Abstract
Context:
Shoulder pain and dysfunction are common, with patients presenting complaints to both primary and orthopaedic physicians. History and physical examination remain essential to creating a differential diagnosis, even as noninvasive imaging has improved.
Evidence Acquisition:
Literature was obtained through keyword searches based on the pathology in question (eg, rotator cuff) and the keywords physical examination using PubMed from January 1, 1980, through September 20, 2017. Additional evidence was obtained through screening references from articles identified through the PubMed searches.
Study Design:
Clinical review.
Level of Evidence:
Level 3.
Results:
A total of 7817 articles were screened for relevance. Several physical examination maneuvers have been described for each specific pathology. The Neer sign has a 75% sensitivity for subacromial impingement (SAI), while the Hawkins-Kennedy test has an 80% sensitivity. The painful arc test has an 80% specificity for SAI. The apprehension test has a hazard ratio of 2.96 for anterior shoulder instability. The Jobe test has a sensitivity of 52.6% and a specificity of 82.4% for full-thickness supraspinatus tears, confirmed on arthroscopy. The lag sign is highly sensitive and specific for combined full-thickness supraspinatus and infraspinatus tears at 97% and 93%, respectively. The Speed test has a sensitivity of 54% and specificity of 81% for biceps pathology. The anterior slide test and O’Brien active compression test have been described for superior labrum anterior posterior tears with inconsistent reliability. The cross-body adduction test has a sensitivity of 77% and a specificity of 79% for acromioclavicular joint pathology.
Conclusion:
Several physical examination maneuvers can isolate specific pathology of the shoulder, with widely ranging sensitivity and specificity.
Keywords: shoulder, physical examination, rotator cuff, biceps, acromioclavicular joint, glenoid labrum
Shoulder pain and dysfunction are among the most commonly diagnosed and treated conditions within orthopaedic surgery.13 A thorough history and physical examination remain essential in evaluating patients with shoulder pain and dysfunction. This comprehensive review focuses on how to perform pathology-specific tests and provides the sensitivity and specificity of those maneuvers for various shoulder injuries.
Subacromial Impingement
Subacromial impingement (SAI) accounts for 44% to 65% of all complaints of shoulder pain in a physician’s office.5 SAI occurs due to the confined anatomy and numerous tendons coursing through a narrow space, often resulting in rotator cuff tendinitis and subacromial bursitis.25 Specifically, patients describing pain in the deltoid with extension to the deltoid tuberosity with associated tenderness at the Codman point should be examined for SAI.48
The Neer sign is performed by passively moving the arm to maximal forward elevation with 1 hand while stabilizing the scapula with the other. The test is considered positive if pain is reproduced (Table 1).34 MacDonald et al28 demonstrated 75% sensitivity of the Neer sign for subacromial bursitis but overall poor specificity.
Table 1.
Instability and impingement shoulder physical examination maneuvers
| Test | Examination Technique | Interpretation of Findings |
|---|---|---|
| Apprehension test | • Patient is supine with shoulder at 90° abduction, elbow flexed to 90°, and full external rotation | Positive if patient experiences sense of instability |
| Relocation test | • Performed after apprehension test • Posterior force is then applied on humeral head |
Positive if patient no longer feels sense of instability |
| Anterior load and shift | • Patient is supine with shoulder at 40°-60° abduction, 90°
forward elevation • Axially load humerus and provide anterior/posterior force • Compare with contralateral side |
Positive if there is increased translation compared with contralateral side |
| Sulcus sign | • Patient standing with arm relaxed at the side • Pull affected arm inferiorly |
Positive if there is a sulcus formed at the superior aspect of the humeral head |
| Neer impingement sign | • Stabilize scapula while patient’s arm is elevated | Positive if patient has pain between 70° and 110° indicating impingement |
| Jobe test | • Shoulder is abducted to 90°, elevated to 30°, and internally
rotated • Patient maintains this position while examiner pushes down on the patient’s arm |
Positive if patient has pain or weakness indicating supraspinatus weakness or impingement |
The Hawkins-Kennedy test is performed with the arm in 90° of forward elevation with the elbow flexed to 90°, essentially creating an “L” shape in front of the body. The examiner then stabilizes the scapula with 1 hand while applying a downward force on the distal forearm to create maximum internal rotation (IR) (Figure 1).16 In a systematic review and meta-analysis, Hegedus et al17 demonstrated a sensitivity of 80% for the Hawkins-Kennedy test for SAI but overall poor specificity.
