Abstract
Objective
Mobile applications (apps) are increasingly being utilized in health behavior change interventions. To determine the presence of underlying behavior change mechanisms, apps for physical activity have been coded for behavior change techniques (BCTs). However, apps for sedentary behavior have yet to be assessed for BCTs. Thus, the purpose of the present study was to review apps designed to decrease sedentary time and determine the presence of BCTs.
Methods
Systematic searches of the iTunes App and Google Play stores were completed using keyword searches. Two reviewers independently coded free (n = 36) and paid (n = 14) app descriptions using a taxonomy of 93 BCTs (December 2016–January 2017). A subsample (n = 4) of free apps were trialed for one week by the reviewers and coded for the presence of BCTs (February 2017).
Results
In the free and paid app descriptions, only 10 of 93 BCTs were present with a mean of 2.42 BCTs (range 0–6) per app. The BCTs coded most frequently were “prompts/cues” (n = 43), “information about health consequences” (n = 31), and “self-monitoring of behavior” (n = 17). For the four free apps that were trialed, three additional BCTs were coded that were not coded in the descriptions: “graded tasks,” “focus on past successes,” and “behavior substitution.”
Conclusions
These sedentary behavior apps have fewer BCTs compared with physical activity apps and traditional (i.e., non-app) physical activity and healthy eating interventions. The present study sheds light on the behavior change potential of sedentary behavior apps and provides practical insight about coding for BCTs in apps.
Keywords: Behavior change techniques, mobile applications, sedentary behavior, mHealth, sitting
Introduction
Sedentary behavior has emerged as a risk factor to overall health that is independent from the amount of physical activity one achieves.1,2 Sedentary behavior is defined as “any waking activity characterized by an energy expenditure ≤1.5 metabolic equivalents while in a sitting or reclining posture.”3 The levels of sitting time have been objectively measured and are high for Canadian adults at 9.5 hours a day4 and 7.7 hours for American adults and children.5 Recent research has called for both public health recommendations specific to sedentary behavior6 and more clarification on the goal of sedentary behavior interventions with respect to physical activity.7
With respect to the latter point, a meta-analysis by Prince et al.8 compared the effectiveness of a variety of interventions focusing on physical activity and/or sedentary behavior for reducing sedentary time in adults. They concluded that interventions focusing on only sedentary behavior resulted in greater reduction of sedentary time, compared with interventions with a goal of increasing physical activity levels or a combined goal to increase physical activity levels and decrease sedentary time. Further, using the same techniques that have been successful in influencing physical activity may not result in a positive influence on sedentary behavior. For example, action planning, an established technique for bridging intention and behavior, was found to increase physical activity in those with weak habits but had no impact on changing sedentary behavior, regardless of habit strength.9 Thus, addressing sedentary behavior independently and exploring novel ways to influence sedentary behavior is imperative.
Mobile applications (apps) and other forms of mHealth are increasingly being utilized in interventions for a variety of health behaviors.10–12 For sedentary behavior specifically, Bond et al.13 outlined several advantages of smartphone-based interventions including the ability to target and monitor sedentary behavior using the built-in accelerometer, prompting users to take breaks, and providing feedback in real-time. Bond et al.13 also saw reduced sedentary time and increased physical activity with using a sedentary behavior app called “B-MOBILE” in a population of overweight/obese individuals.
It has been established that interventions for health behavior change are more likely to be effective if they are based in behavior change theory.14 iPhone apps for physical activity that have been assessed for the presence of health behavior change theory constructs display limited theoretical content.15 Apps for physical activity have also been coded for the presence of specific behavior change techniques (BCTs).16–19 BCTs are the “observable and replicable components of behavior change interventions,” 20 or the “active ingredients” in interventions. Coding interventions for BCTs identifies the components of an intervention that may lead to behavior change. Coding apps for BCTs can inform users, researchers, and developers about the behavior change potential in apps.
