Abstract
Objective
To provide family physicians with an evidence-based and practical approach to managing patients with tinnitus.
Sources of information
MEDLINE was searched for English-language tinnitus guidelines and reviews. All such articles published between 1980 and 2016 were reviewed, with most providing level II and III evidence.
Main message
Tinnitus affects more than 40% of Canadians at least once in their lifetimes, most commonly older adults. Tinnitus is the perception of sound without external stimulation. It can greatly affect a patient’s physical and psychological quality of life. Clinical history taking is directed at eliciting whether symptoms have a pulsatile or nonpulsatile quality, whether symptoms are unilateral or bilateral, and whether there is associated hearing loss. For tinnitus that is pulsatile or unilateral, referral to an otolaryngologist is recommended, as these qualities might be associated with more serious underlying conditions. Most patients with tinnitus can be managed with reassurance, conservative measures, and hearing aids if substantial hearing loss exists.
Conclusion
Family physicians play the primary role in managing patients with tinnitus and are well situated to address both the physiologic and the psychological manifestations. As tinnitus is very common, helping patients cope with the symptoms through conservative measures and reassurance can prove to have the best outcomes.
Tinnitus is the perception of sound in the absence of any external stimulus. Symptoms can be unilateral or bilateral, present with or without hearing loss, and resemble ringing, hissing, whistling, humming, buzzing, chirping, or clicking sounds. Tinnitus can be categorized qualitatively as nonpulsatile (typically subjective) or pulsatile (often objective). Subjective nonpulsatile tinnitus is the most common and is only heard by the patient, whereas objective pulsatile tinnitus can sometimes be heard by an observer and is caused by an internal bodily vibration or noise.1 In Canada, 41% of those aged 3 to 79 years will experience tinnitus at least once in their lifetimes.2 Higher 1-year prevalence is associated with increased age (peaking between ages 60 and 69), body mass index of 30 kg/m2 or greater, smoking (former and current), diabetes mellitus, and hypertension.3 Moreover, tinnitus-related disability claims are among the largest submitted to Veterans Affairs Canada and the Workplace Safety and Insurance Board. Specific compensation guidelines exist for both Veterans Affairs Canada and the Workplace Safety and Insurance Board and require a tinnitus diagnosis to be made by an audiologist or otolaryngologist.4–6
Case description
Mr A. is a 67-year-old retired police officer who presents with concerns about ringing in his ears for the past 2 months. He describes the sound as constant and high-pitched ringing that is nonpulsatile in nature. He has no associated ear pain, but does report progressively decreasing hearing in both ears. Additionally, Mr A. has reported that this ringing has substantially affected his quality of life (QoL), mood, and sleep.
It sounds like Mr A. is suffering from tinnitus. But what are the indications for testing? How is tinnitus diagnosed? Are new treatments available? We aim to answer these questions and provide an approach to tinnitus for Canadian family physicians.
Sources of information
A literature search was performed within MEDLINE for English-language tinnitus guidelines and reviews. All such articles published between 1980 and 2016 were reviewed. Most of the cited studies provided level II and III evidence.
Main message
Expected outcome.
Tinnitus can affect both physical and psychological well-being, with 1 in 5 patients reporting bothersome tinnitus with decreased sleep, concentration, or mood.2 Increasing tinnitus severity is inversely associated with QoL.7 For most patients with chronic tinnitus (symptoms for > 6 months) there is no cure, as the symptoms are the result of hearing loss (typically related to age or noise exposure).8,9 Over time, the severity of tinnitus might fluctuate. Worsening symptoms were reported in 14% of patients after 5 years, while 18% noted improvements.10 Complete resolution of tinnitus was seen in 16% of patients.10 Factors that affect the expected outcome and QoL in patients with tinnitus include mood disorders such as anxiety and depression.11 The need for increasing masking sounds in the management of tinnitus is also associated with long-term distress.12
Symptoms and causes.
Although tinnitus is often considered idiopathic, the most likely causes can be determined from the case history and patient symptoms. Age-related hearing loss (presbyacusis) and noise exposure remain the most common causes.
