Highlights
-
•
Tilt of the IVC filter is the major problem for the filter retrieval rate.
-
•
External compression on the IVC wall can cause filter tilting.
-
•
Identifying external compression factors are necessary before insertion of IVC filter.
Abbreviations: IVC, inferior vena cava; PACS, picture archiving and communication system
Keywords: Inferior vena cava filter, Computed tomography, Abutment, Retrieval, External compression, Filter retrieval
Abstract
Objectives
To investigate risk factors for inferior vena cava (IVC) filter abutment, including external compression on the IVC wall, using venous phase computed tomography (CT).
Methods
One-hundred-forty-one cases of Celect IVC filter insertion between January 2009 and April 2017 were retrospectively reviewed. On pre-procedural CT, IVC diameter and morphological classifications were measured. Filter tilt angle, IVC angle, vertical position, and filter tip abutment to the IVC wall were analyzed on post-procedural CT. IVC compression was examined by pre- and post-procedural CT analysis. Multiple logistic regression analysis was conducted to find factors related to IVC filter abutment.
Results
Of 141 IVC filter insertion cases, 52 were classified in the filter tip abutment group and 89 in the non-abutting group. IVC tilt angle (11.7 ± 5.5° vs. 6.4 ± 5.4°), presence of external compression (14/52, 27% vs. 9/89, 9%), and IVC morphology were different between the groups (p < 0.05). In multiple logistic regression analysis, filter-tilt angle over 9.25° and external compression on the IVC were found to be independent predictors of filter abutment (odds ratios: 4.56, 10.18, respectively).
Conclusion
IVC filter tilt, external compression on IVC wall, and IVC morphology were significantly different between the filter tip abutment and non-abutment groups. External compression and filter tilt over 9.25° were risk factors for filter tip abutment in multiple logistic regression analysis. By identifying these factors, we may be able to reduce filter tilting by preventing the filter from being deployed in a dangerous area.
1. Introduction
While anticoagulant therapy is the treatment of choice for deep vein thrombosis, inferior vena cava (IVC) filters are becoming increasingly popular as the only option to reduce the incidence of pulmonary embolism when anticoagulation is contraindicated. In addition to therapeutic purpose, prophylactic IVC filter insertion is also performed for patients with severe trauma or immobilization [1,2,3]. Permanent placement of a retrievable IVC filter increases the risk of IVC thrombosis and injury to adjacent organs [4,5]. The main reasons IVC filter retrieval fails are: (1) the filter hook is embedded in the IVC wall due to filter tilting; and (2) the filter limbs penetrate into adjacent organs [5,7]. Reducing IVC filter tilting at the time of insertion is essential for successful subsequent retrieval of the filter. However, despite advancement in IVC filter design and insertion techniques, the conditions leading to IVC filter tilting and abutment to the IVC wall are still unclear. Moreover, some factors, such as the connection between adjacent structures and IVC compression have not yet been investigated. Therefore, the purpose of this study was to investigate whether venous phase CT can reveal factors correlated with IVC filter tilting and abutment, and especially whether compression from adjacent structures affects the likelihood of filter tilting and abutment to the IVC wall.
2. Materials and methods
2.1. Patients and study design
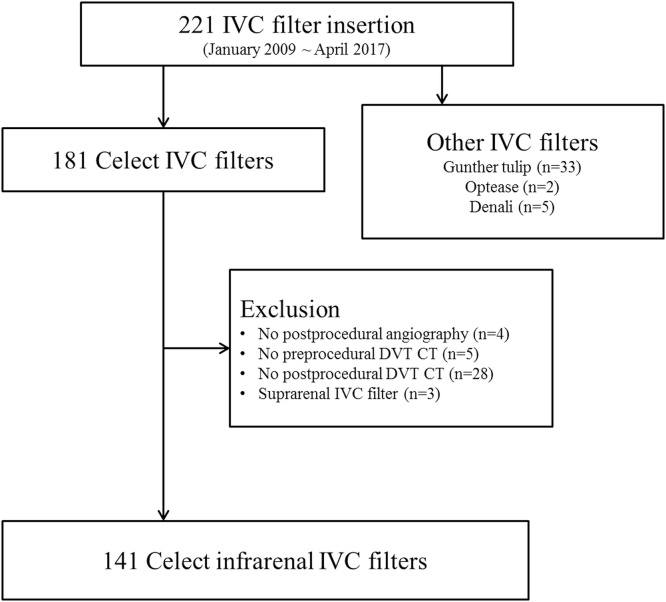
This retrospective study was approved by our institutional review board, and informed consent was waived. We reviewed images in the picture archiving and communication system (PACS) and electronic medical records to identify patients who underwent Celect IVC filter insertion (Cook Medical, Bloomington, Ind, USA) between January 2009 and April 2017. During that period, 221 IVC filters were inserted at our institution. Among 221 filters, 181 were Celect IVC filters, and the remaining were other filters (n = 40). Forty patients were excluded for the following reasons: (1) absence of postprocedural angiography (n = 4), (2) absence of preprocedural venous phase CT (n = 5), (3) absence of postprocedural venous phase CT (n = 28), and (3) suprarenal insertion of the IVC filter (n = 3). Exclusion criteria and patient enrollment data are shown in Fig. 1.