These four studies that coded physical activity apps for BCTs have varied methods for searching and coding. Middelweerd et al.18 utilized a systematic search of the iTunes and Google Play app stores, whereas Yang et al.,19 Conroy et al.,16 and Direito et al.17 reviewed top physical activity apps in the “health and fitness” categories. Middelweerd et al.18 and Direito et al.17 coded apps by using them, Yang et al.19 inspected the apps, and Conroy et al.16 coded for the presence of BCTs using the app description. Despite utilizing different BCT taxonomies for coding, each found a low average number of BCTs for each app: Middelweerd et al.18 found an average of 5 BCTs with a range from 2 to 8 BCTs, Yang et al.19 found an average of 6.6 with a range from 1 to 21, Conroy et al.16 found an average of 4.2 with a range from 1 to 13, and Direito et al.17 found an average of 8.1 with a range from 2 to 18 BCTs. These studies have also made comparisons between free and paid apps and apps from the iTunes and Google Play stores. Yang et al.19 and Middelweerd et al.18 found no difference in the number of BCTs in each app between paid or free apps, but Conroy et al.16 and Direito et al.17 did find some differences between BCTs coded. Middelweerd et al.18 also found no difference in BCTs between apps from the iTunes and Google Play stores.
Although these studies provide important insight into the behavior change capacity of apps designed to increase physical activity, apps designed specifically to decrease sedentary behavior have not been examined (i.e., coded) for the presence of BCTs. Thus, we do not yet know which BCTs are typically utilized and the subsequent behavior change potential in apps for sedentary behavior.
Purpose
The purpose of this study was to review mobile apps designed to reduce sedentary/sitting time for the presence of BCTs. Specifically, we aimed to compare BCTs coded as present: (1) between apps from the iTunes (i.e., for iPhones) and Google Play (i.e., for Androids) stores, (2) between free and paid apps, and (3) with different coding strategies (i.e., coding “by description” and coding (“by use”).
Methods
Search strategy
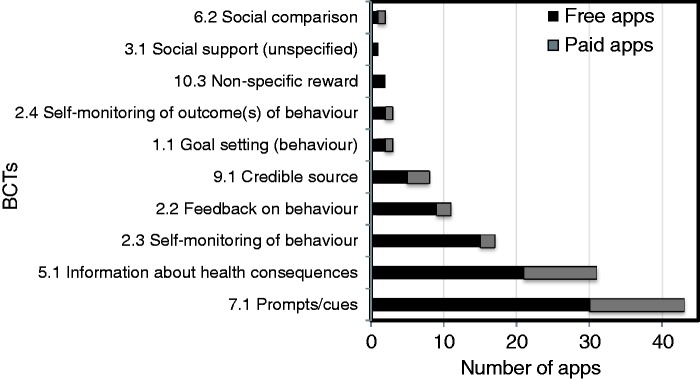
Systematic searches of the iTunes app store for iPhone apps and Google Play app store for Android apps were completed using 10 keyword searches. Search terms included “sitting,” “sit,” “stand,” “standing,” “stand up,” “sedentary,” “break,” “exercise break,” “physical activity break,” and “move.” Although the search terms were consistent between the iTunes and Google Play stores, the search strategy was slightly different for iTunes and Google Play as they employed different search algorithms (as previously noted by Middelweerd et al.18). The iTunes store displays a maximum of 100 apps for each search. A total of 815 iPhone apps were obtained with the keyword searches in iTunes. For Google Play, more search results are obtained, therefore, as per the search performed by Middelweerd et al.,18 the first 100 apps were screened for inclusion. If at least five of those 100 apps met the criteria, the next 100 apps were also screened. If one app met the criteria within these second 100 apps, then the next 100 apps were also screened. This continued until no additional apps were selected in a group of 100 apps. A total of 1400 Android apps were obtained with all the keyword searches in Google Play. Following the search, all apps (n = 2215) were screened in one step for inclusion criteria by title, picture, and description by the first author (ED). A total of 2165 apps were removed and thus a total of 50 apps remained to be coded (see Figure 1).
Figure 1.
Flow chart of systemic search of the app stores.
Inclusion criteria
To be included, the app must have been: (1) focused on sedentary behavior with a goal of disrupting sitting time, with or without providing suggestions of what to do during these interruptions, (2) compatible for mobile smartphones (i.e., not exclusively for iPads or desktops), (3) available in English, and 4) not associated with an external device (e.g., Fitbit® device).
Primary coding process
The taxonomy used to code the apps distinguishes between 93 BCTs (BCTTv1).21 The apps identified in the search that met the inclusion criteria were scored as present or not present for each of the 93 BCTs independently by two reviewers (ED, JRW). Both reviewers completed online certifications for BCT coding using the BCTTv1 training. Apps were only coded for the presence of BCTs related to sedentary behavior. The app could have had other features not related to sedentary behavior (e.g., water intake) that were not coded.
