Abstract
Background The palatine neurovascular bundle is at risk during endoscopic surgery. Injury may result in significant blood loss and anesthesia of the ipsilateral hard palate. Nonetheless, its endoscopic anatomy has not been described previously. This article strives to establish landmarks to identify the greater palatine canal; thus, avoiding injury to its contents.
Methodology This study comprised 50 deidentified computed tomographic angiograms using landmarks that are immediately visible during endoscopic medial maxillectomy to calculate: the angle of the greater palatine canal to the vertical, the distance from the anteroinferior aspect of the greater palatine canal to the orifice of the nasolacrimal duct, the distance from the anteroinferior aspect of the greater palatine canal to the posterolateral free edge of the hard palate, and the distance from the anterior aspect of the greater palatine canal as it enters the hard palate to the posterior wall of the maxillary sinus.
Results The mean angle of the greater palatine canal to the vertical was 23.01 degrees. The mean distance from the anteroinferior aspect of the greater palatine canal to the nasolacrimal duct was 31.52 mm. The mean distance from the anterior aspect of the greater palatine canal to the posterolateral free edge of the hard palate was 7.71 mm and the mean distance from the anterior aspect of the greater palatine canal to the posterior wall of the maxillary sinus was 7.07 mm.
Conclusion Accessible anatomical landmarks help ascertain the location of the greater palatine canal intraoperatively; thus, avoiding injury to its contents.
Keywords: anatomy, epistaxis, nasal, sinus, skull base
Introduction
