Abstract
Digital technologies hold promise for supporting the detection and management of schizophrenia. This exploratory study aimed to generate an initial understanding of whether patterns of communication about depression and anxiety on popular social media among individuals with schizophrenia are consistent with offline representations of the illness. From January to July 2016, posts on Twitter were collected from a sample of Twitter users who self-identify as having a schizophrenia spectrum disorder (n = 203) and a randomly selected sample of control users (n = 173). Frequency and timing of communication about depression and anxiety were compared between groups. In total, the groups posted n = 1,544,122 tweets and users had similar characteristics. Twitter users with schizophrenia showed significantly greater odds of tweeting about depression compared with control users (OR = 2.69; 95% CI 1.76–4.10), and significantly greater odds of tweeting about anxiety compared with control users (OR = 1.81; 95% CI 1.20–2.73). This study offers preliminary insights that Twitter users with schizophrenia may express elevated symptoms of depression and anxiety in their online posts, which is consistent with clinical characteristics of schizophrenia observed in offline settings. Social media platforms could further our understanding of schizophrenia by informing a digital phenotype and may afford new opportunities to support early illness detection.
Keywords: Schizophrenia, depression, anxiety, mental health, technology, social media, digital phenotype
Introduction
Schizophrenia is a serious mental disorder that can have devastating consequences for individuals, their families, and society [1]. Those living with schizophrenia face elevated risk of homelessness [2], high rates of substance use [3], and dramatically reduced life expectancy compared to the general population [4]. People with schizophrenia also experience poor quality of life and difficulty pursuing employment and meaningful life goals owing to debilitating symptoms of anxiety, depression and low motivation [5], as well as the impact of discrimination and societal stigma [6]. Considerable evidence shows that early and effective treatment of schizophrenia can reduce symptoms, improve social functioning and wellbeing, and contribute to better long-term outcomes [7]. However, fewer than half of individuals living with schizophrenia receive any treatment for their condition [8], a gap attributed to delays in illness detection and treatment initiation, poor access to adequate mental healthcare, limited availability of evidence-based services, and high rates of treatment discontinuation or dropout [9, 10]. It is imperative to develop innovative approaches for identifying individuals with schizophrenia and supporting early intervention and long-term engagement in treatment.
Recent research has highlighted the promise that emerging digital technologies hold for supporting the treatment and management of schizophrenia [11, 12]. For example, smartphone systems can facilitate illness management and help individuals with schizophrenia better cope with symptoms [13], and enable intensive symptom monitoring over time to detect relapse and prevent hospitalization [14]. As personal technologies, such as smartphones, wearable devices, social media, and other web applications, become an increasingly important fixture in the daily lives of individuals living with schizophrenia, there may be novel ways to leverage the way these individuals interact with these technologies in order to characterize illness symptoms and detect those at risk of relapse or adverse outcomes. The concept of examining patterns of technology use and online activity to develop a better understanding of human health and disease has been coined as the “digital phenotype” [15]. By capturing data from social media, online communities, and mobile devices, it may be possible to obtain a more comprehensive and fine-grained interpretation of the experiences of those living with schizophrenia. Such insight could inform the design and delivery of evidence-based interventions.
In this exploratory study, we were specifically interested in generating preliminary insights about how social media use among individuals with schizophrenia spectrum disorders could potentially be leveraged to inform our understanding of a digital phenotype for this patient group. To date, studies have examined how individuals with schizophrenia use social media through qualitative inquiry [16, 17], and have provided compelling evidence that people with schizophrenia use popular social media such as Facebook or Twitter at comparable rates as the general population [18, 19]. Less is known about whether patterns of social media use differ between individuals with schizophrenia and individuals from the general population, and how popular social media platforms could support early detection of schizophrenia.
Over the past few years there has been rapid growth in the number of studies that have used popular social media to examine mental health [20]. Twitter has emerged as an especially valuable platform for expanding our understanding of common mental health conditions [21]. For instance, analysis of conversations on Twitter has demonstrated utility for identifying depressive symptoms among users [22], characterizing the onset of depression [23], and detecting users’ mood and affective states [24]. Most recently, a study found that Twitter users who self-disclosed diagnoses of schizophrenia showed significant linguistic differences in their online communications when compared to a randomly selected group of control Twitter users [25]. Another recent study using Twitter characterized linguistic markers before and after users self-disclosed their diagnoses of schizophrenia online [26]. This study showed the potential therapeutic benefit of these online disclosures as reflected through changes in users’ linguistic patterns and fewer posts about symptoms following self-disclosure [26]. These preliminary studies suggest that Twitter may serve as a valuable platform for studying communication patterns among users with schizophrenia.
