Abstract
Introduction
The shoulder joint is the most common major joint to dislocate. Population aged younger than 20 years, recurrent dislocation rates have been reported to be as high as 90%. For those individuals that continue to experience dislocations surgery is often a good decision. The goal of the Bankart surgery is to reconnect the torn labrum to the glenoid fossa. Double-row Bankart repair can both achieve anatomic reduction and enhance fixation stability. The purpose of our study is to assess the clinical outcome of arthroscopic double row repair.
Methods
49 cases with Bankart lesion operated by double row repair were studied. Functional outcome and retear were assessed after at least 6 months of surgery using scores and MRI.
Results
Significant improvement in functional outcome after repair by double row Bankart repair. No retear or redislocation seen.
Conclusion
Double row repair technique improves function of shoulder significantly and potentially minimizes future re-injury or recurrence risk.
Keywords: Bankart lesion, Anterior shoulder instability, Arthroscopic Bankart repair, Double row Bankart repair, Functional outcome
TEXT
1. Introduction
The glenohumeral joint is the most common major joint to dislocate. There are a number of lesions that are associated with anterior instability, main lesion being the Bankart lesion.1 Biomechanical studies have reinforced the importance of preserving and/or re-establishing the normal architectural vault of the glenoid rim as critical to restoring normal shoulder stability.2 The goal of the Bankart surgery is to reconnect the torn labrum to the glenoid fossa. This repairs and stabilizes the joint to prevent further dislocations. The most commonly described and performed Bankart repair is the single-row technique. Recent interest in achieving improved fixation has led to the evolution of a double-row procedure, first described by Zhang3 and further refined and popularized as a “bony Bankart bridge” technique by Millett et al4,5 Double row fixation technique allows healing of the capsule labral complex to a broader bony surface and decreases recurrence rates of instability.6 The purpose of the study is to assess functional outcome and retear rate of double row Bankart repair.
2. Methods
This was a single Centre, single surgeon, prospective study. Among patients who had Bankart lesion and required double row Bankart repair, 49 patients were enrolled for the study.
Preoperative clinical scoring (Constant score and DASH score), Ct scan and MRI of affected shoulder were done which is a routine part of management in our hospital. Post-surgery clinical scoring was repeated at 3, 6 and 12 months. MRI of shoulder was done at the end of 12 months to detect re-tear.
-
•Inclusion criteria
-
1Patients with shoulder instability diagnosed with Bankart lesion
-
2Patients with shoulder instability diagnosed with Bankart lesion
-
3Bony Bankart lesion with <15% of Glenoid involvement
-
4Patient between 18–40 years of age
-
5Those who gave consent to be a part of this study
-
6Patients managed with arthroscopic repair
-
1
-
•Exclusion criteria
-
1Bony Bankart lesion with >15% of Glenoid involvement.
-
2Presence of concomitant “significant” Hill-Sachs lesion or concomitant HAGL (Humeral Avulsion of the Glenohumeral Ligament) or rotator cuff tear.
-
3Failed prior arthroscopic stabilization in the face of poor quality anterior glenoid bone remnant.
-
4Axillary nerve injury with sensory deficit to the overlying dermatome and/or deltoid weakness.
-
5Patients with neurological disorders, epilepsy or psychiatric disorders.
-
6Patients with any other shoulder pathology including osteo-arthritis of shoulder joint.
-
7Patients with past history of fracture around shoulder joint.
