Abstract
Robot-Assisted Therapy (RT) is an innovative approach to neurological rehabilitation that uses intensive, repetitive, interactive, and individualized practice. This systematic review aimed to investigate the effectiveness of RT on the body function and structure of people with upper limb impairments (PROSPERO registration: CRD42017054982). A search strategy conducted on seven databases identified randomized controlled studies. Methodological quality was assessed using the PEDro scale. When possible, the data were pooled, the strength of evidence was assessed using the GRADE system, and the effect sizes were assessed using Cohen coefficient. Subgroup analyses investigated the impact on the estimated effects of the following parameters: methodological quality; portion of the assessed upper limb; duration of stroke; and intervention dose and duration. Thirty-eight studies involving 1174 participants were included. Pooled estimates revealed small effects of RT on motor control and medium effects on strength compared with other intervention (OI) at a short-term follow-up. Standardized differences in means were as follows: 0.3 (95% CI 0.1 to 0.4) and 0.5 (95% CI 0.2 to 0.8). Effects at other time points and on other investigated outcomes related to body function and structure were not found (p>0.05). The strength of the current evidence was usually low quality. Subgroup analyses suggested that the methodological quality, and duration and dose of RT may influence the estimated effects. In conclusion, RT has small effects on motor control and medium effects on strength in people with limited upper limb function. Poor methodological quality, and lower treatment dose and duration may impact negatively the estimated effects.
Introduction
Upper limb motor impairments following a neurological disorder are common and may lead to function limitations, dependence and poor quality of life among the affected people[1]. There are many rehabilitation programs aiming to promote the function, independence and social reintegration of these affected people[2]. These programs include constraint-induced movement therapy, electromyographic biofeedback, mental practice with motor imagery, repetitive task training, functional electrical stimulation and Robot-Assisted Therapy (RT)[3,4,5].
RT is an innovative approach to neurological rehabilitation that involves intensive, repetitive, interactive, and individualized practice[6]. The use of RT for upper limb disorders dates to the 1990s. Since then, a number of robotic devices have become commercially available to clinics and hospitals worldwide[7].
Previous reviews have suggested that RT improves upper limb motor control and muscle strength[8,9,10,11,12]. However, these studies drew limited conclusions about the effectiveness of RT on the body function and structure of people with upper limb impairments. It was not possible to specify comparisons; the use of RT alone or combined with other interventions was compared with minimal or other interventions. Other limitations included few investigated outcomes related to body function and structure in individuals with stroke, absence of protocol registration and assessment of the strength of evidence[11], language restriction for the included studies, and absence of medium- and long-term effects[12].
It also remains unknown whether the estimated effects of RT are impacted by the portion of the assessed upper limb (i.e., proximal shoulder-elbow level or distal hand-wrist level)[9,10], treatment dose and/or duration[11,12], or the methodological quality of the studies. Therefore, the aim of this systematic review was to investigate the effectiveness of RT on outcomes related to body function and structure of people with upper limb impairments at short-, medium- and long-term follow-ups. The potential impacts of the portion of the assessed upper limb, duration of stroke, treatment dose and/or duration, and methodological quality were also investigated.
Methods
Search strategy and inclusion criteria
The protocol of this review was prospectively registered at PROSPERO (CRD42017054982). The search for relevant studies was conducted in PEDro (Physiotherapy Evidence Database), EMBASE (Excerpta Medica Database), Medline (Medical Literature Analysis and Retrieval System Online), CINAHL (Cumulative Index to Nursing and Allied Health Literature), Cochrane (Cochrane Collaboration), AMED (Allied and Complementary Medicine Database) and Compendex (Compendex Engineering Index) without language or date restrictions. In addition, a hand search was conducted in reference lists of previous reviews in this area. The search terms were related to “Robot-Assisted Therapy” (robotics, orthotic devices, bionic device, exoskeleton, robotic aided therapy, therapy computer-assisted, robot-assisted, robotics-assisted, self-help devices, robotic device, dynamic orthotic device, robot-mediated therapy, robot-supported, computer-assisted instruction, computer aided, computer-aided design, computer assisted, artificial limb, rehabilitation robotics, human-robot interaction, robot-aided rehabilitation, robotic rehabilitation, orthosis, taping, splinting, assistive technology devices, assistive device therapy), “upper limb” (upper extremity, arm, arm injuries, hand, hand injuries, shoulder, shoulder injuries, elbow, axilla elbow, forearm injuries, forearm, finger, finger injuries, wrist injuries, wrist) and “randomized controlled trial” (random allocation, double blind method, single blind method, placebo, random, controlled clinical trial, clinical trial, comparative study, evaluation study, follow-up study, prospective study, crossover studies). See S1 Appendix in the Addenda for the detailed search strategy.
This review included prospective randomized or quasi-randomized controlled studies including inpatients and outpatients from any primary, secondary or tertiary care setting and community. Studies were eligible if they included participants of both sexes, regardless of age, with limited upper limb function caused by stroke. The intervention of interest was RT, which was defined as the application of any electronic, computerized control system connected to mechanical devices designed to perform human functions. Studies were eligible if RT was compared with minimal intervention or other intervention (OI). We defined minimal intervention as when the control group received no intervention, received sham or placebo intervention, or was on a waiting list. We considered any other active intervention that was not robotic therapy, such as conventional therapy and physical therapy. Studies investigating additional effects of RT were also included. The outcomes of interest in this review were those related to body function and structure, according to the International Classification of Functioning, Disability and Health[13]. We considered body function as the physiological functions of body systems, including psychological function and body structure, i.e., anatomical parts of the body, such as organs, limbs and their components[14].
Selection of studies
After removing duplicate studies, the relevant retrieved titles and abstracts were selected. Then, we assessed the potential full texts, and studies fulfilling the eligibility criteria were included.
Methodological quality assessment
We assessed the methodological quality of the included studies using the 0 to 10 PEDro scale, with higher scores indicating greater methodological quality. Disagreements were resolved by consensus. When available, we used scores already on the PEDro database (http://www.pedro.org.au/).
Data extraction
We extracted data on the following characteristics of the included studies: number of participants; mean age; percentage of female; cause of the upper limb disorder and its duration; evaluated joints; type of RT; comparison groups; frequency and total duration of intervention; and outcome measures.
The included studies investigated many different outcomes related to body function and structure. For the feasibility of this review, we arbitrarily decided to include the following five most investigated outcomes in the literature: motor control; strength; spasticity; range of motion; and pain. When a given study evaluated these outcomes with more than one instrument, we considered the most consistent instrument among the included studies. When a given study investigated two different RT groups[15–27], we considered both groups, consistent with previous reviews in this area[12, 28]. We extracted data for the complete upper limb, and we separately considered the proximal (i.e., elbow and shoulder) and distal (i.e., wrist and hand) portions of the assessed upper limb, as suggested by previous reviews[9,10]. When more than one measurement was available for the proximal and/or distal upper limb, we considered the elbow and wrist due to their greater consistency among the included studies and clinical implications[29].
The following outcome data were included: sample size, mean and standard deviation (SD) for each group were extracted at the short-, medium- and long-term follow-ups: ≤ 3 months after baseline for short-term; > 3 months but < 12 months after baseline for medium-term; and ≥ 12 months after baseline for long-term. When multiple time points were available within the same follow-up period, the time point closer to the end of the intervention was used for short-term follow-up, that closer to 6 months was used for medium-term follow-up and that closer to 12 months was used for long-term follow-up. SDs were not available in certain included studies, and in those cases, the SDs were imputed from the 95% confidence interval (CI), standard error (SE), p value, interquartile range and average from other included studies with similar sources of participants. See S2 Appendix in the Addenda for the detailed extracted data.
Data analysis
Data for each outcome were pooled when there was sufficient homogeneity among studies. Homogeneity among studies was assessed using I2 statistics. Low heterogeneity was defined as if I2 ≤ 50%, and moderate to high heterogeneity was defined as I2 > 50%[30]. Pooled effects were estimated using standardized mean differences (SMDs) with 95% confidence intervals (CI). A fixed-effects model was used to conduct the meta-analysis when I2 ≤ 50%, and a random-effects model was used to conduct the meta-analysis when I2 > 50%. To judge the clinical relevance of RT, the effect size was assessed using Cohen’s d coefficient according to the following parameters:
0.2 as small effect, 0.5 as medium effect, and 0.8 as large effect [31]. A funnel plot was used to investigated publication bias when at least 10 studies were pooled[30]. The meta-analysis was performed using the software Comprehensive Meta-Analysis, version 3.3.070.
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) system was used to summarize the overall quality of evidence for each outcome[32]. We rated evidence from the high-quality level and downgraded it one point if one of the following pre-specified criteria was present: low methodological quality (average PEDro score < 6); inconsistency of estimates among pooled studies (I2 > 50%) or when its assessment was not possible (no pooling); indirectness of participants (over 50% of the studies did not describe inclusion criteria); and imprecision (pooling < 300 participants for each outcome)[33].
