Abstract
Background
Stress and obesity are interrelated and common among low-income adults. Mind–body interventions have been shown to reduce psychological distress and have been incorporated into many weight loss interventions. However, few of these programs have incorporated a telephone coaching component.
Objective
We designed and piloted a novel weight loss telephone coaching intervention for this population and examined its effectiveness on weight loss and improvements in health behaviors in obese community health center patients.
Methods
This was a 6-month, single-arm, prospective, pre–post pilot study. The study took place at a community health center near Boston, Massachusetts. Participants were 27 overweight and obese community health center patients. The intervention consisted of one in-person intake with the registered dietitian, trained in mind–body approaches, and approximately 1 phone coaching session every 2 weeks for 6 consecutive months. Anthropometric data consisted of weight, body mass index (BMI), and blood pressure. Questionnaires consisted of the Perceived Stress Scale-10 item, the CIGNA Healthy Eating Survey, Section H: Behavioral Eating, a physical activity questionnaire, and a nutritional habits questionnaire. We used paired samples t tests to assess pre–post changes in weight, BMI, blood pressure, perceived stress, behavioral eating, and physical activity. We also conducted semistructured exit interviews to learn about participants’ experiences in this program.
Results
There was a trend toward weight reduction (P < .1, Cohen’s d = 0.33) and significant improvements in systolic blood pressure (P = .001, Cohen’s d = 0.72), perceived stress (P = .001, Cohen’s d = 0.75), and behavioral eating (P = .009, Cohen’s d = 0.54). Improvements in weight were sustained 6 months after completion of the intervention.
Conclusion
Results suggest that a telephone nutrition health coaching intervention is feasible and may facilitate weight loss in obese community health center patients. Future randomized-controlled studies are warranted to better understand these improvements.
Clinicaltrials.gov registration
Keywords: weight loss, mind–body medicine, telemedicine, behavior therapy, obesity
Introduction
Obesity is associated with leading causes of preventable death including heart disease, stroke, type 2 diabetes, and cancer.1 More than 36% of adults in the United States are obese. Vulnerable populations including underrepresented minorities and persons of low socioeconomic status are at particular risk.1–3 Furthermore, annual health-care costs for obese patients are on average $1429 higher than for nonobese patients.4
Stress has been associated with obesity, weight gain, and emotional eating,5,6 and chronic life stress has been linked to greater preference for energy-dense foods and weight gain.7,8 In addition to psychosocial distress, depression and anxiety have been shown to enhance the desire to eat, leading to greater food intake and weight gain.7–9 The link between stress and weight gain suggests that interventions that decrease stress may be useful for promoting weight loss.
Interventions incorporating mind–body practices (MBPs) such as meditation, mindfulness, yoga, and/or deep breathing have been shown to reduce psychological distress and have been incorporated into many weight loss interventions.10–15 In addition, they have been shown to reduce emotional- and binge-eating, promote behavior change, and improve depression and anxiety. Furthermore, it has been suggested that MBPs have efficacy in weight loss.14,15 MBPs elicit the relaxation response (RR), the physiological state characterized by downregulation of the sympathetic nervous system.16
Persons of low socioeconomic status and minorities have reduced access to MBPs.17 In addition, a variety of factors including limited access to transportation, working hours, geographic isolation, chronic health conditions, and forgetting about appointments can reduce participation in medical care.18,19 Telephone coaching is one strategy that has been incorporated into many interventions to increase access to care while providing relevant information and ongoing support.20,21 Interventions incorporating telephone coaching as a delivery model have demonstrated improvements in a number of metabolic syndrome parameters as well as weight loss and improvements in health behaviors.20–23
Given the cost-effectiveness of telehealth interventions, particularly for low-income populations with less access to care, research in this area is burgeoning.20 Some of the active ingredients in these telephone coaching interventions include working one-on-one with participants to develop specific, individualized behavioral and diet plans, encouraging participants to weigh themselves and report to the coach throughout the program, and personal relationships established between the coach and patients.21–23 In addition, the frequency of calls during a telephone-based intervention may influence success, with more calls associated with lower fat and higher fiber intake and greater weight loss.23 Studies have successfully used telephone coaching to deliver multimodal behavior change interventions, including the Diabetes Prevention Program, consisting of goal-setting, self-monitoring, diet/activity modification, and problem-solving.21,22
Although several studies have examined the effectiveness of MBPs or telephone coaching interventions for weight loss, none to our knowledge have combined these 2 approaches or used a dietitian trained in mind–body approaches to deliver the intervention. In response to challenges that low-income patients face, we developed the Total Lifestyle Coaching Program, delivered predominantly by telephone over the course of 6 months. This program used a dietitian trained in MBPs to personalize telephone-based nutrition counseling for obese patients who received care at a community health center. We aimed to examine feasibility and acceptability of this pilot program in this population and to evaluate its effect on weight loss, blood pressure, perceived stress, and behavioral eating patterns.