In the current study, our objective was to expand on these prior studies and to begin to inform a digital phenotype for schizophrenia using social media. Specifically, we aimed to determine whether patterns of communication about depression and anxiety on Twitter among individuals with schizophrenia are consistent with clinical characteristics of schizophrenia observed in offline settings. We elected to examine online conversations about depression and anxiety given the high burden and debilitating effects of these symptoms among people with schizophrenia [27,28], and because Twitter appears to serve as a valuable platform for studying these symptoms [21-24]. Therefore, there may be opportunities to detect these clinically important symptoms among this patient group by investigating conversations on popular social media platforms like Twitter. We examined frequency and timing of communications about depression and anxiety among Twitter users who self-identify as having schizophrenia compared with a randomly selected group of typical Twitter users. We considered this an important preliminary step towards generating an initial understanding of how people who self-identify as having schizophrenia potentially discuss these mental health related topics on Twitter, and whether this could inform a digital phenotype for schizophrenia. Furthermore, we adopted an exploratory approach because it is necessary to begin by validating whether patterns of communication about depression and anxiety on social media among individuals with schizophrenia are consistent with what has been observed in offline settings. With high rates of symptoms of depression and anxiety among persons with schizophrenia, we hypothesized that Twitter users who self-identify as having a schizophrenia spectrum disorder would discuss depression and anxiety more frequently than a randomly selected sample of Twitter users from the general population.
Methods
Twitter Platform
In this study, we collected data from Twitter, an online microblogging platform where individuals can post statuses called “tweets” containing 140 characters or less. We selected Twitter for this study because this platform has been successfully used to explore several health conditions including insomnia [29], infectious diseases like dengue [30], and track foodborne illness outbreaks [31]. Twitter has also demonstrated utility for identifying depression [32], monitoring attitudes about substance use [33], characterizing online discussions about tobacco use among people with schizophrenia [34], and examining psychological traits associated with health outcomes [35]. Furthermore, by early 2017, Twitter had more than 328 million active users who post more than 500 million tweets per day [36]. Twitter has been dubbed as the largest observational study of human behavior [37], and may serve as an effective avenue for identifying symptoms of depression and anxiety among people with schizophrenia.
Data collection
We retrieved data for this study from Twitter’s application programming interface (API) for a 200-day period from January 5th, 2016 to July 23rd, 2016. Ethical review was not required because we only used publicly available data in this study. For the Twitter users included in this study, we extracted the following characteristics (i.e., metadata) for their accounts: total number of tweets; tweets per day (total tweets divided by days active); tweets in last 200 days; number of friends; number of followers; favorites per day; and number of days account has been active. To measure users’ impact, we calculated a “followers-to-friends” ratio by taking a user’s number of followers and dividing by their number of friends [29]. A high ratio indicates that a user has many people who follow their account and tweets but that they follow few other users’ tweets, and has been considered an indicator of influence on Twitter [29].
Sample of Twitter Users
We identified a sample of 250 Twitter users who self-identify as having schizophrenia by searching Twitter using the following terms: “schizophrenia”; “schizoaffective”; “schizotypal”; and “psychosis”. We included only Twitter users who explicitly self-identified as having a schizophrenia spectrum disorder in their profile or in a tweet. The list was generated by one researcher and then confirmed by a second researcher. We then created a general population comparison group intended to represent typical Twitter users. This involved first using the GET statuses/sample feature from the Twitter Developers Platform to collect a random sample of all publicly available tweets [38]. Two research assistants manually looked through these tweets to confirm that the tweet belonged to a real person (i.e., not a bot or spam account), was from a normal user (i.e., not a company or corporation), and was in English. Twitter users were only included in the control sample if both research assistants were in agreement. The research assistants completed this process until a sample of 250 users was identified.
The final study sample consisted of n = 203 Twitter users with schizophrenia and n = 173 control users because some users’ accounts became inaccessible (i.e., private, deleted, banned, or deactivated) or were inactive (i.e., no posts during the 200-day study period) at the time of data collection. We then determined gender for the sample of Twitter users because there is an established association between gender and symptoms of depression or anxiety [39, 40]. Two researchers independently coded Twitter users’ gender as male, female, or unknown/insufficient data according to username, profile name, profile description, profile photo, and tweets. The researchers then reviewed the gender coding to ensure consistency and resolved disagreements through discussion and consensus.