Figure 1.

The Hawkins-Kennedy test performed on a right shoulder. The examiner stabilizes the posterior shoulder with 1 hand, and with the patient’s shoulder flexed to 90° and the elbow flexed to 90°, a downward-directed force is applied to the wrist to evaluate for elicitation of pain.
The painful arc test is conducted by asking the patient to resist elevation slightly posterior to the coronal plane.48 Reproduction of pain is considered a positive test, with pain from 60° to 120° often indicative of rotator cuff pathology. The painful arc test, in contrast with the Neer sign and the Hawkins-Kennedy test, has a specificity of 80%.26
The Jobe test (ie, “empty can” test) evaluates for both SAI and supraspinatus pathology. To perform this test, the examiner abducts the patient’s arm to 90° in the scapular plane (30° from the coronal plane) and internally rotates the wrist so that the thumb is facing the ground with the elbow extended. He or she then applies a gentle downward force to the distal forearm, and if pain is reproduced, the test is considered positive (Figure 2).19 Michener et al,31 in a prospective study comparing the diagnostic reliability and accuracy of 5 examination tests for SAI, demonstrated a sensitivity of 50% and specificity of 87% for the Jobe test.
Figure 2.

The Jobe test performed on a right shoulder. The patient first abducts the arm to 90º then adducts 30º and internally rotates the shoulder so that the thumb is pointing down. The examiner then stabilizes the shoulder with 1 hand and applies a downward-directed force on the patient’s wrist with the other hand.
Internal Impingement
Internal impingement is commonly seen in overhead athletes. Andrews and Wilcox1 described internal impingement as an “overrotation phenomenon” consisting of excessive horizontal extension and rotation, increased glenohumeral translation, and glenohumeral IR deficit. As athletes externally rotate and abduct the arm to throw, the labrum becomes trapped between the rotator cuff and greater tuberosity laterally and the glenoid medially, which can result in rotator cuff and/or labral tears.1 The internal impingement test is performed with the patient supine, arm abducted to 90°, and maximally externally rotated with extension as in the throwing position (late cocking phase). The test is considered positive if this motion reproduces pain.
Instability: Anterior And Posterior
When there is a history of dislocation, subluxation, or a subjective sense of “looseness/instability,” a prompt and thorough evaluation of the shoulder stabilizers, including the glenoid labrum, is necessary (see Table 1). Instability may be multidirectional or only present in a single plane. For patients describing generalized joint laxity, physical examination should include an assessment for the Beighton criteria4 after performing a thorough history to assess for personal or family history of Ehlers-Danlos syndrome, Marfan syndrome, and other connective tissue disorders (Table 2).
Table 2.
Beighton criteria for hypermobility
| Joint Movement | Positive Finding | Scoring |
|---|---|---|
| Fifth finger dorsiflexion | • Passive dorsiflexion >90° | Right: 1 if yes, 0 if no Left: 1 if yes, 0 if no |
| Thumb apposition | • Passive apposition to the volar aspect of the forearm | Right: 1 if yes, 0 if no Left: 1 if yes, 0 if no |
| Elbow hyperextension | • Active hyperextension of the elbows beyond 10° | Right: 1 if yes, 0 if no Left: 1 if yes, 0 if no |
| Knee hyperextension | • Active hyperextension of the knees beyond 10° | Right: 1 if yes, 0 if no Left: 1 if yes, 0 if no |
| Trunk flexion | • Standing forward flexion of the trunk with legs straight and palms flat on the floor | 1 if yes, 0 if no |
| Total score | Sum total points, maximum 9 points >4 points is predictive of hypermobility syndrome |
The apprehension, relocation, and release tests can all be done in quick succession with the patient supine. The apprehension test is performed with the patient’s arm at 90° of abduction, elbow in 90° of flexion, and maximal external rotation (ER) as if he or she were going to throw a ball. Next, with the posterior shoulder stabilized by the examination table, the examiner applies an anterior, external, rotatory force.46 The test is considered positive if the athlete describes an impending sense of dislocation (Figure 3).42 Owens et al,37 in a cohort study of 714 young patients (mean age, 18.8 ± 1.0 years), demonstrated a hazard ratio of 2.96 for having an anterior instability event if the patient had an apprehension sign on exam.
