Abstract
Objective
To determine, using face-to-face diagnostic interviews, the prevalence of common mental disorders (CMD) in a cohort of adult Indigenous Australians, the cultural acceptability of the interviews, the rates of comorbid CMD and concordance with psychiatrists’ diagnoses.
Design
Cross-sectional study July 2014–November 2016. Psychologists conducted Structured Clinical Interviews for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision Axis I Disorders (SCID-I) (n=544). Psychiatrists interviewed a subsample (n=78).
Setting
Four Aboriginal Medical Services and the general community located in urban, regional and remote areas of Southern Queensland and two Aboriginal Reserves located in New South Wales.
Participants
Indigenous Australian adults.
Outcome measures
Cultural acceptability of SCID-I interviews, standardised rates of CMD, comorbid CMD and concordance with psychiatrist diagnoses.
Results
Participants reported that the SCID-I interviews were generally culturally acceptable. Standardised rates (95% CI) of current mood, anxiety, substance use and any mental disorder were 16.2% (12.2% to 20.2%), 29.2% (24.2% to 34.1%), 12.4% (8.8% to 16.1%) and 42.2% (38.8% to 47.7%), respectively—6.7-fold, 3.8-fold, 6.9-fold and 4.2-fold higher, respectively, than those of the Australian population. Differences between this Indigenous cohort and the Australian population were less marked for 12-month (2.4-fold) and lifetime prevalence (1.3-fold). Comorbid mental disorder was threefold to fourfold higher. In subgroups living on traditional lands in Indigenous reserves and in remote areas, the rate was half that of those living in mainstream communities. Moderate-to-good concordance with psychiatrist diagnoses was found.
Conclusions
The prevalence of current CMD in this Indigenous population is substantially higher than previous estimates. The lower relative rates of non-current disorders are consistent with underdiagnosis of previous events. The lower rates among Reserve and remote area residents point to the importance of Indigenous peoples’ connection to their traditional lands and culture, and a potentially important protective factor. A larger study with random sampling is required to determine the population prevalence of CMD in Indigenous Australians.
Keywords: indigenous Australians, common mental disorders, cultural acceptability, aboriginal reserves, SCID-I, regional, metropolitan & remote
Strengths and limitations of this study.
This is the first study to use a face-to-face diagnostic interview capable of diagnosing all common mental disorders in an Indigenous Australian community cohort.
The tool used was culturally acceptable to the participants and showed moderate-to-good concordance with diagnoses made by psychiatrists experienced in Indigenous mental health.
The geographical distribution of our cohort broadly matched that of the general Indigenous Australian population with the exception of remote and very remote residents.
A significant limitation is that our sample was not randomly selected; however, cultural and other factors influence recruitment of Indigenous people for research so approaches differ from those used in mainstream research, and random sampling is highly problematic.
Introduction
Australia’s Indigenous peoples, comprising at least 250 distinct language groups, have inhabited the continent for 50 000–60 000 years and are likely the world’s oldest continuous culture outside Africa.1 At least 700 000 Indigenous people live in Australia, accounting for 3% of the overall Australian population.2 Although estimates are confounded by inadequate or inconsistent data collection,3 little doubt exists that Indigenous Australians have marked health disparities compared with the general population—infant mortality is twofold, lifespan is at least 10 years shorter and death before age 65 years is three to four times more likely.4 Major disparities exist in all key social outcomes.5
As a result of over two centuries of European colonisation, Indigenous Australians have been exposed to multiple risk factors for poor mental health including dislocation from homelands, kinship networks and family, leading to isolation.6 Loss of cultural and spiritual identity, self-esteem, security and happiness have led to a multitude of problems including family violence, welfare dependency, substance and alcohol misuse.7 Lack of understanding between Western and Indigenous concepts of mental disorder has contributed to deficiencies in policies that address these conditions. A burden of disease study done by the Australian Institute of Health and Welfare 20118 reported that disability-adjusted life years (DALY) rates for Indigenous Australians were 2.3-fold higher than those for non-Indigenous Australians. Mental and substance use disorders were the leading cause of both total burden (19% of all DALY) and non-fatal burden (39% of all years living with disability (YLD)).
Despite mental health being estimated as a major contributor to the burden of disease, no robust data are available on the prevalence of common mental disorders (CMD) among Indigenous Australians living in the community. This is because the majority of studies were in criminal justice and mental health settings, or restricted to very remote areas that may not be typical of the general Indigenous population.9 In very remote areas, Indigenous peoples comprise 50% of the total population, and they are more likely to speak an Indigenous language, identify with a clan/tribal group, live on or recognise traditional country, have contact with Elders and not be in the labour force.10 A study conducted in the remote Kimberly region of Western Australia sampled 250 older Aboriginal adults (mean age 61 years, range 46–89) from both isolated and urban populations.11 Using a culturally sensitive tool (Kimberley Indigenous Cognitive Assessment of Depression) that was validated by psychiatrist’s assessments, the prevalence of current major depressive disorder was 4.3%, well above the rate of 1.7% in non-indigenous Australians aged 60 years or older.12
The only published representative study was the National Aboriginal and Torres Strait Islander Social Survey (NATSISS) conducted in 2014–2015 by the Australian Bureau of Statistics.10 This study, however, did not use a diagnostic interview but relied on participants reporting whether a doctor or nurse had told them that they had a mental health condition (depression, anxiety, substance use disorder, behavioural or emotional problems). According to NATSISS, 29% of Indigenous people over 15 years (33.7% of women and 24.6% of men) self-reported that they have a mental health condition. Among those living in remote and very remote areas (22% of the total Indigenous population), the proportion reporting such a condition was half that of those living elsewhere (16.2% versus 33.1%). It is notable that Australia’s ‘benchmark’ mental health prevalence study, the 2007 National Survey of Mental Health and Wellbeing,13 included 8841 from the general population but did not record their Indigenous status. The national prevalence study of children’s mental health (Young Minds Matter)14 specifically excluded Indigenous children.
In this study, we used a structured psychiatric interview (Structured Clinical Interviews for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, Axis I Disorders (SCID-I)15 as opposed to self-reported diagnoses, and a pragmatic recruitment approach, to estimate the standardised prevalence of CMD in a cohort of Indigenous Australians. Our additional objectives were to determine the cultural acceptability of SCID-I, the rates of comorbid CMD and concordance between SCID-I and psychiatrist’s diagnoses.
Methods
Study design
We conducted a cross-sectional prevalence study between July 2014 and November 2016. The main outcome measure was the diagnosis of CMD as assessed by SCID-I.15 Other outcome measures were the cultural acceptability of SCID-1 interviews, rates of comorbid CMD and concordance between SCID-1 and psychiatrist diagnoses.