The greater palatine artery and greater and lesser palatine nerves are at risk of injury during endoscopic medial maxillectomy, when extending a middle meatal antrostomy posteriorly, or when dissecting the posterior wall of the maxillary sinus to enter the pterygopalatine fossa. Injuring the greater palatine artery produces bleeding that may be difficult to control; thus, it has the potential to result in significant blood loss. Its injury may even lead to a pseudoaneurysm postoperatively, posing a serious risk to the patient. Furthermore, the injury itself, or attempts to arrest the hemorrhage caused from arterial damage, may also result in injury to the palatine nerves resulting in hypesthesia or anesthesia of the ipsilateral hard palate.
Previous reports in the maxillofacial literature have described the anatomy of the greater palatine canal in relation to oral structures. 1 2 3 4 5 However, the endoscopic anatomy of the greater palatine canal has not been well characterized. The aim of this study is to present endoscopic landmarks that could help endonasal surgeons in identifying the greater palatine canal; thus, avoiding its inadvertent injury.
Materials and Methods
The study comprised deidentified computed tomographic (CT) angiograms demonstrating no sinonasal pathology. Anatomic landmarks that are accessible during endoscopic surgery were selected for the measurements, which were calculated using OsiriX medical imaging software (Pixmeo, Switzerland). Measurements of the following parameters were included:
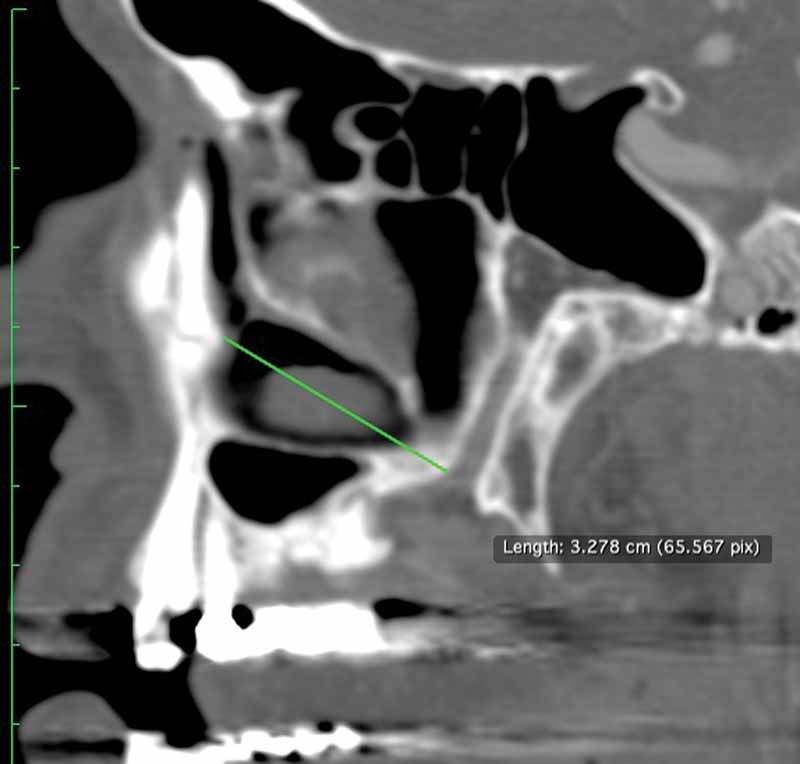
Angle of the greater palatine canal to the vertical ( Fig. 1 )
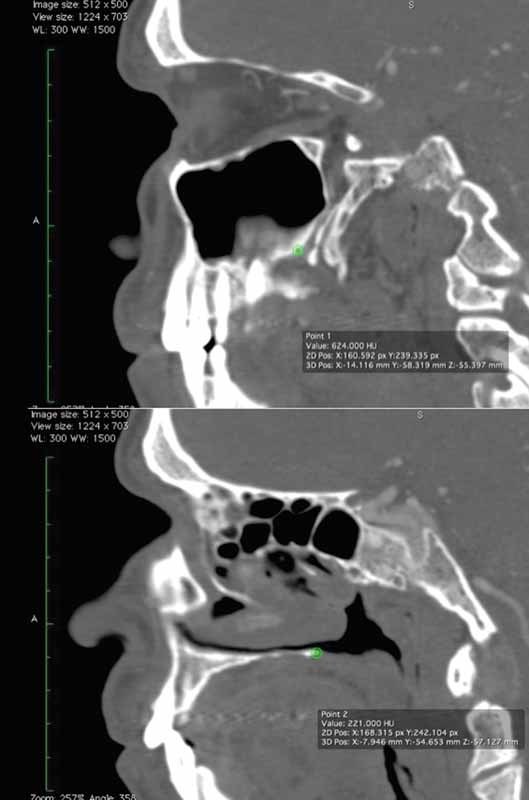
Distance from the anteroinferior aspect of the greater palatine canal to the anteroinferior aspect of the orifice of the nasolacrimal duct ( Fig. 2 )
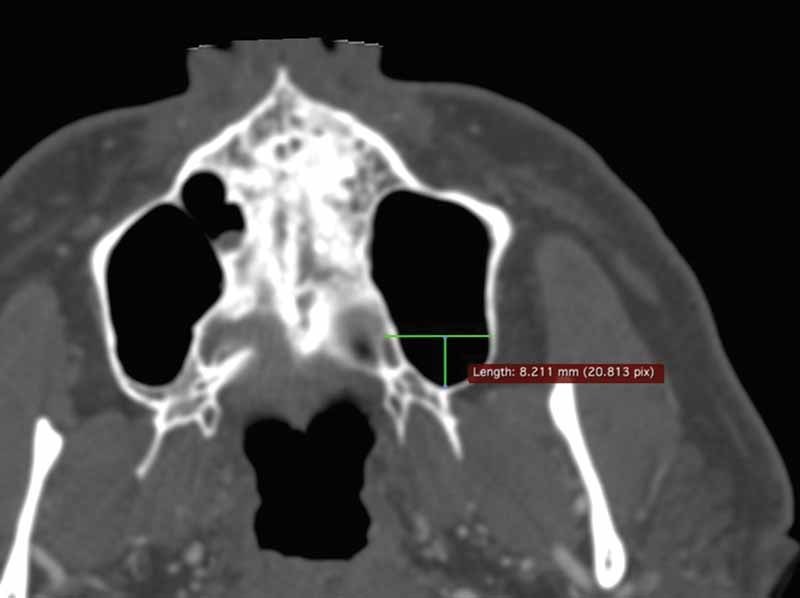
Distance from the anteroinferior aspect of the greater palatine canal to the posterolateral free edge of the hard palate ( Fig. 3 )
Distance from the anterior aspect of the greater palatine canal as it enters the hard palate to the posterior wall of the maxillary sinus ( Fig. 4 ).
Fig. 1.

Angle of the greater palatine canal to the vertical.
Fig. 2.