Figure 3.

Apprehension test. The patient is supine on the examination table and the examiner applies a downward force on the left wrist while stabilizing the elbow to evaluate for anterior shoulder laxity.
In the Jobe relocation test, the examiner braces the shoulder anteriorly to apply a posteriorly directed force to relocate the shoulder. The Jobe relocation test is considered positive if the athlete’s apprehension and/or pain dissipates.20
In the release test, the examiner abruptly releases the posteriorly directed force applied to the anterior shoulder. If the patient again feels a send of impending dislocation, the release test is considered positive.14 In a systematic review and meta-analysis of physical examination tests in the shoulder, Hegedus et al17 demonstrated that the release (surprise) test has the greatest sensitivity for anterior instability, with a negative likelihood ratio of 0.25. In addition, the apprehension, Jobe relocation, and release tests all demonstrated high specificity for anterior instability, with the apprehension test having the greatest positive likelihood ratio at 17.2.17
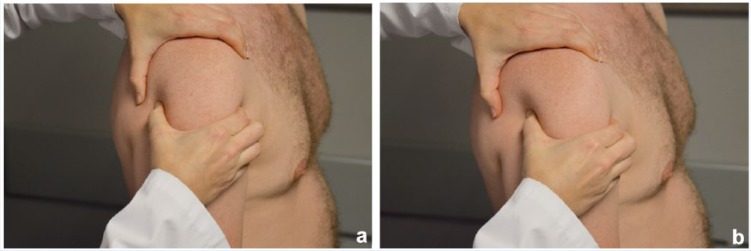
The load and shift test is a test for both anterior and posterior shoulder instability. This maneuver may be performed in both the upright and supine positions with the patient’s shoulder abducted either 0°, 20°, or 90° in the scapular plane and in neutral rotation.25,45 After assuring the humeral head is sitting concentrically within the glenoid (ie, “loaded”), the examiner applies an axial load and anteriorly directed force (to test for anterior instability; apply a posteriorly directed force to evaluate for posterior instability) by holding the proximal humerus with 1 hand while stabilizing the scapula with the other. Reproduction of pain or a palpable clunk associated with subluxation are signs of a positive test (Figure 4). In patients with significant apprehension or a recent dislocation, pain and/or fear may make this test difficult to perform. The examination is graded based on the amount of translation: 0, little to no movement; 1, humeral head moves to the glenoid rim; 2, humeral head dislocates but is spontaneously relocated when the examiner’s force is removed; and 3, humeral head dislocates and does not relocate when pressure is removed.44 The load and shift test has been found to have variable reliability but high specificity for anterior, posterior, and inferior instability despite low sensitivity.45
Figure 4.
(a) The load and shift test performed on a right shoulder. The examiner places 1 hand over the acromion and the other firmly around the humeral head. In this image, the shoulder is resting in its neutral anatomic position. (b) Anteriorly directed force being applied by the examiner to the right shoulder as part of the load and shift test. The examiner is evaluating for excessive translation of the humeral head in relation to the glenoid.
The sulcus test assesses for multidirectional versus unidirectional instability.35 With the patient seated and the arm relaxed at the side in neutral rotation, the examiner gently grasps the arm and applies a downward force while closely assessing for inferior translation of the humeral head relative to the glenoid (Figure 5). Neer and Foster originally described 3 grades of laxity based on the magnitude of translation: 1, translation <1 cm; 2, 1 to 2 cm; and 3, >2 cm.35 When assessing inferior laxity, the sulcus sign has been reported to be more sensitive and equally specific when compared with the load and shift test.45 Additionally, a sulcus sign of 2 cm or greater has been shown to be highly specific (97%), although poorly sensitive, for multidirectional instability.45 Of note, several investigators have demonstrated a positive sulcus sign in patients without pain or instability symptoms.2,18,25 Furthermore, many have demonstrated isolated, often bilateral shoulder laxity in a significant percentage of asymptomatic athletes, further emphasizing the need to correlate examination findings with a thorough history, as laxity is not necessarily indicative of instability.6,12,27,29
Figure 5.