-
8Patient posted for Revision arthroscopic shoulder Bankart repair
-
9Distal neurovascular deficits
-
1
History was elicited from the patients regarding age, sex, mode of injury, side, hand dominance, loss of function, method used for reduction, prior history of subluxation or dislocation, surgery, or other injury and the chronicity of complaints was taken from the patient. Patient was clinically examined for range of motions, strength testing, etc. Pre operative Constant score and DASH score were documented for all patients. A thorough neurovascular examination to evaluate for possible concomitant brachial plexus or vascular injury was also executed. Finally specific tests for instability were performed, including the apprehension test, relocation test, anterior and posterior drawer maneuvers, and sulcus sign. Apprehension test is used to test the integrity of glenohumeral joint capsule, a possible torn labrum or anterior shoulder instability. Performed by placing the patient’s arm in a position of abduction with external rotation. This causes a feeling of uneasiness and an uncomfortable sense of imminent dislocation. If Apprehension test found positive, Jobes relocation test was done, which also tests for anterior instability of shoulder. In supine position with 90° abduction and elbow flexion of 90°, shoulder is externally rotated. At the point when patient reports apprehension, a posteriorly directed force is applied to the shoulder. If patient’s apprehension or pain is reduced in this position, Jobes relocation test is considered to be positive. Sulcus test is demonstrated by a depression visualized between the inferior border of the lateral acromion and the superior aspect of the humeral head while pulling longitudinal traction on the arm. The presence of a sulcus sign greater than 2 cm, suggests inferior laxity to the degree commonly found in patients with multidirectional instability. According to Romeo, a history of a traumatic event with a documented anterior dislocation and a positive apprehension sign is associated with a greater than 95% incidence of a Bankart lesion. Radiological evaluation consists of pre operative radiological evaluation by true Antero-posterior view of shoulder joint, CT scan and MRI of affected shoulder. Glenoid bone loss quantification was done based on glenoid rim distance. The bare spot, intersection of the longitudinal axis and the widest antero-posterior diameter of the glenoid is approximated on the glenoid fossa. A best-fit circle centered at the bare spot is drawn in the inferior two-thirds of the glenoid. The distances from the anterior edge and the posterior rim to the bare spot are measured. Percentage bone loss is calculated using the formula. Final diagnosis was done on the basis of intra operative findings. Repeat MRI was done at the end of 12 months for retear. Assessment scores consist of Constant and DASH score (Fig. 1, Fig. 2).
Fig. 1.
MRI images of 22 yr. male with recurrent shoulder dislocation showing Bony Bankart lesion (Axial view).
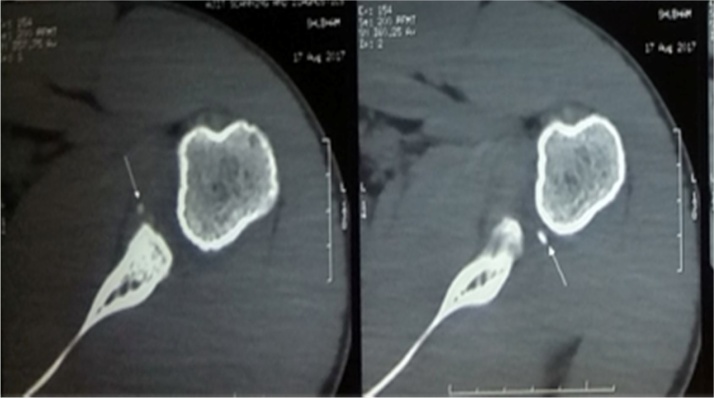
Fig. 2.
CT scan of 22 Year male with recurrent shoulder dislocation showing Bony Bankart lesion (Axial view).
2.1. Surgical technique
Same surgeon performed all the procedures under regional or general anesthesia, with the patient in the floppy lateral position. To confirm instability pattern affected shoulder is examined under anesthesia.
Arthroscopic pump was used to provide constant distention, minimize bleeding, and improve visualization during the procedure. A diagnostic arthroscopy was the first thing in the procedure. Arthroscope was placed through a standard posterior portal, which was located 2 cm distal and medial to the posterolateral border of the acromion.