Subgroup analyses were used to investigated the impact of the following on estimated effects: 1) poor methodological quality (i.e., removing studies with score of five or less out of ten on PEDro scale); 2) investigated portion (proximal and distal portions of the upper limb); 3) duration of stroke (duration of the current episode ≤ 6 months and > 6 months); and 4) treatment dose and duration. For dose, analyses investigated whether the effects of studies providing the same amount of intervention differed from those providing different amounts of intervention for RT and control groups. For duration, analyses investigated whether the effects of studies providing > 20 sessions differed from those providing ≤ 20 sessions. The impact of dose and duration was also investigated using total volume (i.e., number of sessions x time per session in hours), dichotomized into studies with total volume > 20 hours of intervention and those ones with ≤ 20 hours. We arbitrarily decided on these cut-offs because they were the most frequently used cut-offs in the included studies. Subgroup analyses were conducted to compare RT and OI at the short-term follow-up because this was the most investigated follow-up.
Results
Flow of studies through the review
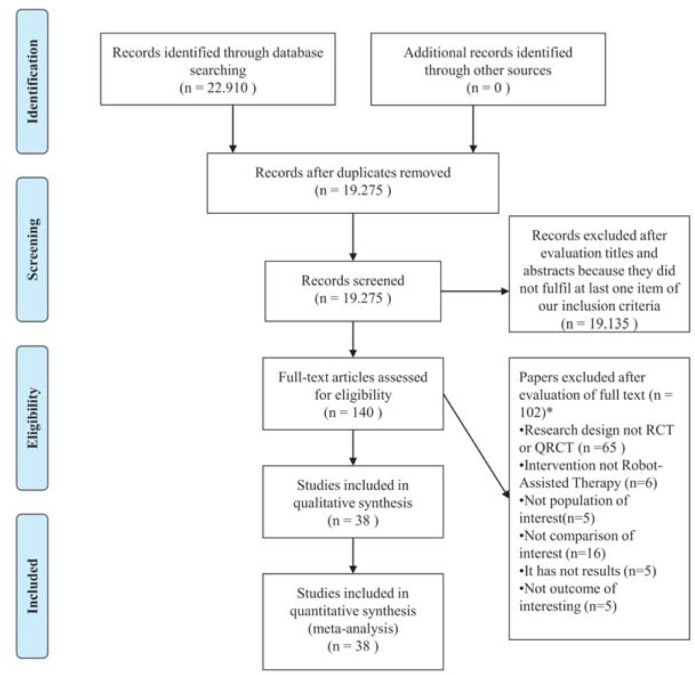
The searches retrieved 22910 references. After removing duplicates, 19275 titles and abstracts were screened. Of these, 19135 were excluded, and 140 potential full texts were assessed. The hand search did not retrieve additional studies. Finally, 38 original studies were included[15–27,34–57]. Fig 1 presents the flow of studies through the review.
Fig 1. Flow chart of studies through the review.
*Papers may have been excluded for failing to meet more than one inclusion criteria. Abbreviations: RCT = randomized controlled trials; QRCT = quasi-randomized controlled trials.
Characteristics of studies
The characteristics of the included studies are presented in Table 1. All included studies were prospective randomized controlled studies published in English between 1997 and 2015. The 38 original studies enrolled 1174 participants of both sexes, with a mean age ranging from 51.2 to 57.8 years. The cause of the upper limb disorder was stroke, with 24 of the 38 studies including people with chronic episodes of this health condition.
Table 1. Characteristics of the included studies (n = 38).
| Study | Health Condition | Source | Participants | Intervention | Duration and frequency | Outcome measures | Robotic Device |
|---|---|---|---|---|---|---|---|
| Abdullah et al. (2011) | Individuals with unilateral stroke, aged between 16–90 years, 2 to 8 weeks post stroke. | Recruited at Chedoke Stroke Rehabilitation Unit at Hamilton Health Sciences in Ontario. | n = 19 Age (yr) = N/A (SD = N/A) Gender = 8M / 11F |
Exp RT = robotic therapy (n = 8) OI = conventional therapy (n = 11) |
Exp RT = 45 min/session; 3/wk x 8-11wk OI = 45 min/session; 3/wk x 8–11 wk |
Motor control: Chedoke McMaster Stroke Assessment of the arm and hand range 1–7 Pain: Chedoke McMaster Stroke Assessment Pain Inventory Scale range 1–7 Follow-up = post-treatment |
Robotic System |
| Aisen et al. (1997) |
Individuals with a single stroke, 3 weeks post stroke. | Recruited at Burke Rehabilitation Hospital in New York. | n = 20 Age (yr) = N/A (SD = N/A) Gender = 11M / 9F |
Exp RT = robotic therapy + conventional therapy (n = 10) MI = sham robotic therapy + conventional therapy (n = 10) |
Exp RT = 60 min/session; 5/wk MI = had weekly to biweekly contact with the robotic device |
Motor control: Fugl-Meyer range 0–66 Strength: Motor power shoulder and elbow (in the biceps, triceps, and anterior and lateral deltoid muscles) range 0–20 Follow-up = post-treatment |
MIT- MANUS |
| Ang et al. (2014) |
Individuals with stroke for at least 4 months, aged between 21–80 years. | Recruited at Tan Tock Seng Hospital in Singapore. | n = 21 Age (yr) = 54.2 (SD = 12.4) Gender = 14M / 7F |
Exp RT = robotic therapy (n = 8) OI = standard arm therapy (n = 7) |
Exp RT = 90 min/session; 3/wk x 6 wk OI = 90 min/session; 3/wk x 6 wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment and 6, 8 weeks |
Haptic Knob (HK) |
| Brokaw et al. (2014) | Individuals with stroke for at least 6 months. | Recruited through the MedStar National Rehabilitation Hospital stroke database. | n = 10 Age (yr) = 57 (SD = 11.7) Gender = N/A |
Exp RT = robotic therapy (n = 7) OI = conventional therapy (n = 5) |
Exp RT = 12 h x 4 wk OI = 12 h x 4 wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment |
ARMin III and HandSOME device |
| Burgar et al. (2000) |
Individuals with chronic stroke at least 6 months. | Recruited and the informed consent was obtained in compliance with Veterans Affairs and Stanford University. | n = 21 Age (yr) = N/A (SD = N/A) Gender = 14M / 7F |
Exp RT = robotic therapy (n = 11) OI = conventional therapy (n = 10) |
Exp RT = 60 min/session; 3/wk x 8 wk OI = 60 min/session; 3/wk x 8 wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Follow-up = post-treatment |
Mirror Image Movement Enabler (MIME) |
| Burgar et al. (2011) |
Individuals with acute stroke | Recruited through the Veterans Affairs (VA) Medical Center (Texas), the VA Greater Los Angeles Healthcare System (California) and the VA Palo Alto Health Care System (California). | n = 54 Age (yr) = N/A (SD = N/A) Gender = N/A |
Exp RT = high dose robotic therapy (n = 17) Exp RT = low dose robotic therapy (n = 19) OI = conventional therapy (n = 18) |
Exp RT = 1 h/session x 30 sessions; 3 wk Exp RT = 1 h/session x 15 sessions; 3 wk OI = 1 h/session x 15 sessions; 3 wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 Strength: Motor Power range 0–70 Spasticity: Modified Ashworth Scale range 0–5 Follow-up = post-treatment and 24 weeks |
Mirror Image Movement Enabler (MIME) |
| Byl et al. (2013) | Individuals with unilateral stroke for at least 6 months, aged between 25–75 years. | Recruited at University of California in San Francisco. | n = 15 Age (yr) = N/A (SD = N/A) Gender = 13M / 2F |
Exp RT = unilateral robotic therapy (n = 5) Exp RT = bilateral robotic therapy (n = 5) OI = task specific repetitive training (n = 5) |
Exp RT = 90 min/session; 2/wk x 6 wk Exp RT = 90 min/session; 2/wk x 6 wk OI = 90 min/session; 2/wk x 6 wk |
Motor control: Fugl-Meyer range 0–66 Spasticity: Modified Ashworth Scale range 0–25 Strength: manual muscle testing elbow range 0–5 Pain: Visual Analogue Scale range 0–10 ROM: total passive range of motion, as the sum of shoulder flexion, abduction, internal rotation and external rotation, elbow flexion and extension and wrist extension and flexion. Range 0–810°. Separate passive range of motion elbow flexion 0–140°. Follow-up = post-treatment |
UL-EXO7 |
| Conroy et al. (2011) | Adults with chronic stroke | Community-dwelling adults were recruited. | n = 62 Age (yr) = 57.8 (SD = 10.7) Gender = N/A |
Exp RT = robotic therapy planar (n = 20) Exp = robotic therapy planar with vertical (n = 18) OI = intensive conventional arm exercise (n = 19) |
Exp RT = 60 min/session; 3/wk x 6 wk Exp RT = 60 min/session; 3/wk x 6 wk OI = 60 min/session; 3/wk x 6 wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment and 12 weeks |
MIT-MANUS |
| Daly et al. (2005) |
Individuals with stroke for at least 12 months. | Recruited through the Louis Stokes Cleveland Department of Veterans Affairs Medical Center. | n = 12 Age (yr) = N/A (SD = N/A) Gender = 9M / 3F |
Exp RT = robotic therapy + motor learning (n = 6) OI = functional neuromuscular stimulation + motor learning (n = 6) |
Exp RT = robotic therapy (90 min) + motor learning (210 min); 5/wk x 12 wk OI = functional neuromuscular stimulation (90 min) + motor learning (210 min); 5/wk x 12 wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment and 24 weeks |
InMotion2 (Interactive Motion Technologies, Inc, Cambridge, Massachusetts) |
| De Araújo et al. (2011) |
Individuals with a single unilateral stroke for at least 3 months, aged ≥18 years and exhibited hemiparesis of the right side. | Recruited at University of Pernambuco. | n = 12 Age (yr) = N/A (SD = N/A) Gender: 10M / 2F |
Exp RT = robotic therapy (n = 6) OI = physical therapy (n = 6) |
Exp RT = 50 min/session; 3/wk x 8 wk OI = 50 min/session; 3/wk x 8 wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–36 wrist/hand range 0–24 Spasticity: Modified Ashworth Scale elbow range 0–5 and wrist/hand range 0–5 Follow-up = post-treatment |
Electromechanical device (Exoskeleton and static orthosis and Glove) |
| Fasoli et al. (2004) |
Individuals with acute stroke, aged between 27–83 years. | Recruited at Burke Rehabilitation Hospital. | n = 56 Age (yr) = N/A (SD = N/A) Gender = 30M / 26F |
Exp RT = robotic therapy + conventional rehabilitation (n = 30) MI = assisted or assisted active movement (exposure robotic therapy) + conventional rehabilitation (n = 26) |
