Cardiopulmonary resuscitation–induced consciousness (CPRIC) is a phenomenon that is receiving increasing attention, and of which family physicians and all care providers with advanced cardiac life support skills should be aware. It has been hypothesized that owing to a variety of physiologic variables, such as autoregulation, comorbidities, and cerebral ischemic thresholds, it is possible for patients receiving high-quality cardiopulmonary resuscitation (CPR) to maintain consciousness.1–3 The case presented here is of a younger man who appeared to regain consciousness several times during CPR.
Case
A 38-year-old man presented to the emergency department in a remote regional hospital staffed by family physicians. He had a 4-hour history of retrosternal chest pain radiating into his neck. In the hour before presentation the patient had also developed lightheadedness and diaphoresis. The patient had type 2 diabetes, for which he took no medications, and he smoked approximately 10 cigarettes daily. He also had a relevant family history of coronary artery disease and early myocardial infarction.
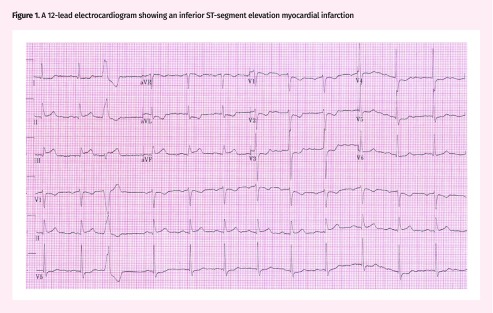
On presentation the patient was alert, pale, diaphoretic, and visibly ill. Vital signs were taken at triage and the patient was found to have a blood pressure of 83/50 mm Hg and a heart rate of 34 beats/min. He was transferred to the resuscitation room and a 12-lead electrocardiogram was obtained, which showed an inferior ST-segment elevation myocardial infarction (Figure 1). The patient was immediately administered 320 mg of acetylsalicylic acid to chew, 300 mg of clopidogrel by mouth, and a litre bolus of normal saline intravenously for a suspected right ventricular infarct. After receiving fluid resuscitation the patient’s blood pressure and heart rate were 158/107 mm Hg and 77 beats/min, respectively. The anticipated transfer time for percutaneous coronary intervention for this patient was approximately 5 hours, and the patient had no contraindications to thrombolysis; therefore, the decision was made to attempt coronary thrombolysis with tenecteplase.
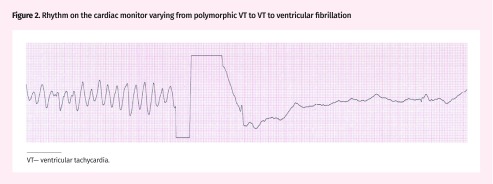
Approximately 7 minutes after receiving tenecteplase the patient became unresponsive, with no pulse, and polymorphic ventricular tachycardia (VT) was identified on the cardiac monitor. Chest compressions were immediately started and the patient was defibrillated 1 minute after cardiac arrest with 200 J. Table 1 provides a summary of the resuscitation, including likely episodes of consciousness. The patient had return of spontaneous circulation (ROSC) at 8 minutes but this was not sustained. The rhythm on the cardiac monitor varied from polymorphic VT to ventricular fibrillation to VT (Figure 2). The patient was ultimately defibrillated 6 times and received 3 mg of epinephrine, 2 g of magnesium sulfate (for suspected torsades de pointes), and 300 mg of amiodarone.
At several points during the resuscitation the patient regained some consciousness. He made purposeful movements to push CPR providers away and verbalized with defibrillations. When signs of consciousness were recognized, CPR was immediately stopped and pulse checks were performed. During pulse checks there was no palpable pulse and the patient lost consciousness shortly after cessation of CPR. The decision was therefore made to continue CPR and defibrillation attempts, and a 4-point restraint was applied to prevent interruptions to CPR. Return of spontaneous circulation was ultimately reobtained 17 minutes after the patient initially went into cardiac arrest. He eventually became fully conscious and was able to speak with family members before being intubated in preparation for transfer to a tertiary care facility. The patient was transferred, received rescue percutaneous coronary intervention for acute occlusion of the circumflex branch of the left coronary artery, and was ultimately discharged from hospital 4 days after cardiac arrest. He had complete neurologic recovery at the time of discharge. When interviewed 3 months later about his recollection of his resuscitation, he recalled experiencing discomfort in his chest and neck, and that he felt 2 “shocks” that made his muscles tense. He had no recollection of CPR specifically and denied any recollection of pain.
Although the patient’s outcome in this case was positive, several care providers who participated in this patient’s resuscitation reported feeling personal distress during the resuscitation. None of the care providers had ever experienced a patient regaining consciousness with CPR, nor were they aware that it was possible. They were therefore uncertain whether the case had been appropriately managed and whether the patient should have been sedated rather than restrained.