A full diagnostic arthroscopy (Fig. 3) was performed. Anatomic lesions such as a suspected detached anteroinferior glenoid labrum, rotator cuff injury, Hill-Sachs lesion, chondral lesion, any other labral tears are looked for. The condition of the labrum and capsule was evaluated. Posterior, anterior-Inferior and antero-superior portals were established for each patient. The posterior portal was used as the viewing portal; the anterior portal was used as the working portals. Several other additional percutaneous portals are useful during Arthroscopic Bony Bankart repair. The most common is the accessory anterior-inferior 5 o’clock portal. Typically this is placed from 1 to 3 cm inferior to the established AI portal. This portal both facilitates anchor placement on the posterior-inferior quadrant of the glenoid, and provides an accessory portal for bony fragment manipulation and suture management.
Fig. 3.
Arthroscopic image of Bankart Lesion seen through anterosuperior portal.
Glenoid neck was prepared by dissecting the labrum from the glenoid neck, using rasp. Medial anchor was inserted approximately 10 to 15 mm medial to the articular surface of the glenoid and lateral to conjoint tendon. Viewing with a 30° lens from the anterosuperior portal, drill guide was placed through the anteroinferior portal or accessory anterior inferior (5 o’clock) portal into the medial glenoid. When drilling the anchor insertion site, make sure to have an appropriate “angle of attack” from lateral to medial, to avoid undermining the articular cartilage (which occurs if one is too parallel to the joint). Also, be careful to avoid too vertical an approach, which can lead to inadvertent penetration of the inferior glenoid rim and extra-osseous anchor placement. Anchor was passed through the same guide after drilling. The first anchor was placed at the inferior-most aspect of the tear, inferior to the Bankart lesion. The anchor must be firmly seated such that its eyelet is below the articular cartilage, and tensioned to ensure it is secure within the bone. Additional medial row anchors were placed from inferior to superior depending upon the length of the lesion (Fig. 4).
Fig. 4.
Arthroscopic image of Bankart lesion with medial row anchors insitu.
Sutures of the medial anchors were brought from inside to outside through separate points in the capsulolabral complex. Double row construct was completed by inserting the medial row sutures into knotless bio composite anchors, for lateral row fixation. The suture pair of the first (most inferiorly placed) medial anchor was retrieved and threaded through the knotless anchor. The first knotless anchor was seated onto the glenoid rim at a point directly lateral to the corresponding medially placed anchor pair, approximately 2 mm onto the anterior lip of the glenoid with medial inclination of approximately 45°. The first knotless anchor was gently seated and impacted into place. These steps were repeated to place all lateral anchors. Lateral anchors were placed corresponding to each of the previously placed medial row anchors (Fig. 5). This provides a suture bridge repair of the capsulolabral defect with two point fixation. The free ends of the suture are cut flush with anchor after lateral fixation.
Fig. 5.
Arthroscopic image of lateral row anchor (Knotless anchor) placed on to the anterior lip of glenoid.
In case of osseous Bankart lesion, repair was done by same technique. The lesion is repaired anatomically between the medial and lateral row anchors. By this, the osseous component is compressed and reduced into the fracture bed on anteroinferior glenoid.
Final repair construct is inspected from both anterosuperior and posterior portals (Fig. 6).
Fig. 6.
Arthroscopic image of Bankart lesion repaired by double row Bankart repair technique.
2.1.1. Postoperative protocol
All the patients followed the same postoperative protocol.
Patients wore a shoulder sling with abduction pillow for two weeks. Skin sutures were removed at 14 days post-operatively. Patients were allowed to come out of the sling twice daily for active elbow flexion/extension exercises, and instructed in scapular and rotator cuff strengthening exercises. Formal physical therapy was started at the 3-week mark, working to restore active and assistive range of motion, with gentle strengthening of the cuff and scapular muscles advanced as tolerated. Combined abduction and external rotation was avoided until week 12. Patients were then allowed to return to sport at 4–6 months and predicated on the achievement of previous benchmarks and goals.
MRI was done at the end of 12th month.
