, such findings suggest that attention to social and ethnocultural dimensions unique to CALD migrant communities successfully engaged participants. For the culturally adapted group, a combination of both surface-level (language, food, music, group interaction and setting) and deep-level (reframing content to align with explanatory models of pain and ethnocultural values) adaptations were included to enhance the cultural relevance of programme content and facilitate patient engagement.25 While programmes were conducted in a similar geographical location (ie, suburb) to the usual care group in the hospital outpatient service, the use of a community venue was an important technique for balancing power differentials in therapeutic relationships and reducing access barriers, thereby contributing to engagement outcomes.49 50 As such broad multidimensional adaptations should be considered in future research.
Treatment adherence is an aspect of patient engagement that has been positively related to patient outcomes in rehabilitation programmes.17 Nevertheless, adherence to exercise interventions for chronic pain conditions is suboptimal.51 For example, adherence rates for osteoarthritis exercise programmes can be as low as 50%,52 and varies between 64% and 71%, respectively, for neck pain and low back pain.51 53 For the current study, there was wide variation in adherence rates for the ‘usual care’ group with a mean of 55% (±43), while for the ‘culturally adapted’ group, adherence was significantly higher and less variable (88%±15%). Low adherence rates in the ‘usual care’ group could have been due to suboptimal communication, patient–provider interactions, and failure to adequately tailor interventions to the sociocultural needs of the individual patient.54 Further, a systematic review28 cited the association between anxiety and depression, highly prominent symptoms in our sample, with reduced adherence to physiotherapy. However, since both treatment arms experienced similar symptoms, this association alone, does not account for the different adherence rates observed. Similarly, the low adherence rate for the ‘usual care’ group could not be ascribed to language barriers, since both groups had similar access to professional interpreting services and translated exercise diaries. Instead, the current findings emphasise a potential role for physiotherapists to optimise the intercultural therapeutic interaction by attending to a patient’s beliefs and values, and aligning treatment components accordingly.
Baseline outcome data from the three CALD communities highlighted participants’ severe pain and psychological symptoms. Participants had higher mean pain duration, and average pain severity scores, than those observed in cohorts attending multidisciplinary pain clinics.55 Similarly, average scores for depression, anxiety and stress according to the DASS-21 were all in the ‘severe’ range, and higher than mean scores observed in a large Australian pain clinic cohort.55 Potentially, such observations were not surprising given 71% of our sample identified as refugees. However, in the context of severe depression, the efficacy of rehabilitation programmes for chronic pain programmes is known to be reduced.56 As such, the physiotherapy approaches employed in our study might be insufficient to induce meaningful changes in pain and psychosocial functioning. While the individualised design of both treatment arms allowed for the involvement of other specialities, such as psychology, participants did not pursue this recommendation in 85% of cases. Such low uptake, in combination with high pain and psychological symptom scores, emphasises a need for treatment adaptations to engage other disciplines and align comprehensive multidisciplinary approaches with the beliefs, values and unique needs of diverse ethnocultural communities. However, the maintained high adherence and attendance data for the culturally adapted group in the presence of high pain scores and psychological symptoms was a positive finding.
Feasibility
Previous research involving CALD communities has identified significant challenges in engagement and retention in clinical research.57 Williams et al 58 enrolled and randomised 78 participants from three CALD backgrounds (Greek, Italian and Vietnamese) living with chronic disease to a medication self-management programme and found less than half completed the post-treatment reassessment (3 months). Similarly, Swerissen et al 59 found a 35% drop-out rate among CALD communities in Australia enrolled to a chronic disease self-management programme. Despite this, our experience supports research inclusive of, and specifically targeted towards, CALD communities. Our high recruitment rates, short recruitment time, absence of adverse outcomes and low trial drop-out rate of 6%, support the feasibility of implementing randomised controlled research trial designs within CALD communities. Specific attention should be given towards involvement of bilingual support workers, professional translation and interpreting services, and engagement of ethnocultural community members in trial design and implementation, to optimise the prospects of the success of our pilot study.10 Further, while cost-effectiveness was not a specific outcome, there were no substantial cost disadvantages of delivering culturally adapted treatment. Both treatment arms were delivered by public health outpatient services. While the cost of hire of community venues was greater ($A1595), this cost was offset by delivering 67% of culturally adapted treatment in groups. Similarly, there were no cost disadvantages of engaging a bilingual support worker in lieu of a health language interpreter, both of which are funded by different sectors of the public health service. This provides further support for feasibility. Finally, sample size estimates using our pilot data inform the feasibility of a fully powered RCT to evaluate the clinical effectiveness of culturally adapted approaches, with the potential to maintain participant engagement.