Tweets about depression and anxiety
We collected all tweets posted during the 200-day period from Twitter users included in this study, and then searched within this body of tweets to examine differences in communication about depression and anxiety between the two groups. We identified and retrieved all tweets that contained the following keywords: “depression”, “depressed”, “anxiety”, and “anxious”. Our goal was to capture all discussions containing these specific terms among our sample of Twitter users with schizophrenia and control users. We selected these key words to increase our certainty that the Twitter users’ were explicitly referring to depression or anxiety in their conversations.
Timing of tweets about depression and anxiety
We were interested in examining potential differences in the timing of tweets about depression or anxiety between the two groups. Therefore, we determined whether Twitter users with schizophrenia discussed depression or anxiety at different times of the day compared with control users. This involved converting the time-of-day data for tweets about depression and anxiety to the Twitter users’ local time zone, and then classifying these tweets into the following time intervals: 00:00-05:59; 06:00-11:59; 12:00-17:59; and 18:00-23:59. We could only perform analysis of tweet timing on the subset of users’ tweets about depression and anxiety with available universal time code (UTC) offset data. All tweets have a UTC, but the UTC offset is only available when Twitter users choose to include their local time zone in their account settings.
Statistical analyses
We used t-tests to compare continuous variables and chi-square tests to compare categorical variables between the group of Twitter users with schizophrenia and the control users. We used logistic regression models controlling for gender to compare both groups on the binary outcomes of whether or not users posted a tweet about depression or anxiety. All tests with a p value of ≤ 0.05 were considered statistically significant. All analyses were performed with the Python Programming Language and Stata version 14.0.
Results
Characteristics of Twitter users
During the 200-day study period from January 2016 to July 2016, we collected a total of 1,544,122 tweets, with 819,491 tweets posted by the Twitter users with schizophrenia (n = 203) and 724,631 tweets posted by the control users (n = 173). Characteristics between the two groups were generally similar. Twitter users with schizophrenia posted a comparable number of tweets per day (mean = 21.10; SD = 58.50) as the control users (mean = 20.80; SD = 34.30). The “followers-to-friends” ratio among Twitter users with schizophrenia (mean = 7.17; SD = 52.40) was also similar to that of control users (mean = 2.56; SD = 6.33). Only gender differed significantly between groups, where a larger proportion of Twitter users with schizophrenia (n = 93; 45.8%) were identified as male compared to control users (n = 57; 33.0%; χ2 = 8.10; p = 0.017).
Tweets about depression and anxiety
Table 1 illustrates differences in the number of tweets about depression and anxiety between the two groups. Overall, Twitter users with schizophrenia tweeted significantly more about depression (mean = 9.47; SD = 17.79) compared with control users (mean = 2.47; SD = 8.55; t = −4.73; p<0.001). Among Twitter users with schizophrenia, n = 136 (67.0%) posted a total of 1923 tweets about depression (mean = 14.14; SD = 1.73), compared to n = 74 (42.8%) users in the control group who tweeted about depression 427 times (mean = 5.77; SD = 20.17). In a logistic regression model adjusting for gender, Twitter users with schizophrenia showed significantly greater odds of tweeting about depression compared with control users (OR = 2.69; 95% CI 1.76-4.10).
Table 1.
Tweets about depression and anxiety among Twitter users with schizophrenia and control users
| Twitter users with schizophrenia (n = 203) |
Control Twitter users (n = 173) |
Test Statistic | P valuea | |||||
|---|---|---|---|---|---|---|---|---|
| Tweets (n) | Mean (SD) tweets per user | Number of users (%) who tweeted | Tweets (n) | Mean (SD) tweets per user | Number of users (%) who tweeted | |||
| Depression Terms | ||||||||
| Depression | 1370 | 6.75 (12.20) | 128 (63.1%) | 275 | 1.59 (6.39) | 49 (28.3%) | −4.34 | <0.001 |
| Depressed | 586 | 2.89 (7.38) | 88 (43.3%) | 155 | 0.90 (2.49) | 54 (31.2%) | −2.76 | 0.006 |
| Tweets with any depression termsb | 1923 | 9.47 (17.79) | 136 (67.0%) | 427 | 2.47 (8.55) | 74 (42.8%) | −4.73 | <0.001 |
| Anxiety Terms | ||||||||
| Anxiety | 1080 | 5.32 (10.68) | 112 (55.2%) | 246 | 1.42 (4.82) | 60 (34.7%) | −3.00 | 0.003 |
| Anxious | 212 | 1.04 (2.84) | 60 (29.6%) | 83 | 0.48 (1.40) | 37 (21.4%) | −2.02 | 0.044 |
| Tweets with any anxiety termsc | 1283 | 6.32 (12.71) | 116 (57.1%) | 328 | 1.90 (6.03) | 74 (42.8%) | −4.20 | <0.001 |
P-values calculated using t-tests for the difference in mean (SD) tweets containing depression or anxiety terms between Twitter users with schizophrenia and control users.