Methods
Setting/Design
This was a single-arm, prospective, pre–post pilot study that took place at a community health center near Boston, Massachusetts, between the spring of 2014 and 2015. Participants were offered a 6-month intervention. This study was approved by the Partners Institutional Review Board and participants gave written, informed consent. Data were collected at consent (baseline) and after completing the 6-month intervention (end point).
Sample
Participants were eligible for this study if they received their primary care at the health center, had a BMI exceeding 25, were at least 21 years, spoke English, and had access to a telephone. Participants who were pregnant or attempting to become pregnant were excluded. Participants were recruited through physician referrals and flyers in clinics. In addition, eligible patients, identified by the dietitian, were mailed letters describing the study and invited to enroll.
Measures
The study staff collected anthropometric data and delivered questionnaires to participants at 2 in-person visits: at consent (baseline) and after completing the 6-month intervention (end point). A study staff member administered the questionnaires and recorded participants’ answers directly into the study database. Anthropometric data consisted of weight, BMI, and blood pressure. Questionnaires consisted of the Perceived Stress Scale-10 item (PSS-10), the CIGNA Healthy Eating Survey, Section H: Behavioral Eating (referred to hereafter as the CIGNA Behavioral Eating Survey or CIGNA), a physical activity questionnaire, and a nutritional habits questionnaire.24–27 We also extracted weight data from participants’ medical records 6 months after the end of the intervention.
The PSS-10 measures nonspecific perceived stress. Total scores range from 0 to 40 with higher scores indicating higher levels of stress.25 The CIGNA Behavioral Eating Survey24 measures unhealthy or emotional eating patterns, including questions such as “I find food comforting, like being with a familiar friend” and “My eating feels out of control.” We used the first 7 items of the questionnaire; higher scores indicate a healthier eating pattern. The physical activity questionnaire assessed the number of minutes spent in different types of physical activity per week including walking, jogging, biking, strength training, low-intensity exercise, and other activities.27 For total physical activity scores, we calculated the number of metabolic equivalents of task (MET) minutes per week for each type and duration of physical activity and summed these. A MET describes the energy expenditure of a type of physical activity and is the ratio between the rate of energy used during an activity to the rate of energy used at rest. Eating habits were assessed by asking participants the number of times a day over the last month they had eaten the following types of food: fruits and vegetables; whole grains; lean meats, fish, or egg whites; high-fat dairy; fatty foods and snacks; sugary foods and drinks; and red and processed meats.26
We also conducted semistructured exit interviews with participants asking about their experiences participating in the program. Interviews were approximately 15 min each and were audio recorded. An iterative, immersion/crystallization approach28 was used to qualitatively analyze transcripts of the interviews. Two independent raters read the transcripts separately, met to discuss the major themes that emerged from the transcripts, went back to the transcripts and coded them based upon the agreed upon coding scheme, and then met again several times to discuss their findings and resolve discrepancies until an inter-rater reliability of 80% was achieved.
Intervention
The total lifestyle coaching program was delivered by a registered dietitian who was trained in motivational interviewing and also the Benson-Henry Institute’s Stress Management and Resiliency Training, Relaxation Response Resiliency Program (SMART-3RP).16 This multimodal resiliency program targets stress with 4 main components: mind–body skills (participants learn a variety of meditation techniques, mini relaxations, walking meditation, and yoga), traditional stress management techniques, healthy lifestyle behaviors (sleep, exercise, nutrition, and social support), and cognitive reappraisal and adaptive coping skills (borrowed from cognitive behavioral therapy, acceptance and commitment therapy, and positive psychology). A dietitian was chosen to administer the intervention given its focus on nutritional coaching and weight loss. The intervention incorporated elements from the SMART-3RP with nutritional coaching and consisted of one in-person intake with the registered dietitian at the health center, and approximately 1 phone coaching session every 2 weeks for 6 consecutive months. For the in-person intake, there were 2 primary goals: (1) to establish rapport between the participant and provider and (2) to conduct an initial assessment of participants’ MBPs, sleep habits, diet patterns, and exercise levels. The dietitian used this assessment to provide calorie-adjusted meal plans and to help participants set individualized goals.
The calorie-adjusted meal plans are a weight loss tool developed and used by the Massachusetts General Hospital Department of Nutrition and Food Services that guides patients in choosing balanced meals utilizing food lists and portion sizes within an individualized calorie level. Participants were provided paper logs for self-monitoring their food, exercise, and any type of relaxation strategy used (breathing, guided meditation, and prayer). The dietitian also provided each participant materials developed as the Total Lifestyle Coaching series (sleep and weight, mindfulness, goal setting, Healthy Eating Plate, exercise, and mini meditations; see Appendix 1). A guided meditation CD developed by the Benson-Henry Institute was also provided to participants. A list of meditation apps was provided to participants who did not have a CD player. All other materials given to participants were based on individual needs as determined during telephone follow-ups.