Two reviewers first coded all the free apps (n = 36) based on their descriptions (December 2016). A third reviewer who is a trained, experienced coder (HG) was consulted to address the app coding issues that arose between the two reviewers. A set of coding rules was developed to address these issues (see Supplementary Table 1). The two initial reviewers then recoded the apps in question, implementing the set of coding rules and any remaining coding issues were resolved through discussion between the three reviewers.
Paid apps (n = 14) were then coded by description (January 2017), implementing the developed set of rules. The third reviewer was again consulted with to resolve disagreements. There were four apps that had a free and paid version. In each of these four cases, both the free and paid versions were coded based on the description.
Secondary coding process
Based on the primary coding process for free and paid apps, a subsample (n = 4) of free iTunes apps with the greatest number of BCTs coded in the description were downloaded and used for one week (8 February to 15 February 2017) by two reviewers (ED, JRW). These apps were Rise & Recharge®, Standland®, Sitting®, and Stand Up®. After the week, the apps were coded for the presence of BCTs. Reviewers took screenshots of the apps as evidence for identifying the BCT. New issues with coding “by use” arose and the third reviewer (HG) was consulted again. The two reviewers then recoded the apps in question and any remaining issues were resolved through discussion.
Statistical analysis
A Cohen’s kappa statistic22 and a prevalence-adjusted bias-adjusted kappa (PABAK)23 statistic were calculated as a measure of inter-rater reliability for the initial round of coding (i.e., before the third reviewer was consulted) for apps coded “by description” and “by use.” PABAK was used to adjust for bias and high prevalence of negative cases between reviewers (i.e., both coded “not present”).23 The PABAK has been previously used to describe agreement between reviewers using the BCTTv1 to code interventions.24,25 Inter-rater reliability values of .61–.80 indicate “substantial” reliability, and those above .80 would be considered “outstanding.”22, 23
Descriptive and frequency statistics were performed to describe the BCTs coded, obtain mean BCTs coded, mean price for paid apps, and mean Cohen’s kappa and PABAK scores. Independent t-tests were performed to compare mean BCTs between free and paid apps and between iPhone and Android apps. After the descriptions had been coded for the presence of BCTs, the word count of each description provided by iTunes or Google Play was calculated. This step was done in order to compare the length of the description and to determine if it might explain the difference in BCTs present. Independent t-tests were performed to compare mean word count between free and paid apps and iPhone and Android apps. Statistical analyses were performed on SPSS Version 24 (IBM Corp Armonk, NY).
Results
Inter-rater agreement
The overall average kappa score across both primary (free n = 36; paid n = 14) and secondary coding (n = 4) was 0.60 (SD = 0.34) and the PABAK score was 0.96 (SD = 0.04). Separately, for the primary coding process, the average kappa score was 0.60 (SD = 0.35) and the PABAK score was 0.96 (SD = 0.04). For the secondary coding process, the average kappa score was 0.65 (SD = 0.15) and the PABAK score was 0.94 (SD = 0.03). The kappa scores indicate substantial agreement and the PABAK scores indicate outstanding agreement, respectively.22,23
Primary coding process
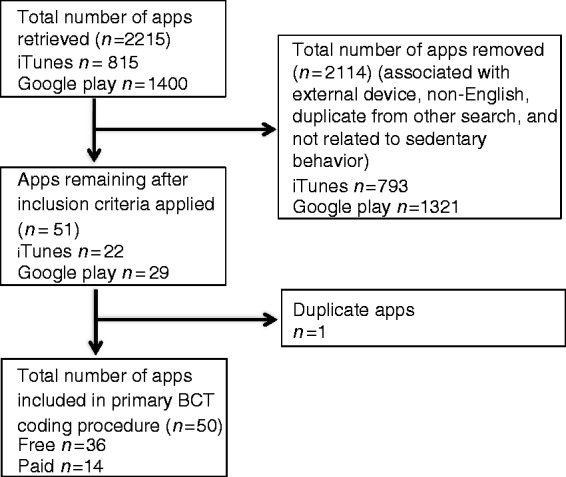
Supplementary Table 2 presents a comprehensive list of BCTs present in each free and paid app in the iTunes and Google Play stores. In the descriptions, only 10 of a potential 93 BCTs were present. A mean of 2.42 BCTs (range 0–6) were present in each app description. The three BCTs that were coded the most frequently include “prompts/cues” (n = 43), “information about health consequences” (n = 31), and “self-monitoring of behavior” (n = 17) (see Figure 2). In the four cases where there was a free and paid version, there were no differences in the number of or specific BCTs present between the versions (see Supplementary Table 2).