Fig. 1.
Flow chart of study enrollment.
IVC, inferior vena cava, DVT, deep vein thrombosis, CT, computed tomography.
2.2. IVC filter insertion and retrieval
All IVC filter insertions and retrievals were performed by one experienced interventional radiologist. After local anesthesia with 2% lidocaine (Jeil Lidocaine, Seoul, Korea), venous access was obtained either through the right internal jugular vein or right common femoral vein. Then inferior vena cavography was performed to identify the levels of renal vein insertion and to check for anatomical variants of the IVC prior to IVC filter deployment. All IVC filters were inserted into the infrarenal IVC. Post-procedure, anteroposterior vena cavography was obtained immediately after IVC filter deployment. Indications for IVC filter insertion are summarized in Table 1 and are categorized according to Society of Interventional Radiology guidelines [3].
Table 1.
Indications of IVC filter insertion.
| Therapeutic indications (evidence of PE or IVC, iliac, or femoropopliteal DVT) | 103 |
|---|---|
| Absolute or relative contraindication to anticoagulation | 93 |
| Massive PE with residual DVT in a patient at risk for further PE | 9 |
| Free-floating iliofemoral or IVC thrombus | 1 |
| Prophylactic indications | 38 |
|---|---|
| Multiple long-bone and pelvic bone fractures with BTK vein thrombosis | 35 |
| Intracranial hemorrhage with BTK vein thrombosis | 3 |
IVC – inferior vena cava.
DVT – deep vein thrombosis.
PE – pulmonary thromboembolism.
BTK – below the knee.
IVC filter retrieval was performed using the standard snare technique with a filter retrieval set (Cook Medical, Bloomington, Ind, USA). Complex retrievals (requiring additional devices, such as balloon catheters) or complicated retrievals (resulting in IVC laceration or rupture) were analyzed. Filter retrieval failure was also analyzed.
2.3. Filter tilting and image analysis
All enrolled patients had a pre- and post-procedural venous phase CT scan. The post-procedural CT scans were conducted for pre-retrieval evaluation or follow-up of deep vein thrombosis. All CT scans were performed using the deep-inspiration breath-hold technique. The scan range was from the top of the intrahepatic IVC to tip of the toe, and was reconstructed with 5 mm section thicknesses. Various image parameters were measured with pre- and post-procedural venous phase CT. The mean interval between pre-procedural CT and procedure was 6 days (range 0–315) and 77 days between procedure and postprocedural CT (range 1–1035), respectively. Filter tilt angle, IVC angle, and vertical position of the filter were measured on a three dimensional workstation (AquariusNET, Terarecon, San Mateo, Calif, USA) using post-procedural CT data. Filter tilt angle was determined by comparing the long axis of the filter and the long axis of the IVC, and the IVC angle was measured by comparing the long axis of the IVC at the level of renal vein insertion with the long axis of the IVC at the level of IVC filter. The vertical position of the IVC filter was determined by measuring the number of vertebral bodies from the renal vein junction to the lower margin of the IVC filter. Filter tip abutment to the IVC wall was defined as visual abutment of the IVC filter hook against the IVC wall on three dimensional CT data, and was determined by consensus between two readers. Based on these data, enrolled patients were divided between the filter tip abutting and non-abutting group.
Measurement of IVC diameter and morphology were performed using the PACS system (Infinitt PACS, Infinitt Heathcare, Seoul, Korea) based on pre-procedural CT. On axial CT images, IVC long and short transverse diameters were measured at a point 4 cm below the lowest renal vein connection to the IVC. Morphologic characterization of the IVC itself was categorized as oval, round, or crescent shaped by analyzing axial CT images of the IVC at the same position.
After obtaining these data, extrinsic compression factors causing direct indentation and filter tip abutment to the IVC wall were analyzed on pre- and postprocedure CT, and were agreed to by our 2 readers. Subsequently, these factors were analyzed in both the abutting and non-abutting group. Additionally, subgroup analyses of these factors were performed with respect to retrieval rate and failed, complex or complicated retrievals.