Participants and recruitment
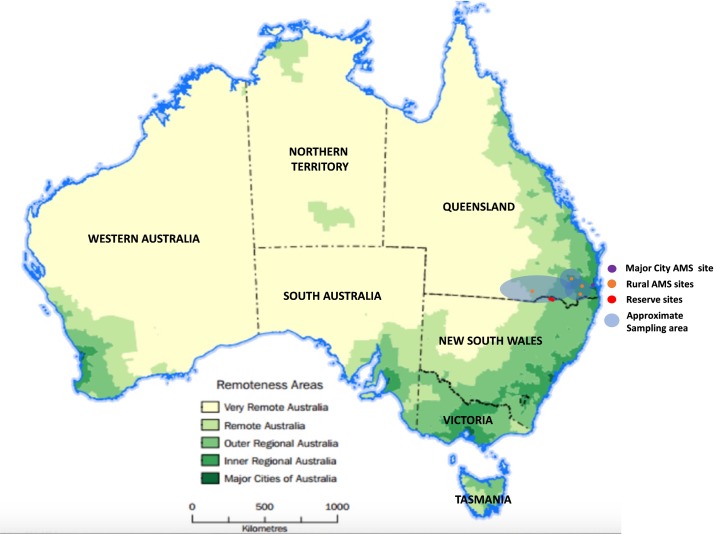
Participants were volunteers identifying as Aboriginal and/or Torres Strait Islander, aged 18 years or older, living in Southern Queensland and an adjacent region in Northern New South Wales (NSW). Those with known cognitive impairment were excluded. Three subgroups were recruited from: (1) three Aboriginal Medical Services (AMS), comprising four sites located in metropolitan, regional and remote areas. AMS are health services funded by the Australian government principally to provide services to Indigenous people. Most are controlled by the local Indigenous community (Aboriginal Community Controlled Health Organisation), approximately 150 operate across Australia; (2) the general community and (3) two NSW Local Aboriginal Land Council (LALC) Reserves, where the majority of the population are Aboriginal people living on their traditional lands (‘on country’). These Reserves arose in 1983 when the NSW government transferred freehold title for 59 historical reserve and mission sites to 49 LALCs in whose area the land was situated, effectively providing Aboriginal collective ownership. The AMS sample was recruited first because of our strong engagement with Elders and community. The three regional/rural AMS that contributed 84.7% of the AMS sample service three local government areas (LGA). They have 6100 registered Indigenous clients and are, therefore, reasonably likely to be representative of the 7786 Indigenous people ≥15 years identified by the 2011 Australian census as resident in these LGA. The total Indigenous population ≥15 years living in the surroundings of the metropolitan AMS is 4197 and the total Indigenous population ≥15 years of the two Reserves is 378. Thus, the total adult Indigenous population of the sampling frame can be estimated as approximately 12 000. Sixty-two per cent of Indigenous Australians live in Queensland and NSW.16 A map of Australia showing remoteness areas, study sites and approximate sampling area is shown in figure 1.
Figure 1.
Map of Australia showing remoteness areas, study sites and approximate sampling area. AMS, Aboriginal Medical Services. Rural denotes Inner Regional, Outer Regional, Remote or Very Remote. The map is based on Australian Bureau of Statistics data.19
Indigenous support workers recruited participants, assisted by posters in the waiting rooms. Recruitment of Reserve and community participants was by word of mouth and ‘snowballing’.17
Patient and public involvement
This research arose when local communities and Indigenous Elders expressed concern about the level of mental illness in their communities and our investigations found that robust evidence was lacking. Our proposal to conduct a prevalence study received overwhelming support from the communities. The involvement of 50 Indigenous participants in a pilot study (see the Cultural appropriateness section) provided valuable feedback on the conduct of the study. Ongoing feedback from all participants was encouraged throughout the study. Participants informally assisted in recruiting via word of mouth and snowballing. On publication of this manuscript, the study results will be disseminated to participants and communities through AMS newsletters. It is expected that MRT will present the results to AMS boards and clients.
Diagnostic tool
SCID-I is conducted by a trained psychologist and uses both clinical judgement and information obtained through the tool to generate diagnoses. Current (30-day), 12-month and lifetime diagnoses are assessed. SCID-I has been validated as a diagnostic tool with high inter-rater, multisite and test–retest reliability,18 although it has not been previously used in Indigenous Australians. Clinical psychologists and Master of Psychology candidates (supervised by the former), trained in the use of the tool and in cultural awareness, conducted the assessments. Participants were provided the option of having an Indigenous Health Worker attend the interview. Weekly clinical supervision by a senior academic clinical psychologist (GB) provided quality control. Psychologists completed diagnosis forms for each participant—a principal diagnosis and up to four other diagnoses were made.
Cultural appropriateness
A pilot study was conducted using SCID-I interviews on 50 consenting Indigenous participants who were asked to provide feedback on cultural issues. Based on qualitative data from the pilot, all participants of the present study were asked to complete a short anonymous open-ended questionnaire that explored cultural issues. Participants responded to questions that investigated how comfortable they felt during the interview, identifying questions that were uncomfortable for them, whether the interviewer understood their responses and if there were any questions that should not be asked of Indigenous people. Survey responses were coded and content analysis performed.
Concordance
A random sample of participants was invited for a clinical interview with a consultant psychiatrist experienced in Indigenous mental health within 6 weeks of a SCID assessment. The psychiatrists did not have access to the SCID assessment at the time of the clinical interview. Concordance was determined using Cohen’s kappa coefficient (κ).
Data analysis and statistical methods
Crude prevalence rates of individual mental disorders and the major classes of disorders were stratified by age group, gender and recruitment location. The latter were categorised according to LGA and the Australian Standard Geographical Classification—Remoteness Area (ASGC-RA)19 system. ASGC-RA 2–5 is considered rural. Standardised prevalence rates were calculated using the 2001 Australian General Population standard and compared with data from the 2007 National Survey of Mental Health and Wellbeing(NSMHWB).13 The NSMHWB survey used WHO Composite International Diagnostic Interview (CIDI), which has high concordance with SCID-I.20 Data were entered in a secure Microsoft Access database and stored within university servers. Access was restricted to authorised staff members.
Results
Participant characteristics
The characteristics of 544 Indigenous participants who completed SCID-I interviews are shown in table 1. As a significant majority (62%) were women, all crude data are presented by gender. The age distribution of the cohort is similar to that of Indigenous Australians nationwide.21
Table 1.