Exp RT = 60 min/session; 5/wk MI = 12 min/session; 5/wk |
Motor control: Fugl-Meyer range 0–66 Motor Status Score shoulder/elbow range 0–40 wrist/hand range 0–42 Strength: Medical Research Council Motor Power shoulder flexion and abduction and elbow flexion and extension range 0–20 Follow-up = discharge |
MIT-MANUS |
| Hesse et al. (2005) |
Individuals with subacute stroke within the past 4 to 8 weeks. | Recruited from two rehabilitation centers. | n = 44 Age (yr) = N/A (SD = N/A) Gender = 20M / 24F |
Exp RT = robotic therapy (n = 22) OI = electrical stimulation (n = 22) |
Exp RT = 20 min/session; 5/wk x 6 wk OI = 20 min/session; 5/wk x 6 wk |
Motor control: Fugl Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Medical Research Council range 0–45 proximal range 0–15 distal range 0–30 Spasticity: Modified Ashworth Scale total range 0–25 proximal range 0–10 distal range 0–15 Follow-up = post-treatment and 18 weeks |
Bi-manu-track |
| Housman et al. (2009) |
Adults with a single stroke at least 6 months, with moderate/severe hemiparesis. | Recruited through the RIC Sensory Motor Performance Program in Chicago. | n = 31 Age (yr) = N/A (SD = N/A) Gender = 18M / 10F |
Exp RT = robotic therapy + occupational therapist (n = 17) OI = conventional therapy + occupational therapist (n = 17) |
Exp RT = 60 min/session; 3/wk x 8–9 wk OI = 60 min/session; 3/wk x 8–9 wk |
Motor control: Fugl-Meyer range 0–66 ROM: was calculated as the mean distance between a marker placed on the subject’s wrist and 5 targets, following 5 reach attempts to each target. Strength: Grip strength with the Jamar dynamometer range 0–200 Follow-up = post-treatment and 24 weeks |
Therapy Wilmington Robotic Exoskeleton (T-WREX) |
| Hsieh et al. (2011) |
Individuals with chronic stroke for at least 6 months. | Recruited from the Departments of Physical Medicine and Rehabilitation of 3 medical centers in Taiwan. | N = 18 Age (yr) = N/A (SD = N/A) Gender = 13M / 5F |
Exp RT = robotic therapy high intensity (n = 6) Exp = robotic therapy lower intensity (n = 6) OI = conventional therapy (n = 6) |
Exp RT = 90–105 min/session; 5/wk x 4 wk Exp RT = 90–105 min/session; 5/wk x 4 wk (half the number of repetitions) OI = 90–105 min/session; 5/wk x 4 wk |
Motor control: Fugl-Meyer range 0–66 Strength: Medical Research Council range 0–5 shoulder flexors/abductors, elbow flexors/ extensors, wrist flexors/extensors, and flexors/extensors of the metacarpophalangeal joints, the average MRC score was calculated Follow-up = post-treatment |
Bi-manu-track |
| Kahn et al. (2006) |
Individuals with chronic stroke for at least 1 year. | Recruited from outpatient population at the Rehabilitation Institute of Chicago and from a participant database. | n = 19 Age (yr) = N/A (SD = N/A) Gender = 11M / 8F |
Exp RT add = robotic therapy + conventional therapy (n = 10) OI = Free reaching (n = 9) |
Exp RT add = 45 min/session; 3/wk x 8wk OI = 45 min/session; 3/wk x 8wk |
Motor control: Chedoke McMaster Stroke Assessment arm section range 1–7 Follow-up = post-treatment and 24 weeks |
The Assisted Rehabilitation and Measurement Guide, ARM Guide |
| Klamroth-Marganska et al. (2014) |
Individuals with chronic stroke, for at least 6 months, aged ≥18 years. | Recruited from four clinical centers in Switzerland. | n = 73 Age (yr) = N/A (SD = N/A) Gender = 46M / 27F |
Exp RT = robotic therapy (n = 38) OI = conventional therapy (n = 35) |
Exp RT = 45 min/session; 3/wk x 8wk OI = 45 min/session; 3/wk x 8wk |
Motor control: Fugl-Meyer range 0–66 Spasticity: Modified Ashworth Scale range 0–5. Mean values from nine single joint movements: flexion and extension of the elbow, wrist, finger, thumb and flexion of the shoulder. Strength: grip strength with a handheld dynamometer Jamar range 0–200 Follow-up = post-treatment, 16 and 34 weeks |
ARMin |
| Liao et al. (2011) |
Individuals with chronic stroke for at least 6 months. | Recruited from Departments of Physical Medicine and Rehabilitation of three medical centers in Taiwan. | n = 20 Age (yr) = N/A (SD = N/A) Gender = 13M / 7F |
Exp RT add = robotic therapy + training in functional activities + conventional therapy (n = 10) OI = conventional therapy + training in functional activities (n = 10) |
Exp RT add = 90–105 min/session; 5/wk x 4wk OI = 90–105 min/session; 5/wk x 4wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment |
Bi-Manu-Track |
| Lin et al. (2015) |
Individuals with chronic stroke, at least 6 months. |
Recruited at Taipei Veterans General Hospital in Taiwan. | n = 33 Age (yr) = 55.1 (SD = 10.5) Gender = 28M / 5F |
Exp RT = robotic therapy (n = 16) OI = conventional therapy (n = 17) |
Exp RT = 30min/session; 3/wk x 4wkOI = 30min/session; 3/wk x 4wk | Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Follow-up = post-treatment |
Bilateral isometric handgrip force training Ya-May Company |
| Lo et al. (2010) |
Individuals with chronic stroke for at least 6 months, who were 18 years of age or older. | Recruited from four participating Veterans Affairs medical centers. | n = 127 Age (yr) = N/A (SD = N/A) Gender = 122M / 5F |
Exp RT = robotic therapy (n = 49) OI = usual care different time and frequency (n = 28) |
Exp RT = 60 min/session; 3/wk x 12wk OI = 60 min/session; 3/wk x 12wk |
Motor control: Fugl-Meyer range 0–66 Spasticity: Modified Ashworth Scale range 0–5 Pain: Visual Analogue Scale range 0–10 Follow-up = 6, 12, 24 and 36 weeks |
MIT-MANUS |
| Lum et al. (2006) |
Individuals with a single subacute stroke within the past 1 to 5 months. | Not informed. | n = 30 Age (yr) = N/A (SD = N/A) Gender = 20M / 10F |
Exp RT = unilateral robotic therapy (n = 9) Exp = robotic therapy bilateral (n = 5) OI = conventional therapy (n = 6) |
Exp RT = 60 min/session; 4wk Exp RT = 60 min/session; 4wk OI = 60 min/session; 4wk |
Motor control: Fugl-Meyer shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Motor Power Scale range 0–70 Spasticity: Modified Ashworth Scale proximal range 0–15 and distal range 0–30 Follow-up = post-treatment and 24 weeks |
Mirror Image Movement Enabler (MIME) |
| Masiero et al. (2014) |
Individuals with a first, single acute stroke within 15 days, aged ≥18 years. | Recruited from the Stroke Unit in Italy. | n = 30 Age (yr) = N/A (SD = N/A) Gender = 20M / 10F |
Exp RT add = robotic therapy + conventional therapy (n = 14) OI = conventional therapy (n = 16) |
Exp RTadd = 120 min/session; 5/wk x 5wk OI = 120min/session; 5/wk x 5wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Spasticity: Modified Ashworth Scale range 0–5 Strength: Medical Research Council biceps range 0–5 shoulder abduction, elbow flexion, elbow extension, wrist flexion, and extension. Follow-up = post-treatment, 12 and 28 weeks. |
NeReBot |
| McCabe et al. (2015) |
Individuals with chronic stroke, for at least 1 year, aged between 21–81 years. | Not informed. | n = 35 Age (yr) = N/A (SD = N/A) Gender = 23M / 12F |
Exp RT add = robotic therapy + motor learning (n = 12) OI = motor learning (n = 11) |
Exp RT add = robotic therapy (90 min) + motor learning (210 min); 5/wk x 12wk OI = 300 min; 5/wk x 12wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Follow-up = post-treatment |
In Motion 2 shoulder-elbow Robot |
| Page et al. (2012) |
Individuals with chronic stroke, for at least 12 months, aged between 21–75 years. | Recruited using approved advertisements distributed to local stroke support groups and outpatient rehabilitation clinics. | n = 16 Age (yr) = N/A (SD = N/A) Gender = 11M / 5F |
Exp RT add = robotic therapy + repetitive task specific practice (n = 8) OI = repetitive task specific practice (n = 8) |
Exp RT add = 60 min/session; 3/wk x 8wk OI = 60 min/session; 3/wk x 8wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = 1 week post-invertention |
Myomo e100 |
| Rabadi et al. (2008) |
Individuals with acute stroke, within 4 weeks of admission. | Recruited from a stroke unit in a Burke Rehabilitation Hospital. | n = 30 Age (yr) = N/A (SD = N/A) Gender = 19M / 11F |
Exp RT add = conventional therapy + robotic therapy (n = 10) OI = occupational therapy (n = 10) |
Exp RT add = conventional therapy (180 min) + robotic therapy (40 min); 12 sessions; 5/wk OI = 220 min; 12 sessions; 5/wk |
Motor control: Fugl-Meyer shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Motor power score is obtained by assessing 14 movements at the scapular, shoulder and elbow joints range 0–70 Spasticity: Modified Ashworth Scale across nine groups of arm muscles range 0–45. Pain: Pain Scale of Fugl-Meyer range 0–24 Follow-up = post-treatment |
MIT-MANUS |
| Ramos-Murguialday et al. (2013) |
Individuals with chronic stroke, for at least 10 months, aged between 18–80 years. | Recruited from via public information (German stroke associations, rehabilitation centers, hospitals) all over Germany. | n = 30 Age (yr) = N/A (SD = N/A) Gender = 18M / 12F |
