Abstract
The current study aimed to assess the secular trends in overweight and obesity status and high blood pressure in Chinese children and adolescents over two decades. Data on 943,128 participants aged 7-17 years were obtained from the Chinese National Survey on Students’ Constitution and Health from 1995 to 2014. The population attributable risk of overweight status for high blood pressure was calculated. The prevalence of overweight increased from 4.3% in 1995 to 18.4% in 2014, while high blood pressure prevalence fluctuated in the range of 4.4% to 6.4% during the same time period, lowest in 2005. Within each survey year, blood pressure levels and high blood pressure prevalence increased with higher body mass index. Notably, the population attributable risk of high blood pressure due to being overweight steadily increased from 6.3% in 1995 to 19.2% in 2014. The same trends of linear growth for obesity, fluctuating blood pressure and its sustained increasing population attributable risk for overweight also occurred among the domestic 29 provinces. Despite dramatic increases in overweight prevalence among Chinese children from 1995 to 2014, the high blood pressure prevalence remained relatively stable, suggesting that other independent factors are affecting high blood pressure trends to a greater extent. Yet, overtime, the magnitude of the impact of being overweight or obese on high blood pressure increased sharply, predicting looming heavy burden of high blood pressure. Reductions in overweight status may aid in preventing high blood pressure so as to prevent coronary risk in adulthood.
Keywords: High Blood pressure, Overweight, Obesity, Trends, Children
Introduction
Hypertension or high blood pressure (HBP) has been a well-recognized important risk factor for cardiovascular disease among adults for nearly 60 years, causing a significant global disease burden, especially in Asia.1–3 Although HBP once was considered a rare disease in children, it is now actually a major public health problem worldwide.4 In addition, studies have revealed that HBP in childhood can be progressive into adulthood and is the strongest predictor of HBP in adulthood.5,6 HBP in childhood also carries an increased risk of organ damage, such as coronary artery calcifications, ventricular hypertrophy and increased carotid intima-media thickness.7,8 Therefore, it is important to identify and treat HBP timely in childhood.
Increasing evidence in recent years has supported that overweight status may be a causal factor for HBP, with the prevalence of HBP ranging from 19% to 22% in obese children, relative to 4% to 6% in normal weight children,9,10 which are pressing health concerns in China and the world. While an extensive literature has documented the increase in overweight and obesity, few data of population-based regular surveillances are available to analyze the HBP trends in children and adolescents. Considering the high prevalence and rapid increase in childhood obesity and its strong connection with HBP, it is generally believed that, the dramatic epidemic of excess body weight over the past several decades, including overweight and obesity, is expected to lead to a parallel rise in HBP in children.11 However, it was not the case in many studies, which argued that trends in HBP in children are not necessarily accompanied by rises in excess body weight.12–15 Chiolero et al.16 found that the worldwide epidemic of overweight and obesity in children has not resulted in a commensurate increase in BP levels in children. Many countries even witnessed downward trends in HBP despite the concomitant epidemic of overweight and obesity in youth, such as Seychelles,17 South Korea,18 Japan,13 and Iran.19 For example, an increase in the prevalence of obesity among children in Seychelles from 5.5% in 1998 to 8.5% in 2006 was accompanied by a mean 3 mm Hg decrease in systolic BP levels.17 Similar evidence from the United States indicated that mean BP levels as well as the prevalence of HBP among children have declined during the past decade,20 despite increasing levels of childhood obesity.
Limited large epidemiologic studies in China are available to examine the trends in HBP with the concomitant epidemic of overweight and obesity in youth during the past two decades. The current study analyzed data on BP in children and adolescents from five large national successive cross-sectional surveys conducted in China to establish how recent increasing trends in overweight status have affected BP and its components in children over time. We aimed to 1) describe the BP levels and HBP prevalence among Chinese children and adolescents from 1995 to 2014; 2) determine whether increases in BMI are related to increases in HBP over time; and 3) calculate and examine secular change in the magnitude of the population attributable risk (PAR) of childhood HBP due to overweight and obesity.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study design and subjects
Data were drawn from five large national successive cross-sectional surveys from the 1995, 2000, 2005, 2010 and 2014 cycles of the Chinese National Survey on Students’ Constitution and Health (CNSSCH) with design to investigate health status in Chinese school-aged children, which adhered to the principles of the Declaration of Helsinki and the Code of Federal Regulations. The surveys were approved by the Medical Research Ethics Committee of the Peking University Health Science Center (IRB00001052-18002). Informed consent was obtained from both children and their parents. The procedures of CNSSCH have been published previously and did not change over the 20-year period.21 In brief, all participants were selected by stratified cluster sampling; that is, sampling took place in classes selected randomly from each grade in the selected schools. Sampling yielded equal numbers at 3 socioeconomic status groups (i.e., upper, moderate, low) at the regional level defined by regional gross domestic product, total yearly income per capita, average food consumption per capita, natural growth rate of population, and the regional social welfare index. The present study only included data from the Han children aged 7 to 17 years, so as to eliminate the influence of ethnic groups on research.