Tweets with any depression terms also includes tweets that contain both ‘depression’ and ‘depressed’ terms.
Tweets with any anxiety terms also includes tweets that contain both ‘anxiety’ and ‘anxious’ terms.
Similarly, Twitter users with schizophrenia tweeted significantly more about anxiety (mean =6.32; SD = 12.71) compared with the control users (mean = 1.90; SD = 6.03; t = −4.20; p<0.001). Among Twitter users with schizophrenia, n = 116 (57.1%) tweeted about anxiety 1283 times (mean = 11.06; SD = 15.19) compared to 74 (42.8%) users in the control group who tweeted about anxiety 328 times (mean = 4.43; SD = 8.62). The Twitter users with schizophrenia also showed significantly greater odds of tweeting about anxiety compared with control users (OR = 1.81; 95% CI 1.20-2.73) after adjusting for gender.
Timing of tweets about depression and anxiety
In our total sample of Twitter users, 71.0% (267 out of 376) had available time zone data. There was no significant difference in availability of time zone information between Twitter users with schizophrenia (67.5%; n = 137) and control users (75.1%; n = 130). The proportions of tweets about depression and anxiety during each time interval between the Twitter users with schizophrenia and control users are illustrated in Figure 1 and Figure 2, respectively. In general, both groups appeared to post a greater proportion of their tweets about depression and anxiety later in the day (afternoon and evening). We did not observe any significant differences in the proportion of tweets about depression or anxiety between the Twitter users with schizophrenia and the control users at any time interval.
Figure 1.
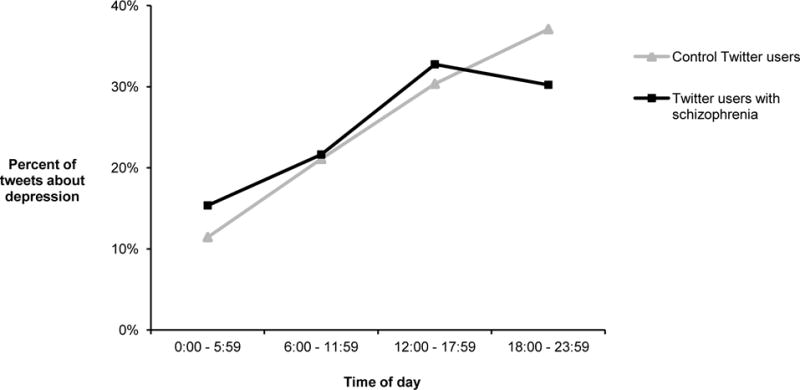
Percent of Tweets about depression by time-of-day among Twitter users with schizophrenia and control usersa
a There were no significant differences in the proportion of tweets about depression between Twitter users with schizophrenia and control users at any time interval.
Figure 2.
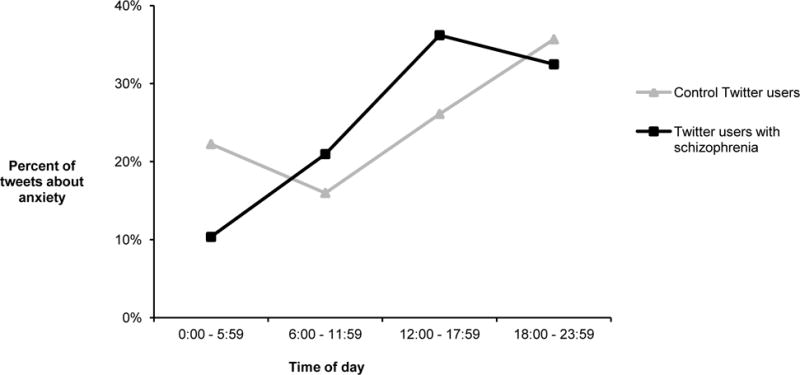
Percent of Tweets about anxiety by time-of-day among Twitter users with schizophrenia and control usersa
a There were no significant differences in the proportion of tweets about anxiety between Twitter users with schizophrenia and control users at any time interval.
Discussion
Research has shown that persons with schizophrenia experience more frequent and debilitating symptoms of depression and anxiety when compared to the general population [41]. Therefore, the purpose of this study was to investigate whether these real world and clinically meaningful mental health symptoms would also be present among social media users who self-identify as having a schizophrenia spectrum disorder. Importantly, we found that Twitter users with schizophrenia appeared to tweet about depression and anxiety significantly more often when compared to a randomly selected control group consisting of typical Twitter users. To our knowledge, this is the first study to examine patterns of communication about depression and anxiety among users with schizophrenia on popular social media. These findings offer preliminary evidence that Twitter users with schizophrenia may share clinical characteristics that are consistent with our understanding of schizophrenia in offline settings. Therefore, communication patterns on popular social media platforms such as Twitter may yield insight necessary to support future efforts aimed at early detection of individuals living with schizophrenia.