Evaluation of a sulcus sign on the right arm. The examiner applies a downward-directed force to the right arm and is indicating the location where a sulcus sign, an indentation due to excessive laxity of the humeral head in relation to the glenoid, would be. This patient does not have a sulcus sign.
Rotator Cuff Tears
Rotator cuff tears are common, with an overall prevalence of 38.9% for asymptomatic tears and 41.4% for symptomatic full- and partial-thickness tears diagnosed by ultrasound.40 The 4 rotator cuff muscles work with the deltoid as dynamic stabilizers to provide stability to the glenohumeral joint, and injury to any of the 4 may lead to shoulder pain or disability.
Supraspinatus function is best assessed with the Jobe test, which has been described previously. Park et al39 investigated 215 patients with full-thickness supraspinatus tears confirmed by arthroscopy and found the Jobe test to have a sensitivity of 52.6% and specificity of 82.4%. For partial-thickness tears, the same study showed the Jobe test to have a 32.1% sensitivity and 67.8% specificity.39 The drop arm sign may also identify supraspinatus pathology and is particularly useful for diagnosing large tears within the rotator cuff (Table 3). The drop arm sign is performed by passively abducting the patient’s arms to 90° and asking them to hold that position. Inability to maintain that position against gravity is considered a positive test. The drop arm test has been reported to be 35% sensitive and 88% specific for full-thickness tears and 14.3% sensitive and 78% specific for partial-thickness tears.39
Table 3.
Rotator cuff and acromioclavicular joint physical examination maneuvers
| Physical Examination Maneuver | Exam Technique | Interpretation of Findings |
|---|---|---|
| Cross-body adduction | • Patient forward elevates the arm to 90° and actively adducts arm across the body | Positive for acromioclavicular joint pathology if pain is elicited with this maneuver |
| Belly press | • Patient presses abdomen with palm of the hand and maintains shoulder in internal rotation | Positive for subscapularis pathology if elbow drops posteriorly and does not remain anterior |
| Jobe test | • Patient abducts arm to 90°, forward elevates to 30°, and
internally rotates with thumb pointing to the
floor • Examiner applies a downward force while patient attempts to maintain position |
Positive for supraspinatus weakness if patient is unable to maintain the position or for impingement if there is pain |
| External rotation lag sign | • Examiner flexes patient’s elbow to 90°, holding the wrist to
maintain maximum shoulder external rotation • Patient is then instructed to maintain that position |
Positive for infraspinatus weakness if the arm begins to drift into internal rotation |
| Hornblower’s sign | • Examiner brings patient’s shoulder to 90° abduction in the
scapular plane and external rotation • Patient is then instructed to maintain that position |
Positive for teres minor pathology if the patient’s arm begins to fall into internal rotation |
Infraspinatus pathology can be elicited during general strength testing, with pain, guarding, or weakness identified during resisted ER. The ER lag sign can be used to identify infraspinatus pathology without eliciting pain. To assess for a lag sign, the patient’s elbow is flexed to 90° and passively externally rotated 20° to 30°. The patient is instructed to maintain the ER position, and the amount of IR is recorded. Inability to maintain ER defines a positive test and indicates posterior-superior rotator cuff pathology. Castoldi et al9 reported the lag sign to be both highly sensitive and highly specific for combined full-thickness supraspinatus and infraspinatus tears at 97% and 93%, respectively.