2.4. Statistical analysis
For statistical analysis of continuous variables, the averages of our 2 readers’ values were used. In univariate analysis, the independent sample t-test was applied for comparing continuous variables, and the Chi-square and Fisher’s exact tests were used for categorical variables. A filter tilt of 15° was the cutoff used to evaluate both groups, in accordance with a previous study [3]. Finally, correlation between various parameters and filter tip abutment to the IVC wall was investigated with multiple logistic regression analysis. Prior to this analysis, an ROC curve was constructed to determine the best cutoff value for continuous variables. For statistical analysis, continuous variables were dichotomized after ROC analyses. Statistical analysis was performed using MedCalc version 17.5 statistical software (MedCalc Software bvba, Ostend, Belgium) and a P value less than 0.05 was considered statistically significant.
3. Results
One hundred forty-one Celect IVC filter cases were finally enrolled in this study. Seventy-three were men and 68 were women, with a mean age of 63 years ±15 and range of 20–88 years. Among 141 patients, 52 patients were in the abutting group, and 89 patients were in the non-abutting group. Baseline patient demographic and imaging analysis data are summarized in Table 2.
Table 2.
Baseline patient characteristics and measurement data.
| Abutting group (n = 52) | Non-abutting group (n = 89) | P-value | |
|---|---|---|---|
| Age (range) | 64 ± 15 (range 20–88) | 63 ± 15 (range 25–87) | 0.567* |
| Sex (male:female) | 26:26 | 47:42 | 0.748** |
| Tilt angleº | 11.7 ± 5.5 | 6.4 ± 5.4 | <0.001* |
| IVC long diameter, mm | 23 ± 3.5 | 22.8 ± 3.6 | 0.743* |
| IVC short diameter, mm | 16 ± 3.7 | 16 ± 3.7 | 0.963* |
| Sum of IVC diameter, mm | 39 ± 5.1 | 37.8 ± 5.1 | 0.846* |
| Extrinsic compression | 14/52 | 8/89 | 0.009** |
| Over 15 degree tilt | 13/52 | 4/89 | 0.0003*** |
| IVC morphology | 0.0134** | ||
| Oval | 36 | 78 | |
| Round | 8 | 8 | |
| Crecent | 8 | 3 | |
| IVC angle° | 5.2 ± 7.1 | 5.3 ± 7.2 | 0.92* |
| Position (vertebral bodies from renal vein insertion) | 2.0 ± 0.6 | 1.9 ± 0.6 | 0.181* |
| Retrieval attempt | 37/52 (71%) | 63/89 (71%) | 0.963** |
| Retrieval success | 34/37 (92%) | 62/63 (98%) | 0.11** |
| Retrieval failure | 3/37 (8%) | 1/63 (2%) | 0.142*** |
| Complex or complicated retrieval | 4/37 (11%) | 1/63 (2%) | 0.061*** |
| Retrieval failure, complex or complicated retrieval | 7/37 (19%) | 2/63 (3%) | 0.012*** |
Independent t-test.
Chi-square test.
Fisher’s exact test.
Retrieval attempts were not statistically different between groups [37/52 (71%) in the abutting group and 63/89(71%) in the non-abutting group; p = 0.963]. Three retrieval failures were recorded in the abutting group and only one failure in the non-abutting group. The incidence of complex or complicated retrievals was higher in the abutting group than in the non-abutting group [4/37 (11%) vs. 1/63(2%), respectively]. Among 5 cases of complex or complicated retrievals, 2 additionally required a balloon-assisted technique, and the remaining 3 showed concealed IVC rupture, which was identified on cavography just after the filter was removed. However, the three patients with concealed IVC rupture did not showed hemodynamic changes during their hospital stay. Although, differences in complex or complicated retrievals alone were not statistically different between the groups (p = 0.142), the incidence of overall retrieval failure, complex retrieval, or complicated retrieval was statistically higher in the abutting group (7/37(19%)) than in the non-abutting group 2/63(8%)) (p = 0.012).
In analysis of pre-procedural CT, IVC diameters, including long axis, short axis, and the sum of both, were not statistically different between the groups (p > 0.05). However, morphological classification was significantly different between the groups (p = 0.013). An oval-shaped IVC on axial CT was the most common type in both groups.
On post-procedural venous CT, filter tilting was significantly higher in the abutting group (mean 11.7 ± 5.5°, range 0.7–25.6°) compared to the non-abutting group (mean 6.4 ± 5.4°, range 0–19.2°) (p < 0.001). However, neither the IVC angle nor the vertical position of the IVC filter were significantly different between the groups (p > 0.05).
This study evaluated whether direct external compression of the IVC was correlated to IVC filter tilting. External compression factors included aorta or iliac artery indentation of the IVC wall, vertebral bony spurs, and huge adjacent renal cysts. Presence of external compression factors was significantly different between the two groups (p < 0.05). In the abutting group, 14 of 52 patients (27%) had at least one of these risk factors, while 8 of 89 (9%) in the non-abutting group had at least one of these risk factors. Interestingly, in subgroup analysis of the external compression group, filter retrieval was attempted in 9/14 (64%) patients; among them, 3/9 (33%) had difficult retrieval (2 failures and 1 complex retrieval). However, in the non-abutting group (n = 8), there were 4/8 (50%) retrieval attempts, and there was no difficult retrievals. More information is given in Table 3.