2.1.2. Consent
Consent was taken a day before surgery. Patient was explained about the study procedure orally and in writing, in a language best understood by them, and signed consent obtained. Details were collected according to a defined format of questions and examination, administered by the investigator.
2.2. Sample size
The sample size for this study was calculated using method described to estimate a mean value of variable in desired sample of population assuming the value remains comparable to true population mean and the sample population is representative.7
The data used in the calculation was based on the previously published literature on suggested mean values, standard deviations and population variance with respect to subscales of Constant score in patients undergoing Arthroscopic double row repair technique for Bankart lesion in patients presenting to tertiary care hospital (Fabbriciani et al)8. In current study we used Constant score as one of the primary variables. From estimation of previous data the mean value of maximum range of motion as per the Constant score in sample of study population was 39.60 ± 0.80° assuming they were surgically repaired. The minimum allowable difference of 20° (μ − μ0) was expected to be observed from baseline condition after 1 year of follow-up (up to 50% of superiority margin). Then the result of sample size at 95% confidence interval (α = 0.05) with population variance of 0.64° for having 80% power (β = 0.2) was 44. Considering 10% dropouts over a study period a sample size of 49 patients was required (N = 49)
Sample size is calculated using the formula:
Where
| Variables | Descriptions |
|---|---|
| α | One-sided significance level |
| 1-β | Power of the test |
| Allowable difference | Acceptable difference between sample mean and known or expected population mean (μ − μ0) |
| Population variance | Population variance |
| δ | δ > 0 for the superiority margin or δ < 0 for the non-inferiority margin |
| N | Sample size |
49 cases of Bankart lesion operated by double row repair technique.
2.3. Statistical analysis
Qualitative data was represented in the form of percentages. Quantitative data was calculated using mean ± SD and/or median with range. Analysis of quantitative data between a qualitative variable was done using RMANOVA where data passed ‘Normality test’ and by Friedman test where data failed ‘Normality test’. Chi-Square test was used for proportions. Results were represented graphically. MS Excel and Graph pad software was used for most analysis. P value < 0.05 will be considered significant.
The Mean age calculated among the study sample was 29 years. A total of 80% males and 20% females were included in the study (Table 1).
Table 1.
Gender distribution. Incidence of tear is more in males than females. Calculated using the sign & binomial test. P < 0.05 considered statistically significant.
| Gender | No. | % | p-valuea |
|---|---|---|---|
| Males | 39 | 79.59 | <0.0001 |
| Females | 10 | 20.41 |
Calculated using the sign & binomial test. P < 0.05 considered statistically significant.
Significant gender difference with men having three to four times higher incidence of repair was found. No statistical difference was found in the side involved. 8.16% of the total study population had bony Bankart lesion.
Clinical outcome of double row Bankart repair was assessed. Mean constant score increased from 38.37 to 88.98 by the end of 1 year, which is a significant improvement (Table 2).
Table 2.
Constant score. Significant improvement seen in score, 12 months postoperative period. Calculated for pre-operative & at 12 months using paired t-test. P < 0.05 considered statistically significant.
| Time period | Mean | SD | P-valuea |
|---|---|---|---|
| Pre-operative | 38.37 | 5.61 | <0.05 |
| 3 months | 65.41 | 4.36 | |
| 6 months | 77.22 | 3.44 | |
| 12 months | 88.98 | 2.45 |
Calculated for pre-operative & at 12 months using paired t-test. P < 0.05 considered statistically significant.
Significant improvement in Mean DASH Score was seen from 52.38 to 6.80 by the end of 12 months (Table 3).
Table 3.
DASH Score. Significant improvement seen in score, 12 months postoperative period. Calculated for pre-operative & at 12 months using paired t-test. P < 0.05 considered statistically significant.
| Time period | Mean | SD | p-valuea |
|---|---|---|---|
| Pre-operative | 52.38 | 3.44 | <0.05 |
| 3 months | 29.08 | 2.86 | |
| 6 months | 15.37 | 2.41 | |
| 12 months | 6.80 | 1.17 |
Calculated for pre-operative & at 12 months using paired t-test. P < 0.05 considered statistically significant.