Distance from the anteroinferior aspect of the greater palatine canal to the orifice of the nasolacrimal duct.
Fig. 3.
Distance from the anteroinferior aspect of the greater palatine canal to the posterolateral free edge of the hard palate.
Fig. 4.
Distance from the anterior aspect of the greater palatine canal as it enters the hard palate to the posterior wall of the maxillary sinus.
Simple length measurement was performed on landmarks that were located in the same plane. However, the majority of measurement points were located in different planes; thus, requiring the plotting of individual points, which supplied three-dimensional coordinates. An extension of the Pythagorean theorem was then used to mathematically calculate the distance between the two points. When measuring the angle of the greater palatine canal to the vertical, the palate was used as a reliable landmark of the horizontal plane. To ensure reliable delineation of the vertical, sagittal CT angiograms were rotated until the palate was horizontal prior to locating the greater palatine canal for measurement. The most inferior portion of the greater palatine canal was chosen as this is the most anterior part of the canal, and therefore, the segment most at risk of injury.
The differences between right and left sides were analyzed by one-way analysis of variance using Excel software (Microsoft for Mac version 14.1.2). All measurements are presented as mean ± standard deviation and statistical significance was set at p < 0.05. Calculations were made using a Student's t -distribution with 5 degrees of freedom.
Results
Fifty CT scans (100 sides) were analyzed. The mean angle of the greater palatine canal to the vertical was 23.01 degrees (95% confidence interval [CI]: 21.79–24.23 degrees, range: 5–44 degrees). The mean distance from the most anterior and inferior aspect of the greater palatine canal to the anteroinferior orifice of the nasolacrimal duct was 31.52 mm (95% CI: 30.96–32.08 mm, range: 20.07–38.33 mm). Injury to the greater palatine canal would be avoided in 97.5% of specimens if dissection does not extend > 30.96 mm posterior to the anteroinferior edge of the nasolacrimal duct. The mean distance from the anterior aspect of the greater palatine canal to the posterolateral free edge of the hard palate was 7.71 mm (95% CI: 7.36–8.05 mm, range: 3.31–12.65 mm). Injury to the greater palatine canal would be avoided in 97.5% of specimens if the dissection proceeds at a distance ≥ 8.05 mm anterior to the posterior free edge of the hard palate. The mean distance from the anterior aspect of the greater palatine canal to the posterior wall of the maxillary sinus was 7.07 mm (95% CI: 6.71–7.42 mm, range: 3.12–11.62 mm). Injury to the greater palatine canal would be avoided in 97.5% of specimens if the dissection proceeds at a minimum distance of 7.42 mm anterior to the posterior maxillary sinus wall. There was no significant difference between right and left sides ( Tables 1 and 2 ).
Table 1. Values (distances and angles) relative to the greater palatine canal.
| Landmarks | Mean distance ± SD (mm) | 95% CI range (mm) |
|---|---|---|
| Anterior inferior NLD to anterior GP canal | 31.52 ± 2.86 | 30.96–32.08 |
| Anterior GP canal to posterior hard palate | 7.71 ± 1.76 | 7.36–8.05 |
| Anterior GP canal to posterior wall of maxillary sinus | 7.07 ± 1.79 | 6.71–7.42 |
| Landmarks | Mean angle ± SD (deg) | 95% CI range (deg) |
| Angle GP canal to vertical (degrees) | 23.01 ± 6.20 | 21.79–24.23 |
Abbreviations: CI, confidence interval; GP, greater palatine; NLD, nasolacrimal duct; SD, standard deviation.
Table 2. Nasal landmark distance analysis: presented as mean ± standard deviation.
| Landmarks | Right (mm) | Left (mm) | Total (mm) | p -Value |
|---|---|---|---|---|
| GP canal to posterior hard palate | 7.70 ± 1.74 | 7.72 ± 1.80 | 7.71 ± 1.76 | 0.96 |
| NLD to GP canal | 31.63 ± 2.59 | 31.42 ± 3.13 | 31.52 ± 2.86 | 0.72 |
| GP canal to posterior wall of maxillary sinus | 7.22 ± 1.59 | 7.63 ± 1.72 | 7.07 ± 1.79 | 0.40 |
| Landmarks | Mean angle ± SD (deg) | Mean angle ± SD (deg) | Total mean angle (deg) | p -Value |
| Angle of GP canal to vertical plane | 23.06 ± 5.42 | 22.96 ± 6.95 | 23.01 ± 6.20 | 0.94 |
Abbreviations: GP, greater palatine; NLD, nasolacrimal duct; SD, standard deviation.