The telephone coaching sessions incorporated each of the 4 program components: elicitation of the RR to buffer stress, sleep, nutrition, and exercise. At each session, the dietitian discussed participants’ changes in weight and diet, stress, use of MBPs, sleep, and exercise. The dietitian also adjusted participants’ personalized goals based on progress. After reviewing each of the core components, the session was focused primarily on the specific concern that a given participant was working on changing. There was an overall effort at each session to help participants realize the interconnectedness of the program components regardless of their individual focus. The sessions were documented in the medical record and provided the starting point for each follow-up session. At the end of each session, the participants were scheduled for their next follow-up in the provider’s schedule. Participants were encouraged to call if they could not make the time and to call the provider back if they missed a call.
Analyses
We used paired samples t tests to assess pre–post changes in weight, BMI, blood pressure, perceived stress, behavioral eating, and physical activity and to assess changes in weight from baseline to 6 months after completion of the intervention. Based upon our a priori hypotheses regarding potential mechanisms, we conducted secondary analyses using linear regressions to assess associations between stress, behavioral eating, and weight loss. We conducted baseline and end point analyses with an intent-to-treat sample (those who completed at least baseline assessments) and a completer sample (participants who completed both baseline and end point assessments). When participants did not complete end point assessments, we used medical records to collect weight and blood pressure closest to the per protocol timing of participants’ end point visits (i.e., 6 months postintake). For psychosocial questionnaires, last value carried forward (i.e., the baseline value) was used for missing end point data.
Fidelity Check
Participants’ medical records were reviewed for documentation of discussion of each of the 4 main intervention components (stress/RR, sleep, exercise, and diet) for each telephone session.
Results
Enrollment
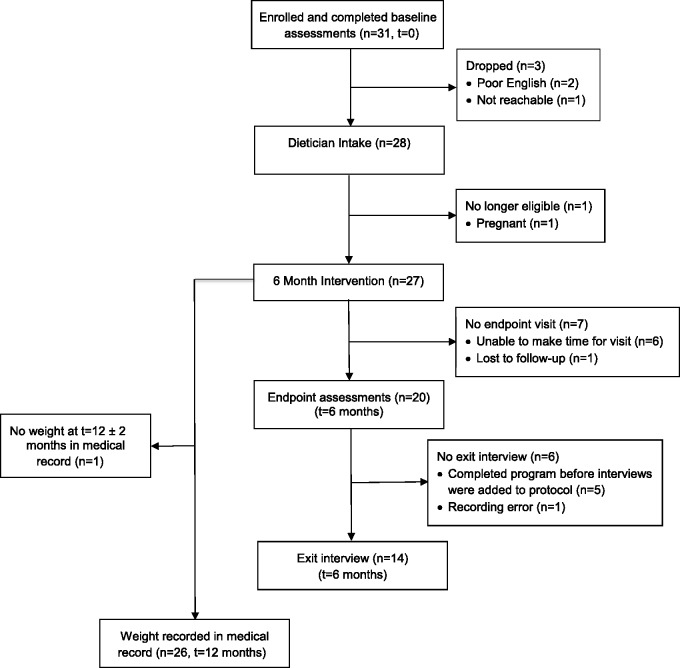
We enrolled 31 participants, 4 of whom dropped or were lost to follow-up (Figure 1). Two participants dropped immediately after enrollment due to difficulties communicating and understanding English, 1 participant was lost to follow-up after consent, and 1 became pregnant and was no longer eligible. These participants’ data were not included in any analyses. All 27 participants completed baseline assessments (intent-to-treat sample) and 20 completed postintervention assessments (Figure 1). Intent-to-treat participants received an average of 7 (SD = 2.3) phone coaching sessions totaling 146 min (SD = 77). Completers received an average of 8 (SD = 1.4) sessions totaling 162 (SD = 70) min. Out of the 20 completers, 14 completed exit interviews.
Figure 1.
Participant Flow Diagram. N = number of participants, t = time point.
Demographics
Table 1 describes the sample demographics. Within the intent-to-treat sample, participants were predominantly female (85%) and had a mean age of 55 (SD = 11.7). The majority of participants were white (85%); 4 were Hispanic (15%). About half of the participants were college-educated (52%) and slightly more were married (59%). More than half of the participants provided regular care to children (30%), grandchildren (15%), and/or a disabled or ill person (26%). Sociodemographic characteristics of the 20 individuals who completed end point measures were similar.
Table 1.