Data were from 29 mainland provinces excluding Tibet, Chongqing, Hong Kong, Macao and Taiwan. In Tibet, the Han ethnicity is in the minority. Chongqing was set up after 1995. The data in Hong Kong, Macao and Taiwan were not available because CNSSCH did not cover these regions. A total of 7,720 observations (0.8%) were removed because of missing data or extreme height, weight and/or BP values (>5 SDs of sex- and age-specific mean from the every survey year), leaving 943,128 observations for analysis.
Measurements
Participants in the five CNSSCH surveys underwent a complete anthropometric evaluation according to the same protocol at all survey sites. Height (cm), weight (kg), and BP (mmHg) were measured by a team of trained technicians following a standardized procedure. Height and weight was measured to the nearest 0.1 cm and 0.1 kg with a portable wall-mounted stadiometer and standardized scale using the mean values of three measurements. Both the stadiometers and scales were calibrated before use. Body mass index (BMI) was calculated as body weight (kg) divided by height (m) squared (kg/m2). Different BMI groups including thinness, normal, overweight, and obesity were defined using the International Obesity Task Force (IOTF) definition. 22,23
BP was measured according to the recommendation of the National High Blood Pressure Education Program (NHBPEP) Working Group 24 in Children and Adolescents, using an auscultation mercury sphygmomanometer. An appropriate cuff for children with an inflatable bladder width that is at least 40% of the arm circumference at a point midway was used, and the cuff bladder length covered 80% to 100% of the circumference of the arm. The cuff was placed ≈2 cm above the crease of the right arm elbow. BP was measured at the first reading after children sat for at least 10 minutes. The feet of children were placed on a platform during BP measurement. SBP was determined by onset of the first “tapping” Korotkoff sound (K1), and DBP was determined by the fifth Korotkoff sound (K5). An average of three BP measurements at a single visit was calculated for each child. Systolic HBP (SHBP) and diastolic HBP (DHBP) were defined as systolic and diastolic BP ⩾ the referent age-, sex- and height-specific 95th centile respectively according to the NHBPEP reference. HBP was defined as SHBP or/and DHBP of children. BP Z-Scores were calculated by using formulas in the NHBPEP reference.24
Statistical analyses
Descriptive statistics were calculated for all variables. For analysis of the trends in levels of BP (SBP and DBP) and BP Z-Scores (SBP Z-Score and DBP Z-Score), multivariate linear regression models that included survey year as the categorical predictor were used. We calculated the OR and 95% confidence intervals (95% CIs) of HBP, SHBP and DHBP in thinness, overweight and obesity groups compared to the normal group in five surveys form 1995 to 2014. Because age, height, province, urban/rural area, and socioeconomic status may influence the trends of BP levels, and BP Z-Scores in different BMI category groups, we adjusted for all of these characteristics in the model when trends were assessed. A logistic regression model using the aflogit module for Stata was adopted to estimate the PAR (%) with corresponding 95% confidence intervals (95% CIs) based on asymptotic approximations.25 Calculation of PAR (%) implies a theoretical causal relationship between overweight/obesity and HBP. We also used PAR (%) to estimate intervention effects on HBP if overweight and obesity were averted in children and adolescents theoretically.26 Finally, subgroup analysis was run for each of China’s domestic 29 provinces to confirm the overall results in our study. All analyses were performed with Stata V.15 software (College Station, TX, USA).
Result
The characteristics of the study population in both sexes aged 7- 17 years in five surveys are shown in Table 1. There was no difference in mean age of study participants, but obvious increases in height, weight and BMI from 1995 to 2014. The SBP levels in both sexes decreased from 1995 to 2005 and increased from 2005 to 2014. The DBP levels in both sexes fluctuated in five surveys from 1995 to 2014.
Table1.
Descriptive characteristics of Chinese children and adolescents aged 7-17 years participating in CNSSCH from 1995 to 2014
| Year | n | Age, y | Height, cm | Weight, kg | BMI | SBP, mm Hg | DBP, mm Hg |
|---|---|---|---|---|---|---|---|
| Boys | |||||||
| 1995 | 92513 | 12.1±3.1 | 148.4±17.8 | 39.4±13.9 | 17.2±2.7 | 104.7±12.5 | 62.6±10.6 |
| 2000 | 92623 | 12.0±3.2 | 149.2±18.0 | 40.7±14.7 | 17.6±2.9 | 104.3±12.0 | 65.0±9.2 |
| 2005 | 100410 | 12.0±3.2 | 150.5±17.7 | 42.2±14.8 | 18.0±3.0 | 103.6±12.2 | 63.9±9.4 |
| 2010 | 92228 | 12.0±3.2 | 151.7±17.6 | 43.7±15.2 | 18.3±3.2 | 105.3±12.4 | 65.1±9.4 |
| 2014 | 91037 | 12.1±3.2 | 153.1±17.4 | 45.6±15.7 | 18.8±3.3 | 105.7±12.9 | 65.6±9.4 |
| Girls | |||||||
| 1995 | 91806 | 12.0±3.1 | 145.0±14.4 | 37.4±11.9 | 17.3±2.9 | 102.8±11.2 | 62.4±9.9 |
| 2000 | 93570 | 12.0±3.2 | 145.6±14.4 | 38.2±12.1 | 17.5±3.0 | 101.9±10.6 | 64.5±8.8 |
| 2005 | 101079 | 12.0±3.2 | 146.5±14.1 | 39.2±12.2 | 17.8±3.0 | 100.5±10.9 | 63.1±9.1 |
| 2010 | 94206 | 12.0±3.2 | 147.4±13.9 | 40.2±12.3 | 18.0±3.1 | 101.9±11.1 | 64.2±8.8 |
| 2014 | 93656 | 12.0±3.2 | 148.6±13.7 | 41.7±12.7 | 18.4±3.2 | 102.2±11.4 | 64.6±8.9 |
Note: BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure.