Exp RT = robotic therapy + physiotherapy (n = 16) MI = sham robotic therapy + physiotherapy (n = 14) |
Exp RT = 5/wk x 4wk MI = 5/wk x 4wk |
Motor control: Fugl-Meyer total range 0–54 shoulder/elbow range 0–30 wrist/hand range 0–24 Spasticity: Modified Ashworth Scale range 0–56 Follow-up = post-treatment |
Brain-Machine-Interface arm and hand orthoses ReoGo robotic arm |
| Reinkensmeyer et al. (2012) | Adults with a single stroke, for at least 3 months. | Recruited through local hospitals and stroke support groups in California. | n = 26 Age (yr) = N/A (SD = N/A) Gender = 17M / 9F |
Exp RT add = robotic therapy + conventional therapy (n = 13) OI = conventional therapy (n = 13) |
Exp RT add = 60 min/session; 3/wk x 8wk OI = 60 min/session; 3/wk x 8wk |
Motor control: Fugl-Meyer range 0–66 Strength: Grip strength with a Jamar Hand Dynamometer range 0–200 Follow-up = post-treatment and 12 weeks |
Pneu-Wrex |
| Sale et al. (2014) |
Individuals with a first acute stroke, after 30 ± 7 days. | Recruited at San Raffaele Pisana and Auxilium Vitae Rehabilitation Centre in Italy. | n = 53 Age (yr) = N/A (SD = N/A) Gender = 31M / 22F |
Exp RT = robotic therapy + physiotherapy (n = 26) OI = conventional therapy + physiotherapy (n = 27) |
Exp RT = robotic therapy (45 min) + physiotherapy (180 min); 5/wk x 6wk OI = conventional therapy (45 min) + physiotherapy (180 min); 5/wk x 6wk |
Motor control: Fugl-Meyer range 0–66 Spasticity: Modified Ashworth Scale elbow range 0–5 ROM: total passive range of motion, as the sum of shoulder and elbow movements (shoulder flexion/extension, abduction, intra/extra rotation and elbow extension) range 0–720 Strength: Motricity Index (MI) as the sum of shoulder and elbow movements (shoulder flexion/extension, abduction, intra/extra rotation and elbow extension) range 0–100. Follow-up = post-treatment |
MIT-MANUS |
| Sale et al. (2014) |
Individuals with a first acute stroke, for at least 30 ± 7 days, aged between 18–80 years. | Not informed. | n = 20 Age (yr) = N/A (SD = N/A) Gender = 14M / 6F |
Exp RT = robotic therapy + physiotherapy (n = 11) OI = conventional therapy + physiotherapy (n = 9) |
Exp RT = robotic therapy (40 min) + physiotherapy (180 min); 4/wk x 4/wk OI = conventional therapy (40 min) + physiotherapy (180 min); 4/wk x 4/wk |
Motor control: Fugl-Meyer wrist/hand range 0–24 Strength: Medical Research Council hand flexor and extensor muscles range 0–5 Spasticity: Modified Ashworth Scale range 0–5 Follow-up = post-treatment and 12 weeks |
Amadeo Robotic System |
| Simkins et al. (2013) | Individuals with chronic stroke, for at least 6 months, aged between 23–69 years. | Recruited at University of California. | n = 15 Age (yr) = N/A (SD = N/A) Gender = N/A |
Exp RT = unilateral robotic therapy (n = 5) Exp = robotic therapy bilateral (n = 5) OI = repetitive task practice (n = 5) |
Exp RT = 90 min/session; 2/wk x 12wk Exp RT = 90 min/session; 2/wk x 12wk OI = 90 min/session; 2/wk x 12wk |
Motor control: Fugl-Meyer range 0–66 ROM: elbow flexion 0–140° wrist flexion range 0–80° Strength: Manual muscle test elbow and wrist range 0–5 Pain: Visual Analogue Scale range 0–10 Follow-up = post-treatment |
EXO-UL7 |
| Susanto et al. (2015) |
Individuals with chronic stroke, within 6 to 24 months. | Not informed. | n = 19 Age (yr) = N/A (SD = N/A) Gender = 14M / 5F |
Exp RT = robotic therapy + conventional therapy (n = 9) MI = non-assisted robot + conventional therapy (n = 10) |
Exp RT = 60 min/session; 4/wk x 5wk MI = 60 min/session; 4/wk x 5wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–36 wrist/hand range 0–24 Follow-up = post-treatment and 24 weeks |
The modified hand exoskeleton robot |
| Timmermans et al. (2014) | Individuals with chronic stroke, post-stroke time ≥ 8 months, aged between 18–85 years. | Recruited from Adelante Rehabilitation Centre (Hoensbroek, NL). | n = 22 Age (yr) = N/A (SD = N/A) Gender = 16M / 6F |
Exp RT add = robotic therapy + task-oriented training method (n = 11) OI = arm-hand training program (n = 11) |
Exp RT add = 30 min/session; 4/wk x 8wk OI = 30 min/session; 4/wk x 8wk |
Motor control: Fugl Meyer range 0–66 Follow-up = post-treatment and 24 weeks |
Haptic Master |
| Volpe et al. (1999) | Individuals with acute stroke. | Recruited from neurologic rehabilitation service. | n = 12 Age (yr) = N/A (SD = N/A) Gender = 7M / 5F |
Exp RT = robotic therapy + conventional therapy (n = 6) MI = sham robotic therapy + conventional therapy (n = 6) |
Exp RT = 60 min/session; 5/wk MI = 60 min/session; 5/wk |
Motor control: Fugl-Meyer shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Motor power scale shoulder/elbow (biceps, triceps, and anterior and lateral deltoid muscles) range 0–20. Follow-up = 144 weeks after discharge |
MIT-MANUS |
| Volpe et al. (2008) | Individuals with chronic stroke and who had impaired arm and hand mobility for at least 6 months. | Recruited form outpatient clinic. | n = 21 Age (yr) = N/A (SD = N/A) Gender = 15M / 6F |
Exp RT = robotic therapy (n = 11) OI = conventional therapy (n = 10) |
Exp RT = 60 min/session; 3/wk x 6wk OI = 60 min/session; 3/wk x 6wk |
Motor control: Fugl-Meyer shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Motor Power Scale shoulder and elbow range 0–70 Spasticity: Modified Ashworth Scale passive movements, across 9 muscle groups range 0–5 Pain: Pain scale from the Fugl-Meyer range 0–24 Follow-up = post-treatment and 12 weeks |
MIT-MANUS |
| Wu et al. (2012) |
Individuals with unilateral chronic stroke, for at least 6 months. | Not informed. | n = 42 Age (yr) = 54.4 (SD = 9.69) Gender = 32M / 10F |
Exp RT = robot-assisted bilateral arm training OI = conventional therapy (n = 14) |
Exp RT = 105 min/session; 5/wk x 4wk OI = 105 min/session; 5/wk x 4wk |
Motor control: Fugl-Meyer range 0–66 Follow-up = post-treatment |
Bi-manu-track |
| Xu et al. (2012) |
Individuals with 6 months to 2 years after a single mild to moderate stroke, aged 55 years and above. | Recruited from outpatients from Zhongda Hospital (affiliated with Southeast University) and Nanjing Tongren Hospital. | n = 18 Age (yr) = N/A (SD = N/A) Gender = 11M / 7F |
Exp RT = robotic therapy (n = 9) OI = conventional therapy (n = 9) |
Exp RT = 3/wk x 16wk OI = 3/wk x 16wk |
Strength: Maximum resistive force with WAM control program Follow-up = post-treatment |
Barrett WAMTM Arm |
| Xu et al. (2014) |
Individuals with chronic stroke, aged 50 years and over. | Recruited from Zhongda Hospital affiliated Southeast University and Nanjing Tongren Hospital. | n = 45 Age (yr) = N/A (SD = N/A) Gender = 27M / 18F |
Exp RT = robotic therapy (n = 23) OI = conventional therapy (n = 22) |
Exp RT = 120 min/session; 6/wk x 20wk OI = 120 min/session; 6/wk x 20wk |
ROM: Passive range of motion with the assistance of WAM or therapist for elbow. Strength: Maximum resistive force Follow-up = post-treatment |
Barrett WAMTM manipulator |
| Yang et al. (2012) |
Individuals with unilateral chronic stroke, within 6 months to 5 years, with an average age of 51.29 years. | Not informed. | n = 21 Age (yr) = 51.2 (SD = N/A) Gender = 14M / 7F |
Exp RT add = unilateral robotic therapy + functional task practice (n = 7) Exp RT add = bilateral robotic therapy + functional task practice (n = 7) OI = standard rehabilitation (90–105 min/session) (n = 7) |
Exp RT add = unilateral robotic therapy (75–180 min) + functional task practice (15–20 min); 5/wk x 4wk Exp RT add = bilateral robotic therapy (75–180 min) + functional task practice (15-20min); 5/wk x 4wk OI = standard rehabilitation (90–105 min/session); 5/wk x 4wk |
Motor control: Fugl-Meyer total range 0–66 shoulder/elbow range 0–42 wrist/hand range 0–24 Strength: Medical Research Councilproximal (shoulder flexors, abductors, elbow flexors and extensors and distal (flexors and extensors of wrist and fingers) range 0–5. Spasticity: Modified Ashworth Scale range 0–4 Follow-up = post-treatment |
Bi-manu-track |
| Yoo et al. (2013) |
Individuals with chronic stroke who had no visual or cognitive problems. | Not informed. | n = 22 Age (yr) = N/A (SD = N/A) Gender = 13M / 9F |
Exp RT add = robotic therapy + conventional therapy (n = 11) OI = conventional therapy (n = 11) |
Exp RT add = robotic therapy (30 min) + conventional therapy (60 min); 3/wk x 6wk OI = conventional therapy (60 min/session); 3/wk x 6wk |
Strength: Medical Research Council range 0–5 Follow-up = post-treatment |
ReogoTM |
n = sample size; SD = standard deviation; Exp = experimental group; Con = control group; N/A = not available; OI = other intervention; MI = minimal intervention; RTP = repetitive task practice; RT = Robot assisted therapy; wk = week(s); yr = year(s); min = minutes; h = hours; ROM = range of motion.