Figure 2.
Number of apps with BCT present
There was a difference in number of BCTs present between apps for iPhones and Androids, t(48) = 2.67, p = 0.01, where iPhones apps (n = 22) had an average of 3 BCTs per app and Android apps (n = 28) had an average of 1.96 BCTs. However, there was no difference in number of BCTs present in free and paid app descriptions, t(48) = 0.19, p = 0.85. The average price of the paid apps was $1.90 CAD(SD = 0.980). The average word count of the descriptions was 226.36 words (SD = 133.70). There was no statistically significant difference in word count between apps for iPhones and Androids, t(48) = 1.466, p = 0.149, where iPhone apps (n = 22) had an average of 257.27 words per description and Android apps (n = 28) had an average of 202.07 words per descriptions. There was also no statistically significant difference in word count between free and paid apps, t(48) = −1.890, p = 0.065, where free apps (n = 36) had an average of 204.64 words per description and paid apps (n = 14) had an average of 282.21 words per description.
Secondary coding process
Several differences emerged in the actual BCTs coded “by use” (see Table 1). Specifically, there were three BCTs coded that were previously not coded in the descriptions: “graded tasks,” “focus on past successes,” and “behavior substitution.” Thus, by coding “by use,” there were 13 out a potential 93 BCTs identified. The BCTs “information on health consequences,” “credible source,” and “self-monitoring of outcome of behavior” were present in descriptions, but not in “by use” coding.
Table 1.
Differences in apps coded “by description” and “by use.”
| App | BCTs by Description | BCTs by Use |
|---|---|---|
| Standland® | 2.2 Feedback on behavior 2.3 Self-monitoring of behavior 3.1 Social support (unspecified) 5.1 Information about health consequences 10.3 Non-specific reward | 1.1 Goal-setting (behavior) 2.2 Feedback on behavior 2.3 Self-monitoring of behavior 3.1 Social support (unspecified) 8.7 Graded tasks 10.3 Non-specific reward 15.3 Focus on past successes |
| Rise & Recharge® | 1.1 Goal-setting (behavior) 2.3 Self-monitoring of behavior 5.1 Information on health consequences 7.1 Prompts/cues 9.1 Credible source 10.3 Non-specific reward | 1.1 Goal-setting (behavior) 2.2 Feedback on behavior 2.3 Self-monitoring of behavior 5.1 Information on health consequences 7.1 Prompts/cues 8.2 Behavior substitution 10.3 Non-specific reward |
| Sitting® | 2.2 Feedback on behavior 2.3 Self-monitoring of behavior 5.1 Information about health consequences 7.1 Prompts/cues | 1.1 Goal-setting (behavior) 2.2 Feedback on behavior 2.3 Self-monitoring of behavior 7.1 Prompts/cues |
| Stand Up®* | 1.1 Goal-setting (behavior) 2.3 Self-monitoring of behavior 2.4 Self-monitoring of outcome(s) of behavior 5.1 Information about health consequences 7.1 Prompts/cues 9.1 Credible source | 1.1 Goal-setting (behavior) 2.2 Feedback behavior 2.3 Self-monitoring of behavior 5.1 Information about health consequences 7.1 Prompts/cue 9.1 Credible source |
Bolded BCTs indicate discrepancies between coding “by description” and “by use.” *This is app 8 as indicated in the Supplementary Table 2.
Discussion
The purpose of the current study was to code and compare mobile apps designed to reduce sedentary/sitting time for the presence of BCTs. Compared with physical activity apps coded previously,16–19 there were substantial differences in the BCTs coded for apps for sedentary behavior in the current research. Overall, the sedentary behavior apps in this review contained fewer BCTs on average, a smaller range of BCTs per app, and fewer BCTs were identified overall. Furthermore, the most prevalent BCT coded in this review was “prompts/cues,” whereas the most prevalent BCTs coded in Yang et al.’s,19 Conroy et al.’s,16 Middelweerd et al.’s,18 and Direito et al.’s17 reviews were “social support (unspecified),” “provide instruction on how to perform behavior,” “provide feedback on performance,” and “provide instruction,” respectively.