As presented in Figure 1, in both sexes, overweight and obesity increased linearly overtime whereas, the prevalence of HBP, SHBP, and DHBP fluctuated from 1995 to 2014 with a bottom in 2005. Specifically, the prevalence of overweight and obesity steadily increased form 3.8% to 14.3% and 0.6% to 4.1% between 1995 and 2014, respectively, which were 3.8- and 6.8-fold greater in 2014 than in 1995. In contrast, the prevalence of HBP fluctuated around 4.3% to 6.1% between 1995 and 2014, and the highest and lowest prevalence was shown in 2010 and 2005, respectively. As a whole, the prevalence of HBP steadily declined from 1995 to 2005, but increased from 2005 to 2014. Similar patterns were found for both sexes in the prevalence of SHBP and DHBP (Table S1).
Figure 1.
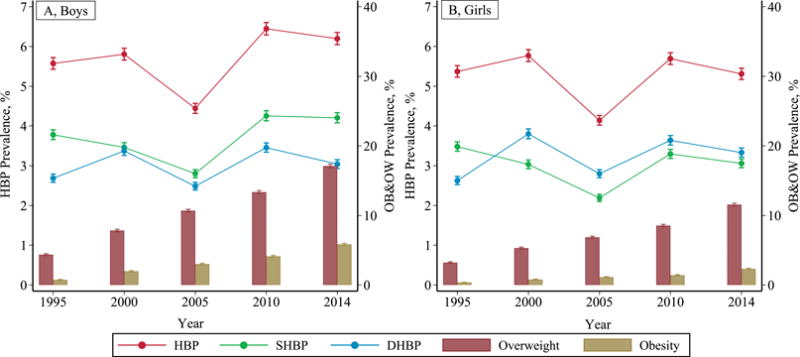
Trends in the prevalence of HBP, SHBP, DHBP, and OB&OW in Chinese boys and girls aged 7-17 years from 1995 to 2014.
After additional controlling for confounders, the change trends in SBP and DBP levels in both sexes for the four BMI groups from 1995 to 2014 are shown in Figure 2. SBP and DBP levels in both sexes increased along with BMI groups at each survey year, and fluctuated over time within the BMI groups from 1995 to 2014. For example, SBP levels for the four BMI groups in 2014 ranged from 102.1 mm Hg to 112.5 mm Hg in boys and 99.4 mm Hg to 109.7 mm Hg in girls. In the obesity group, SBP and DBP were at the highest level and the trends were relatively flat over time for both sexes. In the other three BMI groups, the secular trends of SBP and DBP over time were turbulent.
Figure 2.
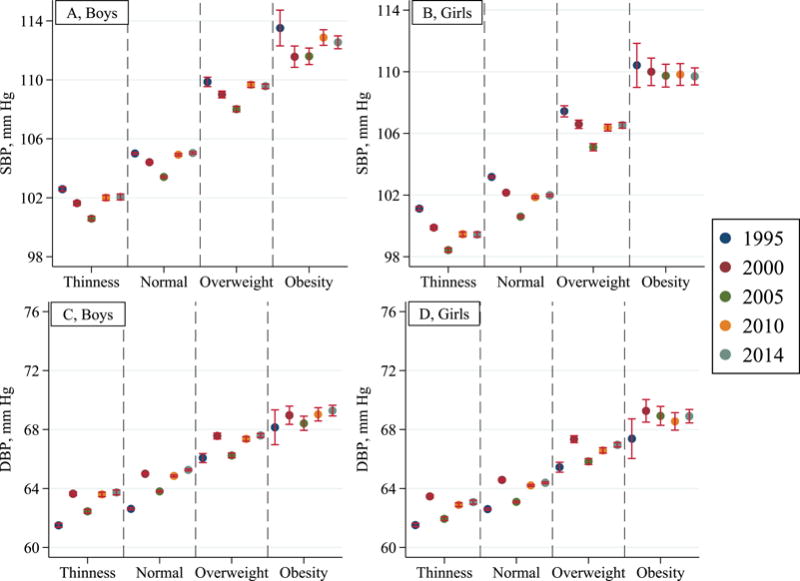
Trends in average SBP and DBP levels in different BMI groups in Chinese boys and girls aged 7-17 years from 1995 to 2014.
There was a sustained decline for SBP in the thin, normal and overweight groups from 1995 to 2005 in both sexes and an increase later from 2010 to 2014. A different pattern was shown for both sexes in DBP levels with sustained increased trends detected from 1995 to 2014, except 2000 (Table S2). After additional controlling for confounders, similar trends for SBP and DBP Z-Scores were observed (Figure S1 and Table S2). As shown in Figure 3, the prevalence of HBP, SHBP and DHBP in both sexes increased along with BMI groups in every survey, and fluctuated over time within the BMI groups from 1995 to 2014.