Characteristics of study participants
| Men (n=207) |
Women (n=337) |
Total (n=544) |
|
| Age (mean (SD)) | 41.8 (15.6) | 41.9 (14.2) | 41.9 (14.7) |
| Age group (n (%)) | |||
| 18–24 | 35 (16.9) | 40 (11.9) | 75 (13.8) |
| 25–34 | 40 (19.3) | 81 (24.0) | 121 (22.2) |
| 35–44 | 45 (21.7) | 72 (21.4) | 117 (21.5) |
| 45–54 | 40 (19.3) | 72 (21.4) | 112 (20.6) |
| 55–64 | 25 (12.1) | 46 (13.6) | 71 (13.1) |
| 65+ | 22 (10.6) | 26 (7.7) | 48 (8.8) |
| Indigenous status (n (%)) | |||
| Aboriginal | 195 (94.2) | 324 (96.1) | 519 (95.4) |
| Torres Strait Islander | 5 (2.4) | 3 (0.9) | 8 (1.5) |
| Aboriginal and Torres Strait Islander | 7 (3.4) | 10 (3.0) | 17 (3.1) |
| Recruitment location (n (%)) | |||
| Aboriginal Medical Services | 168 (81.2) | 252 (74.8) | 420 (77.2) |
| Community | 39 (18.8) | 85 (25.2) | 124 (22.8) |
| Reserves | 25 (12.1) | 45 (13.4) | 70 (12.9) |
| Regional distribution | |||
| ASGC-RA 1: Major Cities | 34 (16.4) | 49 (14.5) | 83 (15.3) |
| ASGC-RA 2: Inner Regional | 121 (58.5) | 185 (54.9) | 306 (56.3) |
| ASGC-RA 3: Outer Regional | 45 (21.7) | 85 (25.2) | 130 (23.9) |
| ASGC-RA 4: Remote | 6 (2.9) | 16 (4.7) | 22 (4.0) |
| ASGC-RA 5: Very Remote | 1 (0.5) | 2 (0.6) | 3 (0.6) |
ASGC-RA, Australian Standard Geographical Classification—Remoteness Areas.
Cultural appropriateness results
Four hundred and ninety-eight participants self-completed post SCID-I questionnaires. The vast majority (95.6%) felt totally or mostly comfortable during the interview. Discomfort was related to questions about culture, personal matters, past life events, trauma, alcohol/substance use or because they did not know the psychologist. Eleven (2.2%) said that there were some inappropriate questions and a lack of cultural consideration.
Prevalence of mental disorders
The crude prevalence by diagnosis, diagnostic class, timeframe and gender are shown in table 2. The most common diagnoses were post-traumatic stress disorder (PTSD), phobias and major depressive disorder. A small number of ‘other’ mental disorders present in 3.9% of the sample, including eating, psychotic/delusional, pain and body-dysmorphic disorders, are not included in the standardised data.
Table 2.
Crude prevalence of common mental disorders
| Thirty-day prevalence (n (%)) | Twelve-month prevalence (n (%)) | Lifetime prevalence (n (%)) | |||||||
| Men (n=207) |
Women (n=337) |
Total (n=544) |
Men (n=207) |
Women (n=337) |
Total (n=544) |
Men (n=207) |
Women (n=337) |
Total (n=544) |
|
| Mood disorders | |||||||||
| Major depressive disorder | 19 (9.2) | 37 (10.9) | 56 (10.3) | 24 (11.6) | 47 (13.9) | 71 (13.1) | 38 (18.4) | 92 (27.3) | 130 (23.9) |
| Dysthymic disorder | 4 (1.9) | 11 (3.73 | 15 (2.8) | 4 (1.9) | 11 (3.3) | 15 (2.8) | 5 (2.4) | 12 (3.6) | 17 (3.1) |
| Bipolar disorders | 1 (0.5) | 8 (2.4) | 9 (1.7) | 1 (0.5) | 8 (2.4) | 9 (1.6) | 2 (0.9) | 11 (3.3) | 13 (2.4) |
| Any mood disorder | 35 (16.9) | 63 (18.7) | 98 (18.0) | 42 (20.3) | 75 (22.3) | 117 (21.5) | 66 (31.9) | 131 (38.9) | 197 (36.2) |
| Anxiety disorders | |||||||||
| Panic disorder | 7 (3.4) | 25 (7.4) | 32 (5.8) | 13 (6.3) | 33 (9.8) | 46 (8.5) | 15 (7.2) | 51 (15.1) | 66 (12.1) |
| Social phobia | 13 (6.3) | 29 (8.6) | 42 (7.7) | 13 (6.3) | 32 (9.5) | 45 (8.3) | 20 (9.7 | 41 (12.2) | 61 (11.2) |
| Specific phobia | 17 (8.2) | 37 (10.9) | 54 (9.9) | 17 (8.2) | 38 (10.1) | 55 (10.1) | 20 (9.7) | 46 (13.6) | 66 (12.1) |
| Generalised anxiety disorder | 11 (5.3) | 18 (5.3) | 29 (5.3) | 12 (5.8) | 20 (5.9) | 32 (5.9) | 12 (5.7) | 21 (6.2) | 33 (6.1) |
| Post-traumatic stress disorder | 17 (8.2) | 58 (17.2) | 75 (13.8) | 19 (9.2) | 64 (18.9) | 83 (15.3) | 28 (13.5) | 85 (25.2) | 113 (20.8) |
| Obsessive–compulsive disorder | 5 (2.4) | 8 (2.74 | 13 (2.4) | 5 (2.4) | 9 (2.7) | 14 (2.6) | 5 (2.4) | 11 (3.3) | 16 (2.9) |
| Any anxiety disorder | 47 (22.7) | 123 (36.5) | 170 (31.3) | 53 (25.6) | 133 (39.5) | 186 (34.2) | 68 (32.9) | 165 (49.0) | 233 (42.8) |
| Substance use disorders | |||||||||
| Alcohol abuse | 13 (6.3) | 11 (3.73 | 24 (4.4) | 24 (11.6) | 16 (4.7) | 40 (7.4) | 53 (25.6) | 52 (15.4) | 105 (19.3) |
| Alcohol dependence | 21 (10.1) | 15 (4.5) | 36 (6.6) | 32 (15.5) | 23 (6.8) | 54 (9.9) | 59 (28.5) | 66 (19.6) | 125 (22.9) |
| Substance abuse | 6 (2.9) | 5 (1.5) | 11 (2.0) | 11 (5.3) | 7 (2.1) | 18 (3.3) | 33 (15.9) | 14 (4.2) | 47 (8.6) |
| Substance dependence | 9 (4.3) | 8 (2.74 | 17 (3.1) | 15 (7.3) | 11 (3.3) | 26 (4.8) | 34 (16.4) | 27 (8.0) | 61 (11.2) |
| Any substance use disorder | 42 (20.3) | 31 (9.2) | 73 (13.4) | 58 (28.0) | 44 (13.1) | 102 (18.8) | 113 (54.6) | 113 (33.5) | 226 (41.5) |
| Any mental disorder* | 99 (47.8) | 148 (43.9) | 247 (45.4) | 116 (56.0) | 165 (49.0) | 281 (51.7) | 151 (72.9) | 213 (63.2) | 364 (66.9) |
*Any mental disorder within one or more of the three classes of anxiety, mood and substance use disorders.