The duration of RT ranged from 2[25] to 20[57] weeks, and the frequency per week varied from 2[16,18] to 6[57] days. The time spent per session of intervention ranged from 0.2[40] to 2[57] hours. The total volume of intervention per week (i.e., number of sessions per week x duration of each session) ranged from 1[54] to 12[57] hours. The total number of sessions ranged from 12[16,25,45] to 120[57], with most studies ranging from 20 to 24. The total duration of the intervention ranged from 6[45] to 240[57] hours. On average, RT sessions occurred three times per week with a total duration of treatment of 8 weeks. For some studies, primarily those comparing RT to minimal intervention, detailed information on the dose and duration of the intervention was not available[35,36,48,54,56].
Thirty-five studies evaluated motor control using three different instruments. Of these 35 studies, 33 (94.2%)[15,16,18–27,35–38,40–41,44–59] used the Fugl Meyer (FM), two studies (5.7%)[34,42] used the Chedoke McMaster Stroke Assessment (CMSA). Fourteen studies[15–17,20,25,26,38,40,43,46,48,50,51,55] evaluated spasticity using the Modified Ashworth Scale (MAS). Twenty-one studies evaluated strength using six different instruments. Of these 21 studies, seven (33.3%)[15,21,39,40,46,51,58] used the Medical Research Council (MRC), three (14.2%)[41,43,49] used the hand-held dynamometer, six (28.5%)[17,20,25,35,54,55] used the Motor Power Scale (MP), two (9.5%) used the Manual Muscle Testing (MMT)[16,18] and the WAM control program[56,57], and one study[51] used the Motricity Index (MI). To homogenize the data, Newton and kilogram-force values were converted into pounds. We arbitrarily decided to use pounds because this was the most consistent unit among the studies. Five studies evaluated range of motion using three different measures. Of these 5 studies, three studies (60.0%)[16,18,50] assessed range of motion using goniometer, one study[57] used the WAM control program, and one study[41] used the mean distance between a marker placed on the participant’s wrist and five targets. Six studies evaluated pain using three different instruments. Of these 6 studies, three studies (50%)[16,18,26] used the Visual Analogue Scale (VAS), two studies (33.3%)[25,56] used the Pain Scale of Fugl-Meyer, and one study[34] used the Chedoke McMaster Stroke Assessment Pain Inventory Scale.
Methodological quality of the included studies
The detailed methodological quality of the included studies is presented in S1 Table on the Addenda. The mean methodological quality of the 38 studies was 6.0 on the 0 to 10 PEDro scale. Most studies included the following: between-group comparisons (n = 37 studies, 97.3%); precision and variability estimates (n = 35 studies, 92%); group similarity at baseline and assessor blinding (n = 32 studies, 84.1%); and outcome measures for at least 85% of participants (n = 27 studies, 71%). Concealed allocation was presented in 12 studies (31.5%), and intention-to-treat analysis was presented in 10 studies (26.3%). The primary methodological quality issues were related to the blinding of participants and therapists, which was included in only three (7.9%) and two (5.2%) studies, respectively.
Effects of robot-assisted therapy
Five studies compared RT with minimal intervention (i.e., sham RT[35,48,54], exposure RT[39,52]), twenty three studies compared RT with OI, i.e., conventional therapy[17,19,20,21,24,34,36,37,41,43,45,50,51,55–57], usual care[26], repetitive task practice[16,18], intensive conventional arm exercise program[22], physical therapy[38], electrical stimulation[23,40], and ten studies investigated the additional effects of RT over OI, i.e., RT added to conventional therapy[25,42,44,49,58], standard therapy[46], motor learning[27], repetitive task-specific practice[47], an arm-hand training program[53] and functional task practice[15]. All 38 included studies reported short-term effects, 15 studies (39.4%) reported medium-term effects[17,20,22,23,26,40–43,46,49,51–53,55] and one study[54] reported long-term effects.
Robot-assisted therapy versus minimal intervention
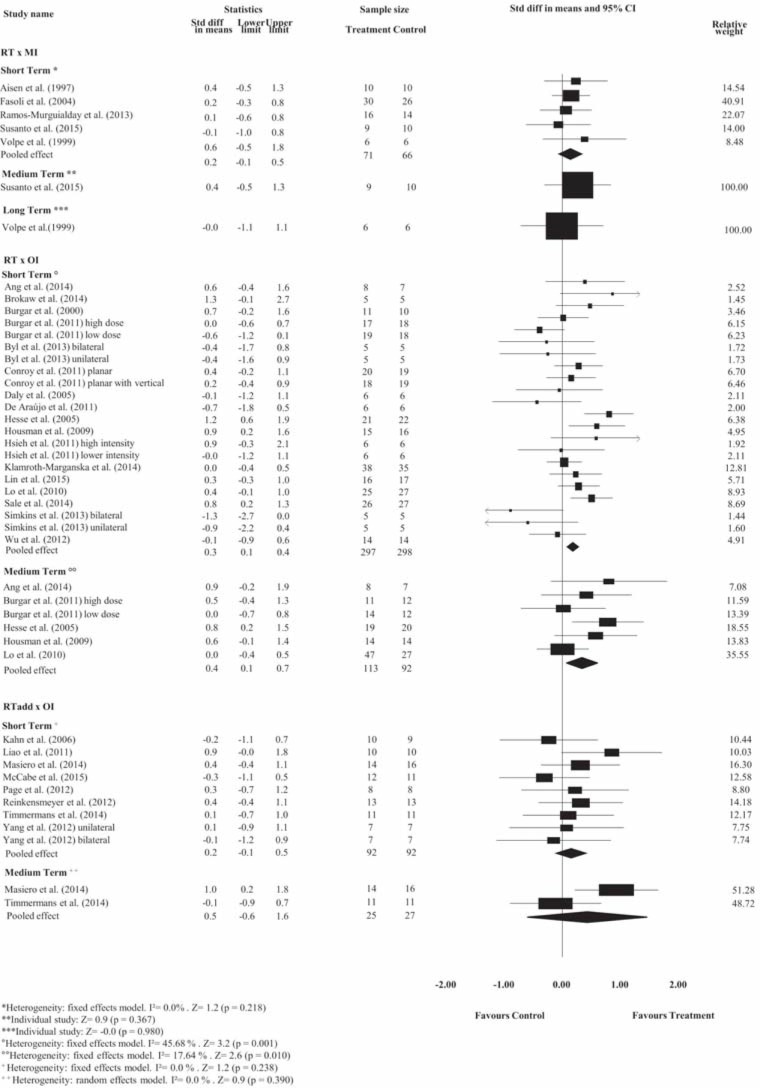
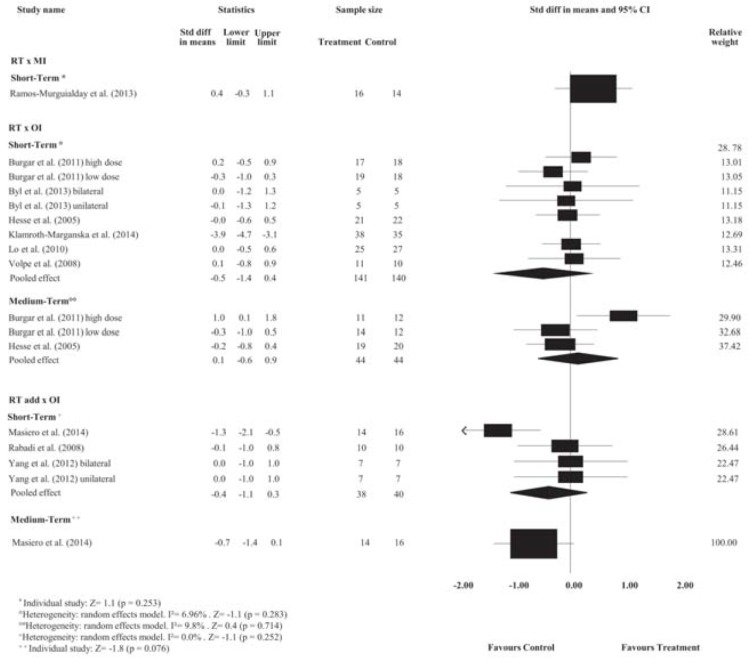
Pooled estimates showed no effects of RT on motor control at short-, medium- or long-term follow-ups and no effects on spasticity at short-, medium- or long-term follow-ups compared with minimal intervention (p> 0.05). Detailed analyses are presented in Figs 2 and 3. The strength of the evidence ranged from low- to very low-quality.