Table 3.
Extrinsic compression factors of the inferior vena cava.
| Abutting group (n = 52) | Non-abutting group(n = 89) | p | |
|---|---|---|---|
| 14 (27%) | 8 (9%) | ||
| Extrinsic compression | 14 | 8 | 0.0094* |
| Aorta | 4 | 4 | |
| Iliac artery | 0 | 1 | |
| Vertebral bony spur | 8 | 2 | |
| Vertebral bony spur + Aorta | 1 | 1 | |
| Renal cyst | 1 | 0 | |
| None | 38 | 81 |
Chi-square test.
Following univariate analysis, filter tilt, presence of external compression, and crescent shape of the IVC were analyzed using multiple logistic regression. After ROC curve analysis, dichotomization using a cutoff value of 9.25° for filter tilt angle achieved maximum diagnostic performance (sensitivity 69.2%, specificity 76.4%). The results of the multiple logistic regression analyses are summarized in Table 4.
Table 4.
Multiple logistic regression analysis of factors associate to significant IVC filter tilt.
| Logistic Regression Coefficient | Standard Error | Wald Test | P value | Odds Ratio (95% CI) | |
|---|---|---|---|---|---|
| Extrinsic compression (+) | 1.52 | 0.58 | 6.85 | 0.0089 | 4.56 (1.16–14.23) |
| Filter tilt >9.25˚ | 2.32 | 0.47 | 24.18 | <0.0001 | 10.18 (4.03–25.68) |
| Crescent IVC | −0.05 | 0.75 | 0.004 | 0.9467 | 0.95 (0.22–4.12) |
| Constant | −1.93 | 0.39 | 24.73 | <0.0001 |
4. Discussion
Over the past few decades, the number of IVC filter placements has increased, and many retrievable filters are not being removed [4,8]. Prolonged presence of an IVC filter can lead to several complications, including filter component fracture, filter leg perforation of the IVC, filter migration, and IVC thrombosis [[9], [10], [11], [12]]. The most common reason for failure of an IVC filter retrieval procedure is tilting of the filter, with the tip of the filter becoming embedded in the wall of the IVC [7]. Although various techniques have been introduced regarding complex filter retrieval, these techniques are time consuming and increase the radiation dose compared to normal retrieval [7,8,[13], [14], [15], [16]]. To minimize difficulties with IVC filter retrieval, it is important to reduce filter tilt that occurs at the time of insertion. We hypothesized that careful evaluation of pre-procedural CT could reveal predisposing factors directly affecting filter tilting, such as direct, external compression of the IVC wall. Furthermore, by identifying these factors, we may be able to reduce filter tilting by preventing the filter from being deployed in a dangerous area.
The degree of IVC filter tilt is known to be correlated with the difficulty of its subsequent retrieval [14,17]. In recent studies, a tilt angle of 15° was the most commonly cited standard [3,18,19]. However, this degree of filter tilt does not always mean an IVC filter is abutting the IVC wall or embedding itself into the IVC wall, because there are other contributing factors, such as the diameter of the IVC, the presence of external compressing structures, or severe angulation of the IVC itself.
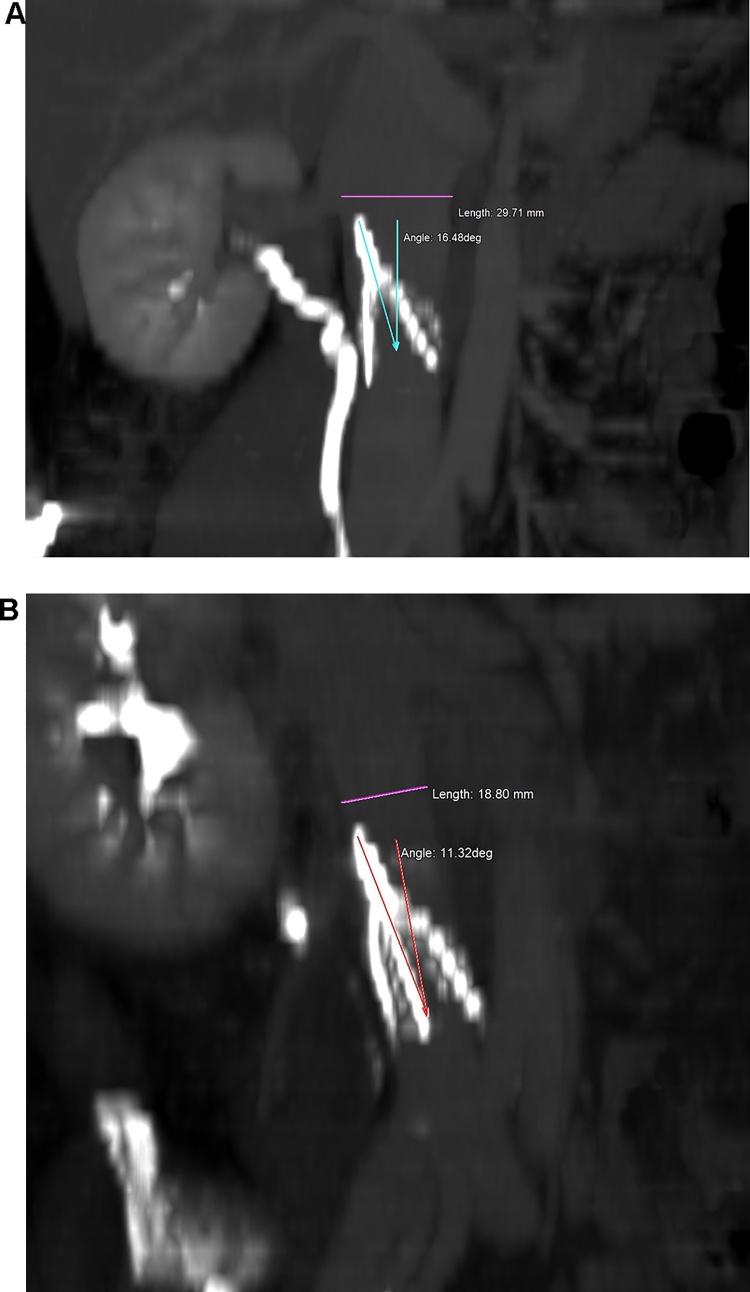
