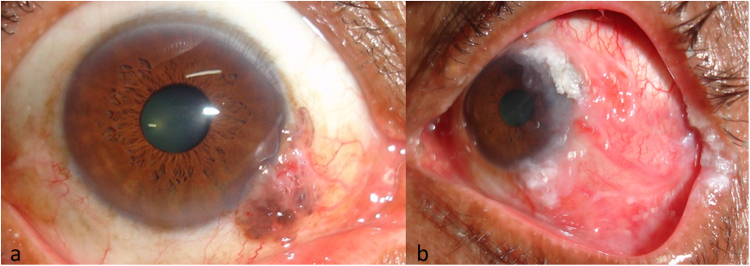
American Joint Committee for Cancer Classification (AJCC-TNM) is routinely used for ocular surface squamous neoplasia (OSSN) staging worldwide. However, recently some limitations of this classification have been reported. Sheilds et al. [1] mentioned the skewed distribution of cases among the various AJCC tumor grades in their study, with most cases being classified as grade T3. Similar trend was observed in our study, where 81% of tumors were classified as grade T3 [2]. This may be explained by the fact that majority of OSSN arise at the limbus [2], and therefore tend to involve the adjacent cornea. In AJCC classification, tumor with corneal involvement are clubbed in tumor grade T3 along with tumors that involve other adjacent structures like plica, eyelid, caruncle, lacrimal punctum, and eyelid margin. Unlike a small corneal involvement, extension to other specified structures usually reflects a more extensive disease in terms of area of involvement (Fig. 1). Therefore, smaller tumors with minimal corneal involvement should be classified separately.
Fig.1.
Clinical photograph showing a small OSSN at the limbus (AJCC grade T3), b diffuse OSSN with involvement of eyelid margin (AJCC grade T3)
Second modification required is the separate categorization of tumors with overt intraocular extension (that is intraocular extension that can be picked up clinically or on ultrasound biomicroscopy (UBM)). Currently, these tumors are classified as AJCC grade T3. Unlike other T3 grade tumors that may be treated with wide surgical excision or immunotherapy/chemotherapy, tumors with intraocular extension require enucleation, and therefore are associated with a greater morbidity.
Newer edition of AJCC (8th edition) has brought minor modifications to tumor grades T1 and T2, where histological criteria has been included along with clinical criteria [3]. Unlike previously when surgical excision was the gold standard for treatment, chemotherapy/immunotherapy is gaining popularity and has been accepted as the first line treatment for non-invasive cases. As excision biopsy has become less common and incision biopsy is a relative contraindication for OSSN, a histological grading becomes irrelevant to the current treatment scenario. Most medical management is done based on clinical diagnosis. With the availability of better anterior segment imaging like optical coherence tomography and UBM, invasion into sclera can be picked up without the need of tissue sampling. Therefore, we wonder how this modification may be applied in the current management scenario.
Also, the current AJCC classification does not provide any guideline for the choice of treatment for different tumor stages. Hence, we propose a new classification scheme for OSSN that takes into account the limitations of AJCC classification, and in addition provides a rough guide for the treatment of tumor in the current management situation (Table 1). Here, we have classified the tumor grades on the basis of tumor size, and tumor invasion as picked up on imaging. Cases with invasion beyond the conjunctiva and into the sclera have been classified separately as grade II, and those with intraocular extension have been categorized as grade III. A treatment guide has been provided for various tumor grades based on risk of side effects of upfront surgical excision in non-invasive tumor, and tumor extension in coats, globe, or orbit.
Table 1.
Proposal for the new classification
| Group/grade | Limbal involvement (clock hours) | Maximal basal diameter (mm) | Imaging findings | Treatment recommended | Risk with upfront surgical excision |
|---|---|---|---|---|---|
| Grade I: OSSN with no invasion into ocular coats clinicallya/on imaging(UBM) | |||||
| A (small) | ≤3 | ≤5 | No invasion into ocular coats/globe on UBM | Surgical excision with edge control | Minimal risk of side effects |
| B (large) | >3 to <6 | 5–15 | No invasion into ocular coats/globe on UBM | Immunotherapy/immunoreduction f/b surgical excision | Moderate risk of side effects (limbal stem cell deficiency, symblepharon formation) |
| C (diffuse) | ≥6 | ≥15 | No invasion into ocular coats/globe on UBM | Immunoreduction with interferons f/b surgical excision | High risk of side effects, high risk of recurrence |
| Grade II: OSSN with no invasion into ocular coats (sclera/corneal stroma) on imaging | |||||
| Any | Any | Scleral or corneal stromal invasion on UBM | Excision with lamellar sclerectomy or keratectomy + cryotherapy of margins and base | ||
| Grade III: OSSN with intraocular invasion | |||||
| Any | Any | Intraocular involvement present (clinically/UBM) | Enucleation | — | |
| Grade IV: OSSN with intraorbital extension | |||||
| Any | Any | Orbital extension on CT/MRI | Exenteration | — | |
UBM ultrasound biomicroscopy, CT computed tomography scan, MRI magnetic resonance imaging, MMC mitomycin C, 5FU 5 fluorouracil, IO intraocular, f/b followed by
aClinically as suggested by mobility of conjunctival lesions in non-limbal tumors
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Shields CL, Kaliki S, Kim HJ, Al-Dahmash S, Shah SU, Lally SE, et al. Interferon for ocular surface squamous neoplasia in 81 cases: outcomes based on the American Joint Committee on Cancer classification. Cornea. 2013;32:248–56. doi: 10.1097/ICO.0b013e3182523f61. [DOI] [PubMed] [Google Scholar]
- 2.Meel R, Dhiman R, Vanathi M, Pushker N, Tandon R, Devi S. Clinicodemographic profile and treatment outcome in patients of ocular surface squamous neoplasia. Indian J Ophthalmol. 2017;65:936–41. doi: 10.4103/ijo.IJO_251_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amin MB, Greene FL, Edge SB, Crompton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67:93–9. doi: 10.3322/caac.21388. [DOI] [PubMed] [Google Scholar]