Fig 2. Standardized mean difference (95% CI) comparing RT or additional effect of RT versus MI or OI for motor control of people with limited upper limb function.
RT = Robot-assisted therapy; RT add = additional effect of Robot-assisted therapy; OI = other intervention; MI = minimal intervention.
Fig 3. Standardized mean difference (95% CI) comparing RT or additional effect of RT versus OI or MI for spasticity of people with limited upper limb function.
RT = Robot-assisted therapy; RT add = additional effect of Robot-assisted therapy; OI = other intervention; MI = minimal intervention.
Robot-assisted therapy versus other intervention
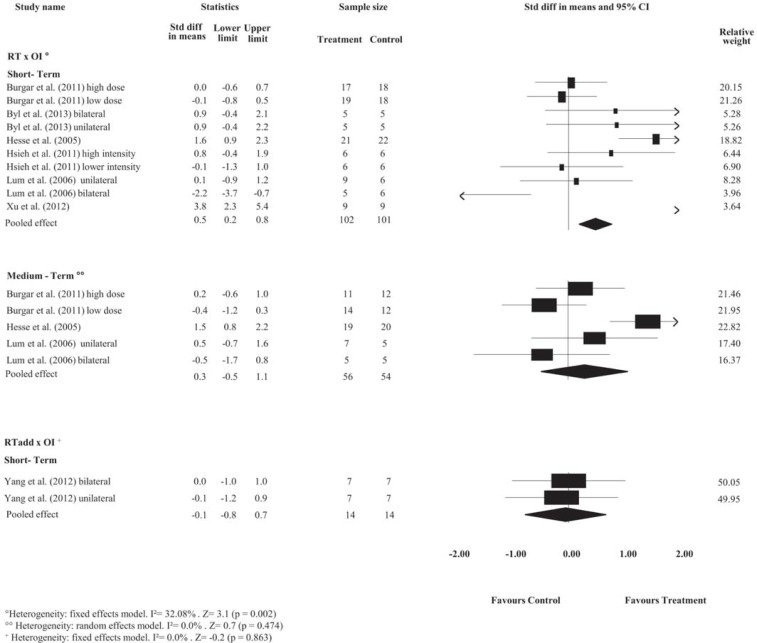
The pooled estimates showed small effects of RT on motor control and medium effects on strength compared with OI at the short-term follow-up. The SMDs were, respectively, 0.3 (95% CI 0.1 to 0.4); and 0.5 (95% CI 0.2 to 0.8). Detailed analyses are presented in Figs 2 and 4. There is high- and very low-quality evidence showing that RT has effects on motor control and strength, respectively, compared to OI at the short-term follow-up.
Fig 4. Standardized mean difference (95% CI) comparing RT versus OI for strength in people with limited upper limb function.
RT = Robot-assisted therapy; OI = other intervention.
Pooled estimates showed no effects of RT on spasticity, range of motion and pain at short-term follow-up, or on motor control, spasticity and strength at medium-term follow-up, when compared with OI (p> 0.05). Detailed analyses are presented in Figs 2 to 4 and S1 and S2 Figs. The strength of the evidence ranged from low- to very low-quality.
Additional effects of robot-assisted therapy over other interventions
Pooled estimates showed no additional effects of RT on motor control, spasticity and pain at short-term follow-up, or on motor control and spasticity at the medium-term follow-up in stroke compared with stand-alone OI (p> 0.05). Detailed analyses are presented in Figs 2 and 3 and S1 and S2 Figs. The strength of the evidence ranged from low- to very low-quality.
Subgroup analysis
We investigated the impact of methodological quality, portions of the assessed upper limb, duration of stroke, and treatment dose and duration on the estimated short-term effects of RT compared with OI (see detailed subgroup analyses in S3 Fig). Methodological quality, and dose impacted the estimated effects for motor control. Poor methodological quality, and lower treatment dose and duration may impact negatively the estimated effects.
Discussion
This review included 38 studies comparing the efficacy of RT with minimal intervention or OI, and investigating additional effects of RT combined with OI on body function and structure in people with upper limb limitations caused by stroke. RT has small effects on motor control and medium effects on muscle strength. Moreover, the methodological quality, portion of the upper limb, treatment dose, duration and volume may impact the estimated effects. The current low-quality evidence suggests that estimated effects are likely to change with future high-quality studies, and effects are not consistent among outcomes related to body function and structure.
Our findings revealed that compared with OI, RT has statistically significant but small effects on motor control and medium effects on strength. These short-term findings comparing RT with OI are consistent with other reviews on stroke. Veerbeek et al.[12] showed a small improvement on motor control and muscle strength and no effect on spasticity. Prange et al.[8] also found improvement on motor control at the short-term follow-up compared to conventional rehabilitation.
Previous reviews[8,10] did not investigate the medium- and long-term effects. Despite this, Norouzi-Gheidari et al.[10] suggested no effects on motor control at medium-term follow-up when the same doses of RT and OI were used. Our results were consistent with those of the previous study and suggest that upper limb motor control improvement occurs within the short-term (≤ 3 months after stroke)[59]. Moreover, Prange et al.[8] found long-term effects on motor control when RT was used compared to OI. Their findings were not consistent with our results, and a possible explanation is that the previous review[8] included poor-quality studies (i.e., non-randomized controlled studies). As suggested by Norouzi-Gheidari et al.[10], future high-quality studies should confirm our findings because current evidence for the estimated effect is very low and likely to change.
When comparing the efficacy of RT with minimal intervention at different time points, despite trends favouring treatment, the current low-quality evidence showed no significant effects. Susanto et al.[52] stated that there is an insignificant effect, but there are few studies, and they have small samples.
The average methodological quality of the 39 included studies was 6 points on the 0 to 10 PEDro scale, ranging from 2 to 8 points. This quality was consistent with that reported by Veerbeek et al.[12], with an average quality of 6.0 points. The primary methodological issues were related to blinding, which is expected due to the difficulty of fulfilling these criteria in the area of RT.
A subgroup analysis showed that the portions of the assessed upper limb influence the estimated effects only for range of motion. These findings were not consistent with other studies[9,10,12] and were similar to those reported by Mehrholz et al.[11]. Therefore, there is no consensus on the impact of portions of the assessed upper limb, and current evidence is low but likely to change with further high-quality studies that include larger samples. Subgroup analysis also suggested a greater effect on motor control in chronic stroke, similar to most recent review[28]. Subgroup analysis also suggested that when conventional therapy (CT) is used at the same dose as robot-assisted therapy (RT), there is a significant effect on motor control, unlike the findings reported by Kwakell[9]. Subgroup analysis also suggested an impact of the number of sessions and treatment volume on some estimated effects. Greater number of sessions seems to impact motor control, and greater treatment volume seems to impact motor control. The effect of greater treatment dose was suggested by Lohse et al.[60]; however, time as a dose representation is a rather crude estimate and provides no evidence of the actual amount of movement or types of movement, nor does this representation take into account periods of inactivity or rest[61]. In this regard, a previous review indicated that although there is no consensus, the minimum dose should be at least 16 hours of training[62].
This review and the current literature have some potential limitations. First, there is only a small number of randomized controlled studies that mainly investigate range of motion and pain, and few studies comparing RT with minimal intervention at different time points. Second, studies typically had small sample sizes. Third, subgroup analyses did not investigate impact of types of RT devices, and dichotomization was a potential limitation to get full information regarding the impact of the investigated factors.