Population Demographics for Intent to Treat (n = 27) and Completers (n = 20).
| n = 27 |
n = 20 |
|
|---|---|---|
| n (%) | n (%) | |
| Age (mean ± SD), years | 55 ± 12 | 59 ± 11 |
| Female gender | 23 (85) | 16 (80) |
| Race | ||
| White | 23 (85) | 19 (95) |
| African-American | 2 (7) | 1 (5) |
| Other | 2 (7) | 0 (0) |
| Hispanic or Latino ethnicity | 4 (15) | 2 (10) |
| Education | ||
| High school | 10 (37) | 7 (35) |
| Diploma program | 2 (7) | 2 (10) |
| College | 14 (52) | 10 (50) |
| Graduate school | 1 (4) | 1 (5) |
| Marital status | ||
| Married | 16 (59) | 12 (60) |
| Living with significant other | 3 (11) | 1 (5) |
| Single | 8 (30) | 7 (35) |
| Provide regular care to | ||
| Children | 8 (30) | 7 (35) |
| Grandchildren | 4 (15) | 4 (20) |
| Disabled/ill person | 7 (26) | 5 (25) |
| Do not provide care | 13 (48) | 9 (45) |
Abbreviation: SD, standard deviation.
Anthropometric Outcomes
Within the intent-to-treat sample, there was a significant improvement in systolic blood pressure from baseline to end point (130–122 mm Hg, P = .001, Cohen’s d = 0.72; Table 2) and a nonsignificant improvement in weight (209–205 lbs, P = .095, Cohen’s d = 0.33) and BMI (P = .058, Cohen’s d = 0.38). Six months following study completion, weight loss was largely maintained (N = 26, mean weight = 206 lbs). Among the sample of 20 completers, significant improvements were found across all anthropometric measures, with the exception of diastolic blood pressure. Completers lost an average of 8 pounds (P = .011, Cohen’s d = 0.63), and BMI decreased on average by 1.5 points (P = .006, Cohen’s d = 0.69). Systolic blood pressure also decreased by 8 mm Hg (P = .006, Cohen’s d = 0.69; Table 2).
Table 2.
Anthropometric, Stress, and Behavioral Eating Data.
| Intent to Treat, n = 27 |
Completers, n = 20 |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline M (SD) | End point M (SD) | P | Cohen’s d | Baseline M (SD) | End point M (SD) | P | Cohen’s d | |
| Weight (lbs) | 209 (35.5) | 205 (36.7) | .095 | 0.33 | 211 (35.9) | 203 (35.8) | .011 | 0.63 |
| BMI | 36.5 (5.2) | 35.6 (5.6) | .058 | 0.38 | 36.8 (5.4) | 35.3 (5.6) | .006 | 0.69 |
| SBP | 130 (12.1) | 122 (8.9) | .001 | 0.72 | 131 (13.0) | 123 (9.5) | .006 | 0.69 |
| DBP | 78 (13.4) | 75 (8.0) | .273 | 0.22 | 75 (13.6) | 74 (8.3) | .695 | 0.09 |
| CIGNA | 11 (5.4) | 13 (5.8) | .009 | 0.54 | 12 (5.2) | 14 (5.2) | .003 | 0.76 |
| PSS | 19 (7.1) | 13 (7.5) | .001 | 0.75 | 19 (6.8) | 12 (6.7) | <.001 | 0.94 |
Abbreviations: BMI, body mass index; CIGNA, CIGNA Behavioral Eating Survey; DBP, diastolic blood pressure; M, mean; PSS, Perceived Stress Scale 10-item; SBP, systolic blood pressure; SD, standard deviation.
Psychosocial Outcomes
Scores on the CIGNA Behavioral Eating Survey and the Perceived Stress Scale improved following completion of the intervention. In the intent-to-treat sample, participants improved 2 points on the CIGNA (P = .009, Cohen’s d = 0.54) and reported decreased stress levels on the PSS-10 with an average score decrease of 6 points (P = .001, Cohen’s d = 0.75). Among completers, scores on the CIGNA also increased by 2 points (P = .003, Cohen’s d = 0.76) and scores on the PSS-10 decreased by 7 points (P < .001, Cohen’s d = 0.94; Table 2). Among completers, there was a trend toward increased physical activity (350–512 MET-min/week, P = .11).