One reason for these discrepancies could be due to the differences in taxonomies used by Conroy et al.,16 Middelweerd et al.,18 and Direito et al.17 However, Yang et al.19 used the same 93-BCT taxonomy implemented here and coded 39 BCTs present in 100 physical activity apps. A second reason for these discrepancies reflects the different strategies employed by app developers for physical activity compared with sedentary behavior apps. Explicitly, apps for physical activity appear to employ more behavior change strategies compared with apps for sedentary behavior. In addition, the sedentary behavior apps reviewed here also contained fewer BCTs compared with traditional (i.e., non-app) physical activity and healthy eating interventions coded previously.26 At this time, interventions would benefit from using sedentary behavior apps in conjunction with other behavior change methods (i.e., as part of a multi-component, theory-based intervention). As Schoeppe et al.27 suggested, apps that are used in multi-component interventions for physical activity appear to result in better behavioral and health outcomes than stand-alone app interventions. Although determining the stand-alone impact of apps in multi-component studies is challenging, based on the lack of BCTs, sedentary behavior apps in their current form may be insufficient for changing behavior on their own. In order to implement sedentary behavior apps as independent interventions, and as per recent recommendations from Schoeppe et al.,27 further investigation is warranted to “determine the optimal number and combination of app features, BCTs, and level of participant contact needed to maximize user engagement and ultimately intervention efficacy.” As noted there, app features will influence user engagement. Recently, a review of apps for weight management found a link between indicators of app quality and BCT features.28 Thus, incorporating BCT features could lead to better engagement and long-term use.
In comparison to physical activity, BCTs most effective for sedentary behavior alone have yet to be established. In Direito et al.’s17 app analysis, they commented on the presence of BCTs associated with greater behavior change effectiveness in apps for physical activity, however such a comparison specifically for sedentary behavior is not possible in this analysis. However, the comparison of BCTs between physical activity and sedentary behavior apps might provide insight into how app developers are already using different techniques to address these behaviors. For example, Direito et al.17 reported that zero physical activity apps included the BCT “teach to use prompts/cues,” but in the present study the related BCT “prompts/cues” was coded most frequently. Further, a recent review by Gardner et al.29 of sedentary behavior interventions for adults found that interventions that were more promising (i.e., saw reductions in sedentary behavior) had significantly more BCTs than interventions that were not promising. Additionally, they identified several BCTs associated with promising results. Of these BCTs, making changes to the environment and problem solving were two that were missing from our own review of sedentary behavior apps. On the other hand, self-monitoring and providing health outcome information were found in our review and in Gardner et al.’s29 review. These discrepancies could be the function of the app as the mode of delivery and might reflect that certain BCTs lend themselves better to app functions, whereas the inclusion of other BCTs, for example making changes to the environment, are not directly supported by app functions. Nevertheless, future apps and interventions might benefit from creative solutions that incorporate these BCTs highlighted by Gardner et al.29 into their function.