In our study, filter tip abutment to the IVC wall was analyzed. This characterizes IVC wall abutment by the IVC filter more objectively than IVC filter tilt angle alone. In our study, there were 17/141 (12%) cases of filter tilt angle greater than 15°, with 13 of those cases in the abutting group and 4 in the non-abutting group. Thirty-nine out of 52 patients in the abutting group showed less than 15° of filter tilt in relation to the IVC, and 21/52 (40%) patients even showed less than 10 degrees of filter tilt. If the diameter of the IVC is large, the filter tip may not impact the IVC wall, even if the filter tilt is severe (Fig. 2a). If the IVC diameter is small, however, the filter tip may contact the vessel wall even without a severe angle of tilt (Fig. 2b). The authors suggest that not only filter tilting over 15°, but also filter tip abutment to the IVC wall, may play an important role in filter tip embedding after prolonged indwelling. Although no single parameter was significantly different between the groups, the filter abutting group showed a statistically higher rate of either retrieval failure, complex retrieval, or complicated retrieval (p = 0.012). However, in this study, retrieval success rates were high in both groups (92% in the abutting group and 98% in the non-abutting group). The authors believe this is due to the relatively short indwelling time of the IVC filters compared to other studies (mean indwelling time: 21 days in abutting group and 23 days in non-abutting group, respectively) [17,20].
Fig. 2.
A. Thirty-two-year-old male patient shows IVC filter tilting. The tilting of the IVC filter is 16.5 degrees; however, the IVC filter tip has not abutted the IVC wall because the IVC diameter is large (29.7 mm long diameter, 14.7 mm short diameter).
B. Fifty-four-year-old male patient shows IVC filter tip abutment to the IVC wall. The tilting of the filter is 11.3 degrees, but the long diameter of the IVC is small (18.8 mm).
Theoretically, a severely angulated IVC could cause the tip of the filter to contact the IVC wall in the absence of any IVC filter tilt. However, our data showed no statistical difference between the two groups with respect to angulated IVC. And the vertical positioning of the IVC filter to the origin of the renal vein was not significantly different between the two groups. This might be related to a single operator inserting all the IVC filters, as there were no remarkable variations of the vertical positioning of the filter.
Previous studies have shown that the incidence of filter strut penetration into the IVC wall is increased when the IVC diameter is small (IVC diameter less than 24.2 mm) [21]. However, our study focused on filter tip abutment, and IVC diameter was not significantly different between both groups.
In our study, we divided the axial morphology of the IVC into three categories for analysis purposes. And those three categorizations were statistically different between the abutting and non-abutting group (P = 0.013). We theorized that a morphologically-collapsed (crescent-type) IVC might have a higher incidence of filter tip abutment than an oval- or round-shaped IVC. However, morphologic subtypes were not associated with a significant odds ratio in multiple logistic regression analysis when predicting filter abutment.