The prevalence of CMD standardised against the Australian general population ≥16 years by class and gender is shown in table 3. Rates of lifetime substance use disorders in men were almost double than those in women, while mood and anxiety disorders tended to be higher in women.
Table 3.
Thirty-day, 12-month and lifetime prevalence of common mental disorders by diagnosis class and gender, standardised to and compared with the 2001 Australian general population (95% (CI))
| Men (n=207) |
Women (n=337) |
Total Indigenous (n=544) |
Total NSMHWB*13
(n=8841) |
Rate ratio† | |
| 30-day prevalence | |||||
| Any mood disorder | 16.1 (12.1 to 20.1) | 15.8 (11.8 to 19.8) | 16.2 (12.2 to 20.2) | 2.4 (1.9 to 2.8) | 6.7 |
| Any anxiety disorder | 22.0 (17.5 to 26.6) | 32.4 (27.3 to 37.5) | 29.2 (24.2 to 34.1) | 7.7 (7.0 to 8.5) | 3.8 |
| Any substance use disorder | 19.4 (15.1 to 23.7) | 7.8 (4.8 to 10.7) | 12.4 (8.8 to 16.1) | 1.8 (1.4 to 2.1) | 6.9 |
| Any mental disorder‡ | 45.8 (40.4 to 51.3) | 38.7 (334 to 44.0) | 42.2 (36.8 to 47.7) | 10.0 (9.3 to 10.8) | 4.2 |
| 12-month prevalence | |||||
| Any mood disorder | 19.5 (15.2 to 23.8) | 18.8 (14.5 to 23.1) | 19.5 (15.1 to 23.8) | 6.2 (5.5 to 6.9) | 3.1 |
| Any anxiety disorder | 24.9 (20.2 to 29.7) | 34.9 (29.7 to 40.1) | 31.9 (26.9 to 37.1) | 14.4 (13.4 to 15.3) | 2.2 |
| Any substance use disorder | 26.3 (21.5 to 31.1) | 11.0 (7.6 to 14.4) | 17.1 (12.9 to 21.2) | 5.1 (4.5 to 5.8) | 3.4 |
| Any mental disorder‡ | 53.6 (48.1 to 59.0) | 42.9 (37.6 to 48.4) | 47.9 (42.5 to 53.4) | 20.0 (18.9 to 21.0) | 2.4 |
| Lifetime prevalence | |||||
| Any mood disorder | 30.3 (25.2 to 35.3) | 32.4 (27.2 to 37.5) | 32.2 (27.1 to 37.3) | 15.0 (14.1 to 16.0) | 2.2 |
| Any anxiety disorder | 31.0 (25.9 to 36.1) | 42.4 (37.0 to 47.9) | 38.9 (33.6 to 44.3) | 26.3 (24.9 to 27.6) | 1.5 |
| Any substance use disorder | 49.9 (44.5 to 55.4) | 28.7 (23.8 to 33.7) | 37.2 (31.9 to 42.5) | 24.7 (23.5 to 26.0) | 1.5 |
| Any mental disorder‡ | 68.2 (63.1 to 73.3) | 54.4 (48.9 to 59.8) | 60.6 (55.2 to 65.9) | 45.5 (44.1 to 46.9) | 1.3 |
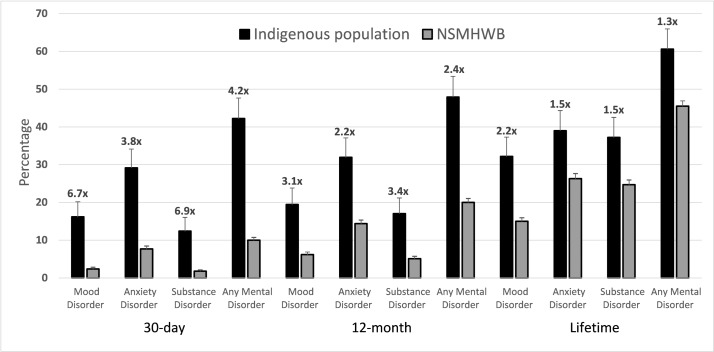
The absolute prevalence of all classes of disorders was higher than in the general Australian population6 particularly for current diagnoses, where mood, anxiety, substance use or any mental disorder was 6.7-fold, 3.8-fold, 6.9-fold and 4.2-fold higher, respectively (table 3 and figure 2). Although the prevalence of 12-month and lifetime disorders remained higher than the general population, the rate ratios were substantially less—2.2-fold to 3.4-fold for 12-month and 1.3-fold to 2.2-fold for lifetime.
Figure 2.
Standardised 30-day, 12-month and lifetime prevalence of common mental disorders among Indigenous Australians compared with the general Australian population. Superscripts are rate ratios; total Indigenous % ÷ total NSMHWB %. NSMHWB, National Survey of Mental Health and Wellbeing.
Subgroup analyses
The rates of current CMD in the AMS and community subgroups were not significantly different. Substantially lower rates, however, were found in the Reserve subgroup, especially for mood and anxiety disorders. For example, the rates of current mood, anxiety and substance use disorders were approximately one-third, one-half and two-thirds, respectively, lower than those in the AMS subgroup (table 4). Nevertheless, they remained higher than those of the Australian general population—2.3-fold for mood disorder, 2.2-fold for anxiety disorder, 4.6-fold for substance use disorder and 2.5-fold higher for any CMD. After stratification by remoteness area (table 5), participants living in major cities, inner and outer regional (ASGC-RA 1–3) areas had similar rates of mental disorders by class and duration. Those living in remote and very remote (ASGC-RA 4–5) (n=25), however, had significantly lower rates of 30-day (approximately one-fifth), 12-month (one-quarter) and lifetime (one-half) CMD.
Table 4.