Redislocation was not seen in any of the study subject in 1-year follow up in postoperative period (Table 4).
Table 4.
Redislocation. Redislocation was not seen in any of the study subjects in 1 year post operative period. Calculated using the sign & binomial test. P < 0.05 considered statistically significant.
| Re-dislocation | No. | % | p-valuea |
|---|---|---|---|
| Yes | 0 | 0 | <0.0001 |
| No | 49 | 100 |
Calculated using the sign & binomial test. P < 0.05 considered statistically significant.
3. Discussion
Surgical treatments for anterior shoulder instability are either open surgical stabilization or arthroscopic stabilization of the detached capsulolabral complex.9 Anterior shoulder instability with a Bankart lesion was initially treated with open repair, as performed by Bankart himself, published by Dickson and Devas in 1957. With the evolution of shoulder arthroscopy in the last two decades, from a limited diagnostic modality to a surgical tool, the arthroscopic stabilization for recurrent anterior instability with varying stabilizing techniques, varying success are being reported. Arthroscopic Bankart procedures have been regarded as inferior to the open Bankart procedure in terms of stability, where the classical study by Rowe et al10 showed a recurrence rate of only 3.5%. Recent literature suggests that the outcomes of arthroscopic stabilization approach those of open stabilization in appropriately selected patients.6
Open surgical stabilization reattaches the capsulolabral complex to the anterolateral glenoid rim and the capsule to the anterior glenoid neck. This enables fixation and reattachment of the capsulolabral complex close to its original anatomical insertion site. However, current arthroscopic stabilization techniques focus on recreating the labral bumper effect as a locating suture anchor to the glenoid articular surface, when suturing of capsulolabral complex. Arthroscopic approaches avoid the risk of rupture of subscapularis, reduce operative time, improve cosmesis, and are associated with a near normal range of motion postoperatively.
A major complication of postoperative capsulolabral complex repair is recurrence of the instability. Special surgical technique including repair of the labrum 1–2 mm onto the glenoid articular surface11,12 or at the articular edge13,14, have been recommended by many authors. The anterior glenoid bone is prepared using burr, shaver or rasp, to facilitate healing of the capsulolabral complex to the anterior glenoid bone.15 However, Suture anchors set suture on articular surface of the glenoid. This leads to healing on the glenoid articular surface instead of intended anatomical footprint area. Thus, the current single row repair technique cannot make an adequate environment to facilitate the healing of the tendon on the footprint area, and it can become one of the reasons for recurrence of dislocation.
Ahmad et al16, in a cadaveric study, found that the mean surface area of the native capsulolabral complex footprint was 256 ± 40 mm2, whereas the native footprint of the labrum was 152.3 ± 24.4 mm2. The labrum attachment comprised 59% of the overall capsulolabral complex. They reported that the single row repair recreated 42.3% (108 ± 27 mm2) of the native footprint surface area while the double row repair recreated 85.9% (220 ± 39 mm2). Also, Ahmad et al16 argued that double row repair of the capsulolabral complex reestablishes the native insertional footprint on the anterior glenoid better than single row repair.