Coding challenges
An issue that arose frequently in the coding process was appropriate coding for the behavior of interest (i.e., sitting). For example, in the apps coded “by use,” all four apps had “goal-setting (behavior)” present but most of these goals were “not-sitting” behaviors (e.g., standing minutes, number of stands). However, “not sitting” can involve physical activity behaviors ranging in intensity from light (e.g., standing, slow walking) to moderate-to-vigorous (e.g., running, squats, push-ups).7 Thus, we chose to clarify that in order to code “goal-setting (behavior)” the app could have had a goal opposite of sitting (e.g., minutes spent standing) but not a goal that specified moderate-to-vigorous physical activity (MVPA). These challenges reflect current consideration of what is called the “dual-hinge approach,” which Spence et al.7 describe as substituting sedentary behavior with MVPA. As seen with the “goal-setting (behavior)” BCT, some of these apps employ the dual-hinge approach, which makes coding challenging because the BCTs are supposed to be specific to the behavior of interest (i.e., sitting) and not physical activity. Although MVPA substitution-based interventions may result in more significant health outcome benefits,7 interventions specific to sedentary behavior are more effective for decreasing sitting time.8
As well, the discrepancies that existed between coding “by description” and coding “by use” were the result of inaccurate app descriptions or app functions not working. Therefore, just because a BCT is present in the app description, it may not actually be present as a BCT for use. As previously noted by Cowan et al.,15 as app developers are using app descriptions as a marketing platform to sell their apps, the app descriptions alone might not adequately represent the content and functionality of the app. However, in our small sample we were able to code most of the BCTs present in the description as compared to by use, thus the description is able to highlight at least the main features of the app. A future study should purposefully trial and then code a larger number of paid and free sedentary behavior apps with a range of BCTs in order to ascertain the presence of BCTs between coding by description vs. use. This would allow for better understanding of the accuracy of by description vs. by use coding within sedentary behavior apps, as well as allow for comparisons with previous by description and/or use physical activity app coding studies.16–19
Limitations
The findings presented here should be considered within the context of several limitations. Most importantly, as noted by Middelweerd et al.,18 BCT taxonomies were not designed to score app-based interventions, and therefore interpreting BCTs as app functionalities may result in biases while coding, which potentially complicates comparisons with other studies that coded apps with BCT taxonomies. Moreover, each previous app coding study has used a different taxonomy for coding, which further complicates comparing the BCTs coded between studies. Despite the comprehensiveness of the systematic search of the app stores, some apps may still not have been identified because they were missed in the search process or had a poor description, and we did not code BCTs for other health behaviors that some apps also included. Additonally missing are a small subset of apps that are designed to support external devices (e.g., Fitibit®). As these types of apps can assist with sedentary behavior, future studies should examine apps associated with external devices in comparison to stand-alone apps on a smartphone. Furthermore, only four apps were coded by trialing, therefore the majority of coding presented here reflects the app descriptions only.
Conclusions
Overall, the present study contributes to understanding the behavior change potential in mobile apps for sedentary behavior, which can inform researchers designing sedentary behavior interventions that utilize apps and developers in app design. Moving forward, in line with previous recommendations,15 health behavior change specialists should look to work with app developers in creating apps based in theory. Based on the present review, some suggestions to consider in future collaborative investigations are that sedentary behavior apps should look to incorporate more appropriate BCTs, or, in their current form, sedentary apps could be utilized in multi-component interventions to increase effectiveness. Furthermore, apps should avoid promoting the replacement of sedentary behavior with MVPA (the dual-hinge approach) and focus on strategies that relate specifically to sedentary behavior.
Supplemental Material
Supplemental material, Supplementary tables for Behavior change techniques in mobile applications for sedentary behavior by Emily E Dunn, Heather L Gainforth and Jennifer E Robertson-Wilson in Digital Health
Acknowledgements
The contents of this manuscript reflect a portion of ED’s Master’s Thesis. Contents of this manuscript were presented at ISBNPA (June 2017) conference.
Contributorship
ED conceived the study, researched literature, conducted the search, app coding, and analysis and drafted the manuscript. JRW conceived the study and conducted app coding. HG served as an app coder and assisted with development of the coding protocol and reliability analysis. All authors reviewed and edited the manuscript and approved the final version.
Conflict of interests
There are no conflicting interests related to this research.
Ethical approval
This work did not require ethics approval.
Funding
This work did not receive funding.
Guarantor
The corresponding author and guarantor for this manuscript is Emily Dunn.
Peer review
This manuscript was reviewed by two individuals who have chosen to remain anonymous.
Supplementary Material
Supplementary material is available for this article online.