Our study expands on prior research demonstrating the utility of Twitter for understanding mental health conditions, including qualitative studies that have assessed attitudes about schizophrenia through content analysis of conversations on Twitter [42, 43]. Furthermore, our study builds on preliminary studies aimed at identifying text-based and other linguistic markers for schizophrenia on Twitter using machine learning and natural language processing techniques [25, 26, 44, 45]. For example, McManus et al (2015) found through the use of sentiment analysis of conversations on Twitter that users who self-identify as having schizophrenia appeared to exhibit unique tendencies [45], while Mitchell et al (2015) found evidence to suggest that Twitter users with schizophrenia show linguistic differences compared to control users [44]. The presence of linguistic differences between Twitter users with schizophrenia and control users was further identified in a study by Birnbaum et al (2017) [25]. Additionally, Ernala et al (2017) observed potential therapeutic benefits of self-disclosing diagnoses of schizophrenia on Twitter as reflected by positive changes in linguistic markers following online self-disclosure [26]. Importantly, our findings expand on this prior work and offer new insights about Twitter users with schizophrenia by showing that these individuals may also communicate more frequently about topics related to their mental health, such as depression and anxiety.
Specifically, we were able to show that Twitter users who self-identify as having schizophrenia may express elevated symptoms of depression and anxiety in their online posts, which is potentially consistent with clinical characteristics of schizophrenia observed in offline settings. For instance, research shows that among people with schizophrenia, depressive symptoms are associated with greater disability [46], poor physical health [47], and elevated risk of substance use [48]. Depressive symptoms have an independent negative effect on quality of life controlling for a range of socio-demographic, social, clinical, and psychosocial variables [27]. Similarly, research shows that anxiety symptoms are prominent among people with schizophrenia [49], and contribute to impaired social functioning, increased risk of suicide, and poorer recovery and low quality of life [50]. By potentially reflecting the elevated burden of these clinically meaningful mental health symptoms in this group using Twitter, there may be opportunities to leverage this online platform to further our understanding of schizophrenia by informing a digital phenotype, that is the development of a more comprehensive interpretation of the experiences of those living with schizophrenia that could potentially be leveraged to support new avenues for illness detection and management.
While the timing of tweets about depression and anxiety did not differ between groups, it was clear from our findings that Twitter users with schizophrenia discussed these common mental health topics significantly more than the control users. We acknowledge that our study affords only an incremental step towards quantifying the online attributes of individuals with schizophrenia. Though, our findings also contribute preliminary insights to further our understanding of a digital phenotype for schizophrenia, whereby drawing from novel digital data streams could provide insights about the manifestation of illness [15]. Despite the promise that the digital phenotype for schizophrenia holds for advancing psychiatric care [51], it is critical for future research to examine how passively collected data from social media can translate into improvements in clinically relevant outcomes such as mental or physical wellbeing, functioning, and quality of life among individuals living with schizophrenia [52]. The key challenge will be to determine how novel insights about schizophrenia derived from popular social media data can contribute to improvement in clinicians’ practices and align with patient priorities in order to inform the design and implementation of new care models for this at-risk patient group.
Limitations
There are several limitations with this study that are important to consider. First, and importantly, this was an exploratory study, and as such the findings presented here should be interpreted cautiously. Second, the Twitter users with schizophrenia included in this study self-identified as having a schizophrenia spectrum disorder; therefore, it was not possible to confirm their diagnosis clinically and they may differ from individuals with schizophrenia who choose not to disclose their illness online or who do not use social media. Third, the control group was comprised of a randomly selected sample of Twitter users representative of ‘typical users’, which means there is a possibility that users in this group may also have schizophrenia or other mental illnesses. Fourth, only well-defined terms for depression and anxiety were used in this study. This means that it is likely that there were many additional tweets reflecting these symptoms that used different terms, suggesting that we potentially underestimated the overall discussion about depression and anxiety among the Twitter users included in this study. Fifth, we could not collect demographic or clinical details for the Twitter users in this study. This is a common limitation with studies involving the use of popular social media because there are difficulties with retrieving this type of information from publicly available online data sources. Lastly, while we observed more frequent posts containing depression or anxiety terms among Twitter users with schizophrenia, this likely does not reflect a unique digital phenotype of schizophrenia given that use of these terms may similarly be common among Twitter users with other mental health conditions. However, we purposely selected depression and anxiety terms in this study because prior research has examined online discussion about these symptoms on Twitter. Additionally, our goal was to determine whether Twitter users with schizophrenia showed any differences in communication about depression or anxiety as compared to a randomly selected control group of typical Twitter users. The differences observed in this study highlight the need for future studies to expand on this work using popular social media platforms such as Twitter for studying schizophrenia.