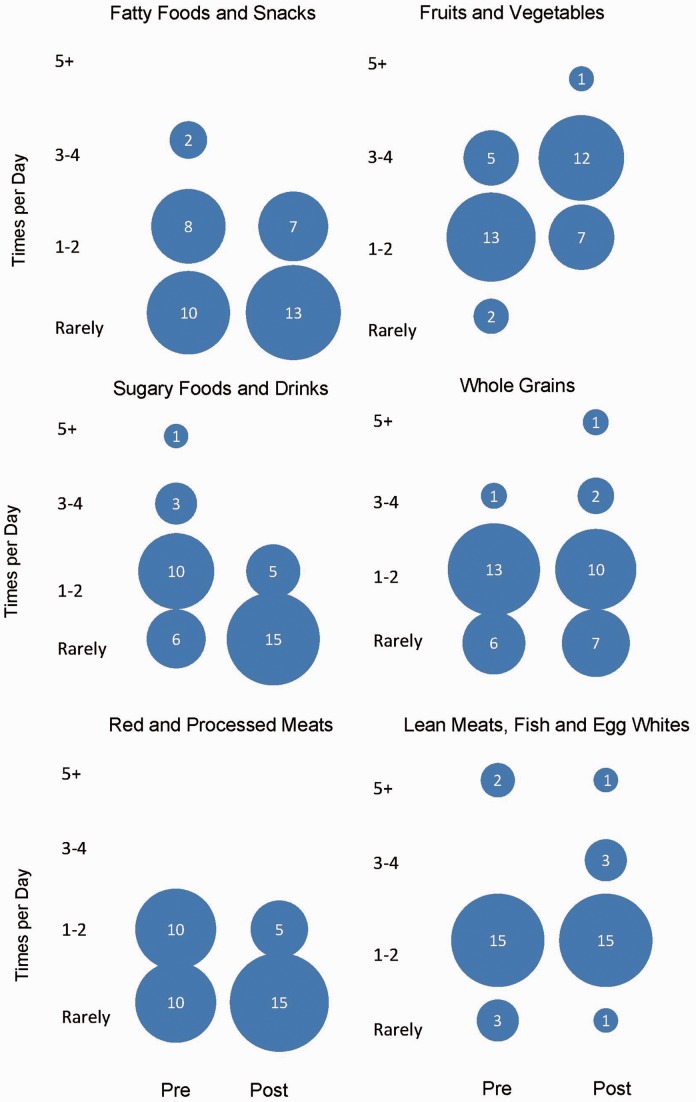
There was also a trend toward improved food choices from baseline to end point with completers increasing their intake of (1) lean meats, fish, and egg whites; (2) fruits and vegetables; and (3) whole grains and decreasing their intake of (1) red meat, (2) fatty foods and snacks, and (3) sugary foods and drinks (Figure 2).
Figure 2.
Participant Eating Habits at Baseline (Pre) and End Point (Post). The y-axis shows the number of times per day each type of food was consumed. Circle size is proportional to the number of respondents which is embedded in the middle of the circle.
Linear regression analyses demonstrated that improvements in scores on the CIGNA Behavioral Eating Survey were significantly associated with weight loss for the intent-to-treat group (F(1,25) = 4.9, B = − 1.5, SE(B) = 0.67, P = .036). Similarly, decrease in stress as measured by the PSS-10 was associated with improvements in behavioral eating (F(1, 25) = 4.4, B = −0.2, SE(B) = 0.1, P = .047). However, decrease in stress was not associated with weight loss (F(1, 25) =1.040, B = −0.303, SE(B) = 0.297, P = .318). Among completers, there was also a significant association between decreased stress and improved CIGNA scores (F(1, 18) = 4.6, B = −0.2, SE(B) = 0.1, P = .045). No other associations were significant in this smaller sample.
Analysis of the exit interviews showed enthusiasm for the coaching program among participants (Table 3). Participants attributed the success of the program to the personal connection that came from the one-on-one phone conversations with the registered dietitian. All participants expressed feeling emotionally supported by the dietitian and connected to the program. Participants also found benefit in the convenience of the phone sessions and the personalized education and feedback they received from the dietitian. In addition, participants learned how to apply mindfulness to their food choices and noticed improvements in awareness of hunger cues and eating behaviors. Participants also noted challenges with engaging in formal meditation practice. Other challenges included health and life distractions interfering with participants’ abilities to engage with and commit to the program. Suggested areas for program improvement included a more comprehensive discussion of sleep challenges and built-in time for exercise.
Table 3.
Qualitative Data From Exit Interviews.