Figure 3.
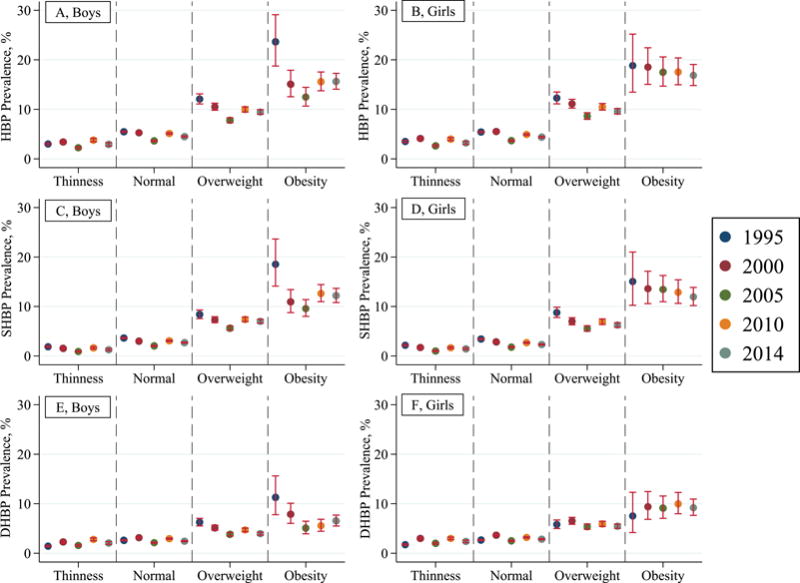
Trends in the prevalence of HBP, SHBP and DHBP for different BMI groups in Chinese boys and girls aged 7-17 years from 1995 to 2014.
In the obesity group, the prevalence of HBP, SHBP and DHBP was the highest in five surveys in both sexes compared to the other three groups. In the thin and normal BMI group, the prevalence of HBP, SHBP and DHBP did not change significantly over time. In the overweight and obesity groups, there was a sustained decline in HBP for boys form 1995 to 2005 and then an increase from 2010 to 2014, while in the obesity group for girls, no real changes in HBP, SHBP and DHBP prevalence were observed over time (Table S3). The association analysis presented the same trends from 1995 to 21014 (Figure S2).
Table 2 presents the PAR% for HBP due to overweight and obesity steadily increased from 6.3% in 1995 to 19.2% in 2014; the PAR% for SHBP and DHBP were 7.4% and 6.2% in 1995 and increased to 26.2% and 13.4% in 2014, respectively. Similar patterns for PAR% in HBP, SHBP and DHBP for overweight and obesity were observed in both sexes from 1995 to 2014. The other finding was that the PAR% for SHBP due to overweight and obesity in both sexes was always nearly twofold greater than that for DHBP.
Table 2.
PAR and 95% Confidence Intervals for HBP, SHBP and DHBP due to overweight and obesity in Chinese boys and girls aged 7-17 years from 1995 to 2014
| Variables | Boys | Girls | Total |
|---|---|---|---|
| HBP | |||
| 1995 | 7.5(6.6,8.3) | 5.3(4.5,6.0) | 6.3(5.7,6.9) |
| 2000 | 10.8(9.7,11.9) | 7.1(6.2,7.9) | 8.8(8.0,9.4) |
| 2005 | 15.9(14.5,17.4) | 11.5(10.2,12.7) | 13.5(12.5,14.5) |
| 2010 | 16.4(15.0,17.7) | 11.3(10.2,12.5) | 13.8(12.9,14.6) |
| 2014 | 22.6(20.9,24.2) | 16.1(14.7,17.5) | 19.2(18.1,20.3) |
| SHBP | |||
| 1995 | 8.3(7.2,9.4) | 6.6(5.6,7.6) | 7.4(6.6,8.2) |
| 2000 | 14.7(13.1,16.2) | 10.5(9.1,11.8) | 12.6(11.5,13.6) |
| 2005 | 22.4(20.2,24.4) | 17.8(15.8,19.8) | 20.2(18.7,21.6) |
| 2010 | 22.3(20.4,24.1) | 16.0(14.3,17.7) | 19.4(18.1,20.7) |
| 2014 | 29.5(27.4,31.6) | 22.1(20.1,24.1) | 26.2(24.7,27.6) |
| DHBP | |||
| 1995 | 8.1(6.8,9.4) | 4.6(3.5,5.7) | 6.2(5.4,7.1) |
| 2000 | 8.1(6.7,9.5) | 5.3(4.2,6.3) | 6.4(5.5,7.2) |
| 2005 | 11.7(9.8,13.6) | 9.2(7.7,10.7) | 10.0(8.8,11.2) |
| 2010 | 11.2(9.4,12.9) | 8.5(7.1,9.9) | 9.4(8.3,10.5) |
| 2014 | 15.2(13.0,17.4) | 12.6(10.8,14.3) | 13.4(12.0,14.8) |
Note: All such values are PAR% (95% confidence intervals) calculated after adjusting for age, height, province, urban/rural area, and province-level socioeconomic status.