Nonpulsatile tinnitus: Nonpulsatile tinnitus can have a unilateral or bilateral presentation. When tinnitus occurs unilaterally, it might result from cerumen impaction, tympanic membrane perforation, chronic otitis media, otosclerosis, or cholesteatomas, all of which can cause conductive hearing loss.13 Unilateral tinnitus might also result from chronic noise exposure, acoustic trauma, semicircular canal dehiscence, or Ménière disease, most of which cause sensorineural hearing loss (SNHL).14–16 Finally, unilateral tinnitus might have a more complex cause when exhibited together with neurologic symptoms, vertigo, or hearing loss. These causes include multiple sclerosis, cerebellopontine angle tumours, and brainstem infarctions.17
Bilateral tinnitus is most commonly caused by age-related hearing loss, noise exposure, acoustic trauma, or otosclerosis.1,17 Individuals who are taking or who have taken ototoxic medications, including high-dose acetylsalicylic acid, nonsteroidal anti-inflammatory drugs, aminoglycoside antibiotics (eg, gentamicin), loop diuretics (eg, furosemide), and chemotherapeutics (eg, cisplatin, valproic acid, quinine), might also experience bilateral tinnitus.8,18,19 Moreover, poor sleep and excessive use of caffeine or alcohol can aggravate the severity of tinnitus.8
Pulsatile tinnitus: Pulsatile tinnitus can be categorized as either pulse synchronous, where the rhythm of the noise or click is synchronous with the heartbeat (detected at the radial pulse), or pulse asynchronous.20,21 Pulse-synchronous tinnitus might have an underlying vascular cause. The most common is idiopathic intracranial hypertension, caused by elevated intracranial pressure that transfers pulsations through the cerebrospinal fluid.20,22 Vibrations are transferred to fluid in the cochlea causing tinnitus.20,22 Arterial bruits and venous hums can also present as pulse-synchronous tinnitus, with an associated “whooshing” sound caused by the turbulent flow of blood in vessels near the cochlea.23 Moreover, systemic hypertension, arteriovenous malformation, aneurysms, and vascular ear tumours such as paragangliomas (eg, glomus tympanicum and glomus jugulare) can present with pulse-synchronous tinnitus.23
Pulse-asynchronous tinnitus usually has an associated mechanical cause. These are often pulsatile noises owing to spasm or myoclonus of muscles within the middle ear, including the tensor tympani and stapedius muscles.21 The rapid contraction of the palatal muscles and the eustachian tube might also produce a rapid pulsatile clicking sound.14,24
Diagnosis
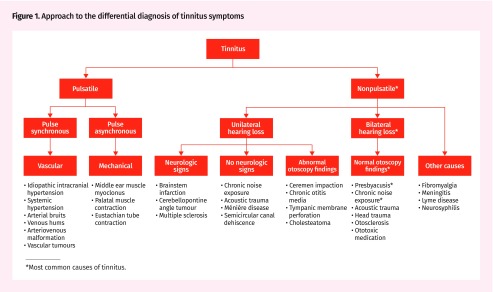
History: The patient’s clinical history guides the differential diagnosis (Figure 1). Key areas of inquiry include past history of acoustic trauma, occupational noise exposure, or ototoxic medication use. Tinnitus can be unilateral or bilateral, low pitched (buzzing or humming) or high pitched (ringing or hissing), and pulsatile (pulse synchronous or pulse asynchronous) or nonpulsatile. The clinician can determine if the tinnitus is bothersome or nonbothersome (ie, the patient is aware of the tinnitus, but it does not affect his or her daily activity or functioning). Related symptoms, such as hearing loss and vertigo, are sought in addition to focal neurologic symptoms.
Figure 1.
Approach to the differential diagnosis of tinnitus symptoms
*Most common causes of tinnitus.
Physical examination: Physical examination can be directed based on the working differential diagnosis, but is typically limited to cranial nerve examination and otoscopy, looking for signs of infection, eardrum perforation, or middle ear tumours. Auscultation for bruits is performed over the neck, mastoid, and preauricular areas for patients with pulsatile tinnitus.