Discussion
The greater palatine artery branches from the third segment of the maxillary artery within the pterygopalatine fossa. It descends, anterior to the accompanying greater palatine nerve, into the greater palatine canal in the perpendicular plate of the palatine bone, traveling for approximately 10 mm in an anterior, inferior, and slightly medial direction. 3 The medial wall of the greater palatine canal is thinnest in the region of the posterior portion of the inferior turbinate overlying the canal. 6 Therefore, this area is a potential site of injury, especially during a medial maxillectomy when the inferior turbinate has been removed. The greater palatine artery and nerve emerge in the oral cavity via the greater palatine foramen, just anterior to the posterior border of the hard palate, adjacent to the second or third molar. 7 The greater palatine artery then travels anteriorly, lateral to the greater palatine nerve, along the hard palate to enter the incisive foramen; thus, supplying the posterior two-thirds of the hard palate. 2 8
Despite the widespread use of intraoperative image guidance, surgical landmarks remain as the preferred method to identify anatomical structures within a surgical field. Intraoperative image guidance systems have inherent margins of error, their accuracy may degrade during surgery, they may suffer electronic malfunction, they are not necessary for all operations or may not be available altogether; therefore, despite their usefulness, one cannot and should not rely completely on these devices. The chosen anatomical landmarks, namely, the nasolacrimal duct, the posterior edge of the hard palate, and the posterior wall of the maxillary sinus, are immediately visible or may be easily exposed during endoscopic sinonasal or skull base surgery. This is particularly the case when anatomy is grossly abnormal or difficult to determine due to tumors or other destructive lesions. The nasolacrimal duct is often identified during a prelacrimal approach, endoscopic Denker's or Sturman–Canfield's approach or a modified endoscopic Denker's approach (preserving the ascending process of the maxilla/pyriform aperture). Therefore, it may be of use as a landmark when using these approaches to access a tumor that involves both the pterygopalatine and infratemporal fossae, for example.
Therefore, prior to extending the opening of the maxillary sinus ostium posteriorly or prior to removing the posterior wall of the maxillary sinus, these landmarks may be used to ascertain the likely location of the greater palatine canal and to avoid injury to its contents. These measurements will allow the greater palatine canal to be identified and its contents exposed, if necessary. If indicated, the contents can then be clipped or ligated prior to further dissection into the pterygopalatine fossa and beyond.
From a practical standpoint, based on these mean values, rounding to clinically useful numbers and factoring in a margin of safety that considers the extremes of range, this study suggests that the endoscopic surgeon should dissect with caution when within a distance of < 10 mm anterior to the posteroinferior wall of the maxillary sinus during a medial maxillectomy or mega-antrostomy, when dissecting > 30 mm posterior to the inferior nasolacrimal orifice and within a distance of < 10 mm anterior to the posterolateral free edge of the hard palate ( Fig. 5 ). These recommendations were chosen with a conservative margin that considered the extremes of range noted in our results. An instrument with a known diameter (such as the 5 mm burr of a drill) may be used to estimate these distances during endoscopic dissection. Careful dissection within these limits should permit the surgeon to identify the greater palatine canal and manage its contents accordingly prior to continuing the dissection. In addition, surgeons should be cautious during manipulation of the posterior aspect of the inferior turbinate to avoid injury to the greater palatine canal in the area where it is thinnest.
Fig. 5.