The teres minor contributes to ER when the shoulder is abducted to 90° in the scapular plane. Isolated pathology of the teres minor is uncommon, but tears develop from inferior extension of posterosuperior pathology.32 The hornblower’s sign can be used to detect rotator cuff tears involving the teres minor. To perform the examination, the patient’s shoulder is abducted to 90° in the scapular plane and the elbow is flexed to 90°. While maintaining this arm position, the patient is asked to externally rotate against resistance. A positive test occurs when the patient’s arm falls into IR. Walch et al47 found the hornblower’s test to be 100% sensitive and 94% specific for rotator cuff pathology involving the teres minor.
The subscapularis may be involved with anterosuperior rotator cuff tears or may be torn in isolation. Subscapularis pathology may be present with weakness on IR; however, specific tests, including the belly press, lift-off, bear hug, and IR lag tests, may be performed.
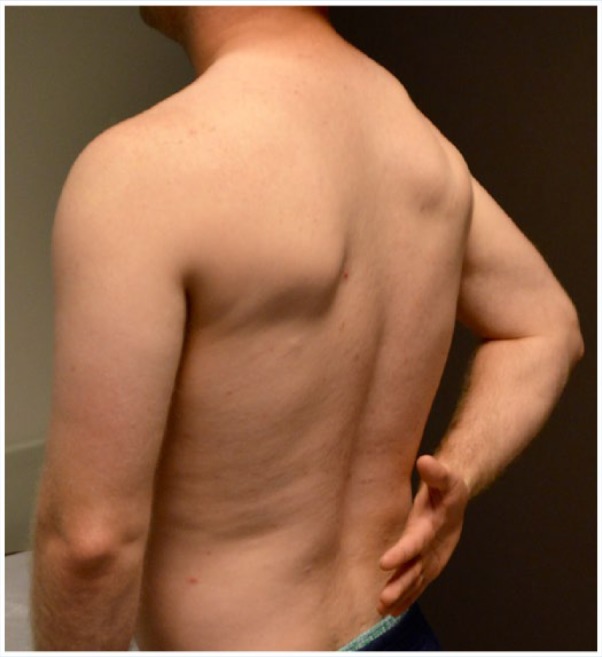
The belly press test is performed by having the patient press on their abdomen with their elbow within the coronal plane (Figure 6). A positive test occurs when the elbow on the affected side moves posteriorly due to recruitment of other muscles to perform the movement (Figure 7). Bartsch et al3 reported the belly press test to have 80% sensitivity and 88% specificity for subscapularis tears.
Figure 6.
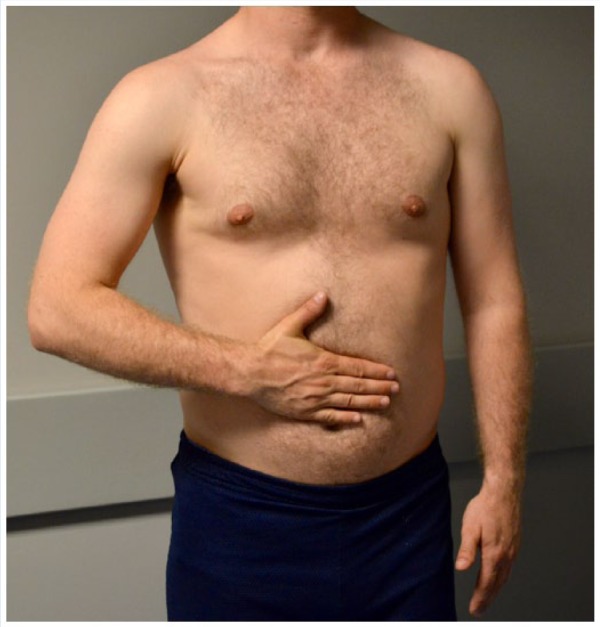
Belly press test performed on a right shoulder. The patient presses the hand into the abdomen with the elbow in the coronal plane. The examiner is evaluating for the elbow dropping posteriorly.
Figure 7.