Audiologic testing: All patients with tinnitus should be referred to an audiologist to undergo an audiologic evaluation to help determine auditory function and the presence of any hearing loss.19,25 An audiologist can also quantify the tinnitus perceived by the patient through dedicated tinnitus testing. Specifically, 4 parameters are measured, including pitch, loudness, maskability, and residual inhibition.26
Laboratory testing and imaging: Laboratory testing in tinnitus is typically not indicated. For most patients who present with bilateral nonpulsatile symptoms, we recommend against routine imaging. For patients with pulsatile tinnitus, a magnetic resonance angiogram and venogram of the brain and neck is the most useful test to rule out vascular abnormalities. For patients with nonpulsatile unilateral tinnitus and normal otoscopy findings, or asymmetrical SNHL, a referral to an otolaryngologist or screening noncontrast magnetic resonance imaging of the internal auditory canals is recommended.27
Referral to an otolaryngologist: When tinnitus is pulsatile or unilateral in nature, or abnormal otoscopy findings are noted, referral to an otolaryngologist is recommended to rule out underlying conditions.1,17 Imaging can be ordered in advance of the referral, if appropriate.
Management
Primary and secondary prevention: Most cases of tinnitus are caused by SNHL. As SNHL cannot be reversed, primary prevention is vital. High-volume music through headphones from portable listening devices, including smartphones, has a substantial damaging effect on the auditory system.28 Similar to the perceived effects of smoking, which are distant and intangible, so too are the adverse effects of noise exposure. As noise damage is related to the intensity and duration of exposure, the 80-to-90 rule (volume 80% of maximum, listen for < 90 minutes a day) is recommended to prevent noise damage.29 Using occlusive headphones can also decrease external noise and lessen the intensity of sound delivered.29 To prevent noise damage in the workplace, employers must be aware of occupational exposure limits, employ regular audiometry evaluations, and provide appropriate hearing protection.30
Dietary factors, including increased glycemic load and hypercholesterolemia, are associated with increased risk of age-related hearing loss.31 Dietary changes to reduce carbohydrate and cholesterol intake might prevent or delay the onset of SNHL.31
Conservative management: For persistent and bothersome tinnitus, conservative management options can first be tried to relieve symptoms and improve QoL. These include lifestyle changes to improve sleep, reduce stress, and reduce caffeine and alcohol consumption.8
Sound amplification: Some individuals with tinnitus find relief from hearing aids, which act as a masker by introducing more ambient noise. For those patients for whom basic amplification is not sufficient, specialized tinnitus maskers, including adjustable nature sounds or broadband noise, can be used to provide additional tinnitus relief.19 Additionally, the use of white-noise generators has been shown to be beneficial in decreasing the severity of tinnitus and improving sleep.32,33 Other types of background noise (eg, a fan, music) at bedtime can also be helpful.
Pharmacologic therapy: Some pharmacologic therapies can be beneficial when given in combination with conservative management. Exogenous melatonin has been shown to improve tinnitus symptoms, and particularly improves sleep.34 Current tinnitus guidelines recommend against the routine use of antidepressant, anticonvulsant, or anxiolytic medication for bothersome tinnitus.19 However, for patients with pre-existing anxiety and depression, the use of tricyclic antidepressants and selective serotonin reuptake inhibitors has been shown to be effective in managing tinnitus symptoms, decreasing the level of annoyance.35,36
Rehabilitation therapies: Tinnitus retraining therapy helps to dissociate tinnitus from a patient’s negative response by using a combination of directive counseling and ear-level noise generators. Tinnitus retraining therapy is a time-intensive therapy designed to help patients understand and habituate to tinnitus.37 This therapy is notably different from sound therapy because of directive counseling.