| Coding Themes | n | (%) | Quotation |
|---|---|---|---|
| A. Benefits of the Program | |||
| Connected to program | 14 | (100) | “When I was on the phone with her, it was all about me. It was like she didn’t have another patient.” |
| Convenience | 9 | (64) | “It’s better than going into the doctor because you don’t have to get dressed and go. If I ever had a problem, I would email her and she would email me back.” |
| Personalized education | 12 | (86) | “She sent me emails on certain foods that I might want to eat that would help me because she kn(e)w that I couldn’t exercise.” |
| Accountability | 9 | (64) | “Once it’s on paper and you see it, you plan accordingly for the next meal or you try to fix what didn’t work well.” |
| Mind–body benefits | 8 | (57) | “Meditation helped me get to sleep. I would use it when I would wake up during the night to get back to sleep, so there was definite value in that.” |
| Mindful decision-making | 10 | (71) | “The other night I said ‘Oh I’m gonna get an ice cream,’ and I just said ‘Nope’. And I didn’t.” |
| Health behavior improvements | 13 | (93) | “Reading a book, listening to some music or whatever just to unwind helped a lot … I was strict with myself about being in bed at a certain time every night to ensure that I got enough sleep.” |
| Confidence | 6 | (43) | “I lost the weight, my clothes feel better, and I feel great.” |
| B. Requirements to be Successful | |||
| Readiness to change | 8 | (57) | “It’s making that connection to yourself, and standing in your own truth … I was so sick of saying I’m fat … It’s taking control of your life.” |
| Self-care | 5 | (36) | “Just focusing on myself more, as opposed to being worried about everyone else. I’m a person too and I need to sit back and take time for me.” |
| C. Program Challenges | |||
| Mind–body challenges | 7 | (50) | “I’m trying to listen (to the meditation CD, but) my mind is going to other things. I just can’t focus. I didn’t really think I needed [meditation] all that much. Maybe I do and I just don’t know I do.” |
| Health distractions | 9 | (64) | “There were a lot of bumps in the road … my physical health.” |
| Life distractions | 10 | (71) | “Once I got started, there were other things that I needed to do either work-wise, family-wise, school-wise, so I think if I had been more ready to go, I think it would have been better.” |
| Motivation | 9 | (64) | “I wasn’t really motivated.” |
Review of medical records to assess intervention fidelity showed documentation of all 4 of the main program components for 89% of the visits and documentation of 3 of the 4 components for 97% of the visits. Some components were not covered either because they were not problematic for a participant (e.g., sleep was good) or due to time limitations in which case they were addressed during subsequent coaching sessions.
Discussion
We found that in this 6-month mind–body and nutrition telephone coaching program, subjects had modest weight loss and clinically meaningful improvements in blood pressure. In addition to physical health improvements, participants noted decreased stress and improved behavioral eating patterns, physical activity, and eating habits after participating in the program. Not surprisingly, participants who completed the program showed better results on all outcomes. The fact that weight loss was maintained even after the program ended may suggest that participants learned important skills and successfully implemented sustained lifestyle changes. Because the intervention was multidimensional, different participants were able to take advantage of the tools they found most useful.
Many weight loss trials demonstrate weight regain after program completion.29,30 People are at highest risk for weight regain during the period after initial weight loss and rarely recover from this regain.31 One study found that perceived stress was associated with weight regain across gender, race, and treatment condition.32 Research has shown that many eating behaviors, such as behavioral or emotional eating, are used as maladaptive coping mechanisms in response to stress and can lead to weight gain.33 MBPs have been used to help reduce stress.34,35 Our intervention’s effect on perceived stress may explain why weight loss was maintained. This conclusion is supported by our linear regression results demonstrating an association between decreases in stress and improvements in behavioral eating patterns, which, in turn, were related to weight loss. In line with previous research, these associations suggest that stress reduction may be a mechanism contributing to weight loss in this program.6,36
Our participants’ success in losing and maintaining weight was likely enhanced by their own self-monitoring and involvement in their progress. By completing logs and weight check-ins with the dietitian on the phone, these participants practiced the regular self-monitoring that has been shown to increase self-awareness and promote sustained behavior change.37
The sustained involvement of a dietitian trained in MBPs was likely another contributor to successful weight loss in this study. Exit interviews suggested that participants found the program useful in motivating weight loss and healthy behaviors; they endorsed the one-on-one telephone sessions as enjoyable and supportive. In particular, participants found the personalized care and recommendations helpful to staying on target. In addition to individualized feedback, these responses suggest that the patient–provider relationship was important in enhancing weight loss and improving health behaviors. Other studies have come to similar conclusions. A randomized controlled behavioral weight loss trial found that participants’ satisfaction with the provider’s involvement was associated with greater weight loss.38 Moreover, increased clinician mindfulness is associated with care that is more patient-centered and leads to increased patient satisfaction.39,40 Thus, the dietitian’s training in MBPs may have affected her approach to participants and contributed to weight loss in this intervention.
Limitations
Our study findings are limited by its small sample size, absence of a control group, and use of a single dietitian. In addition, given the multidimensional nature of the program, we cannot attribute our results to a single component. Nonetheless, many MBPs and many nutrition interventions are themselves multidimensional.10,12,21,22,41 Moreover, some participants (10 of 27) had previously worked with the dietitian (1–2 visits in most cases) prior to beginning this study, and these prior relationships may have contributed to the success of some participants in completing the intervention and maintaining weight loss. However, the outcomes for those participants who had a previous relationship with the dietitian were not significantly different from those who had no prior relationship (data not shown).
Another limitation was the survey collection method used. Many participants were not comfortable reading or completing questionnaires on their own either printed on paper or on a tablet, so a study staff member administered the questionnaires orally to all participants. Thus, some participants may have been biased when reporting sensitive information directly to a study staff member.