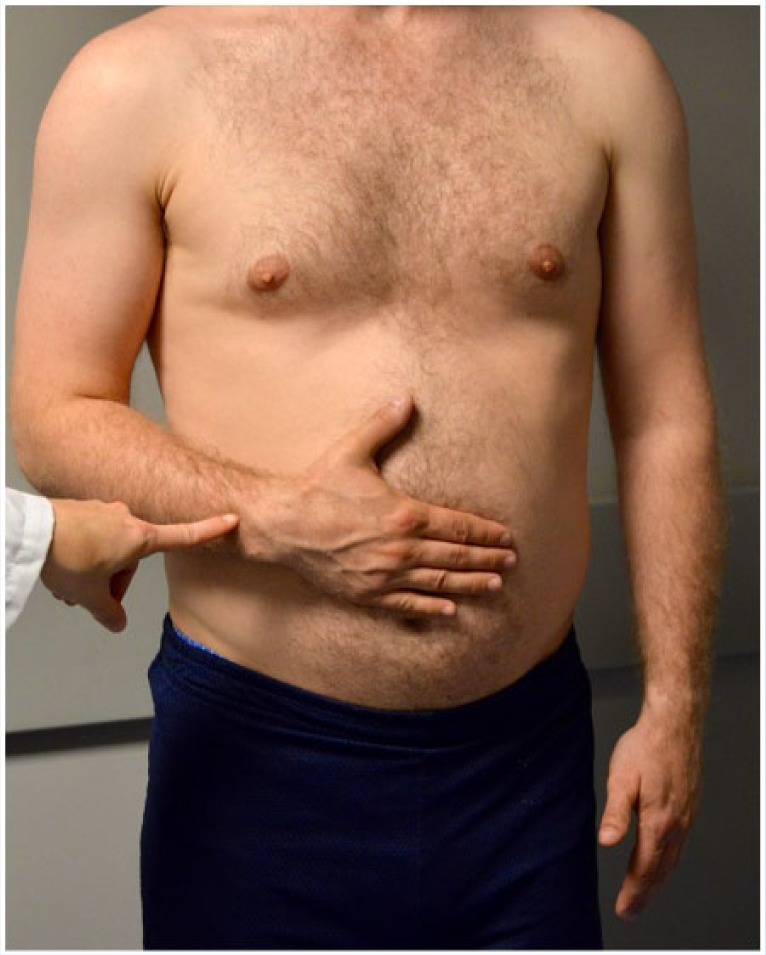
Positive belly press test performed on a right shoulder. The patient presses the hand into the abdomen with the elbow but is unable to maintain the elbow in the coronal plane and the wrist flexes as a result.
The lift-off test is performed by having the patient place the dorsum of their hand against their lumbar spine and attempt to move his or her hand away from the spine (Figure 8). A positive test is defined by inability to move the hand away from the spine. The lift-off test has been reported to be less sensitive and specific than the belly press test, at 40% and 79%, respectively.3
Figure 8.
Lift-off test performed on a right shoulder. The patient reaches to the small of the back with the palm facing posteriorly and then attempts to move the hand away from the spine.
The bear hug test is performed by having the patient place the hand of the affected arm on the contralateral acromioclavicular joint with the hand flat and fingers extended. The elbow of the affected arm should be positioned anterior to the body at the same height as the shoulders. The patient is asked to maintain that position while the examiner applies an ER force to the forearm. Weakness or inability to maintain that position is considered a positive test. Yoon et al49 found the bear hug test to be 19% sensitive but 99% specific for subscapularis tears.
While individual tests can be used to identify rotator cuff pathology, it is recommended that the multiple clinical tests be used in conjunction to evaluate the rotator cuff. Murrell and Walton33 reported that the combination of supraspinatus weakness, ER weakness, and impingement with IR or ER is highly predictive of rotator cuff tears (98% posttest probability, P < 0.0001). When 2 or fewer of the 3 findings are present, however, the posttest probability decreases, showing that the triad of tests should be used frequently for the clinical diagnosis of rotator cuff tears.
Biceps Tendon Injury
Overhead activities, including throwing, can cause shoulder pain due to biceps tendinitis or long head of the biceps tendon (LHBT) instability. The bicipital sling can become disrupted due to partial-thickness tears of the upper border of the subscapularis and/or anterior supraspinatus, resulting in instability of the LHBT.48 Patients with biceps tendinitis typically present with complaints of anterior shoulder pain with activities that place the biceps tendon at risk of subluxation or impingement.