Cognitive-behavioural therapy aims to eliminate the perception of sound and correct one’s negative responses to tinnitus, focusing primarily on counseling and relaxation techniques.38 Cognitive-behavioural therapy has been shown to improve QoL and decrease depression in sufferers, and is currently recommended for persistent and bothersome tinnitus.19,38
Magnetic stimulation: Transcranial magnetic stimulation has been proposed as an innovative and noninvasive treatment for chronic bothersome tinnitus; it is currently only available in research trials. The current model of tinnitus centres on the overstimulation of the subcortical auditory pathway, and it has been suggested that low-frequency electromagnetic pulses from transcranial magnetic stimulation help reduce the neural activity in the directly stimulated and structurally connected regions of the patient’s brain.39–42
Surgical management: Surgical management is very rarely used in patients with tinnitus, and is only used for treatable underlying causes.43,44 These can include the surgical resection of acoustic neuroma or other brainstem or cerebellopontine angle tumours and lesions, endolymphatic sac shunting for Ménière disease, or stapedectomy for otosclerosis. Tensor tympani and stapedius myoclonus syndromes are also correctable with surgery by sectioning the affected muscles.45
Case resolution
The bilateral, high-pitched, nonpulsatile characteristics of tinnitus that Mr A. is experiencing are consistent with SNHL. Taking into account Mr A.’s age, reported decrease in hearing, and previous occupation (as a police officer with the associated substantial amount of noise exposure), the most likely possible causes include presbyacusis, acoustic trauma, and noise exposure.
Otoscopic examination reveals no signs of infection or middle ear masses, and bilaterally intact tympanic membranes. Findings of a neurologic examination were unremarkable and did not show focal neurologic deficits. An audiogram reveals symmetric, high-frequency SNHL, with normal speech discrimination. Based on the findings of the physical examination and audiologic investigation, Mr A.’s tinnitus is most likely caused by a combination of presbyacusis and noise exposure or acoustic trauma.
Conservative management strategies are tried first, including dietary changes, hearing protection in noisy environments, and white-noise generators, with the goal of improving QoL. Mr A. is referred for tinnitus retraining therapy. Cognitive-behavioural therapy is planned if the tinnitus continues to be bothersome after an adequate trial of conservative measures.
Mr A. returns to the clinic 2 months later. Although he is still aware of his tinnitus, it is no longer bothersome. He has returned to regular activities and finds his mood and sleep have improved. He is asked to continue with the conservative management.
Conclusion
Most patients with tinnitus can be managed conservatively by family physicians. Red flags for referral to another specialist include pulsatile or unilateral tinnitus, and abnormal findings on otoscopy. Family physicians are well situated to address both the physiologic and the psychological burdens experienced by patients with tinnitus. As most cases of tinnitus cannot be cured, helping patients cope with the symptoms through conservative measures and reassurance can prove to have the best results.
Editor’s key points
▸ Family physicians are well situated to address both the physiologic and the psychological burdens experienced by patients with tinnitus. Most patients with tinnitus can be managed conservatively by family physicians. Red flags for referral to another specialist include pulsatile or unilateral tinnitus, and abnormal findings on otoscopy.
▸ As most tinnitus cannot be cured, helping patients cope with the symptoms through conservative measures and reassurance can have the best results. These measures include lifestyle changes to improve sleep, reduce stress, and reduce caffeine and alcohol consumption.
▸ Some individuals with tinnitus find relief from hearing aids, which act as a masker by introducing more ambient noise. For persistent and bothersome tinnitus, cognitive-behavioural therapy has been shown to improve quality of life and decrease depression.
Footnotes
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de juillet 2018 à la page e293.