Study limitations
While the ‘culturally adapted’ programme was successfully piloted across the three ethnocultural communities, it is important to note the study’s limitations. First, participant adherence data relied on self-report. A log book was developed to facilitate recording of adherence, but many participants (15/48) had difficulty completing and/or did not complete the log-book. As such self-report during sessions was used, and therefore data could have been compromised by recall error, or desire to please the treatment provider.60 This is a challenge for researchers working with CALD communities who have linguistic limitations, with a need for reliable, valid measures for recording patient adherence to address such issues. Second, some participants with low education and literacy levels (33% of the sample had either no or primary-level schooling) were challenged by the log-book and scale outcome measures, potentially compromising results. However, the challenge of literacy was similar for both groups and is unlikely to explain any between-group differences because all participants were provided with assistance from the bilingual blinded assessor to interpret and complete outcome measures. Third, 44% of participants were potentially unblinded, based on their responses to the participant blinding question. However, since the difference between the two treatment arms (‘culturally adapted’ versus ‘usual physiotherapy’) and study hypothesis was not disclosed to participants, it is unlikely that this substantially influenced their treatment outcomes. Fourth, since there was no follow-up beyond treatment conclusion, we cannot report the sustainability of treatment gains. Thus, there is a need for long-term outcomes. Finally, current results only relate to the three ethnocultural communities of interest and are not generalisable to broader CALD communities within Australia or internationally. Nonetheless, improved engagement by all three communities highlights that treatment approaches can be effectively adapted to suit individual communities, using a structured adaptation framework.25
A final consideration is the healthcare context within which this study was conducted. Australia is a multicultural society and healthcare providers, including participating physiotherapists, comprise a multitude of ethnocultural, religious and professional identities, that influence their provision of healthcare and the intercultural relationship.61 62 As such, cultural concordance and healthcare provider cultural responsiveness are factors that may have influenced treatment outcomes.63 Future studies may wish to consider the assessment of healthcare provider cultural competence to allow treatment effects to be delineated between adaption elements and therapist characteristics. Culture is a highly complex construct and it must be considered that the culture of healthcare providers, along with the health system itself, will influence treatment outcomes.64
Conclusions
To meet the needs of multicultural populations, interventions should be tailored to the individual, social and ethnocultural factors that influence health. Novel interventions, such as the culturally adapted physiotherapy approaches documented in this study, are likely to be critical for the development of effective pain management approaches that fully engage CALD patients with chronic pain.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the bilingual community educators and volunteers who supported the design and implementation of this trial. Special thanks to the physiotherapy and administrative staff who assisted with aspects of trial implantation and delivery of interventions.
Footnotes
Contributors: All authors made a substantial contribution to this work. Conception, design, analysis and interpretation of data completed by BB under the supervision of IV, SS and LC. All authors involved in interpretation of the data, writing and editing of the manuscript. All authors read and approved the final manuscript.
Funding: This work was supported by the Physiotherapy Research Foundation, grant number S16-005. The development of the culturally adapted assessment protocols used in this trial was supported by a South Western Sydney Local Health District and Ingham Institute Research Scholarship. BB is the recipient of a Sir Robert Menzies Memorial Research Scholarship in the Allied Health Sciences, from the Menzies Foundation, while SS receives salary support from the National Health and Medical Research Council of Australia (1105040).
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: The study was approved by the South Western Sydney Local Health District (SWSLHD) Human Research Ethics Committee (HREC/16/LPOOL/194), Western Sydney University Human Research Ethics Committee (RH11741).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available by contacting the corresponding author at Bernadette.brady@health.nsw.gov.au.