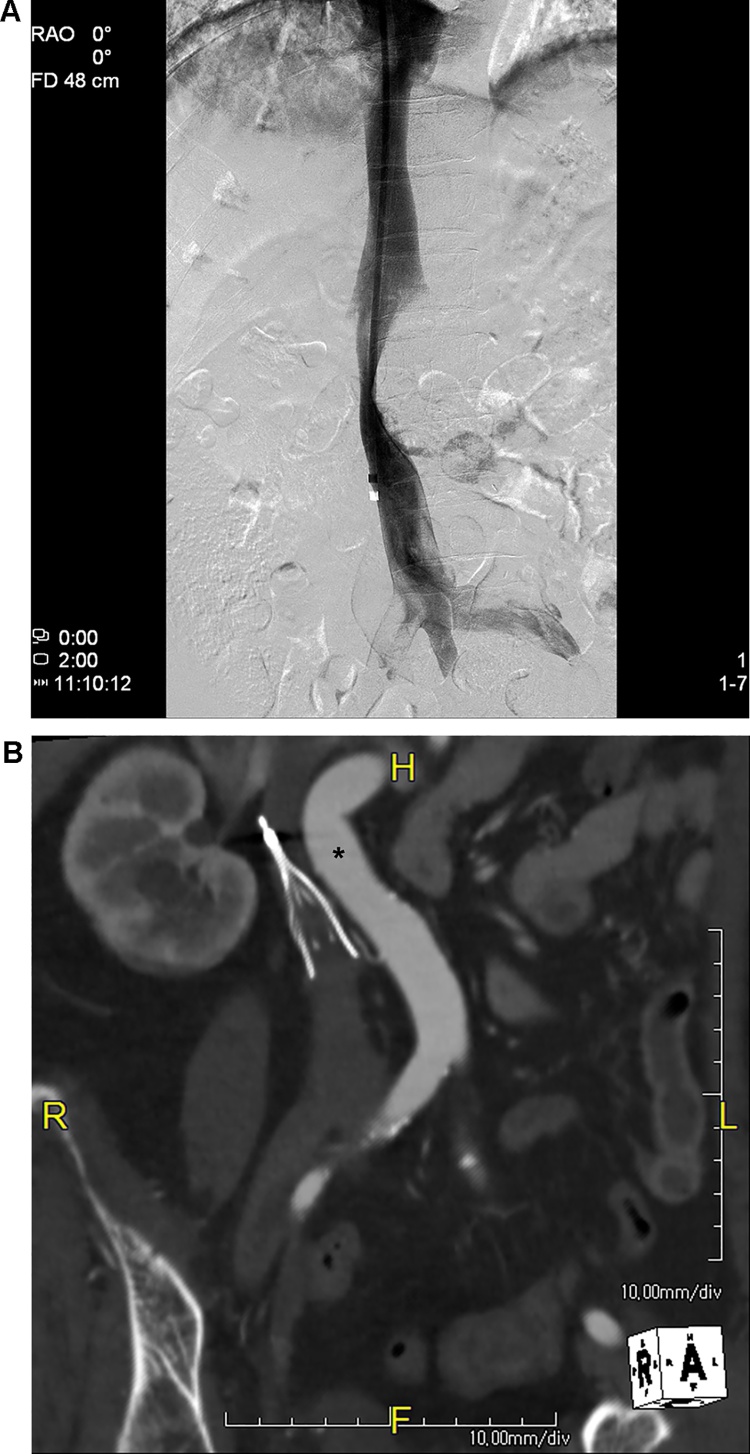
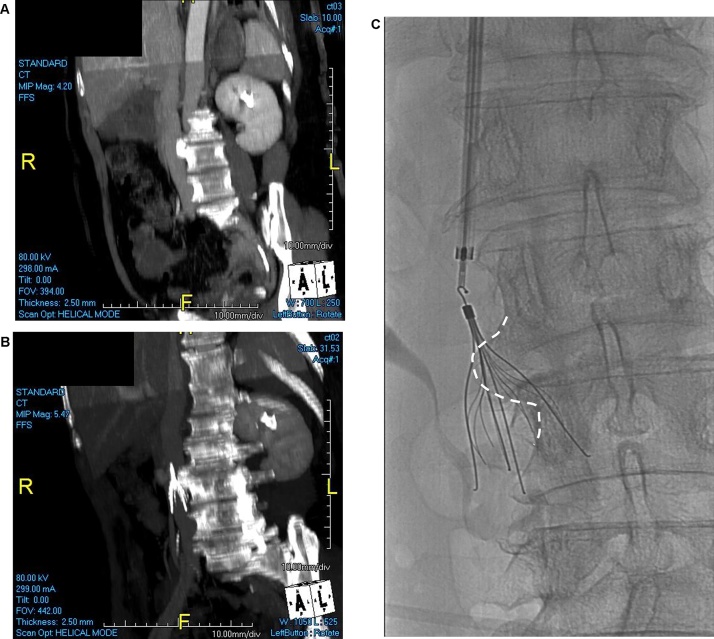
In the pre- and post-procedural CT analysis, we found direct, external compression of the IVC to be a risk factor for filter abutment. In our study, several anatomical structures were found to compress the IVC in certain patients: the abdominal aorta, the iliac artery, a vertebral bony spur, and a renal cyst (Fig. 3, Fig. 4). Identification of these external IVC compressing structures prior to filter insertion may prevent or minimize IVC filter tilting by allowing the operator to place the filter in an area of the IVC which avoids these problems. Although there were no statistical significant differences in subgroup analysis of the abutting group, likely due to the small number of cases, patients who had presence of external compression on the IVC showed a higher rate of difficult retrieval [3/9 (33%), 2 failures and 1 complex retrieval] in comparison to the non-abutting group (0/4, 0%). This suggests external compression factors could affect not only filter abutment but also difficulty in filter retrieval.