Figure 1.
A 12-lead electrocardiogram showing an inferior ST-segment elevation myocardial infarction
Table 1.
Summary of cardiac arrest events and actions
| TIME ELAPSED, MIN | RESUSCITATION EVENTS AND ACTIONS |
|---|---|
| 0 | Patient becomes unresponsive and exhibits decorticate rigidity |
| Pulseless polymorphic VT | |
| CPR started | |
| 1 | First defibrillation with 200 J |
| 3 | Pulseless VF |
| Second defibrillation with 200 J | |
| 4 | 1 mg of IV epinephrine administered (dose 1) |
| 5 | Pulseless polymorphic VT |
| Third defibrillation with 200 J | |
| 7 | 1 mg of IV epinephrine administered (dose 2) |
| 8 | ROSC with return of consciousness (spontaneous movements) |
| CPR stopped | |
| 9 | Loss of consciousness |
| Re-arrest with pulseless polymorphic VT | |
| CPR resumed | |
| Patient makes purposeful movements against CPR provider | |
| 10 | CPR stopped |
| Patient loses consciousness | |
| Pulseless polymorphic VT | |
| Fourth defibrillation with 200 J | |
| Patient cries out with defibrillation | |
| CPR resumed immediately | |
| 11 | Patient makes purposeful movements against CPR provider |
| CPR stopped | |
| Pulseless VF with no consciousness | |
| CPR resumed | |
| 12 | Pulseless VF with no consciousness |
| Fifth defibrillation with 200 J | |
| CPR resumed immediately | |
| Patient makes purposeful movements against CPR providers | |
| No palpable pulse | |
| CPR resumed | |
| 4-point restraint applied | |
| 13 | 2 g of IV magnesium sulfate administered |
| 14 | 300 mg of IV amiodarone administered |
| 15 | Pulseless VT |
| Sixth defibrillation with 200 J | |
| 16 | 1 mg of IV epinephrine administered (dose 3) |
| 17 | ROSC |
CPR—cardiopulmonary resuscitation, IV—intravenous, ROSC—return of spontaneous circulation, VF—ventricular fibrillation, VT—ventricular tachycardia.
Figure 2.
Rhythm on the cardiac monitor varying from polymorphic VT to VT to ventricular fibrillation
VT—ventricular tachycardia.
Discussion
A 2015 systematic review of case reports of CPRIC by Olaussen et al identified 10 cases of CPRIC in the literature.1 Reported levels of consciousness included eye opening, agonal breathing, localizing painful stimuli, purposeful arm movements, verbal and nonverbal communication with the resuscitation team, and following instructions. This systematic review also found that in half of the identified cases patients were alert enough to interfere with the resuscitation by “pushing and grabbing the rescuer, withdrawing from the compressions, and pulling on endotracheal tubes and mechanical devices.”1 Patient consciousness also led to CPR being interrupted more frequently for pulse checks. Several care providers commented on their uncertainty about how to appropriately manage CPRIC.1,4–6 Management strategies included sedation, physical restraint, instructions to the patient, and reassurance. Medications that have been used for sedation in CPRIC include ketamine, midazolam, propofol, etomidate, and fentanyl.1,4,6,7 Of note, a prospective study of awareness in CPR found that only 2% of patients recalled visual or auditory awareness of their resuscitation and no patients remembered experiencing pain.8
An observational study of CPRIC in 112 patients with out-of-hospital cardiac arrest in Australia provides some guidance on how to best manage CPRIC.7 In this study, the frequency of CPRIC in all cardiac arrests increased from 0.3% in 2008 to 0.9% in 2014. Patients who experienced CPRIC were more likely to be younger, male, have an initial rhythm of ventricular fibrillation or VT, and have a shorter interval between cardiac arrest and provision of emergency medical services care. The most common manifestations of CPRIC in this study were body movement (87.5%), speech (29.5%), eye opening (20.5%), jaw tone (20.5%), and being combative (19.6%). The study described 2 clinically relevant associations with CPRIC and survival, although both must be taken in the context of small sample size and retrospective analysis. First, CPRIC was independently associated with ROSC and survival to hospital discharge. Additionally, patients with CPRIC who were administered opiates, benzodiazepines, or muscle relaxants took longer to obtain ROSC and were less likely to survive to discharge. The use of ketamine and other dissociative agents was not described in this study; however, ketamine might be safer than other medications in CPRIC owing to its lower risk of inducing hypotension.4,6,7
Conclusion
Cardiopulmonary resuscitation–induced consciousness is a newly identified phenomenon of increasing incidence and might be related to early high-quality CPR in younger, healthier patients.5 Care providers should be aware that CPRIC can occur and that although it can be distressing to care providers, CPRIC is associated with improved survival. Once identified, the priority in the management of CPRIC should be the continuation of high-quality CPR with minimal interruptions. Physical restraints and patient reassurance might be required to minimize interruptions to CPR and continue effective resuscitation, as was done in this case. Few survivors have any recollection of their resuscitation. If needed, ketamine might also be used to sedate the patient to minimize CPR interruption, but further research is needed to confirm its safety and appropriate dosing in CPRIC.4 Hypotension-inducing medications should be avoided. Further research is required to determine the frequency of CPRIC in Canada and to develop guidelines on how to best manage this condition.