Conclusions
It is promising that in this preliminary study we found that the attributes of Twitter users who self-identify as having schizophrenia may appear consistent with known clinical characteristics of the illness. In recent years there have been increasing efforts aimed at characterizing mental health through popular social media, though the field remains in its infancy. Nonetheless, the future of using social media to inform a digital phenotype affords exciting opportunities to ensure that early manifestations of diseases such as schizophrenia do not go unnoticed, or that serious symptoms among those living with the disease can be identified and targeted with appropriate treatment and support [15]. It is critical for researchers and mental health providers to recognize that digital platforms could serve as an adjunct to traditional approaches for disease detection, treatment and management. To achieve this potential, ongoing research is needed to further refine and develop the digital phenotype for schizophrenia by leveraging social media and other digital platforms as a means to inform improved treatment modalities for this serious and debilitating illness. The current study offers preliminary insights towards this end.
Acknowledgments
Funding: This study was supported by the Computational Epidemiology Group at Boston Children’s Hospital. YH reports receiving funding from the Canadian Institutes of Health Research and the Robert Wood Johnson Foundation (Grant 73495). JSB reports receiving funding from the National Institutes of Health, National Library of Medicine (R01LM010812) and from the Bill & Melinda Gates Foundation (OPP1093011). JBH reports receiving funding from the National Library of Medicine (T15LM007092) and the Robert Wood Johnson Foundation (Grant 73495). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors report no competing interests.
Biographies
Yulin Hswen, MPH, is a doctoral candidate in social and computational epidemiology in the Department of Social and Behavioral Sciences at the Harvard T.H. Chan School of Public Health.
John A. Naslund, PhD, is a Research Fellow in the Department of Global Health and Social Medicine at Harvard Medical School.
John S. Brownstein, PhD, is Professor of Pediatrics at Harvard Medical School and Chief Innovation Officer at Boston Children’s Hospital.
Jared B. Hawkins, PhD, MMSc, is Director of Informatics in the Innovation and Digital Health Accelerator at Boston Children’s Hospital, and a faculty member in the Department of Pediatrics at Harvard Medical School.
Footnotes
Compliance with Ethical Standards:
Conflict of Interest: No financial disclosures were reported by any of the authors of this manuscript. The authors report no conflicts of interest.
Ethical Approval: This study was considered exempt from ethical review because only publicly available online data collected from the Twitter platform was analyzed in this study.
Informed Consent: No human subjects were recruited in this study; therefore, informed consent was not necessary.
References
- 1.Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophrenia bulletin. 2004;30(2):279–293. doi: 10.1093/oxfordjournals.schbul.a007078. [DOI] [PubMed] [Google Scholar]
- 2.Folsom D, Jeste DV. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatrica Scandinavica. 2002;105(6):404–413. doi: 10.1034/j.1600-0447.2002.02209.x. [DOI] [PubMed] [Google Scholar]
- 3.Fowler IL, et al. Patterns of current and lifetime substance use in schizophrenia. Schizophrenia bulletin. 1998;24(3):443–455. doi: 10.1093/oxfordjournals.schbul.a033339. [DOI] [PubMed] [Google Scholar]
- 4.Brown S, Barraclough B, INSKIP H. Causes of the excess mortality of schizophrenia. The British journal of psychiatry. 2000;177(3):212–217. doi: 10.1192/bjp.177.3.212. [DOI] [PubMed] [Google Scholar]
- 5.Rosenheck R, et al. Barriers to employment for people with schizophrenia. American Journal of Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- 6.Dickerson FB, et al. Experiences of stigma among outpatients with schizophrenia. Schizophrenia bulletin. 2002;28(1):143–155. doi: 10.1093/oxfordjournals.schbul.a006917. [DOI] [PubMed] [Google Scholar]