Examined at the province level, and consistent with the overall findings, the prevalence of HBP, SHBP, and DHBP fluctuated from 1995 to 2014 despite the concomitant linear increase in pediatric overweight and obesity in every province (Figure S3). Consistently, the PAR% for HBP, SHBP and DHBP due to overweight and obesity increased dramatically in every province. For example, the PAR% for HBP in the Yunnan province increased from 8.55% in 1995 to 39.02% in 2014, and its PAR% for SHBP even surpassed 50% (Figure 4).
Figure 4.
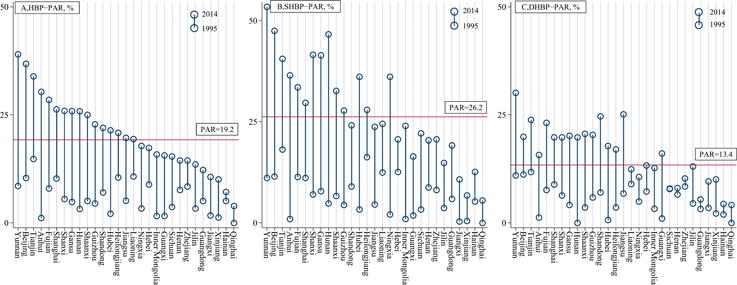
The change in PAR for HBP, SHBP and DHBP due to overweight and obesity in Chines youth by province between 1995 and 2014.
Discussion
Based on nearly a million children and adolescents aged 7 to 17 years in China during the past two decades, we found, as anticipated, large increases in BMI level and overweight and obeseity status over time. In constrast, BP levels and HBP prevalence fluctuated over time and did not show an increasing trend parallel with changes in body mass. Few large scale studies have analysed the HBP trends among children, and the findings have suggested increases, decreases, and fluctuations over time. Two studies conducted with Chinese children reported an upward trend in BP levels and HBP prevalence.27,28 One of the studies27 reported an increase in HBP between 2005 and 2010, consistent with the results of our study during this period. The other study showed an increase in HBP from 1993 to 2009, though with local and small sample sizes; the trend between these two year points was also consistent with our results between 1995 and 2010.28 Some studies witnessed downward trends in HBP during the rising youth obesity epidemic, even after adjusting for some confounding factors.17–19 For example, one study analyzing data from Seychelles’ children witnessed that the prevalence of HBP decreased from 9.8% in 2000 to 6.9% in 2004, despite marked increase in the prevalence of obesity.17 A US study found that BP levels and HBP among children have slightly declined between 1999 and 2012, after adjustment for the increase in BMI Z-Score.20 These two downward trends were also consistent with our results in the same two periods of 2000-2005 and 2000-2014. The previous investigations of secular trends in BP and BMI among children were mainly drawn from cross-sectional data collected at only two time-points, which may yield an inadequate snapshot of the true HBP trends. The study with the most similarity in findings was conducted in the US and reported on data every 10 years. The trends in childhood BP levels were downward from 1963 to 1988, and then upward from 1999 to 2002, despite sustained increases in youth obesity over time.15 As a group, the available studies support the hypothesis that HBP in children might be a fluctuating trend, which has not paralleled the rising obesity epidemic. Further, the real trends in BP levels and HBP prevalence require repeated surveillance.
Study findings indicated that PAR increased with time, while the overall prevalence did not, which suggests that other effective ‘interventions’ or events occurred, which may contribute to BP trends, such as salt intake, early life exposures, and physical inactivity. Salt intake is a risk factor for HBP and may be particularly relevant due to the high salt preference in Chinese cooking. Thus, reduced salt dietary interventions have been increasingly promoted across the country, especially in recent years.29 One national survey of Chinese adults revealed that salt intake decreased form 6.6 g/day in 1991 to 4.7 g/day in 2009, which may counteract the effect of obesity on HBP and contribute to reductions in population BP levels.30,31 Although the data on salt intake was from adults, the dietary patterns of children are largely dependent upon their parents for cooking the meals. Hence, the change in salt intake among adults over time may approximate that of children. Early life exposures, such as high birth weight, also have been associated with downward trends in BP.32,33 China witnessed an increase in mean birth weight over the last two decades:34,35 from 3,271 kg in 1996 to 3,331 kg in 2010,35 comparable to that observed in many other countries, such as the US, Canada, the United Kingdom, and India.36 Physical inactivity, a strong correlate of HBP,37 was not consistently measured in CNSSCH, though research indicates increases in sedentary behavior among Chinese children and adolescents.38,39 The discordant and intersecting effects of increased birth weight, reduced salt intake, and reduced physical activity, combined with the increase in obesity, may synchronously contribute to fluctuations in BP population trends over time. Thus, efforts should focus on controlling hypertension in youth by curbing the dramatic increase in childhood obesity and by emphasizing proven prevention and intervention strategies including lifestyle modification to reduce sodium intakes, increase physical exercise, and promote health-supporting family environments, all of which were recommended in the updated pediatric hypertension guidelines in 2017.40
Notably, we found that the contribution of overweight and obesity to HBP in Chinese children 20 years ago was relatively low, and then became stronger with time, consistent for all 29 domestic provinces in China. For example, the attribution of risk for HBP from overweight and obesity in Yunnan province increased by nearly 5 times from 8.6% to 39.0% and reached 53.4% for SHBP. Obesity has became an increasingly dominant health factor in Chinese children, and the findings suggest it will be the leading factor in HBP status in the near future. US studies reported a downward HBP trend before 1988, followed by an upward trend from 1999 to 2002, which suggested that there might be a time lag of approximately 10 years between the rise in obesity and the rise in HBP in children and adolescents.15 Although the HBP trends did not parallel with the increased trends of obesity, albeit with an average of 19.2% attributable proportion in HBP, the continued increased PAR for overweight and obesity on HBP across the country predicts an explosive epidemic of HBP in children because of the time lag. Furthermore, our results indicated the change in BP levels were flatter in obesity groups compared with other groups, which suggests that obesity remained the dominant determinant for obese children.