Our study showed significant gender difference with men having three to four times higher incidence of repair. No statistical difference was found in the side involved. The average age of the patients operated was 29.69 ± 7.10. Bone loss was seen in 8.16% of the study population. Our repair has shown complete healing. Re-dislocation was not seen in any of the study subject within the 1 year follow up postoperatively. Ahmed et al17 in their study about functional outcomes and risk factors for recurrence of shoulder dislocation after arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability found that recurrent glenohumeral instability after single row Bankart repair was 13.2%, and this complication developed within one year in 55% of these patients. Thus, the recurrence of instability is less in double row repair. Significant differences were found in Constant and DASH scores at 3,6 and 12 months. Mean constant score increased from 38.37 to 88.98. Mean DASH Score decreased from 52.38 to 6.80. MRI done at 12 months postoperative period showed signs of healing, anchors were in place and there were no signs of tear. Peter et al4 also found improvement in shoulder scores, which was almost three times the minimal clinically important difference. Out of 15 study subjects, Peter et al reported only one failure with redislocation from a fall. Spiegl et al18 in a biomechanical analysis of single-versus double-row repair for bony Bankart lesion showed that the double-row repair provided both improved stability and fracture reduction compared to the single-row repair. Studies have shown that double row repair technique provide increased stability, more stable reduction of the osseous fragment, and overall potential for improved fracture healing, restoration of normal articular surface, and improved long-term outcome with low surgical morbidity than open procedures.
The most important limitation of the study is number of anchors. Double row Bankart repair technique requires more anchors than needed for single row repair. This technique of repair demand more surgical skill and takes longer time than single row repair. Patients were followed only for a period of 1 year. This timeframe showed improvement in clinical features but longer follow up is needed for more definitive results. The strengths of our study were, it was a single surgeon series, with uniform surgical skills and adopted rigid inclusion and exclusion criteria. In summary, double row Bankart repair technique showed good clinical results. The described technique of Bankart repair can provide excellent shoulder stability and favorable clinical outcomes when applied to appropriately selected patients. Successful implication of this technique requires thorough preoperative planning and a complete understanding of the size and extent of the involved lesion.
4. Conclusion
The current evidences suggest that use of the double-row technique for rotator cuff repair decreases the incidence of retear and thus redislocation.6,19, 20, 21 In our study there was a significant improvement in functional outcome. The arthroscopic double row Bankart repair technique for anterior glenohumeral instability successfully restores shoulder stability with very low complication rate. There is significant improvement is functional outcome. Surgeons should use the double row Bankart repair technique to improve the structural and functional outcome of the repaired Bankart lesion. Nevertheless, future long term randomized control trials on this topic are needed.
Contributor Information
Roshan Wade, Email: roshanwade@gmail.com.
Bhanuprakash Reddy P V, Email: dr.bhnauprakash28@gmail.com.
References
- 1.Matsen F.A., Thomas S.C., Rockwood C.A., Wirth M.A. Glenohumeral instability. In: Rockwood C.A., Matsen F.A., editors. The Shoulder. 2nd edition. W.B. Saunders; Philadelphia: 1998. P 611–689. [Google Scholar]
- 2.Itoi E., Lee S.B., Berglund L.J., Berge L.L., An K.N. The effect of the glenoid defect on anterioinferior stability of the shoulder after Bankart repair. A cadaveric study. JBJSA. 2000;82(1):35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Zhang J., Jiang C. A new “double pulley” dual row technique for arthroscopic fixation of bony Bankart lesion. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1558–1562. doi: 10.1007/s00167-010-1390-z. [DOI] [PubMed] [Google Scholar]