Further high-quality randomized controlled studies with larger sample sizes are warranted to elucidate more precise effects of RT on outcomes related to body function and structure, especially the long-term effects. Studies comparing RT with minimal intervention should be conducted, since the current evidence is very low-quality. These studies should report the treatment dose and duration. Future studies should investigate whether RT is effective on psychological factors, and other outcomes related to the activity and participation domains in the ICF. In addition, it is imperative to conduct studies on the cost-effectiveness of RT.
In conclusion, RT has small effects on motor control and medium effects on strength in people with limited upper limb function caused by stroke. Poor methodological quality, and lower treatment dose and duration may impact negatively the estimated effects. Clinicians consider this approach because it has few or no side effects. In addition, there may be long-term financial benefits to employing therapeutic robots. The current low-quality evidence suggests that the estimated effects are likely to change with future high-quality studies and that the effects are not consistent among outcomes related to body function and structure.
Supporting information
(DOC)
RT = Robot-assisted therapy; OI = other intervention.
(EPS)
RT = Robot-assisted therapy; RT add = additional effect of Robot-assisted therapy; OI = other intervention.
(EPS)
RT = Robot-assisted therapy; OI = other intervention; ROM = range of motion.
(EPS)
(EPS)
Y = yes; N = no.
(DOC)
(DOC)
(DOCX)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Maciejasz P, Eschweiler J, Gerlach-Hahn K, Jansen-Troy A, Leonhardt S. A survey on robotic devices for upper limb rehabilitation. J Neuroeng Rehabil 2014; 11:1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poli P, Morone G, Rosati G, Masiero S. Robotic technologies and rehabilitation: new tools for stroke patients’ therapy. Biomed Res Int 2013; article ID 153872:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol 2009; 8:741–754. 10.1016/S1474-4422(09)70150-4 [DOI] [PubMed] [Google Scholar]
- 4.Jarrassé N, Proietti T, Crocher V, Robertson J, Sahbani A, Morel G, et al. Robotic exoskeletons: a perspective for the rehabilitation of arm coordination in stroke patients. Front Hum Neurosci 2014; 8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duret C, Courtial O, Grosmaire A, Hutin E. Use of a robotic device for the rehabilitation of severe upper limb paresis in subacute stroke: exploration of patient/robot interactions and the motor recovery process. Biomed Res Int 2015; ID 482389:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hsieh Y, Wu C, Lin K, Yao G, Wu K, Chang Y. Dose–response relationship of robot-assisted stroke motor rehabilitation—the impact of initial motor status. Stroke 2012; 43:1–7. [DOI] [PubMed] [Google Scholar]
- 7.Basteris A, Nijenhuis SM, Stienen AHA, Buurke JK, Prange GB, Amirabdollahian F. Training modalities in robot-mediated upper limb rehabilitation in stroke: a framework for classification based on a systematic review. J Neuroeng Rehabil 2014; 11:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prange GB, Jannink MJA, Groothuis-Oudshoorn CGM, Hermes HJ, IJzerman MJ. Systematic review of the effect of robot-aided therapy on recovery of the hemiparetic arm after stroke. J Rehabil Res Dev 2006; 43:171–184. [DOI] [PubMed] [Google Scholar]
- 9.Kwakkel G, Kollen BJI, Krebs HI. Effects of robot-assisted therapy on upper limb recovery after stroke: a systematic review. Neurorehabil Neural Repair 2008; 22:111–121. 10.1177/1545968307305457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Norouzi-Gheidari N, Archambault PS, Fung J. Effects of robot-assisted therapy on stroke rehabilitation in upper limbs: systematic review and meta-analysis of theliterature. J Rehabil Res Dev 2012; 49:479–496. [DOI] [PubMed] [Google Scholar]
- 11.Mehrholz J, Pohl M, Platz T, Kugler J, Elsner B. Electromechanical and robot-assisted armtraining for improving activities of daily living, arm function, and arm muscle strength after stroke (review). Cochrane Database Syst Rev 2015; 11:1–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veerbeek JM, Langbroek-Amersfoort AC, Van Wegen EEH, Meskers CGM, Kwakkel G. Effects of robot-assisted therapy for the upper limb after stroke: a systematic review and meta-analysis. Neurorehabil Neural Repair 2016; 1–15. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. International Classification of Functioning, Disability and Health, ICF WHO Library Cataloguing-in-Publication Data, Geneva, 2001.
- 14.Sivan M, O'Connor RJ, Makower S, Levesley M, Bhakta B. Systematic review of outcome measures used in the evaluation of robot-assisted upper limb exercise in stroke. J Rehabil Med 2011; 43:181–189. 10.2340/16501977-0674 [DOI] [PubMed] [Google Scholar]
- 15.Yang C, Lin K, Chen H, Wu C, Chen C. Pilot comparative study of unilateral and bilateral robot-assisted training on upper-extremity performance in patients with stroke. Am J Occup Ther 2012; 66:198–206. 10.5014/ajot.2012.003103 [DOI] [PubMed] [Google Scholar]
- 16.Byl NN, Abrams GM, Pitsch E, Fedulow I, Kim H, Simkins M, et al. Chronic stroke survivors achieve comparable outcomes following virtual task specific repetitive training guided by a wearable robotic orthosis (UL-EXO7) and actual task specific repetitive training guided by a physical therapist. J Hand Ther 2013; 26:343–352. 10.1016/j.jht.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 17.Lum PS, Burgar CG, Van der Loos M, Shor PC, Majmundar M, Yap R. MIME robotic device for upper-limb neurorehabilitation in subacute stroke subjects: a follow-up study. J Rehabil Res Dev 2006; 43:631–642. [DOI] [PubMed] [Google Scholar]
- 18.Simkins M, Kim H, Abrams G, Byl N, Rosen J. Robotic unilateral and bilateral upper-limb movement training for stroke survivors afflicted by chronic hemiparesis. IEEE Int Conf Rehabil Robot 2013; June:1–6. [DOI] [PubMed] [Google Scholar]
- 19.Wu C, Yang C, Chuang L, Lin KC, Chen HC, Chen MD, et al. Effect of therapist-based versus robot-assisted bilateral arm training on motor control, functional performance, and quality of life after chronic stroke: a clinical trial. Phys Ther 2012; 92:1006–1016. 10.2522/ptj.20110282 [DOI] [PubMed] [Google Scholar]
- 20.Burgar CG, Lum PS, Scremin AME, Garber SL, Van der Loos HF, Kenney D, et al. Robot-assisted upper-limb therapy in acute rehabilitation setting following stroke: Department of Veterans Affairs multisite clinical trial. J Rehabil Res Dev 2011; 48:445–458. [DOI] [PubMed] [Google Scholar]
- 21.Hsieh Y, Wu C, Liao W, Lin K, Wu K, Lee C. Effects of treatment intensity in upper limb robot-assisted therapy for chronic stroke: a pilot randomized controlled trial. Neurorehabil Neural Repair 2011; 25:503–511. 10.1177/1545968310394871 [DOI] [PubMed] [Google Scholar]
- 22.Conroy SS, Whitall J, Dipietro L, Jones-Lush LM, Zhan M, Finley MA, et al. Effect of gravity on robot-assisted motor training after chronic stroke: a randomized trial. Arch Phys Med Rehabil 2011; 92:1754–1761. 10.1016/j.apmr.2011.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daly JJ, Hogan N, Perepezko EM, Krebs HI, Rogers JM, Goyal KS, et al. Response to upper-limb robotics and functional neuromuscular stimulation following stroke. J Rehabil Res Dev 2005; 42:723–736. [DOI] [PubMed] [Google Scholar]
- 24.Ang KK, Guan C, Phua KS, Wang C, Zhou L, Tang KY, et al. Brain-computer interface based robotic end effector system for wrist and hand rehabilitation: results of a three-armed randomized controlled trial for chronic stroke. Front Neuroeng 2014; 7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rabadi MH, Galgano M, Lynch D, Akerman M, Lesser M, Volpe BT. A pilot study of activity-based therapy in the arm motor recovery post stroke: a randomized controlled trial. Clin Rehabil 2008; 22:1071–1082. 10.1177/0269215508095358 [DOI] [PubMed] [Google Scholar]
- 26.Lo AC, Guarino PD, Richards LG, Haselkorn JK, Wittenberg GF, Federman DG, et al. Robot-assisted therapy for long-term upper-limb impairment after stroke. N Engl J Med 2010; 362:1772–1783. 10.1056/NEJMoa0911341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCabe J, Monkiewicz M, Holcomb J, Pundik S, Daly JJ. Comparison of robotics, functional electrical stimulation, and motor learning methods for treatment of persistent upper extremity dysfunction after stroke: a randomized controlled trial. Arch Phys Med Rehabil 2015; 96:981–990. 10.1016/j.apmr.2014.10.022 [DOI] [PubMed] [Google Scholar]
- 28.Bertani R, Melegari C, De Cola MC, Bramanti A, Bramanti P, Calabrò RS. Effects of robot-assisted upper limb rehabilitation in stroke patients: a systematic review with meta-analysis. Neurol Sci 2017; 38:1561–1569. 10.1007/s10072-017-2995-5 [DOI] [PubMed] [Google Scholar]
- 29.Dietz V, Sinkjaer T. Spastic movement disorder: impaired reflex function and altered muscle mechanics. Lancet Neurol 2007; 6:725–733. 10.1016/S1474-4422(07)70193-X [DOI] [PubMed] [Google Scholar]
- 30.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions, Version 5.1.0 [update March 2011]. The Cochrane Collaboration, 2011. Available from: www.cochrane-handbook.org. [acessed 3 September 2016].