- 7.Penttilä M, et al. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. The British Journal of Psychiatry. 2014;205(2):88–94. doi: 10.1192/bjp.bp.113.127753. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, et al. The prevalence and correlates of untreated serious mental illness. Health services research. 2001;36(6 Pt 1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- 9.Drake RE, Bond GR, Essock SM. Implementing evidence-based practices for people with schizophrenia. Schizophrenia Bulletin. 2009;35(4):704–713. doi: 10.1093/schbul/sbp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mojtabai R, et al. Unmet need for mental health care in schizophrenia: an overview of literature and new data from a first-admission study. Schizophrenia Bulletin. 2009;35(4):679–695. doi: 10.1093/schbul/sbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naslund JA, et al. Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health. 2015;24(5):321–332. doi: 10.3109/09638237.2015.1019054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alvarez-Jimenez M, et al. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophrenia Research. 2014;156(1):96–106. doi: 10.1016/j.schres.2014.03.021. [DOI] [PubMed] [Google Scholar]
- 13.Ben-Zeev D, et al. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophrenia Bulletin. 2014;40(6):1244–1253. doi: 10.1093/schbul/sbu033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ben-Zeev D, et al. CrossCheck: Integrating Self-Report, Behavioral Sensing, and Smartphone Use to Identify Digital Indicators of Psychotic Relapse. Psychiatric Rehabilitation Journal. 2017;40(3):266–275. doi: 10.1037/prj0000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jain SH, et al. The digital phenotype. Nature biotechnology. 2015;33(5):462–463. doi: 10.1038/nbt.3223. [DOI] [PubMed] [Google Scholar]
- 16.Highton-Williamson E, Priebe S, Giacco D. Online social networking in people with psychosis: A systematic review. International Journal of Social Psychiatry. 2015;61(1):92–101. doi: 10.1177/0020764014556392. [DOI] [PubMed] [Google Scholar]
- 17.Schrank B, et al. How patients with schizophrenia use the internet: qualitative study. Journal of medical Internet research. 2010;12(5):e70. doi: 10.2196/jmir.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Birnbaum ML, et al. Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non-psychotic mood disorders. Early intervention in psychiatry. 2017;11(4):290–295. doi: 10.1111/eip.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naslund JA, Aschbrenner KA, Bartels SJ. How people with serious mental illness use smartphones, mobile apps, and social media. Psychiatric Rehabilitation Journal. 2016;39(4):364–367. doi: 10.1037/prj0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naslund JA, et al. The future of mental health care: peer-to-peer support and social media. Epidemiology and Psychiatric Sciences. 2016;25(02):113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coppersmith G, Dredze M, Harman C. Workshop on Computational Linguistics and Clinical Psychology: From Linguistic Signal to Clinical Reality. Baltimore, MD: Association for Computation Linguistics; 2014. Quantifying mental health signals in Twitter. [Google Scholar]
- 22.Park M, Cha C, Cha M. Proceedings of the ACM SIGKDD Workshop on healthcare informatics (HI-KDD) Beijing, China: 2012. Depressive moods of users portrayed in Twitter. [Google Scholar]
- 23.De Choudhury M, et al. Predicting Depression via Social Media. Association for the Advancement of Artificial Intelligence. 2013 [Google Scholar]
- 24.De Choudhury M, Gamon M, Counts S. Happy, nervous or surprised? classification of human affective states in social media. Sixth International AAAI Conference on Weblogs and Social Media. 2012 [Google Scholar]
- 25.Birnbaum ML, et al. A Collaborative Approach to Identifying Social Media Markers of Schizophrenia by Employing Machine Learning and Clinical Appraisals. Journal of Medical Internet Research. 2017;19(8):e289. doi: 10.2196/jmir.7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ernala SK, et al. Linguistic Markers Indicating Therapeutic Outcomes of Social Media Disclosures of Schizophrenia. Proc ACM Hum-Comput Interact. 2017;1(1):43. [Google Scholar]
- 27.Mechanic D, et al. Effects of illness attribution and depression on the quality of life among persons with serious mental illness. Social science & medicine. 1994;39(2):155–164. doi: 10.1016/0277-9536(94)90324-7. [DOI] [PubMed] [Google Scholar]
- 28.Cosoff SJ, Hafner R Julian. The prevalence of comorbid anxiety in schizophrenia, schizoaffective disorder and bipolar disorder. Australian and New Zealand Journal of Psychiatry. 1998;32(1):67–72. doi: 10.3109/00048679809062708. [DOI] [PubMed] [Google Scholar]
- 29.McIver DJ, et al. Characterizing sleep issues using Twitter. Journal of Medical Internet Research. 2015;17(6):e140. doi: 10.2196/jmir.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nsoesie EO, et al. Social media as a sentinel for disease surveillance: what does sociodemographic status have to do with it? PLOS Currents Outbreaks. 2016 doi: 10.1371/currents.outbreaks.cc09a42586e16dc7dd62813b7ee5d6b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hawkins JB, et al. A digital platform for local foodborne illness and outbreak surveillance. Online Journal of Public Health Informatics. 2016;8(1):e60. [Google Scholar]