References
- 1.Schleuning AJ., 2nd Management of the patient with tinnitus. Med Clin North Am. 1991;75(6):1225–37. doi: 10.1016/s0025-7125(16)30383-2. [DOI] [PubMed] [Google Scholar]
- 2.Statistics Canada [website]. Hearing loss of Canadians, 2012 and 2013. Ottawa, ON: Statistics Canada; 2015. Available from: www.statcan.gc.ca/pub/82-625-x/2015001/article/14156-eng.htm. Accessed 2016 Aug 27. [Google Scholar]
- 3.Shargorodsky J, Curhan GC, Farwell WR. Prevalence and characteristics of tinnitus among US adults. Am J Med. 2010;123(8):711–8. doi: 10.1016/j.amjmed.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 4.Workplace Safety and Insurance Board Ontario [website]. Tinnitus. Toronto, ON: Workplace Safety and Insurance Board; 2004. Available from: www.wsib.on.ca/WSIBPortal/faces/WSIBManualPage?cGUID=16-01-08&fGUID=835502100635000503. Accessed 2016 Aug 31. [Google Scholar]
- 5.Building Trades BC. Permanent disability awards for tinnitus. BC Building Trades position. Burnaby, BC: British Columbia and Yukon Territory Building and Construction Trades Council; 2011. Available from: www.bcbuildingtrades.org/files/WCB_Sub-Tinnitus.pdf. Accessed 2016 Aug 31. [Google Scholar]
- 6.Veterans Affairs Canada [website]. Tinnitus. Ottawa, ON: Veterans Affairs Canada; 2014. Available from: www.veterans.gc.ca/eng/services/after-injury/disability-benefits/benefits-determined/entitlement-eligibility-guidelines/tinnitus. Accessed 2016 Aug 31. [Google Scholar]
- 7.Nondahl DM, Cruickshanks KJ, Dalton DS, Klein BE, Klein R, Schubert CR, et al. The impact of tinnitus on quality of life in older adults. J Am Acad Audiol. 2007;18(3):257–66. doi: 10.3766/jaaa.18.3.7. [DOI] [PubMed] [Google Scholar]
- 8.Folmer RL, Martin WH, Shi Y. Tinnitus: questions to reveal the cause, answers to provide relief. J Fam Pract. 2004;53(7):532–40. [PubMed] [Google Scholar]
- 9.Piccirillo JF, Finnell J, Vlahiotis A, Chole RA, Spitznagel E., Jr Relief of idiopathic subjective tinnitus: is gabapentin effective? Arch Otolaryngol Head Neck Surg. 2007;133(4):390–7. doi: 10.1001/archotol.133.4.390. [DOI] [PubMed] [Google Scholar]
- 10.Gopinath B, McMahon CM, Rochtchina E, Karpa MJ, Mitchell P. Incidence, persistence, and progression of tinnitus symptoms in older adults: the Blue Mountains Hearing Study. Ear Hear. 2010;31(3):407–12. doi: 10.1097/AUD.0b013e3181cdb2a2. [DOI] [PubMed] [Google Scholar]
- 11.Bhatt JM, Bhattacharyya N, Lin HW. Relationships between tinnitus and the prevalence of anxiety and depression. Laryngoscope. 2017;127(2):466–9. doi: 10.1002/lary.26107. Epub 2016 Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersson G, Vretblad P, Larsen HC, Lyttkens L. Longitudinal follow-up of tinnitus complaints. Arch Otolaryngol Head Neck Surg. 2001;127(2):175–9. doi: 10.1001/archotol.127.2.175. [DOI] [PubMed] [Google Scholar]
- 13.Kim DK, Park SN, Kim MJ, Lee SY, Park KH, Yeo SW. Tinnitus in patients with chronic otitis media before and after middle ear surgery. Eur Arch Otorhinolaryngol. 2011;268(10):1443–8. doi: 10.1007/s00405-011-1519-9. Epub 2011 Feb 18. [DOI] [PubMed] [Google Scholar]
- 14.Vernon J, Johnson R, Schleuning A. The characteristics and natural history of tinnitus in Meniere’s disease. Otolaryngol Clin North Am. 1980;13(4):611–9. [PubMed] [Google Scholar]