References
- 1. Chen J, Mullins CD, Novak P, et al. Personalized strategies to activate and empower patients in health care and reduce health disparities. Health Educ Behav 2016;43:25–34. 10.1177/1090198115579415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Barello S, Graffigna G, Vegni E, et al. Patient engagement as an emerging challenge for healthcare services: mapping the literature. Nurs Res Pract 2012;2012:1–7. 10.1155/2012/905934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khoo S-E. Ethnic disparities in social and economic well-being of the immigrant aged in Australia. J Popul Res 2012;29:119–40. 10.1007/s12546-012-9080-y [DOI] [Google Scholar]
- 4. Henderson S, Kendall E, See L. The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: a systematic literature review. Health Soc Care Community 2011;19:225–49. 10.1111/j.1365-2524.2010.00972.x [DOI] [PubMed] [Google Scholar]
- 5. Griner D, Smith TB. Culturally adapted mental health intervention: a meta-analytic review. Psychotherapy 2006;43:531–48. 10.1037/0033-3204.43.4.531 [DOI] [PubMed] [Google Scholar]
- 6. Chowdhary N, Jotheeswaran AT, Nadkarni A, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med 2014;44:1131–46. 10.1017/S0033291713001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nierkens V, Hartman MA, Nicolaou M, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLoS One 2013;8:e73373 10.1371/journal.pone.0073373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guadagnolo BA, Petereit DG, Coleman CN. Cancer care access and outcomes for American Indian populations in the United States: challenges and models for progress. Semin Radiat Oncol 2017;27:143–9. 10.1016/j.semradonc.2016.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Harper Shehadeh M, Heim E, Chowdhary N, et al. Cultural adaptation of minimally guided interventions for common mental disorders: a systematic review and meta-analysis. JMIR Ment Health 2016;3:e44 10.2196/mental.5776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brady B, Veljanova I, Chipchase L. Are multidisciplinary interventions multicultural? A topical review of the pain literature as it relates to culturally diverse patient groups. Pain 2016;157:321–8. 10.1097/j.pain.0000000000000412 [DOI] [PubMed] [Google Scholar]
- 11. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hall A, Richmond H, Copsey B, et al. Physiotherapist-delivered cognitive-behavioural interventions are effective for low back pain, but can they be replicated in clinical practice? A systematic review. Disabil Rehabil 2018;40:1–9. 10.1080/09638288.2016.1236155 [DOI] [PubMed] [Google Scholar]
- 13. Kääpä EH, Frantsi K, Sarna S, et al. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine 2006;31:371–6. 10.1097/01.brs.0000200104.90759.8c [DOI] [PubMed] [Google Scholar]
- 14. Sullivan MJ, Adams H. Psychosocial treatment techniques to augment the impact of physiotherapy interventions for low back pain. Physiother Can 2010;62:180–9. 10.3138/physio.62.3.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brady B, Veljanova I, Chipchase L. An exploration of the experience of pain among culturally diverse migrant communities. Rheumatology Advances in Practice 2017;1:1–rkx002. 10.1093/rap/rkx002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hall AM, Ferreira PH, Maher CG, et al. The influence of the therapist-patient relationship on treatment outcome in physical rehabilitation: a systematic review. Phys Ther 2010;90:1099–110. 10.2522/ptj.20090245 [DOI] [PubMed] [Google Scholar]
- 17. Nicholas MK, Asghari A, Corbett M, et al. Is adherence to pain self-management strategies associated with improved pain, depression and disability in those with disabling chronic pain? Eur J Pain 2012;16:93–104. 10.1016/j.ejpain.2011.06.005 [DOI] [PubMed] [Google Scholar]
- 18. Sloots M, Scheppers EF, van de Weg FB, et al. Higher dropout rate in non-native patients than in native patients in rehabilitation in The Netherlands. Int J Rehabil Res 2009;32:232–7. 10.1097/MRR.0b013e32832b081c [DOI] [PubMed] [Google Scholar]
- 19. Mir G, Sheikh A. ’Fasting and prayer don’t concern the doctors… they don’t even know what it is': communication, decision-making and perceived social relations of Pakistani Muslim patients with long-term illnesses. Ethn Health 2010;15:327–42. 10.1080/13557851003624273 [DOI] [PubMed] [Google Scholar]