Standardised prevalence of common mental disorders by subgroup (95% (CI))
| AMS (n=420) |
Community (n=54) |
Reserve (n=70) |
Total (n=544) |
|
| 30-day prevalence | ||||
| Any mood disorder | 17.8 (13.6 to 22.0) | 17.9 (13.7 to 22.1) | 5.5 (3.0 to 8.0) | 16.2 (12.2 to 20.2) |
| Any anxiety disorder | 31.7 (26.6 to 36.8) | 27.9 (23.0 to 32.9) | 17.0 (12.9 to 21.1) | 29.2 (24.2 to 34.1) |
| Any substance disorder | 13.2 (9.5 to 16.9) | 11.3 (7.8 to 14.8) | 8.3 (5.3 to 11.3) | 12.4 (8.8 to 16.0) |
| Any mental disorder* | 45.9 (40.4 to 51.3) | 37.5 (32.2 to 42.8) | 25.4 (20.7 to 30.2) | 42.2 (36.8 to 47.6) |
| 12-month prevalence | ||||
| Any mood disorder | 21.5 (16.9 to 26.0) | 20.3 (15.9 to 24.7) | 6.8 (4.0 to 9.5) | 19.5 (15.1 to 23.8) |
| Any anxiety disorder | 35.2 (29.9 to 40.4) | 29.1 (24.2 to 34.1) | 17.0 (12.9 to 21.1) | 31.9 (26.9 to 37.1) |
| Any substance disorder | 17.5 (13.4 to 21.7) | 15.2 (11.2 to 19.1) | 16.4 (12.3 to 20.4) | 17.0 (12.9 to 21.2) |
| Any mental disorder* | 52.3 (46.8 to 57.8) | 38.7 (33.3 to 44.0) | 30.7 (25.6 to 35.7) | 47.9 (42.5 to 53.4) |
| Lifetime prevalence | ||||
| Any mood disorder | 36.3 (31.0 to 41.6) | 29.7 (24.7 to 34.7) | 9.7 (6.5 to 12.9) | 32.2 (27.1 to 37.3) |
| Any anxiety disorder | 42.8 (37.3 to 48.2) | 31.7 (26.6 to 36.8) | 23.8 (19.1 to 28.4) | 38.9 (33.6 to 44.3) |
| Any substance disorder | 39.6 (34.2 to 44.9) | 36.3 (31.0 to 41.6) | 24.7 (19.9 to 29.4) | 37.2 (31.9 to 42.5) |
| Any mental disorder* | 65.8 (60.6 to 71.0) | 48.2 (42.7 to 53.7) | 40.2 (34.8 to 45.6) | 60.6 (55.2 to 65.9) |
*Any mental disorder: any mental disorder from one or more of the three classes of anxiety, mood and substance use disorders.
AMS, Aboriginal Medical Services.
Table 5.
Standardised prevalence of common mental disorders by remoteness (ASGC-RA) (95% (CI))
| Major Cities (n=83) |
Inner Regional (n=306) |
Outer Regional (n=130) |
Remote/Very Remote (n=25) | |
| 30-day prevalence | ||||
| Any mood disorder | 13.6 (9.9 to 17.7) | 18.2 (13.9 to 22.4) | 16.4 (12.3 to 20.4) | 7.5 (4.6 to 10.3) |
| Any anxiety disorder | 24.7 (19.9 to 29.5) | 36.4 (31.1 to 41.7) | 22.4 (17.7 to 26.9) | 5.3 (2.8 to 7.7) |
| Any substance use disorder | 19.2 (14.9 to 23.5) | 10.0 (6.7 to 13.3) | 14.5 (10.7 to 18.4) | 2.2 (0.6 to 3.8) |
| Any mental disorder* | 42.8 (37.4 to 48.2) | 47.8 (42.3 to 53.2) | 36.9 (31.6 to 42.2) | 7.5 (4.6 to 10.3) |
| 12-month prevalence | ||||
| Any mood disorder | 14.8 (10.9 to 18.7) | 23.0 (18.4 to 27.7) | 17.8 (13.6 to 22.0) | 12.2 (8.6 to 15.7) |
| Any anxiety disorder | 27.5 (22.7 to 32.4) | 39.4 (34.0 to 44.7) | 25.6 (20.8 to 30.4) | 5.3 (2.8 to 7.7) |
| Any substance use disorder | 22.8 (18.2 to 27.4) | 14.5 (10.7 to 18.4) | 20.0 (15.6 to 24.4) | 9.9 (6.7 to 13.3) |
| Any mental disorder* | 48.5 (43.0 to 53.9) | 53.3 (47.8 to 58.8) | 44.3 (38.9 to 49.8) | 12.2 (8.6 to 15.7) |
| Lifetime prevalence | ||||
| Any mood disorder | 24.1 (19.4 to 28.7) | 40.4 (35.0 to 45.8) | 23.4 (18.7 to 28.0) | 22.1 (17.6 to 26.7) |
| Any anxiety disorder | 31.8 (26.7 to 36.9) | 47.4 (42.0 to 52.9) | 31.9 (26.8 to 37.0) | 21.8 (17.3 to 26.4) |
| Any substance use disorder | 39.2 (33.8 to 44.5) | 39.1 (33.8 to 44.4) | 36.4 (31.1 to 41.6) | 17.1 (13.0 to 21.3) |
| Any mental disorder* | 56.2 (50.8 to 61.6) | 68.5 (63.5 to 73.6) | 54.2 (48.8 to 59.7) | 27.1 (22.2 to 32.0) |
*Any mental disorder within one or more of the three classes of anxiety, mood and substance use disorders.
ASGC-RA, Australian Standard Geographical Distribution—Remoteness Areas.
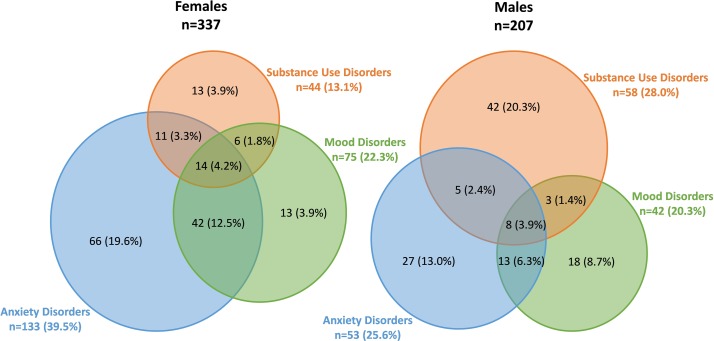
Comorbid mental disorder
Comorbid mental disorder is defined as having diagnoses in two or more classes of CMD. The patterns of comorbid 12-month CMD in women and men showed notable gender differences (figure 3). Among women, 17.5% had two and 4.2% had three classes of comorbid mental disorders; whereas among men, 10.1% had two and 3.9% had three comorbid mental disorders. As in women in the general population,22 comorbid mood and anxiety disorder was the most common combination at 20%. Comorbid mood and anxiety was present in 9.9% of the men. Among those with substance use disorders, 27.6% of men and 70.5% of women had another diagnosis. The rates of comorbid 12-month CMD in this Indigenous population were 4.0-fold higher in women and 3.0-fold higher in men, than reported in the general Australian population (NSMHWB).22 The Reserve subgroup had a much lower rate of comorbid mental disorder than the AMS subgroup—16.8% with any CMD have a diagnosis in more than one class compared with 31.0% in the AMS subgroup.
Figure 3.
Twelve-month crude prevalence of single and comorbid mood, anxiety and substance use disorders among Indigenous women and men.
Concordance of SCID-I and psychiatrist diagnoses
Participants for the concordance study were sampled from all four AMS sites (sampling frame 420) but not from the community (participants scattered over a wide area) or Reserves (250–360 km travel for the two psychiatrists). The agreement (Cohen’s kappa) between SCID-I and psychiatrist diagnoses among 78 participants who consented to both examinations was 0.55 for any mood disorder, 0.58 for any anxiety disorder, 0.67 for any substance use disorder and 0.59 for any CMD. All values of κ are significant at p<0.001.