Although the study incorporated MBPs, participants reported that these techniques were difficult to learn over the phone, and many participants did not practice these skills on their own. In addition, many participants did not have a CD player to listen to guided recordings of MBPs. Instead, many preferred using smartphone applications. Future studies should examine this population’s preferences for learning mind–body skills and consider incorporating more in-person instruction and/or more emphasis on these skills during phone visits.
Challenges in Working With This Population
We encountered several challenges working with this population: Some participants had difficulty reading, making it challenging to administer questionnaires. Participants also reported a variety of barriers to engaging in this weight loss program including challenges fitting phone meetings into their schedules and not wanting to deny their children foods that did not comply with their own eating goals.
Conclusions
This pilot study found that a telephone-based mind–body and nutrition coaching program was feasible to develop and administer. The program found improvements in weight loss in completers, behavioral eating patterns, stress, and health behaviors in overweight and obese adults receiving care at a community health center. This program was unique in that it combined mind–body skills and telephone coaching to promote weight loss. The telephone-based design made this intervention available in real time to people who need it and decreased barriers to accessing care. The intervention provided a less expensive approach to weight loss through replacement of frequent in-person visits. Future randomized-controlled studies are needed to confirm these findings and better understand mechanisms of action and delivery for clinicians and patients.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Alana Alves, Courtney Colgan, Leah Howard, Megan McCormick, Nicolas Robison, Lillian Sonnenberg, and Liora Zhrebker for their contributions to this study.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Basis/Intel provided devices for an investigator-initiated research for JWD. Onyx/Amgen provided funding for an investigator-initiated research for JWD. All other authors have no conflicts of interest.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funds from the Taff Family and the Vela Foundation. MLD was supported by K23AT009218 from the National Center for Complementary and Integrative Health.
Ethical Approval
This study was approved by the Partners Human Research Committee. All procedures were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Centers for Disease Control and Prevention. Adult obesity facts. https://www.cdc.gov/obesity/data/adult.html. Published 2016. Accessed December 30, 2016.
- 2.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. Washington, DC: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. https://www.cdc.gov/nchs/data/databriefs/db219.pdf. Accessed December 29, 2016.
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014; 311(8): 806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009; 28(5): w822–w831. [DOI] [PubMed] [Google Scholar]
- 5.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009; 170(2): 181–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. 2007; 23(11–12): 887–894. [DOI] [PubMed] [Google Scholar]
- 7.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001; 26(1): 37–49. [DOI] [PubMed] [Google Scholar]
- 8.Rutters F, Nieuwenhuizen AG, Lemmens SGT, Born JM, Westerterp-Plantenga MS. Acute stress-related changes in eating in the absence of hunger. Obesity (Silver Spring). 2009; 17(1): 72–77. [DOI] [PubMed] [Google Scholar]
- 9.Privitera GJ, King-Shepard QW, Cuifolo KN, Doraiswamy PM. Differential food intake and food choice by depression and body mass index levels following a mood manipulation in a buffet-style setting [published online ahead of print May 1, 2016]. J Health Psychol. doi:10.1177/1359105316650508. [DOI] [PubMed]
- 10.Chacko SA, Yeh GY, Davis RB, Wee CC. A mindfulness-based intervention to control weight after bariatric surgery: preliminary results from a randomized controlled pilot trial. Complement Ther Med. 2016; 28: 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katterman SN, Kleinman BM, Hood MM, Nackers LM, Corsica JA. Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eat Behav. 2014; 15(2): 197–204. [DOI] [PubMed] [Google Scholar]
- 12.Levoy E, Lazaridou A, Brewer J, Fulwiler C. An exploratory study of Mindfulness Based Stress Reduction for emotional eating. Appetite. 2017; 109: 124–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olson KL, Emery CF. Mindfulness and weight loss: a systematic review. Psychosom Med. 2015; 77(1): 59–67. [DOI] [PubMed] [Google Scholar]
- 14.Rogers JM, Ferrari M, Mosely K, Lang CP, Brennan L. Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obes Rev Off J Int Assoc Study Obes. 2017; 18(1): 51–67. [DOI] [PubMed] [Google Scholar]
- 15.Ruffault A, Czernichow S, Hagger MS, et al. The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract. 2017; 11(5S1): 90–111. [DOI] [PubMed] [Google Scholar]