We also found that the PAR for overweight and obesity in the development of SHBP was more than twofold higher than for DHBP, especially in the three most recent survey points, also consistent across all 29 domestic provinces. A good deal of previous literature revealed that SHBP remained the most important cardiovascular risk indicator in adults, entitled the era of “systolic hypertension”.41 Due to the rarity of cardiovascular events caused by HBP in children, it is difficult to determine the differential effect of SHBP and DHBP on cardiovascular disease in youth. However, obesity is major risk factor for HBP in children, which may affect HBP components to different extents. In the early phase of hypertension evolving from children to young adults, the evolution of SHBP requires further attention. Thus, a potential implication of the present study is that the control of overweight and obesity is quite important to reduce the risk of HBP in children, particularly SHBP, which is more significant to reduce the onset risk of cardiovascular disease in early adulthood. This is one of the first studies examining the influence of differences in nutritional status on BP components over time in Chinese children using successive datasets over two decades.
The present study has several strengths. First, nearly a million participants of Han nationality accounting for nearly 92% of the total Chinese population were included in the five CNSSCH surveys over a 20 year period to analyze secular trends, which supports the extrapolation of our conclusions. Further, because CNSSCH adopted a consistent sampling procedure and the same examination methodology in five surveys, such as the use of mercury sphygmomanometer and cuff size, it is acceptable to achieve comparability of data in different years. Limitations of the present study should also be noted. First, BP levels in our study were obtained at a single visit, which may overestimate the HBP prevalence.42 The US pediatric BP guidelines in 2004 and 2017 recommended that clinical diagnosis of HBP needed at least 3 occasions in children and adolescents.24,40 However, the same method of BP measurements was employed in five surveys over the entire period, and therefore was unlikely to influence the secular trends in HBP. Further, we examined consistency of findings in all 29 domestic provinces and witnessed the same results. In most epidemiological studies, screening of hypertension for adults or children mainly depends on 1 to 3 readings at a single visit.43 Second, study findings indicated that the trends of hypertension in children did not correspond with the explosive epidemic of obesity, even with an ever-increasing PAR of hypertension for obesity. Yet, we cannot exclude the further progression of hypertension during adulthood following from obesity in adolescence. Needed are intensive regular surveillances and cohort studies with data into adulthood. Third, other confounders were not included in our analyses, such as individual-level socioeconomic status, which was not available for such a large-scale epidemiologic survey. We did, however, control for province-level socioeconomic status.
Perspectives
Our study revealed that BP levels and HBP prevalence in Chinese children have not paralleled the explosive increasing trends in overweight and obesity over the past 20 years. Intensive surveillance helped us draw a real picture of fluctuating BP trends in children over time during the past two decades. However, overweight and obese children consistently demonstrated a higher level of BP and greater risk of HBP in each survey. A dramatic increase in attribution of HBP by overweight and obesity status in Chinese youth was observed over time, especially for SHBP, suggesting the possibility of a future epidemic in youth HBP, which would impose considerable burdens in future cardiovascular diseases in adulthood. Routine intensive BP surveillance in other countries and additional epidemiologic studies assessing a wider range of risk or protective factors related to BP is warranted.
Supplementary Material
Novelty and Significance.
1) What’s new?
Explosive epidemic for obesity did not result in secular increase in blood pressure among Chinese children aged 7-17 years from 1995 to 2014.
Other independent factors affecting HBP trends in children might exist. But the impact of obesity on HBP increased sharply, predicting looming heavy burden of HBP in children.
2) What is relevant?
Overweight status and HBP are related. Epidemiologic studies have reported on steady increases in childhood overweight and obesity. Unstudied are the associated changes overtime with HBP in youth.
Considering the high prevalence and rapid increase in childhood obesity and its strong connection with HBP, it is generally believed that, the dramatic epidemic of excess body weight is expected to lead to a parallel rise in HBP in children.
Summary.
We assessed the secular trends in overweight and obesity status and high blood pressure in Chinese children from 1995 to 2014. We add the new findings in the present study that despite dramatic increases in overweight and obesity prevalence among Chinese children from 1995 to 2014, the high blood pressure prevalence remained relatively fluctuant during this period. Other independent factors affecting high blood pressure trends in children might exist. Even though, we still found that the impact of being overweight or obese on high blood pressure increased sharply, predicting looming heavy burden of high blood pressure in children. Our study provides evidence that intensive routine surveillance and the comprehensive prevention and intervention strategies on blood pressure, including lifestyle intervention and the control of obesity, are needed so as to maintain a healthy blood pressure levels in children.
Acknowledgments
The authors would like to acknowledge the support from all the team members and the participated students, teachers, parents and local education and health staffs in the the programs.