References
- 1.Owen N, Healy GN, Matthews CE, et al. Too much sitting: the population-health science of sedentary behavior. Exerc Sport Sci Rev 2010; 38: 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katzmarzyk PT, Church TS, Craig CL, et al. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc 2009; 41: 998–1005. [DOI] [PubMed] [Google Scholar]
- 3.Sedentary Behavior Research Network. Standardized use of the terms “sedentary” and “sedentary behaviors”. Appl Physiol Nutr Metab 2012; 37: 540–542. [DOI] [PubMed] [Google Scholar]
- 4.Colley RC, Garriguet D, Janssen I, et al. Physical activity of Canadian adults: accelerometer results from the 2007 to the 2009 Canadian health measures survey. Health Rep 2011; 22: 7–14. [PubMed] [Google Scholar]
- 5.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 2008; 167: 875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Healy GN, Dunstan DW, Salmon J, et al. (2008). Breaks in sedentary time. Diabetes Care 2008; 31: 661–666. [DOI] [PubMed] [Google Scholar]
- 7.Spence JC, Rhodes RE, Carson V. Challenging the dual-hinge approach to intervening on sedentary behavior. Am J Prev Med 2017; 52: 403–406. [DOI] [PubMed] [Google Scholar]
- 8.Prince SA, Saunders TJ, Gretsy K, et al. A comparison of the effectiveness of physical activity and sedentary behavior interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obesity Rev 2014; 15: 905–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maher JP, Conroy DE. Habit strength moderates the effects of daily action planning prompts on physical activity but not sedentary behavior. J Sport Exerc Psychol 2015; 37: 97–107. [DOI] [PubMed] [Google Scholar]
- 10.Iacoviello BM, Steinermen JR, Klein DB, et al. Clickotine, a personalized smartphone app for smoking cessation: initial evaluation. JMIR mHealth uHealth 2017; 5: e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Puszkiewicz P, Roberts AL, Smith L, et al. Assessment of cancer survivors’ experiences of using a publicly available physical activity mobile application. JMIR Cancer 2016; 2: e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turner T, Hingle M. Evaluation of a mindfulness-based mobile app aimed at promoting awareness of weight-related behaviors in adolescents: a pilot study. JMIR Res Protoc 2017; 6: e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bond DS, Thomas JG, Raynor HA, et al. B-MOBILE – a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: a within-subjects experimental trail. PLoS ONE 2014; 9: e100821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Webb TL, Joseph J, Yardley L, et al. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res 2010; 12: e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cowan LT, Van Wagenen SA, Brown BA, et al. Apps of steel: are exercise apps providing consumers with realistic expectations? A content analysis of exercise apps for presence of behavior change theory. Health Educ Behav 2012; 40: 133–139. [DOI] [PubMed] [Google Scholar]
- 16.Conroy DE, Yang C, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med 2014; 46: 649–652. [DOI] [PubMed] [Google Scholar]
- 17.Direito A, Dale LP, Shields E, et al. Do physical activity and dietary smartphone applications incorporate evidence-based behavior change techniques? BMC Public Health 2014; 14: 646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Middelweerd A, Mollee JS, Van Der Wal CN, et al. Apps to promote physical activity among adults: a review and content analysis. Int J Behav Nutr Phys 2014; 11: 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang C, Maher JP, Conroy DE. Implementation of behavior change techniques in mobile applications for physical activity. Am J Prev Med 2015; 48: 452–455. [DOI] [PubMed] [Google Scholar]
- 20.Michie S, Johnston M. Theories and techniques of behavior change: developing a cumulative science of behavior change. Health Psychol Rev 2012; 6: 1–6. [Google Scholar]
- 21.Michie S, Richardson M, Johnston M, et al. The behavior technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95. [DOI] [PubMed] [Google Scholar]
- 22.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174. [PubMed] [Google Scholar]
- 23.Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol 1993; 46: 423–429. [DOI] [PubMed] [Google Scholar]
- 24.Cradock KA, ÓLaighin G, Finucane FM, et al. Behavior change techniques targeting both diet and physical activity in type 2 diabetes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act 2017; 14: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wood CE, Hardeman W, Johnston M, et al. Reporting behavior change interventions: do the behavior change technique taxonomy v1, and training in its use, improve the quality of intervention descriptions? Implement Sci 2006; 11: 84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psych 2009; 28: 690–701. [DOI] [PubMed] [Google Scholar]
- 27.Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behavior: a systematic review. Int J Behav Nutr Phys 2016; 13: 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bardus M, van Beurden SB, Smith JR, et al. A review and content analysis of engagement, functionality, aesthetics, information quality, and change techniques in the most popular commercial apps for weight management. Int J Behav Nutr Phys 2016; 13: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gardner B, Smith L, Lorencatta F, et al. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction intervention among adults. Health Psychol Rev 2016; 10: 89–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary tables for Behavior change techniques in mobile applications for sedentary behavior by Emily E Dunn, Heather L Gainforth and Jennifer E Robertson-Wilson in Digital Health