- 31.Cohen J. Statistical Power Analysis for the Behavioural Sciences New York, NY: Academic Press; 1977. [Google Scholar]
- 32.Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011; 64:401–406. 10.1016/j.jclinepi.2010.07.015 [DOI] [PubMed] [Google Scholar]
- 33.Henschke N, Ostelo RWJG, Van Tulder MW, Vlaeyen JW, Morley S, Assendelft WJ, et al. Behavioural treatment for chronic low-back pain. Cochrane Database Syst Rev 2010; 7:CD002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abdullah HA, Tarry C, Lambert C, Barreca S, Allen BO. Results of clinicians using a therapeutic robotic system in an inpatient stroke rehabilitation unit. J Neuroeng Rehabil 2011; 8:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aisen ML, Krebs HI, Hogan N, McDowell F, Volpe BT. The effect of robot-assisted therapy and rehabilitative training on motor recovery following stroke. Arch Neurol 1997; 54:443–446. [DOI] [PubMed] [Google Scholar]
- 36.Brokaw EB, Nichols D, Holley RJ, Lum PS. Robotic therapy provides a stimulus for upper limb motor recovery after stroke that is complementary to and distinct from conventional therapy. Neurorehabil Neural Repair 2014; 28:367–376. 10.1177/1545968313510974 [DOI] [PubMed] [Google Scholar]
- 37.Burgar CG, Lum PS, Shor PC, Van der Loos M. Development of robots for rehabilitation therapy: the Palo Alto VA/Stanford experience. J Rehabil Res Dev 2000; 37:663–673. [PubMed] [Google Scholar]
- 38.De Araújo RC, Junior FL, Rocha DN, Sono TS, Pinotti M. Effects of intensive arm training with an electromechanical orthosis in chronic stroke patients: a preliminary study. Arch Phys Med Rehabil 2011; 92:1746–1753. 10.1016/j.apmr.2011.05.021 [DOI] [PubMed] [Google Scholar]
- 39.Fasoli SE, Krebs HI, Ferraro M, Hogan N, Volpe BT. Does shorter rehabilitation limit potential recovery poststroke? Neurorehabil Neural Repair 2004; 18:88–94. 10.1177/0888439004267434 [DOI] [PubMed] [Google Scholar]
- 40.Hesse S, Werner C, Pohl M, Rueckriem S, Mehrholz J, Lingnau ML. Computerized arm training improves the motor control of the severely affected arm after stroke: a single-blinded randomized trial in two centers. Stroke 2005; 36:1960–1966. 10.1161/01.STR.0000177865.37334.ce [DOI] [PubMed] [Google Scholar]
- 41.Housman SJ, Scott KM, Reinkensmeyer DJ. A randomized controlled trial of gravity-supported, computer-enhanced arm exercise for individuals with severe hemiparesis. Neurorehabil Neural Repair 2009; 23:505–514. 10.1177/1545968308331148 [DOI] [PubMed] [Google Scholar]
- 42.Kahn LE, Zygman ML, Rymer WZ, Reinkensmeyer DJ. Robotassisted reaching exercise promotes arm movement recovery in chronic hemiparetic stroke: a randomized controlled pilot study. J Neuroeng Rehabil 2006; 3:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Klamroth-Marganska V, Blanco J, Campen K, Curt A, Dietz V, Ettlin T, et al. Three dimensional, task-specific robot therapy of the arm after stroke: a multicentre, parallel-group randomised trial. Lancet Neurol 2014; 13:159–166. 10.1016/S1474-4422(13)70305-3 [DOI] [PubMed] [Google Scholar]
- 44.Liao W, Wu C, Hsieh Y, Lin K, Chang W. Effects of robot-assisted upper limb rehabilitation on daily function and real-world arm activity in patients with chronic stroke: a randomized controlled trial. Clin Rehabil 2011; 26:111–120. 10.1177/0269215511416383 [DOI] [PubMed] [Google Scholar]
- 45.Lin C, Chou L, Luo H, Tsai P, Lieu F, Chiang S, et al. Effects of computer-aided interlimb force coupling training on paretic hand and arm motor control following chronic stroke: a randomized controlled trial. Plos One 2015; 10:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Masiero S, Armani M, Ferlini G, Rosati G, Rossi A. Randomized trial of a robotic assistive device for the upper extremity during early inpatient stroke rehabilitation. Neurorehabil Neural Repair 2014; 28:377–386. 10.1177/1545968313513073 [DOI] [PubMed] [Google Scholar]
- 47.Page SJ, Hill V, White S. Portable upper extremity robotics is as efficacious as upper extremity rehabilitative therapy: a randomized controlled pilot trial. Clin Rehabil 2012; 27:494–503. 10.1177/0269215512464795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ramos-Murguialday A, Broetz D, Rea M, Läer L, Yilmaz O, Brasil F, et al. Brain-machine-interface in chronic stroke rehabilitation: a controlled study. Ann Neurol 2013; 74:100–108. 10.1002/ana.23879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinkensmeyer DJ, Wolbrecht ET, Chan V, Chou C, Cramer SC, Bobrow JE. Comparison of 3D, assist-as-needed robotic arm/hand movement training provided with Pneu-WREX to conventional tabletop therapy after chronic stroke. Am J Phys Med Rehabil 2012; 91:S232–S241. 10.1097/PHM.0b013e31826bce79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sale P, Franceschini M, Mazzoleni S, Palma E, Agosti M, Posteraro F. Effects of upper limb robot-assisted therapy on motor recovery in subacute stroke patients. J Neuroeng Rehabil 2014; 11:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sale P, Mazzoleni S, Lombardi V, Galafate D, Massimiani MP, Posteraro F, et al. Recovery of hand function with robot-assisted therapy in acute stroke patients: a randomized-controlled trial. Int J Rehabil Res 2014; 37:236–242. 10.1097/MRR.0000000000000059 [DOI] [PubMed] [Google Scholar]
- 52.Susanto EA, Tong RKY, Ockenfeld C, Ho NSK. Efficacy of robot-assisted fingers training in chronic stroke survivors: a pilot randomized-controlled trial. J Neuroeng Rehabil 2015; 12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Timmermans A, Lemmens R, Monfrance M, Geers RP, Bakx W, Smeets RJ, et al. Effects of task-oriented robot training on arm function, activity, and quality of life in chronic stroke patients: a randomized controlled trial. J Neuroeng Rehabil 2014; 11:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Volpe BT, Krebs HI, Hogan N, Edelsteinn L, Diels CM, Aisen ML. Robot training enhanced motor outcome in patients with stroke maintained over 3 years. Neurology 1999; 53:1874–1876. [DOI] [PubMed] [Google Scholar]
- 55.Volpe BT, Lynch D, Rykman-Berland A, Ferraro M, Galgano M, Hogan N, et al. Intensive sensorimotor arm training mediated by therapist or robot improves hemiparesis in patients with chronic stroke. Neurorehabil Neural Repair 2008; 22:305–310. 10.1177/1545968307311102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu G, Song A, Pan L, Li H, Liang Z, Zhu S, et al. Adaptive hierarchical control for the muscle strength training of stroke survivors in robot-aided upper-limb rehabilitation. Int J Adv Robotic Sy 2012; 9:1–12. [Google Scholar]
- 57.Xu G, Song A, Pan L, Gao X, Liang Z, Li F, et al. Clinical experimental research on adaptive robot-aided therapy control methods for upper-limb rehabilitation. Robotica 2014; 32:1081–1100. [Google Scholar]
- 58.Yoo DH, Cha YJ, Kim SK, Lee JS. Effect of three-dimensional robot-assisted therapy on upper limb function of patients with stroke. J Phys Ther Sci 2013; 25:407–409. [Google Scholar]
- 59.Broeks JG, Lankhorst GJ, Rumping K, Prevo AJ. The long-term outcome of arm function after stroke: results of a follow-up study. Disabil Rehabil 1999; 21:357–364. [DOI] [PubMed] [Google Scholar]
- 60.Lohse KR, Lang CE, Boyd LA. Is more better? Using meta-data to explore dose-response relationships in stroke rehabilitation. Stroke 2014; 45:2053–2058. 10.1161/STROKEAHA.114.004695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hayward KS, Brauer SG. Dose of arm activity training during acute and subacute rehabilitation post stroke: a systematic review of the literature. Clin Rehabil 2015; 29:1234–1243. 10.1177/0269215514565395 [DOI] [PubMed] [Google Scholar]
- 62.Kwakkel G. Intensity of practice after stroke: more is better. Schweiz Arch Neurol Psychiatr 2009; 160:295–298. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
RT = Robot-assisted therapy; OI = other intervention.
(EPS)
RT = Robot-assisted therapy; RT add = additional effect of Robot-assisted therapy; OI = other intervention.
(EPS)
RT = Robot-assisted therapy; OI = other intervention; ROM = range of motion.
(EPS)
(EPS)
Y = yes; N = no.
(DOC)
(DOC)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.