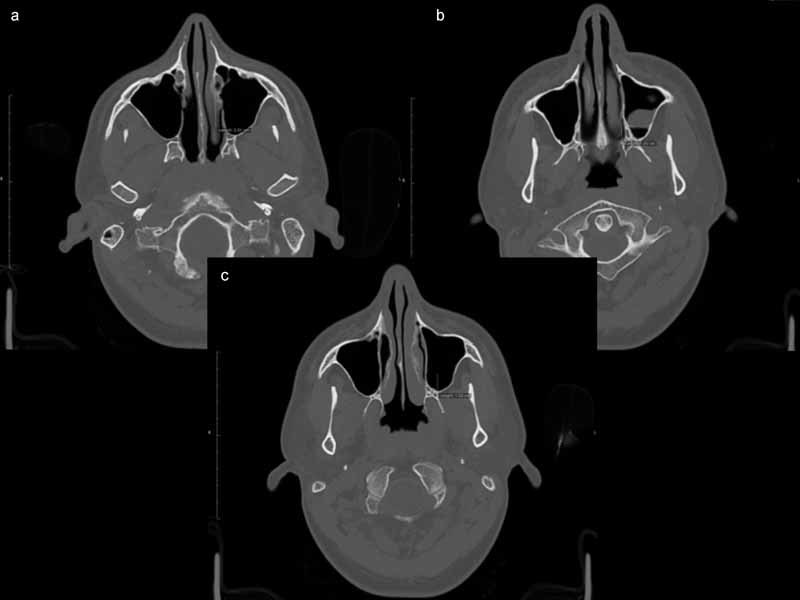
Recommended limitations of dissection: (a) not > 30 mm from the anteroinferior aspect of the nasolacrimal duct, (b) not < 10 mm anterior to the posterolateral free edge of the hard palate, and (c) 10 mm anterior to the posterior wall of the maxillary sinus.
Conclusion
This is the first article to provide endoscopic landmarks, which may be used in the intraoperative identification of the greater palatine canal. These landmarks may assist the endoscopic surgeon in avoiding inadvertent arterial or neural injury.
Acknowledgments
Financial support was provided by the Anatomy Laboratory Toward Visuospatial Surgical Innovations in Otolaryngology and Neurosurgery ( ALT-VISION ) at the Wexner Medical Center at OSU. The laboratory is self-funded by the tuition of hands-on courses.
Conflict of Interest None.
Authors' Contribution
Raewyn G. Campbell: preparation of article, statistical analysis, and literature review. Eric C. Mason: collection of data and statistical analysis. Ricardo L. Carrau, Daniel M. Prevedello, and C. Arturo Solares: review of article.
Financial Disclosure
None.
Level of Evidence/Type of Article
This study is a Level 4/case series.
References
- 1.Yu S K, Lee M H, Park B S, Jeon Y H, Chung Y Y, Kim H J. Topographical relationship of the greater palatine artery and the palatal spine. Significance for periodontal surgery. J Clin Periodontol. 2014;41(09):908–913. doi: 10.1111/jcpe.12288. [DOI] [PubMed] [Google Scholar]
- 2.Kim D H, Won S Y, Bae J H et al. Topography of the greater palatine artery and the palatal vault for various types of periodontal plastic surgery. Clin Anat. 2014;27(04):578–584. doi: 10.1002/ca.22252. [DOI] [PubMed] [Google Scholar]
- 3.Li K K, Meara J G, Alexander A., JrLocation of the descending palatine artery in relation to the Le Fort I osteotomy J Oral Maxillofac Surg 19965407822–825., discussion 826–827 [DOI] [PubMed] [Google Scholar]
- 4.Klosek S K, Rungruang T. Anatomical study of the greater palatine artery and related structures of the palatal vault: considerations for palate as the subepithelial connective tissue graft donor site. Surg Radiol Anat. 2009;31(04):245–250. doi: 10.1007/s00276-008-0432-4. [DOI] [PubMed] [Google Scholar]
- 5.Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Okabe K, Yamamoto E. Determining the anatomy of the descending palatine artery and pterygoid plates with computed tomography in Class III patients. J Craniomaxillofac Surg. 2009;37(08):469–473. doi: 10.1016/j.jcms.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 6.Mellema J W, Tami T A. An endoscopic study of the greater palatine nerve. Am J Rhinol. 2004;18(02):99–103. [PubMed] [Google Scholar]
- 7.Regan B O, Bharadwaj G. The identification and protection of the descending palatine artery in Le Fort I osteotomy: a forgotten technique? Br J Oral Maxillofac Surg. 2007;45(05):412–414. doi: 10.1016/j.bjoms.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 8.McMinn R MH, ed.Last's Anatomy: Regional and Applied, 9th ed Edinburgh: Churchill Livingstone; 1994 [Google Scholar]