Editor’s key points
▸ Advanced cardiac life support providers should be aware that cardiopulmonary resuscitation–induced consciousness (CPRIC) can occur and is being reported with increasing frequency.
▸ Although it can be distressing to the care providers, few survivors of cardiac arrest with CPRIC have any recollection of their resuscitation. In fact, CPRIC is associated with positive patient outcomes.
▸ Physical restraints and patient reassurance might be required to minimize interruptions to CPR in patients with CPRIC. Medications for sedation can also be administered, but those that can induce hypotension should be avoided.
Points de repère du rédacteur
▸ Les prestataires de soins spécialisés de réanimation cardiorespiratoire (RCR) devraient être au fait de la possibilité qu’une reprise de conscience provoquée par la réanimation cardiorespiratoire (RCRCR) puisse survenir, et que de telles situations sont de plus en plus souvent signalées.
▸ Même si ce phénomène peut être bouleversant pour les prestataires de soins, il y a lieu de mentionner que peu de survivants à un arrêt cardiaque ayant repris connaissance durant la RCR se souviennent de leur réanimation. En réalité, la RCRCR est associée à des résultats favorables chez les patients.
▸ Il peut être nécessaire de recourir à des mesures de contention physique et de rassurer le patient pour minimiser les interruptions de la RCR chez les patients qui reprennent connaissance. Des sédatifs peuvent aussi être administrés, mais il faut éviter ceux qui peuvent induire une hypotension.
Footnotes
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Olaussen A, Shepherd M, Nehme Z, Smith K, Bernard S, Mitra B. Return of consciousness during ongoing cardiopulmonary resuscitation: a systematic review. Resuscitation. 2015;86(1):44–8. doi: 10.1016/j.resuscitation.2014.10.017. Epub 2014 Nov 4. [DOI] [PubMed] [Google Scholar]
- 2.Jespersen SN, Østergaard L. The roles of cerebral blood flow, capillary transit time heterogeneity, and oxygen tension in brain oxygenation and metabolism. J Cereb Blood Flow Metab. 2012;32(2):264–77. doi: 10.1038/jcbfm.2011.153. Epub 2011 Nov 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bandera E, Botteri M, Minelli C, Sutton A, Abrams KR, Latronico N. Cerebral blood flow threshold of ischemic penumbra and infarct core in acute ischemic stroke: a systematic review. Stroke. 2006;37(5):1334–9. doi: 10.1161/01.STR.0000217418.29609.22. Epub 2006 Mar 30. [DOI] [PubMed] [Google Scholar]
- 4.Pound J, Verbeek PR, Cheskes S. CPR induced consciousness during out-of-hospital cardiac arrest: a case report on an emerging phenomenon. Prehosp Emerg Care. 2017;21(2):252–6. doi: 10.1080/10903127.2016.1229823. Epub 2016 Oct 28. [DOI] [PubMed] [Google Scholar]
- 5.Bihari S, Rajajee V. Prolonged retention of awareness during cardiopulmonary resuscitation for asystolic cardiac arrest. Neurocrit Care. 2008;9(3):382–6. doi: 10.1007/s12028-008-9099-2. [DOI] [PubMed] [Google Scholar]
- 6.Olaussen A, Shepherd M, Nehme Z, Smith K, Jennings PA, Bernard S, et al. CPR-induced consciousness: a cross-sectional study of healthcare practitioners’ experience. Australas Emerg Nurs J. 2016;19(4):186–90. doi: 10.1016/j.aenj.2016.07.002. Epub 2016 Jul 29. [DOI] [PubMed] [Google Scholar]
- 7.Olaussen A, Nehme Z, Shepherd M, Jennings PA, Bernard S, Mitra B, et al. Consciousness induced during cardiopulmonary resuscitation: an observational study. Resuscitation. 2017;113(4):44–50. doi: 10.1016/j.resuscitation.2017.01.018. Epub 2017 Feb 1. [DOI] [PubMed] [Google Scholar]
- 8.Parnia S, Spearpoint K, de Vos G, Fenwick P, Goldberg D, Yang J, et al. AWARE—AWAreness during REsuscitation—a prospective study. Resuscitation. 2014;85(12):1799–805. doi: 10.1016/j.resuscitation.2014.09.004. Epub 2014 Oct 7. [DOI] [PubMed] [Google Scholar]