Psychiatrists tended to diagnose CMD slightly more often than SCID-I: current 43.6% versus 38.5%, 12-month 51.3% versus 42.3% and lifetime 76.9% versus 67.9%. The rate of current psychiatrist diagnoses was 4.4-fold than that of the general population but only 2.7-fold for 12-month and 1.7-fold for lifetime, a pattern similar to the SCID-I results.
Discussion
Prevalence of CMD in Indigenous Australians
We found that the prevalence of any current CMD in this Indigenous cohort is markedly higher than in the general Australian population. Comorbid mental disorder was also much more common. The differences between the Indigenous and the general population, however, were substantially less for 12-month and lifetime disorders. It is implausible that this finding is due to a recent increase in incidence. Non-current diagnoses, whether by SCID-I or psychiatrist, depend on the person’s recall of previous symptoms, episodes or being given a diagnosis by a health professional. Given that Indigenous people may not conceptualise a medical model of mental illness,23 they may not recall such events. This attitude to illness is also likely to result in them not seeking medical advice regarding their symptoms. Furthermore, limited availability of mental health services, especially in rural areas, reduces opportunity to seek medical advice. If Indigenous patients do seek help, practitioners may be overwhelmed by their multimorbid physical disorders, lack confidence in treating mental disorders and have limited options to refer to psychiatric services that are generally only accessible to those with severe mental disorders such as psychosis. The results of psychiatrist interviews also showed lower relative rates of 12-month and lifetime diagnoses. Although the number of psychiatrist interviews was too low (n=78) to provide accurate prevalence data, this finding does suggest that the phenomenon is not just a characteristic of the SCID-I tool.
International comparisons
Limited data on rates of mental disorders are available in Indigenous communities worldwide. In a recent meta-analysis of 19 studies conducted in the Americas,24 no differences were found in the 12-month prevalence of depressive, generalised anxiety and panic disorders between Indigenous and similar non-Indigenous groups. In five studies conducted in Canada, Brazil and the USA that compared rates of depressive disorders in Indigenous with non-Indigenous people, no differences were observed after adjusting for socioeconomic variables (overall OR 1.0). Indigenous people were, however, more likely to have 12-month PTSD and lifetime social phobia, both conditions characterised by fear. This is consistent with our finding that the most frequent 12-month standardised diagnoses were phobias and PTSD. A number of possibilities exist for the difference in our results with those of a meta-analysis from the Americas. One possibility is that some of the studies in the meta-analysis adjusted for more sociodemographic variables than age or sex as in the present study. These included socioeconomic status and educational level. This, however, is unlikely to be the sole explanation, as the lack of any overall difference for many of the outcomes was not greatly affected by adjustment for these variables. Another explanation might be that a sizeable proportion of the participants came from Reserves and, as in the present study, this may have some protective benefits. A third possibility is that there is a true difference between Indigenous peoples of the Americas and Australia such that even on Reserve, Indigenous Australians have higher rates of CMD. An alternative approach is to look at the relative contribution of mental health problems to the burden of disease faced by Indigenous populations.8 25
Subgroup analyses
The AMS and community subgroups have similar high rates of current CMD, suggesting that recruiting through medical facilities has not caused significant bias. The rates of current CMD in the Reserve population are, however, 69% (mood), 46% (anxiety), 37% (substance use) and 45% (any) lower than those in the AMS population despite there being similar major disparities in key social determinants.
Rates of CMD do not appear to be related to the population size of the place of residence of participants, at least within the population range of 12 000 to 110 000. Those living in remote or very remote areas (at least 450–500 km from a metropolitan area) appear, however, to have markedly lower rates. This result should be interpreted with caution because of the small number, although it is consistent with the results of the 2014–2015 NATSISS (approximately 2500 remote Indigenous adults)10 and a study of 250 older Indigenous Kimberly residents.11 Importantly, many Indigenous Australians living in remote/very remote areas live on traditional lands and in discrete majority-Indigenous communities. Our Reserve cohort resides in an area classified as Outer Regional although just 40 km from the Remote area boundary. Thus, it is not clear whether the lower rates of CMD is related to living in remote areas, in discrete communities, or on traditional land.
Strengths and limitations
This is the first study to use a face-to-face diagnostic interview capable of diagnosing all CMD in an Indigenous Australian cohort. The tool used was culturally acceptable to the participants and showed moderate-to-good concordance with diagnoses made by psychiatrists experienced in Indigenous mental health.
Although the majority of participants were recruited in cities and towns, the distribution of their residential addresses matched the ASGC-RA distribution of the Indigenous Australian population with the exception of remote and very remote. It should be noted, however, that the NSMHWB13 did not include very remote areas so the prevalence of mental disorders in the general Australian population living in such areas is also unknown. Nevertheless, given the lower prevalence among remote/very remote area residents, the fact that only 4.6% of our sample, compared with 21.4% of the overall Indigenous population, live in these areas is a significant weakness. Likewise, we have only sampled two Reserves.
Our prevalence rates have not been adjusted for socioeconomic variables, which are generally recognised to be associated with mental disorders.26 In Australia, however, data from the 2007 NSMHWB (n=6558)27 show that only those in the highest quintile of Index of Relative Social Disadvantage (IRSD) (ie, the most advantaged) had lower rates of CMD than those in the other four quintiles, with no evidence of ‘dose’ effect. Having any mental disorder was not associated with area of residence categorised as ‘major urban’, ‘other urban’ or other. These data suggest that the very high rates of mental disorder in our cohort are unlikely to be related to their low IRSD or area of residence, although remote or very remote residence may be an exception.
A significant limitation is that our sample was not randomly selected. It is important to understand, however, that cultural and other factors influence recruitment of Indigenous people for research so approaches differ from those used in mainstream research, and random sampling is highly problematic. Laycock et al28 have articulated the guiding principles of research in Indigenous Australians spirit and integrity; reciprocity; respect; equality; survival and protection; and responsibility. The barriers and enablers of randomised sampling and recruitment in larger Indigenous epidemiological studies have been documented by Fox et al29 and Marin et al.30 A prerequisite is meaningful and respectful engagement with Indigenous communities using community-specific approaches. Individuals in such communities volunteer to participate and do not appreciate the Western concept of being randomised ‘in’ or ‘out’ of the study, the latter being considered disrespectful. Some other barriers to randomised recruitment include the transient nature of Indigenous populations and households, the lack of robust site-specific population and household data,31 cultural requirements to attend funerals (‘sorry business’) and other community functions, high-turnover of Indigenous staff, kinship structures within communities and high rates of substance abuse in some communities. In an example of a pragmatic approach to recruitment, Brown and colleagues used non-random sampling of 436 Indigenous Australians living in remote, peri-urban (‘Town Camps’) and urban areas of the Northern Territory to conduct a cross-sectional prevalence study of the burden and determinants of cardiovascular and metabolic risk.32
The future
Indigenous Australians are culturally, geographically and sociologically diverse so a much larger study will be required to determine the total population prevalence of CMD, including further studies in Reserve and remote populations. Clearly, self-report surveys are inadequate: our findings highlight the importance of formal face-to-face diagnostic interviews using instruments such as SCID-I or CIDI33 rather than self-report surveys, in obtaining accurate estimates of mental illness, although even with these, our results suggest that the diagnosis of past disorders is problematic in Indigenous populations.