Funding Source: The present study was supported by the National Natural Science Foundation to Jun Ma (81673192) and China Scholarship Council to Yi Song (201606015038) and the National Heart, Lung and Blood Institute to Judith Prochaska (R01HL11773).
Footnotes
Contributors: Y. Dong and Y. Song conceptualized and designed the study; Y. Dong completed the statistical analyses, drafted the initial manuscript, and reviewed and revised the manuscript; J. Ma and Y. Song designed the study and collected the data; Y. Ma, B. Dong, Z. Zou and J.J. Prochaska assisted with the statistical analyses and critically reviewed and revised the manuscript; all authors approved the final manuscript.
Financial Disclosure: None.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Y, Wang DD, Ley SH, Howard AG, He Y, Lu Y, Danaei G, Hu FB. Potential Impact of Time Trend of Life-Style Factors on Cardiovascular Disease Burden in China. Journal of the American College of Cardiology. 2016;68:818–833. doi: 10.1016/j.jacc.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NCD. Risk Factor Collaboration. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet. 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ingelfinger JR. The child or adolescent with elevated blood pressure. The New England journal of medicine. 2014;370:2316–2325. doi: 10.1056/NEJMcp1001120. [DOI] [PubMed] [Google Scholar]
- 5.Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–3180. doi: 10.1161/CIRCULATIONAHA.107.730366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tirosh A, Afek A, Rudich A, et al. Progression of normotensive adolescents to hypertensive adults: a study of 26,980 teenagers. Hypertension. 2010;56:203–209. doi: 10.1161/HYPERTENSIONAHA.109.146415. [DOI] [PubMed] [Google Scholar]
- 7.Erlingsdottir A, Indridason OS, Thorvaldsson O, Edvardsson VO. Blood pressure in children and target-organ damage later in life. Pediatr Nephrol. 2010;25:323–328. doi: 10.1007/s00467-009-1350-3. [DOI] [PubMed] [Google Scholar]
- 8.Daniels SR, Pratt CA, Hayman LL. Reduction of risk for cardiovascular disease in children and adolescents. Circulation. 2011;124:1673–1686. doi: 10.1161/CIRCULATIONAHA.110.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwandt P, Scholze JE, Bertsch T, Liepold E, Haas GM. Blood pressure percentiles in 22,051 German children and adolescents: The PEP Family Heart Study. Am J Hypertens. 2014;28(5):672–679. doi: 10.1093/ajh/hpu208. [DOI] [PubMed] [Google Scholar]
- 10.Salvadori M, Sontrop JM, Garg AX, Truong J, Suri RS, Mahmud FH, Macnab JJ, Clark WF. Elevated blood pressure in relation to overweight and obesity among children in a rural Canadian community. Pediatrics. 2008;122:e821–827. doi: 10.1542/peds.2008-0951. [DOI] [PubMed] [Google Scholar]
- 11.Rahmouni K. Obesity-associated hypertension: recent progress in deciphering the pathogenesis. Hypertension. 2014;64:215–221. doi: 10.1161/HYPERTENSIONAHA.114.00920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freedman DS, Goodman A, Contreras OA, DasMahapatra P, Srinivasan SR, Berenson GS. Secular trends in BMI and blood pressure among children and adolescents: the Bogalusa Heart Study. Pediatrics. 2012;130:e159–166. doi: 10.1542/peds.2011-3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shirasawa T, Ochiai H, Nishimura R, Morimoto A, Shimada N, Ohtsu T, Hoshino H, Tajima N, Kokaze A. Secular trends in blood pressure among Japanese schoolchildren: a population-based annual survey from 1994 to 2010. J Epidemiol. 2012;22:448–453. doi: 10.2188/jea.JE20110137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters H, Whincup PH, Cook DG, Law C, Li L. Trends in blood pressure in 9 to 11-year-old children in the United Kingdom 1980-2008: the impact of obesity. J Hypertens. 2012;30:1708–1717. doi: 10.1097/HJH.0b013e3283562a6b. [DOI] [PubMed] [Google Scholar]
- 15.Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. doi: 10.1161/CIRCULATIONAHA.106.683243. [DOI] [PubMed] [Google Scholar]
- 16.Chiolero A, Bovet P, Paradis G, Paccaud F. Has blood pressure increased in children in response to the obesity epidemic? Pediatrics. 2007;119:544–553. doi: 10.1542/peds.2006-2136. [DOI] [PubMed] [Google Scholar]
- 17.Chiolero A, Paradis G, Madeleine G, Hanley JA, Paccaud F, Bovet P. Discordant secular trends in elevated blood pressure and obesity in children and adolescents in a rapidly developing country. Circulation. 2009;119:558–565. doi: 10.1161/CIRCULATIONAHA.108.796276. [DOI] [PubMed] [Google Scholar]
- 18.Khang YH, Lynch JW. Exploring determinants of secular decreases in childhood blood pressure and hypertension. Circulation. 2011;124:397–405. doi: 10.1161/CIRCULATIONAHA.110.014399. [DOI] [PubMed] [Google Scholar]