- 15.Nam EC, Lewis R, Nakajima HH, Merchant SN, Levine RA. Head rotation evoked tinnitus due to superior semicircular canal dehiscence. J Laryngol Otol. 2010;124(3):333–5. doi: 10.1017/S0022215109991241. Epub 2009 Sep 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Gompel JJ, Patel J, Danner C, Zhang AN, Samy Youssef AA, van Loveren HR, et al. Acoustic neuroma observation associated with an increase in symptomatic tinnitus: results of the 2007–2008 Acoustic Neuroma Association survey. J Neurosurg. 2013;119(4):864–8. doi: 10.3171/2013.5.JNS122301. Epub 2013 Jun 21. [DOI] [PubMed] [Google Scholar]
- 17.Crummer RW, Hassan GA. Diagnostic approach to tinnitus. Am Fam Physician. 2004;69(1):120–6. [PubMed] [Google Scholar]
- 18.Chen GD, Stolzberg D, Lobarinas E, Sun W, Ding D, Salvi R. Salicylate-induced cochlear impairments, cortical hyperactivity and re-tuning, and tinnitus. Hear Res. 2013;295:100–13. doi: 10.1016/j.heares.2012.11.016. Epub 2012 Nov 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tunkel DE, Bauer CA, Sun GH, Rosenfeld RM, Chandrasekhar SS, Cunningham ER, Jr, et al. Clinical practice guideline: tinnitus. Otolaryngol Head Neck Surg. 2014;151(2 Suppl):S1–40. doi: 10.1177/0194599814545325. [DOI] [PubMed] [Google Scholar]
- 20.Wall M. Idiopathic intracranial hypertension. Neurol Clin. 2010;28(3):593–617. doi: 10.1016/j.ncl.2010.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park SN, Bae SC, Lee GH, Song JN, Park KH, Jeon EJ, et al. Clinical characteristics and therapeutic response of objective tinnitus due to middle ear myoclonus: a large case series. Laryngoscope. 2013;123(10):2516–20. doi: 10.1002/lary.23854. Epub 2013 Aug 5. [DOI] [PubMed] [Google Scholar]
- 22.Böhmer A. Hydrostatic pressure in the inner ear fluid compartments and its effects on inner ear function. Acta Otolaryngol Suppl. 1993;507:3–24. [PubMed] [Google Scholar]
- 23.Hofmann E, Behr R, Neumann-Haefelin T, Schwager K. Pulsatile tinnitus: imaging and differential diagnosis. Dtsch Arztebl Int. 2013;110(26):451–8. doi: 10.3238/arztebl.2013.0451. Epub 2013 Jun 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fortune DS, Haynes DS, Hall JW., 3rd Tinnitus: current evaluation and management. Med Clin North Am. 1999;83(1):153–62. x. doi: 10.1016/s0025-7125(05)70094-8. [DOI] [PubMed] [Google Scholar]
- 25.Henry JA, Zaugg TL, Myers PJ, Kendall CJ. Progressive tinnitus management. Clinical handbook for audiologists. San Diego, CA: Plural Publishing Inc; 2010. [Google Scholar]
- 26.Henry JA, Meikle MB. Psychoacoustic measures of tinnitus. J Am Acad Audiol. 2000;11(3):138–55. [PubMed] [Google Scholar]
- 27.Fortnum H, O’Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al. The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost effectiveness and natural history. Health Technol Assess. 2009;13(18):iii–iv. ix–xi, 1–154. doi: 10.3310/hta13180. [DOI] [PubMed] [Google Scholar]
- 28.Portnuff CD. Reducing the risk of music-induced hearing loss from overuse of portable listening devices: understanding the problems and establishing strategies for improving awareness in adolescents. Adolesc Health Med Ther. 2016;7:27–35. doi: 10.2147/AHMT.S74103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Portnuff CD, Fligor BJ, Arehart KH. Teenage use of portable listening devices: a hazard to hearing? J Am Acad Audiol. 2011;22(10):663–77. doi: 10.3766/jaaa.22.10.5. [DOI] [PubMed] [Google Scholar]
- 30.Canadian Centre for Occupational Health and Safety [website]. Noise – occupational exposure limits in Canada. Hamilton, ON: Canadian Centre for Occupational Health and Safety; 2017. Available from: www.ccohs.ca/oshanswers/phys_agents/exposure_can.html. Accessed 2017 Jan 15. [Google Scholar]