- 4.Millett Peter J., Horan Marilee P., Frank Martstschlager. The “Bony Bankart bridge” technique for restoration of anterior shoulder instability. AJSM. 2013;41(3):608–614. doi: 10.1177/0363546512472880. [DOI] [PubMed] [Google Scholar]
- 5.Millett P.J., Braun S. The “Bony Bankart bridge” procedure: a new arthroscopic technique for reduction and internal fixation of a bony Bankart lesion. Arthroscopy. 2009;25(1):102–105. doi: 10.1016/j.arthro.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Lafosse L., Baier G.P., Jost B. Footprint fixation for arthroscopic reconstruction in anterior shoulder instability: the cassiopeia double-row technique. Arthroscopy. 2006;22(February (2)):231.e1–231.e6. doi: 10.1016/j.arthro.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 7.Chow, Shao, Wang . In: Sample Size Calculations in Clinical Research. Taylor, Francis, editors. 2003. New York. p 50–52. [Google Scholar]
- 8.Fabbriciani C., Milano G., Demontis A., Fadda S., Ziranu F., Mulas P.D. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20(May (5)):456–462. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Cole B.J., Millett P.J., Romeo A.A. Arthroscopic treatment of anterior glenohumeral instability: indications and techniques. Instr Course Lect. 2004;53:545–558. [PubMed] [Google Scholar]
- 10.Rowe C.R., Patel D., Southmayd W.W. The Bankart procedure: a long-term end-result study. J Bone Jt Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- 11.Mazzocca A.D., Brown F.M., Jr, Carreira D.S., Hayden J., Romeo A.A. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33(1):52–60. doi: 10.1177/0363546504268037. [DOI] [PubMed] [Google Scholar]
- 12.Rhee Y.G., Ha J.H., Cho N.S. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34(6):979–985. doi: 10.1177/0363546505283267. [DOI] [PubMed] [Google Scholar]
- 13.Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Arthroscopic separate labral repair and capsular plication with a suture anchor. Arch Orthop Trauma Surg. 2008;12895:535–538. doi: 10.1007/s00402-007-0406-8. [DOI] [PubMed] [Google Scholar]
- 14.Magit D.P., Tibone J.E., Lee T.Q. In vivo comparison of changes in glenohumeral translation after arthroscopic capsulolabral reconstructions. Am J Sports Med. 2008;36(7):1389–1396. doi: 10.1177/0363546508315199. [DOI] [PubMed] [Google Scholar]
- 15.Carreira D.S., Mazzocca A.D., Oryhon J., Brown F.M., Hayden J.K., Romeo A.A. A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2 tear follow up. Am J Sports Med. 2006;34(5):771–777. doi: 10.1177/0363546505283259. [DOI] [PubMed] [Google Scholar]
- 16.Christopher S.A., Gregory J.G., Christian Vorys, Covey M.D., Thomas R.G., William N.L. Evaluation of glenoid capsulolabral complex insertional anatomy and restoration with single- and double-row capsulolabral repairs. J Shoulder Elbow Surg. 2009;18(November (6)):948–954. doi: 10.1016/j.jse.2009.03.022. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed I., Ashton F., Robinson C.M. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability: functional outcomes and identification of risk factors for recurrence. J Bone Jt Surg Am. 2012;94(14):1308–1315. doi: 10.2106/JBJS.J.01983. [DOI] [PubMed] [Google Scholar]
- 18.Ulrich J.S., Sean D.S., Jocelyn N.T. Biomechanical comparison of arthroscopic single- and double-row repair techniques for acute bony bankart lesions. Am J Sports Med. 2014;42(July (8)):1939–1946. doi: 10.1177/0363546514532782. [DOI] [PubMed] [Google Scholar]
- 19.Iwaso, Hiroshi &, Uchiyama, Eiji &, Sakakibara, Sei-Ichirou &, Fukui Naoshi. Modified double-row technique for arthroscopic Bankart repair: surgical technique and preliminary results. Acta Orthop Belg. 2011;7:252–257. [PubMed] [Google Scholar]
- 20.Tang K.L., Chen G.X., Guo L., Gong J.C., Zhou B.H., Yang H.F., Gu L.C., Li H.Z., Yang L., Xu J.Z. Arthroscopic Bankart lesion repair by double-row vertical mattress suture with anchors for anteroinferior glenohumeral instability. Zhonghua Wai Ke Za Zhi. 2007;45(October (20)):1379–1381. [PubMed] [Google Scholar]
- 21.Kim K.C., Rhee K.J., Shin H.D. Arthroscopic three-point double-row repair for acute bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc. 2009;17(January (1)):102–106. doi: 10.1007/s00167-008-0659-y. [DOI] [PubMed] [Google Scholar]