- 20. Sloots M, Dekker JH, Pont M, et al. Reasons of drop-out from rehabilitation in patients of Turkish and Moroccan origin with chronic low back pain in The Netherlands: a qualitative study. J Rehabil Med 2010;42:566–73. 10.2340/16501977-0536 [DOI] [PubMed] [Google Scholar]
- 21. Drwecki BB, Moore CF, Ward SE, et al. Reducing racial disparities in pain treatment: the role of empathy and perspective-taking. Pain 2011;152:1001–6. 10.1016/j.pain.2010.12.005 [DOI] [PubMed] [Google Scholar]
- 22. Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health 2015;105:e60–e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shen MJ, Peterson EB, Costas-Muñiz R, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities 2018;5:117–40. 10.1007/s40615-017-0350-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013;3:e001570 10.1136/bmjopen-2012-001570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brady B, Veljanova I, Schabrun S, et al. Integrating culturally informed approaches into the physiotherapy assessment and treatment of chronic pain: protocol for a pilot randomised controlled trial. BMJ Open 2017;7:e 014449 10.1136/bmjopen-2016-014449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cheng L, Leon V, Liang A, et al. Patient-centered care in physical therapy: definition, operationalization, and outcome measures. Physical Therapy Reviews 2016;21:109–23. 10.1080/10833196.2016.1228558 [DOI] [Google Scholar]
- 27. Critchley DJ, Ratcliffe J, Noonan S, et al. Effectiveness and cost-effectiveness of three types of physiotherapy used to reduce chronic low back pain disability: a pragmatic randomized trial with economic evaluation. Spine 2007;32:1474–81. 10.1097/BRS.0b013e318067dc26 [DOI] [PubMed] [Google Scholar]
- 28. Jack K, McLean SM, Moffett JK, et al. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther 2010;15:220–8. 10.1016/j.math.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Attkisson CC, Zwick R. The client satisfaction questionnaire. Psychometric properties and correlations with service utilization and psychotherapy outcome. Eval Program Plann 1982;5:233–7. [DOI] [PubMed] [Google Scholar]
- 30. Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19. 10.1016/j.pain.2004.09.012 [DOI] [PubMed] [Google Scholar]
- 31. Keller S, Bann CM, Dodd SL, et al. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain 2004;20:309–18. 10.1097/00002508-200409000-00005 [DOI] [PubMed] [Google Scholar]
- 32. Kassardjian CD, Gardner-Nix J, Dupak K, et al. Validating PRISM (Pictorial Representation of Illness and Self Measure) as a measure of suffering in chronic non-cancer pain patients. J Pain 2008;9:1135–43. 10.1016/j.jpain.2008.06.016 [DOI] [PubMed] [Google Scholar]
- 33. Harding VR, Williams AC, Richardson PH, et al. The development of a battery of measures for assessing physical functioning of chronic pain patients. Pain 1994;58:367–75. 10.1016/0304-3959(94)90131-7 [DOI] [PubMed] [Google Scholar]
- 34. Peppin JF, Marcum S, Kirsh KL. The chronic pain patient and functional assessment: use of the 6-minute walk test in a multidisciplinary pain clinic. Curr Med Res Opin 2014;30:361–5. 10.1185/03007995.2013.828587 [DOI] [PubMed] [Google Scholar]
- 35. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd edn Sydney: Psychology Foundation, 1995. [Google Scholar]
- 36. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008;31:180–91. 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- 37. Whitehead AL, Julious SA, Cooper CL, et al. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res 2016;25:1057–73. 10.1177/0962280215588241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen 2012;141:2–18. 10.1037/a0024338 [DOI] [PubMed] [Google Scholar]
- 39. Richardson JTE. Eta squared and partial eta squared as measures of effect size in educational research. Educational Research Review 2011;6:135–47. 10.1016/j.edurev.2010.12.001 [DOI] [Google Scholar]
- 40. Templeton G. A two-step approach for transforming continuous variables to normal: implications and recommendations for IS research. Communictions of the Association for Information Systems 2011;28:41–58. [Google Scholar]
- 41. Streiner D, Geddes J. Intention to treat analysis in clinical trials when there are missing data. Evid Based Ment Health 2001;4:70–1. 10.1136/ebmh.4.3.70 [DOI] [PubMed] [Google Scholar]
- 42. Perera S, Mody SH, Woodman RC, et al. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9. 10.1111/j.1532-5415.2006.00701.x [DOI] [PubMed] [Google Scholar]