- 16.Park ER, Traeger L, Vranceanu A-M, et al. The development of a patient-centered program based on the relaxation response: the Relaxation Response Resiliency Program (3RP). Psychosomatics. 2013; 54(2): 165–174. [DOI] [PubMed] [Google Scholar]
- 17.Clarke T, Black L, Stussman B, Barnes P, Nahin R. Trends in the Use of Complementary Health Approaches among Adults: United States, 2002-2012. National Health Statistics Reports, Hyattsville, MD: National Center for Health Statistics, 2015. [PMC free article] [PubMed] [Google Scholar]
- 18.Murdock A, Rodgers C, Lindsay H, Tham TCK. Why do patients not keep their appointments? Prospective study in a gastroenterology outpatient clinic. J R Soc Med. 2002; 95(6): 284–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Paterson BL, Charlton P, Richard S. Non-attendance in chronic disease clinics: a matter of non-compliance? J Nurs Healthc Chronic Illn. 2010; 2(1): 63–74. [Google Scholar]
- 20.Wolever RQ, Eisenberg DM. What is health coaching anyway? Standards needed to enable rigorous research: comment on “Evaluation of a behavior support intervention for patients with poorly controlled diabetes.”. Arch Intern Med. 2011; 171(22): 2017–2018. [DOI] [PubMed] [Google Scholar]
- 21.Weinstock RS, Trief PM, Cibula D, Morin PC, Delahanty LM. Weight loss success in metabolic syndrome by telephone interventions: results from the SHINE study. J Gen Intern Med. 2013; 28(12): 1620–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelly JT, Reidlinger DP, Hoffmann TC, Campbell KL. Telehealth methods to deliver dietary interventions in adults with chronic disease: a systematic review and meta-analysis. Am J Clin Nutr. 2016; 104(6): 1693–1702. [DOI] [PubMed] [Google Scholar]
- 23.Ayisi Addo S, Steiner-Asiedu M. Telephone based weight loss intervention: relevance for developing countries. Crit Rev Food Sci Nutr. 2018, pp. 1–7. DOI: 10.1080/10408398.2018.1437536. [DOI] [PubMed] [Google Scholar]
- 24.CIGNA Healthy Eating Survey. http://humanresources.brevardschools.org/CompBenefits/Wellness/Weight%20Documents/healthy%20eating%20survey.pdf. Accessed December 29, 2016.
- 25.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983; 24(4): 385–396. [PubMed] [Google Scholar]
- 26.Thorndike AN, Sonnenberg L, Healey E, Myint-UK, Kvedar JC, Regan S. Prevention of weight gain following a worksite nutrition and exercise program: a randomized controlled trial. Am J Prev Med. 2012; 43(1): 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994; 23(5): 991–999. [DOI] [PubMed] [Google Scholar]
- 28.Borkan J. Immersion/crystallization. In: Crabtree B, Miller W. (eds). Doing Qualitative Research, 2nd ed Thousand Oaks, CA: SAGE, 1999. [Google Scholar]
- 29.Barte JCM, ter Bogt NCW, Bogers RP, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev Off J Int Assoc Study Obes. 2010; 11(12): 899–906. [DOI] [PubMed] [Google Scholar]
- 30.Turk MW, Yang K, Hravnak M, Sereika SM, Ewing LJ, Burke LE. Randomized clinical trials of weight loss maintenance: a review. J Cardiovasc Nurs. 2009; 24(1): 58–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006; 355(15): 1563–1571. [DOI] [PubMed] [Google Scholar]
- 32.Brantley PJ, Stewart DW, Myers VH, et al. Psychosocial predictors of weight regain in the weight loss maintenance trial. J Behav Med. 2014; 37(6): 1155–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spoor STP, Bekker MHJ, Van Strien T, van Heck GL. Relations between negative affect, coping, and emotional eating. Appetite. 2007; 48(3): 368–376. [DOI] [PubMed] [Google Scholar]
- 34.Dusek JA, Benson H. Mind-body medicine: a model of the comparative clinical impact of the acute stress and relaxation responses. Minn Med. 2009; 92(5): 47–50. [PMC free article] [PubMed] [Google Scholar]
- 35.Tang Y-Y, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. 2015; 16(4): 213–225. [DOI] [PubMed] [Google Scholar]
- 36.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009; 17(5): 941–964. [DOI] [PubMed] [Google Scholar]
- 37.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011; 111(1): 92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bennett WL, Wang N-Y, Gudzune KA, et al. Satisfaction with primary care provider involvement is associated with greater weight loss: results from the practice-based POWER trial. Patient Educ Couns. 2015; 98(9): 1099–1105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beach MC, Roter D, Korthuis PT, et al. A multicenter study of physician mindfulness and health care quality. Ann Fam Med. 2013; 11(5): 421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dobkin PL, Bernardi NF, Bagnis CI. Enhancing clinicians’ well-being and patient-centered care through mindfulness. J Contin Educ Health Prof. 2016; 36(1): 11–16. [DOI] [PubMed] [Google Scholar]
- 41.Wayne PM, Manor B, Novak V, et al. A systems biology approach to studying tai chi, physiological complexity and healthy aging: design and rationale of a pragmatic randomized controlled trial. Contemp Clin Trials. 2013; 34(1): 21–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.