Fig. 3.
A. Infrarenal venacavography shows external compression of the IVC lumen.
B. Coronal reformatted computed tomography image shows the tip of the IVC filter embedded into the IVC wall and external IVC compression by a tortuous abdominal aorta (asterisk). This IVC filter could not be removed.
Fig. 4.
External IVC compression by vertebral spur results in IVC filter tilting.
A. Pre-procedural, multiplanar reconstructed CT image of 62-year-old female patient shows vertebral bony spur indenting the IVC lumen.
B. Maximal intensity, projection-reformatted image shows IVC filter abutment to the IVC wall.
C. This bony spur is not evident in the anteroposterior fluoroscopic image.
To the best of our knowledge, this is the first study to demonstrate that external vena cava compression is a risk factor for filter tip abutment. There has been no reliable data regarding an optimal IVC filter insertion point different from the usual placement zone, located between the IVC bifurcation and the renal vein origin. Meticulous analysis of pre-procedural CT and intraprocedural venography is required to avoid this CT risk factor, thereby reducing subsequent filter tilting and filter abutment to the IVC wall.
Our study has several limitations. First, this study was retrospective and represents the experience of a single center. Second, our patients had a relatively short indwelling time for the IVC filter, and we did not evaluate other risk factors of difficult retrieval, such as filter strut penetration. Further long term data is required to validate whether filter tip abutment is a potential risk of filter strut penetration and retrieval failure. Third, we evaluated only one type of IVC filter. We believe a carefully-designed, prospective study of various types of new, commercially available IVC filters should be performed. Fourth, most of our cases had filters inserted using the internal jugular vein approach, so we did not separately analyze results of filter insertion through the femoral vein.
5. Conclusions
In this study, higher IVC filter tilt, existence of external compression on CT, and IVC morphological differences were significantly different between the filter tip abutting and non-abutting groups. External compression on the IVC and filter tilt over 9.25° were demonstrated to be risk factors of filter tip abutment to the IVC wall. Careful evaluation of pre-procedural venous CT prior to IVC filter insertion is necessary to avoid these predictable risk factors.
Conflict of interest statement
All authors (Sang Yub Lee and Jongmin Lee) declare that they have no conflicts of interest.
Acknowledgments
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF-2017R1C1B5075931).
Contributor Information
Sang Yub Lee, Email: sangyub@knu.ac.kr.
Jongmin Lee, Email: jonglee@knu.ac.kr.
References
- 1.Hammond C.J., Bakshi D.R., Currie R.J. Audit of the use of IVC filters in the UK: experience from three centres over 12 years. Clin. Radiol. 2009;64(5):502–510. doi: 10.1016/j.crad.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Athanasoulis C.A., Kaufman J.A., Halpern E.F., Waltman A.C., Geller S.C., Fan C.M. Inferior vena caval filters: review of a 26-year single-center clinical experience. Radiology. 2000;216(1):54–66. doi: 10.1148/radiology.216.1.r00jl1254. [DOI] [PubMed] [Google Scholar]
- 3.Caplin D.M., Nikolic B., Kalva S.P. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J. Vasc. Interv. Radiol. 2011;22(11):1499–1506. doi: 10.1016/j.jvir.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 4.Angel L.F., Tapson V., Galgon R.E., Restrepo M.I., Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J. Vasc. Interv. Radiol. 2011;22(11):1522–1530. doi: 10.1016/j.jvir.2011.08.024. [DOI] [PubMed] [Google Scholar]
- 5.Ray C.E., Jr., Mitchell E., Zipser S., Kao E.Y., Brown C.F., Moneta G.L. Outcomes with retrievable inferior vena cava filters: a multicenter study. J. Vasc. Interv. Radiol. 2006;17(10):1595–1604. doi: 10.1097/01.RVI.0000239102.02956.65. [DOI] [PubMed] [Google Scholar]