In 2007, the Council of Australian Governments pledged to close key gaps in outcomes between Indigenous and non-Indigenous Australians. The Closing the Gap Program developed specific targets to reduce inequalities in Indigenous life expectancy, mortality, education and employment but a decade later only three of seven of the current targets (those relating to child mortality, early childhood education and final year high school achievement) are on track to achieve targets.34 Recently, ‘Closing the Gap Refresh’ that aims to develop more appropriate and operational targets was launched.
Closing the Gap is an agreed Australian national priority35 and a strong case exists for Indigenous mental health to be a specific national priority. Thus, it is encouraging that Aboriginal and Torres Strait Islander Mental Health and Suicide Prevention is listed as a Priority Area in the Fifth National Mental Health Plan.36
Programmes addressing Indigenous mental health should incorporate the Indigenous concept of Social and Emotional Wellbeing, which recognises the importance of connection to land, culture, spirituality, ancestry, family and community, and how these affect the individual.6 In addition, given the likely benefit of early diagnosis and treatment of mental disorders,37 routine screening may be warranted.
Our finding of much lower rates of CMD in Reserve and remote area residents suggests that the connection of Indigenous peoples to their traditional lands and their communities is an important determinant of their mental health. Thus, the possibility exists that facilitating the reconnection of Indigenous Australians to their lands may enhance their social and emotional wellbeing, and their mental health.38 39 Major barriers, however, to reconnection exist—historic events such as forced removal have broken the connections40 and native title has been ‘extinguished’ by urbanisation and agricultural development. It seems that under current Australian Native Title legislation, those most in need of reconnection with their lands are the least likely to achieve it.
Maintaining existing and building new connections to ‘country’ for Indigenous Australians is arguably best achieved by economic development within traditional lands/homelands by facilitating economic participation and leveraging land assets.34 For example, 43% of all land in the Northern Territory (ie, 0.6 million km2) is held under Native Title. Australian government programmes to build Indigenous economies such as the Indigenous procurement policy and the proposed Indigenous business sector strategy hold promise.
Supplementary Material
Acknowledgments
The authors sincerely thank the study participants who contributed their time and energy in completing the interviews and providing feedback. They are most grateful for the generous help provided by AMS staff and the strong support of Community Elders and Leaders. They also thank the Masters of Psychology candidates for their contribution to the interviews.
Footnotes
Contributors: BFN: study project officer, data collection, maintenance of database, statistical analyses and wrote manuscript draft. MRT: senior Aboriginal academic, principal chief investigator and oversight of the entire project, concept and design of the study, engagement with indigenous communities, cultural matters oversight, editing and approval of the manuscript. SK-C: chief investigator, supervision of epidemiology and biostatistics, data analyses, editing and approval of the manuscript. SK: chief investigator, senior academic psychiatrist, clinical psychiatry oversight, psychiatric examinations, data analyses, editing and approval of the manuscript. NSG: academic psychiatrist, psychiatric examinations, clinical psychiatry advice, editing and approval of the manuscript. EB: academic psychologist, conducted SCID examinations, design of the study, data analyses, editing and approval of the manuscript. NH: chief investigator, senior Aboriginal leader, clinician and academic, cultural guidance, editing and approval of the manuscript. GR: chief investigator, study design, editing and approval of the manuscript. GB: senior academic psychologist, supervised all psychologists, quality control of SCID examinations, editing and approval of the manuscript. RO: analyses of comorbidities, editing and approval of the manuscript. GCN: chief investigator, concept, design and analyses of the study and wrote final version of manuscript.
Funding: This study was funded by National Health and Medical Research Council, Australia, Project Grant 1061963.
Disclaimer: The study funder had no role in the study design, planning, data collection, analysis, interpretation or manuscript preparation of this study.
Competing interests: MRT is an Aboriginal woman who is Chair of the Board of one of the participating AMS but played no role in the decision of the AMS to participate in the study.
Patient consent: Obtained.
Ethics approval: The University of Queensland Human Research Ethics Committee approved the study (clearance number: 2012001315) as did the Boards of Directors of the AMS. Permission from Indigenous Elders was obtained prior to recruiting from the reserves and communities. The study was conducted according to National Health and Medical Research Council of Australia Guidelines (Values and Ethics: Guidelines for Ethical Conduct in Aboriginal and Torres Strait Islander Health Research, National Health and Medical Research Council of Australia, 2003).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The University of Queensland (UQ) Human Ethics Committee imposes restrictions on the data. Anonymised data are available to researchers who meet the conditions of the ethics approval and research governance policy that applies to this study via UQ eSpace. Requests for the data may be sent to the Director of Research, Rural Clinical School, UQ (rcsrc@uq.edu.au).
Author note: In this article, we respectfully refer to Aboriginal and Torres Strait Islander Peoples as Indigenous Australians or Indigenous people(s).