- 32.Mowery D, et al. Identifying Depression-Related Tweets from Twitter for Public Health Monitoring. Online Journal of Public Health Informatics. 2016;8(1) [Google Scholar]
- 33.Seaman I, Giraud-Carrier C. Healthcare Informatics (ICHI), 2016 IEEE International Conference on. IEEE; 2016. Prevalence and Attitudes about Illicit and Prescription Drugs on Twitter. [Google Scholar]
- 34.Hswen Y, Naslund JA, Chandrashekar P, Siegel R, Brownstein JS, Hawkins JB. Exploring online communication about cigarette smoking among Twitter users who self-identify as having schizophrenia. Psychiatry Res. 2017;257:479–84. doi: 10.1016/j.psychres.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eichstaedt JC, et al. Psychological language on Twitter predicts county-level heart disease mortality. Psychological science. 2015;26(2):159–169. doi: 10.1177/0956797614557867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Statista. Number of monthly active Twitter users worldwide from 1st quarter 2010 to 1st quarter 2017 (in millions) 2017 [cited 2017 June 16]; Available from: https://www.statista.com/statistics/282087/number-of-monthly-active-twitter-users/
- 37.McCormick TH, et al. Using Twitter for Demographic and Social Science Research: Tools for Data Collection and Processing. Sociological Methods & Research. 2015 doi: 10.1177/0049124115605339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Twitter. Twitter Developer Documentation: GET statuses/sample. 2017 [cited 2016 July 23]; Available from: https://dev.twitter.com/streaming/reference/get/statuses/sample.
- 39.Piccinelli M, Wilkinson G. Gender differences in depression. The British Journal of Psychiatry. 2000;177(6):486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- 40.McLean CP, et al. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. Journal of psychiatric research. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Emsley RA, et al. Depressive and anxiety symptoms in patients with schizophrenia and schizophreniform disorder. The Journal of clinical psychiatry. 1999;60(11):747–751. doi: 10.4088/jcp.v60n1105. [DOI] [PubMed] [Google Scholar]
- 42.Reavley NJ, Pilkington PD. Use of Twitter to monitor attitudes toward depression and schizophrenia: an exploratory study. PeerJ. 2014;2:e647. doi: 10.7717/peerj.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Joseph AJ, et al. # Schizophrenia: use and misuse on Twitter. Schizophrenia research. 2015;165(2):111–115. doi: 10.1016/j.schres.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 44.Mitchell M, Hollingshead K, Coppersmith G. Proceedings of the 2nd Workshop on Computational Linguistics and Clinical Psychology: From Linguistic Signal to Clinical Reality. Denver, CO: Association for Computational Linguistics; 2015. Quantifying the language of schizophrenia in social media. [Google Scholar]
- 45.McManus K, et al. Mining Twitter data to improve detection of schizophrenia. AMIA Summits on Translational Science Proceedings. 2015;2015:122–126. [PMC free article] [PubMed] [Google Scholar]
- 46.Meesters PD, et al. Prevalence and correlates of depressive symptoms in a catchment-area based cohort of older community-living schizophrenia patients. Schizophrenia research. 2014;157(1):285–291. doi: 10.1016/j.schres.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 47.Sajatovic M, et al. Clinical characteristics of individuals with serious mental illness and type 2 diabetes. Psychiatric Services. 2015;66(2):197–199. doi: 10.1176/appi.ps.201300538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kerfoot KE, et al. Substance use and schizophrenia: adverse correlates in the CATIE study sample. Schizophrenia research. 2011;132(2):177–182. doi: 10.1016/j.schres.2011.07.032. [DOI] [PubMed] [Google Scholar]
- 49.Huppert JD, Smith TE. Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS spectrums. 2005;10(09):721–731. doi: 10.1017/s1092852900019714. [DOI] [PubMed] [Google Scholar]
- 50.Pallanti S, Quercioli L, Hollander E. Social anxiety in outpatients with schizophrenia: a relevant cause of disability. American Journal of Psychiatry. 2004;161(1):53–58. doi: 10.1176/appi.ajp.161.1.53. [DOI] [PubMed] [Google Scholar]
- 51.Onnela JP, Rauch SL. Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology. 2016;41:1691–1696. doi: 10.1038/npp.2016.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fisher CE, Appelbaum PS. Beyond Googling: The Ethics of Using Patients’ Electronic Footprints in Psychiatric Practice. Harvard Review of Psychiatry. 2017:1–10. doi: 10.1097/HRP.0000000000000145. [DOI] [PubMed] [Google Scholar]