- 7.Kuo W.T., Cupp J.S., Louie J.D. Complex retrieval of embedded IVC filters: alternative techniques and histologic tissue analysis. Cardiovasc. Intervent. Radiol. 2012;35(3):588–597. doi: 10.1007/s00270-011-0175-1. [DOI] [PubMed] [Google Scholar]
- 8.Iliescu B., Haskal Z.J. Advanced techniques for removal of retrievable inferior vena cava filters. Cardiovasc. Intervent. Radiol. 2012;35(4):741–750. doi: 10.1007/s00270-011-0205-z. [DOI] [PubMed] [Google Scholar]
- 9.Oh J.C., Trerotola S.O., Dagli M. Removal of retrievable inferior vena cava filters with computed tomography findings indicating tenting or penetration of the inferior vena cava wall. J. Vasc. Interv. Radiol. 2011;22(1):70–74. doi: 10.1016/j.jvir.2010.09.021. [DOI] [PubMed] [Google Scholar]
- 10.Piecuch J., Wiewiora M., Nowowiejska-Wiewiora A., Szkodzinski J., Polonski L. Perforation of inferior vena cava during filter placement. Vasa. 2011;40(2):157–162. doi: 10.1024/0301-1526/a000087. [DOI] [PubMed] [Google Scholar]
- 11.Nicholson W., Nicholson W.J., Tolerico P. Prevalence of fracture and fragment embolization of bard retrievable vena cava filters and clinical implications including cardiac perforation and tamponade. Arch. Intern. Med. 2010;170(20):1827–1831. doi: 10.1001/archinternmed.2010.316. [DOI] [PubMed] [Google Scholar]
- 12.Stawicki S.P., Sims C.A., Sharma R. Vena cava filters: a synopsis of complications and related topics. J. Vasc. Access. 2008;9(2):102–110. [PubMed] [Google Scholar]
- 13.Kuo W.T., Odegaard J.I., Louie J.D. Photothermal ablation with the excimer laser sheath technique for embedded inferior vena cava filter removal: initial results from a prospective study. J. Vasc. Interv. Radiol. 2011;22(6):813–823. doi: 10.1016/j.jvir.2011.01.459. [DOI] [PubMed] [Google Scholar]
- 14.Cho E., Lim K.J., Jo J.H., Jung G.S., Park B.H. Failed inferior vena cava filter retrieval by conventional method: analysis of its causes and retrieval of it by modified double-loop technique. Phlebology. 2015;30(8):549–556. doi: 10.1177/0268355514545353. [DOI] [PubMed] [Google Scholar]
- 15.Stavropoulos S.W., Ge B.H., Mondschein J.I., Shlansky-Goldberg R.D., Sudheendra D., Trerotola S.O. Retrieval of tip-embedded inferior vena cava filters by using the endobronchial forceps technique: experience at a single institution. Radiology. 2015;275(3):900–907. doi: 10.1148/radiol.14141420. [DOI] [PubMed] [Google Scholar]
- 16.Van Ha T.G., Vinokur O., Lorenz J. Techniques used for difficult retrievals of the gunther tulip inferior vena cava filter: experience in 32 patients. J. Vasc. Interv. Radiol. 2009;20(1):92–99. doi: 10.1016/j.jvir.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Zhu X., Tam M.D., Bartholomew J., Newman J.S., Sands M.J., Wang W. Retrievability and device-related complications of the G2 filter: a retrospective study of 139 filter retrievals. J. Vasc. Interv. Radiol. 2011;22(6):806–812. doi: 10.1016/j.jvir.2011.01.430. [DOI] [PubMed] [Google Scholar]
- 18.Dinglasan L.A., Oh J.C., Schmitt J.E., Trerotola S.O., Shlansky-Goldberg R.D., Stavropoulos S.W. Complicated inferior vena cava filter retrievals: associated factors identified at preretrieval CT. Radiology. 2013;266(1):347–354. doi: 10.1148/radiol.12120372. [DOI] [PubMed] [Google Scholar]
- 19.Hong S., Park K.M., Jeon Y.S. Can pre-retrieval computed tomography predict the difficult removal of an implementing an inferior vena cava filter? Vasc. Specialist Int. 2016;32(4):175–179. doi: 10.5758/vsi.2016.32.4.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuo W.T., Tong R.T., Hwang G.L. High-risk retrieval of adherent and chronically implanted IVC filters: techniques for removal and management of thrombotic complications. J. Vasc. Interv. Radiol. 2009;20(12):1548–1556. doi: 10.1016/j.jvir.2009.08.024. [DOI] [PubMed] [Google Scholar]
- 21.Lee J.K., So Y.H., Choi Y.H. Clinical course and predictive factors for complication of inferior vena cava filters. Thromb. Res. 2014;133(4):538–543. doi: 10.1016/j.thromres.2014.01.004. [DOI] [PubMed] [Google Scholar]