- 43. van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19–39. 10.1007/s00586-010-1518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 2015;350:h444 10.1136/bmj.h444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Geneen LJ, Moore RA, Clarke C, et al. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev 2017;4:CD011279 10.1002/14651858.CD011279.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Martín J, Torre F, Aguirre U, et al. Evaluation of the interdisciplinary PSYMEPHY treatment on patients with fibromyalgia: a randomized control trial. Pain Med 2014;15:682–91. 10.1111/pme.12375 [DOI] [PubMed] [Google Scholar]
- 47. Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine 2004;29:2593–602. [DOI] [PubMed] [Google Scholar]
- 48. Rooks DS, Gautam S, Romeling M, et al. Group exercise, education, and combination self-management in women with fibromyalgia: a randomized trial. Arch Intern Med 2007;167:2192–200. 10.1001/archinte.167.20.2192 [DOI] [PubMed] [Google Scholar]
- 49. Scheppers E, van Dongen E, Dekker J, et al. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 2006;23:325–48. 10.1093/fampra/cmi113 [DOI] [PubMed] [Google Scholar]
- 50. Degrie L, Gastmans C, Mahieu L, et al. "How do ethnic minority patients experience the intercultural care encounter in hospitals? a systematic review of qualitative research". BMC Med Ethics 2017;18:2 10.1186/s12910-016-0163-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. McLean SM, Klaber Moffett JA, Sharp DM, et al. A randomised controlled trial comparing graded exercise treatment and usual physiotherapy for patients with non-specific neck pain (the GET UP neck pain trial). Man Ther 2013;18:199–205. 10.1016/j.math.2012.09.005 [DOI] [PubMed] [Google Scholar]
- 52. Carr A. Barriers to the effectiveness of any intervention in OA. Best Pract Res Clin Rheumatol 2001;15:645–56. 10.1053/berh.2001.0179 [DOI] [PubMed] [Google Scholar]
- 53. Kolt GS, McEvoy JF. Adherence to rehabilitation in patients with low back pain. Man Ther 2003;8:110–6. 10.1016/S1356-689X(02)00156-X [DOI] [PubMed] [Google Scholar]
- 54. Butow P, Sharpe L. The impact of communication on adherence in pain management. Pain 2013;154(Suppl 1):S101–7. 10.1016/j.pain.2013.07.048 [DOI] [PubMed] [Google Scholar]
- 55. Nicholas MK, Asghari A, Blyth FM. What do the numbers mean? Normative data in chronic pain measures. Pain 2008;134:158–73. 10.1016/j.pain.2007.04.007 [DOI] [PubMed] [Google Scholar]
- 56. Bair MJ, Robinson RL, Katon W, et al. Depression and pain comorbidity: a literature review. Arch Intern Med 2003;163:2433–45. 10.1001/archinte.163.20.2433 [DOI] [PubMed] [Google Scholar]
- 57. Gayet-Ageron A, Agoritsas T, Schiesari L, et al. Barriers to participation in a patient satisfaction survey: who are we missing? PLoS One 2011;6:e26852 10.1371/journal.pone.0026852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Williams A, Manias E, Liew D, et al. Working with CALD groups: testing the feasibility of an intervention to improve medication self-management in people with kidney disease, diabetes, and cardiovascular disease. Ren Soc Australas J 2012;8:62–9. [Google Scholar]
- 59. Swerissen H, Belfrage J, Weeks A, et al. A randomised control trial of a self-management program for people with a chronic illness from Vietnamese, Chinese, Italian and Greek backgrounds. Patient Educ Couns 2006;64:360–8. 10.1016/j.pec.2006.04.003 [DOI] [PubMed] [Google Scholar]
- 60. Bollen JC, Dean SG, Siegert RJ, et al. A systematic review of measures of self-reported adherence to unsupervised home-based rehabilitation exercise programmes, and their psychometric properties. BMJ Open 2014;4:e005044 10.1136/bmjopen-2014-005044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Brady B, Veljanova I, Chipchase L. Culturally informed practice and physiotherapy. J Physiother 2016;62:121–3. 10.1016/j.jphys.2016.05.010 [DOI] [PubMed] [Google Scholar]
- 62. Aguilar A, Stupans I, Scutter S, et al. Exploring the professional values of Australian physiotherapists. Physiother Res Int 2013;18:27–36. 10.1002/pri.1525 [DOI] [PubMed] [Google Scholar]
- 63. Horvat L, Horey D, Romios P, et al. Cultural competence education for health professionals. Cochrane Database Syst Rev 2014;5:Cd009405 10.1002/14651858.CD009405.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Betancourt JR, Green AR, Carrillo JE, et al. Cultural competence and health care disparities: key perspectives and trends. Health Aff 2005;24:499–505. 10.1377/hlthaff.24.2.499 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-021999supp001.pdf (109.9KB, pdf)