References
- 1.Rasmussen M, Guo X, Wang Y, et al. An Aboriginal Australian genome reveals separate human dispersals into Asia. Science 2011;334:94–8. 10.1126/science.1211177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AIHW. The health and welfare of Australia’s Aboriginal and Torres Strait Islander People. Canberra: Australian Institute of Health and Welfare, 2011. [Google Scholar]
- 3.Rosenstock A, Mukandi B, Zwi AB, et al. Closing the Gaps: competing estimates of Indigenous Australian life expectancy in the scientific literature. Aust N Z J Public Health 2013;37:356–64. 10.1111/1753-6405.12084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.AIHW. Mortality and life expectancy of Indigenous Australians, 2009-12. Canberra: Australian Institute of Health and Welfare, 2014. [Google Scholar]
- 5.Anderson I, Crengle S, Kamaka ML, et al. Indigenous health in Australia, New Zealand, and the Pacific. Lancet 2006;367:1775–85. 10.1016/S0140-6736(06)68773-4 [DOI] [PubMed] [Google Scholar]
- 6.Hunter E, Gill N, Toombs M. Mental health among Indigenous Australians: Indigenous Australians and Health: The Wombat in the Room: Oxford University Press, 2013. [Google Scholar]
- 7.Parker R. Australia’s aboriginal population and mental health. J Nerv Ment Dis 2010;198:3–7. 10.1097/NMD.0b013e3181c7e7bc [DOI] [PubMed] [Google Scholar]
- 8.AIHW. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2011. Canberra: Australian Institute of Health and Welfare, 2016. [Google Scholar]
- 9.Black EB, Ranmuthugala G, Kondalsamy-Chennakesavan S, et al. A systematic review: identifying the prevalence rates of psychiatric disorder in Australia’s Indigenous populations. Aust N Z J Psychiatry 2015;49:412–29. 10.1177/0004867415569802 [DOI] [PubMed] [Google Scholar]
- 10.ABS. 4714.0 National Aboriginal and Torres Strait Islander Social Survey, 2014-15. Canberra: Australian Bureau of Statistics, 2016. [Google Scholar]
- 11.Almeida OP, Flicker L, Fenner S, et al. The Kimberley assessment of depression of older Indigenous Australians: prevalence of depressive disorders, risk factors and validation of the KICA-dep scale. PLoS One 2014;9:e94983–7. 10.1371/journal.pone.0094983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pirkis J, Pfaff J, Williamson M, et al. The community prevalence of depression in older Australians. J Affect Disord 2009;115:54–61. 10.1016/j.jad.2008.08.014 [DOI] [PubMed] [Google Scholar]
- 13.Slade T, Johnston A, Oakley Browne MA, et al. 2007 National Survey of Mental Health and Wellbeing: methods and key findings. Aust N Z J Psychiatry 2009;43:594–605. 10.1080/00048670902970882 [DOI] [PubMed] [Google Scholar]
- 14.Lawrence D, Johnson S, Hafekost J, et al. ; Young Minds Matter(YMM): the mental health of children and adolescents. Department of Health: Report on the second Australian Child and Adolescent Survey of Mental Health and Wellbeing Canberra, 2015. [Google Scholar]
- 15.First M, Spitzer R, Gibbon M, et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders- Non-Patient Edition (SCID-I/NP, 1/2010 revision). New York: Biometrics Research Department, New York State Psychiatric Institute, 2010. [Google Scholar]
- 16.ABS. 2071.0 - Census of population and housing: reflecting Australia - stories from the census, 2016. Canberra: Australian Bureau of Statistics, 2017. [Google Scholar]
- 17.Johnson T. Snowball Sampling: Introduction Wiley StatsRef: Statistics Reference Online, 2014. [Google Scholar]
- 18.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother 2011;18:75–9. 10.1002/cpp.693 [DOI] [PubMed] [Google Scholar]
- 19.ABS. Australian Statistical Geography Standard (ASGS): Volume 5 - remoteness structure. Canberra: Australian Bureau of Statistics, 2011. [Google Scholar]
- 20.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res 2006;15:167–80. 10.1002/mpr.196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ABS. 3238.0.55.001 - Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. Canberra: Australian Bureau of Statistics, 2013. [Google Scholar]
- 22.Teesson M, Slade T, Mills K. Comorbidity in Australia: findings of the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 2009;43:606–14. 10.1080/00048670902970908 [DOI] [PubMed] [Google Scholar]
- 23.Ypinazar VA, Margolis SA, Haswell-Elkins M, et al. Indigenous Australians' understandings regarding mental health and disorders. Aust N Z J Psychiatry 2007;41:467–78. 10.1080/00048670701332953 [DOI] [PubMed] [Google Scholar]
- 24.Kisely S, Alichniewicz KK, Black EB, et al. The prevalence of depression and anxiety disorders in indigenous people of the Americas: A systematic review and meta-analysis. J Psychiatr Res 2017;84:137–52. 10.1016/j.jpsychires.2016.09.032 [DOI] [PubMed] [Google Scholar]
- 25.Leske S, Harris MG, Charlson FJ, et al. Systematic review of interventions for Indigenous adults with mental and substance use disorders in Australia, Canada, New Zealand and the United States. Aust N Z J Psychiatry 2016;50:1040–54. 10.1177/0004867416662150 [DOI] [PubMed] [Google Scholar]
- 26.Ngui EM, Khasakhala L, Ndetei D, et al. Mental disorders, health inequalities and ethics: A global perspective. Int Rev Psychiatry 2010;22:235–44. 10.3109/09540261.2010.485273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Enticott JC, Meadows GN, Shawyer F, et al. Mental disorders and distress: Associations with demographics, remoteness and socioeconomic deprivation of area of residence across Australia. Aust N Z J Psychiatry 2016;50:1169–79. 10.1177/0004867415615948 [DOI] [PubMed] [Google Scholar]
- 28.Laycock A, Walker D, Harrison N, et al. ; Researching indigenous health: a practical guide for researchers. Melbourne: The Lowitja Institute, 2011. [Google Scholar]
- 29.Fox S, Arnold AL, Dunn R, et al. Sampling and recruitment methodology for a national eye health survey of Indigenous Australians. Aust N Z J Public Health 2010;34:554–62. 10.1111/j.1753-6405.2010.00635.x [DOI] [PubMed] [Google Scholar]
- 30.Marin T, Taylor AW, Grande ED, Dal Grande E, et al. Culturally appropriate methodology in obtaining a representative sample of South Australian Aboriginal adults for a cross-sectional population health study: challenges and resolutions. BMC Res Notes 2015;8:200 10.1186/s13104-015-1080-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor J. Data issues for regional planning in aboriginal communities, centre for aboriginal economic policy research. Canberra: The Australian National University, 2003. [Google Scholar]
- 32.Brown A, Carrington MJ, McGrady M, et al. Cardiometabolic risk and disease in Indigenous Australians: the heart of the heart study. Int J Cardiol 2014;171:377–83. 10.1016/j.ijcard.2013.12.026 [DOI] [PubMed] [Google Scholar]
- 33.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res 2004;13:93–121. 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Commonwealth of Australia Department of the Prime Minister and Cabinet. Closing the gap - prime ministers report, 2017. [Google Scholar]
- 35.National aboriginal and torres strait islander health plan 2013-2023. Canberra, 2013. [Google Scholar]
- 36.Department of Health. Fifth National mental health plan. Canberra: Australian Government, Department of Health, 2016. [Google Scholar]
- 37.Kisely S, Scott A, Denney J, et al. Duration of untreated symptoms in common mental disorders: association with outcomes: International study. Br J Psychiatry 2006;189:79–80. 10.1192/bjp.bp.105.019869 [DOI] [PubMed] [Google Scholar]
- 38.Burgess P, Morrison J. Social determinants of Indigenous health : Carson B, Dunbar T, Chenhall R, et al. Sydney: Allen & Unwin, 2007:177–202. [Google Scholar]
- 39.Scrimgeour D. Town or country: which is best for Australia’s Indigenous peoples? Med J Aust 2007;186:532–3. [DOI] [PubMed] [Google Scholar]
- 40.Calma T. A human rights based approach to social and emotional wellbeing. Australas Psychiatry 2009;17(Suppl 1):S15–S19. 10.1080/10398560902948613 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.