- 31.Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol. 2009;30(2):139–45. doi: 10.1097/MAO.0b013e318192483c. [DOI] [PubMed] [Google Scholar]
- 32.Sandlin RE, Olsson RJ. Evaluation and selection of maskers and other devices used in the treatment of tinnitus and hyperacusis. Trends Amplif. 1999;4(1):6–26. doi: 10.1177/108471389900400102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hazell JW, Wood S. Tinnitus masking—a significant contribution to tinnitus management. Br J Audiol. 1981;15(4):223–30. doi: 10.3109/03005368109081442. [DOI] [PubMed] [Google Scholar]
- 34.Megwalu UC, Finnell JE, Piccirillo JF. The effects of melatonin on tinnitus and sleep. Otolaryngol Head Neck Surg. 2006;134(2):210–3. doi: 10.1016/j.otohns.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 35.Robinson S. Antidepressants for treatment of tinnitus. Prog Brain Res. 2007;166:263–71. doi: 10.1016/S0079-6123(07)66024-5. [DOI] [PubMed] [Google Scholar]
- 36.Fornaro M, Martino M. Tinnitus psychopharmacology: a comprehensive review of its pathomechanisms and management. Neuropsychiatr Dis Treat. 2010;6:209–18. doi: 10.2147/ndt.s10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gelfand SA. Audiological management II. In: Gelfand SA, editor. Essentials of audiology. 3rd ed. New York, NY: Thieme Medical Publishers; 2009. pp. 444–86. [Google Scholar]
- 38.Jun HJ, Park MK. Cognitive behavioral therapy for tinnitus: evidence and efficacy. Korean J Audiol. 2013;17(3):101–4. doi: 10.7874/kja.2013.17.3.101. Epub 2013 Dec 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen R, Classen J, Gerloff C, Celnik P, Wassermann EM, Hallett M, et al. Depression of motor cortex excitability by low-frequency transcranial magnetic stimulation. Neurology. 1997;48(5):1398–403. doi: 10.1212/wnl.48.5.1398. [DOI] [PubMed] [Google Scholar]
- 40.Siebner HR, Filipovic SR, Rowe JB, Cordivari C, Gerschlager W, Rothwell JC, et al. Patients with focal arm dystonia have increased sensitivity to slow-frequency repetitive TMS of the dorsal premotor cortex. Brain. 2003;126(Pt 12):2710–25. doi: 10.1093/brain/awg282. Epub 2003 Aug 22. [DOI] [PubMed] [Google Scholar]
- 41.May A, Hajak G, Gänssbauer S, Steffens T, Langguth B, Kleinjung T, et al. Structural brain alterations following 5 days of intervention: dynamic aspects of neuroplasticity. Cereb Cortex. 2007;17(1):205–10. doi: 10.1093/cercor/bhj138. Epub 2006 Feb 15. [DOI] [PubMed] [Google Scholar]
- 42.Folmer RL, Theodoroff SM, Casiana L, Shi Y, Griest S, Vachhani J. Repetitive transcranial magnetic stimulation treatment for chronic tinnitus: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2015;141(8):716–22. doi: 10.1001/jamaoto.2015.1219. [DOI] [PubMed] [Google Scholar]
- 43.De Ridder D, Menovsky T, Van de Heyning P. An otoneurosurgical approach to nonpulsatile and pulsatile tinnitus. B-ENT. 2007;3(Suppl 7):79–86. [PubMed] [Google Scholar]
- 44.McFerran DJ, Phillips JS. Tinnitus. J Laryngol Otol. 2007;121(3):201–8. doi: 10.1017/S0022215106002714. Epub 2006 Sep 25. [DOI] [PubMed] [Google Scholar]
- 45.Bhimrao SK, Masterson L, Baguley D. Systematic review of management strategies for middle ear myoclonus. Otolaryngol Head Neck Surg. 2012;146(5):698–706. doi: 10.1177/0194599811434504. Epub 2012 Jan 18. [DOI] [PubMed] [Google Scholar]