- 19.Hosseini F, Mousavi A, Mirmiran P, Ghanbarian A, Azizi F. Trends in risk factors for cardiovascular disease among Iranian adolescents: the Tehran Lipid and Glucose Study, 1999-2008. J Epidemiol. 2011;21:319–328. doi: 10.2188/jea.JE20100162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xi B, Zhang T, Zhang M, Liu F, Zong X, Zhao M, Wang Y. Trends in Elevated Blood Pressure Among US Children and Adolescents: 1999-2012. Am J Hypertens. 2016;29:217–225. doi: 10.1093/ajh/hpv091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ji CY, Chen TJ, Working Group on Obesity in China Empirical changes in the prevalence of overweight and obesity among Chinese students from 1985 to 2010 and corresponding preventive strategies. BES. 2013;26:1–12. doi: 10.3967/0895-3988.2013.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cole TJ, Flegal KM, Nicholls D, Jackson AA. Body mass index cut offs to define thinness in children and adolescents: international survey. BMJ. 2007;335:e194. doi: 10.1136/bmj.39238.399444.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 25.Greenland S, Drescher K. Maximum likelihood estimation of the attributable fraction from logistic models. Biometrics. 1993;49:865–872. [PubMed] [Google Scholar]
- 26.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong B, Wang HJ, Wang Z, Liu JS, Ma J. Trends in blood pressure and body mass index among Chinese children and adolescents from 2005 to 2010. Am J Hypertens. 2013;26:997–1004. doi: 10.1093/ajh/hpt050. [DOI] [PubMed] [Google Scholar]
- 28.Xi B, Liang Y, Mi J. Hypertension trends in Chinese children in the national surveys, 1993 to 2009. Int J Cardiol. 2013;165:577–579. doi: 10.1016/j.ijcard.2012.09.032. [DOI] [PubMed] [Google Scholar]
- 29.He FJ, Wu Y, Feng XX, Ma J, Ma Y, Wang H, Zhang J, Yuan J, Lin CP, Nowson C, MacGregor GA. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ. 2015;350:h770. doi: 10.1136/bmj.h770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Du S, Batis C, Wang H, Zhang B, Zhang J, Popkin BM. Understanding the patterns and trends of sodium intake, potassium intake, and sodium to potassium ratio and their effect on hypertension in China. Am J Clin Nutr. 2014;99:334–343. doi: 10.3945/ajcn.113.059121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48:861–869. doi: 10.1161/01.HYP.0000245672.27270.4a. [DOI] [PubMed] [Google Scholar]
- 32.Chiolero A, Paradis G, Kaufman JS. Assessing the possible direct effect of birth weight on childhood blood pressure: a sensitivity analysis. American journal of epidemiology. 2014;179:4–11. doi: 10.1093/aje/kwt228. [DOI] [PubMed] [Google Scholar]
- 33.Dong YH, Zou ZY, Yang ZP, Wang ZH, Jing J, Luo JY, Zhang X, Luo CY, Wang H, Zhao HP, Pan DH, Ma J. Association between high birth weight and hypertension in children and adolescents: a cross-sectional study in China. J Hum Hypertens. 2017;31:737–743. doi: 10.1038/jhh.2017.22. [DOI] [PubMed] [Google Scholar]
- 34.Dai L, Deng C, Li Y, Zhu J, Mu Y, Deng Y, Mao M, Wang Y, Li Q, Ma S, Ma X, Zhang Y. Birth weight reference percentiles for Chinese. PloS one. 2014;9:e104779. doi: 10.1371/journal.pone.0104779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shan X, Chen F, Wang W, Zhao J, Teng Y, Wu M, Teng H, Zhang X, Qi H, Liu X, Tan C, Mi J. Secular trends of low birthweight and macrosomia and related maternal factors in Beijing, China: a longitudinal trend analysis. BMC Pregnancy Childbirth. 2014;14:105–214. doi: 10.1186/1471-2393-14-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kramer MS, Morin I, Yang H, Platt RW, Usher R, McNamara H, Joseph KS, Wen SW. Why are babies getting bigger? Temporal trends in fetal growth and its determinants. The Journal of pediatrics. 2002;141:538–542. doi: 10.1067/mpd.2002.128029. [DOI] [PubMed] [Google Scholar]
- 37.Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368:299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- 38.Tian Y, Jiang C, Wang M, et al. BMI, leisure-time physical activity, and physical fitness in adults in China: results from a series of national surveys, 2000-14. Lancet Diabetes Endocrinol. 2016;4:487–497. doi: 10.1016/S2213-8587(16)00081-4. [DOI] [PubMed] [Google Scholar]
- 39.Wang C, Chen P, Zhuang J. A national survey of physical activity and sedentary behavior of Chinese city children and youth using accelerometers. Res Q Exerc Sport. 2013;84(Suppl 2):S12–28. doi: 10.1080/02701367.2013.850993. [DOI] [PubMed] [Google Scholar]
- 40.Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics. 2017;140(3) doi: 10.1542/peds.2017-1904. pii: e20171904. [DOI] [PubMed] [Google Scholar]
- 41.Lewington S, Clarke R, Qizilbash N, P R, Collins R, Prospective Studies, Collaboration Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 42.Sun J, Steffen LM, Ma C, Liang Y, Xi B. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary? Hypertension research. 2017;40:496–503. doi: 10.1038/hr.2016.179. [DOI] [PubMed] [Google Scholar]
- 43.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