The Speed test evaluates the LHBT and is performed with the shoulder at 90° of flexion, the arm fully supinated, and the elbow fully extended (Table 4). The examiner applies a downward force on the arm, which the patient attempts to resist (Figure 9). Reproduction of pain in the anterior shoulder is considered a positive result. Kibler et al23 showed the Speed test to have a sensitivity of 54% and specificity of 81% for biceps pathology.
Table 4.
Biceps tendon and superior labrum anterior-posterior physical examination maneuvers
| Physical Examination Maneuver | Examination Technique | Interpretation of Findings |
|---|---|---|
| O’Brien test | • Shoulder is elevated to 90° while elbow is
extended • Arm is adducted to 15° and pronated • Examiner then applies downward force to the wrist • Patient then supinates the forearm with palm up and examiner applies downward force again |
Positive for superior labrum anterior-posterior tear when patient has pain when forearm is pronated, but not when the forearm is supinated |
| Bicipital groove tenderness | • Examiner palpates long head of the biceps tendon | Pain elicited with palpation |
| Speed test | • Patient attempts to forward elevate their shoulder against resistance while keeping their elbow extended and forearm supinated | Positive for biceps tendinitis when the patient has pain in the bicipital groove |
| Upper cut test | • Patient attempts to bring their hand to their chin in a boxing
“upper cut” motion starting with their shoulder in the neutral
position, the elbow flexed to 90°, the forearm supinated, and
the hand in a fist • Clinician places his or her hand over the patient’s fist to resist upward motion |
Positive if pain or a popping sensation is elicited over the anterior aspect of the involved shoulder |
Figure 9.

Speed test. The examiner stabilizes the posterior shoulder with 1 hand and applies a downward-directed force to the distal forearm while the patient has the shoulder flexed to 90° and the elbow fully extended. Elicitation of pain in the anterior aspect of the shoulder is considered a positive test.
The Yergason test is performed by having the patient seated with the elbow against the thoracic wall, the elbow flexed at 90°, and the forearm fully pronated. The examiner and patient join hands and the examiner resists the patient’s attempted supination. A positive result is indicated by pain over the bicipital groove or subluxation of the long head of the biceps. Authors have reported the Yergason test to have a sensitivity of 41% and a specificity of 79% for biceps pathology.23
The upper cut test is another maneuver to evaluate biceps tendon pathology. With the shoulder in neutral position, the elbow flexed to 90°, the forearm supinated, and the hand in a fist, the patient moves the hand toward the chin in an “upper cut” motion as a boxer would do while the clinician places his or her hand over the patient’s fist to resist upward motion. The test is considered positive if pain or a popping sensation is elicited over the anterior aspect of the involved shoulder.23 Kibler et al23 reported a sensitivity of 73%, accuracy of 77%, and a positive likelihood ratio of 3.38 for this maneuver.
Slap Lesions
Superior labrum anterior posterior (SLAP) tears are anterior to posterior–directed tears of the superior labrum that are commonly found in throwing athletes and patients who frequently conduct overhead activities.8 Kim et al24 noted a 26% incidence of SLAP tears at time of arthroscopy in 544 patients being treated for a variety of shoulder complaints. The mechanism of injury is thought to be excessive strain on the bicipitolabral complex during the late cocking phase of throwing, which causes the “peeling away” of the superior labrum.7,48 Numerous examination maneuvers have been described to aid in diagnosis of SLAP lesions (Table 4). Authors have recently reported high incidence of SLAP tears in middle-aged patients (45-60 years) with asymptomatic shoulders, emphasizing the need to correlate with clinical examination findings when making treatment decisions.43
Kibler21 originally described the anterior slide test in 1995. With the patient seated, the patient flexes their arm at the elbow with their hand on the hip and thumb facing posteriorly. The examiner then places 1 hand on the superior aspect of the shoulder with the other on the elbow and applies an anterior and superiorly directed force to the elbow while stabilizing the shoulder. Reproduction of pain or a clicking noise in the anterior part of the shoulder is considered a positive test. Kibler21 demonstrated a sensitivity of 78% and a specificity of 91% in his original article.
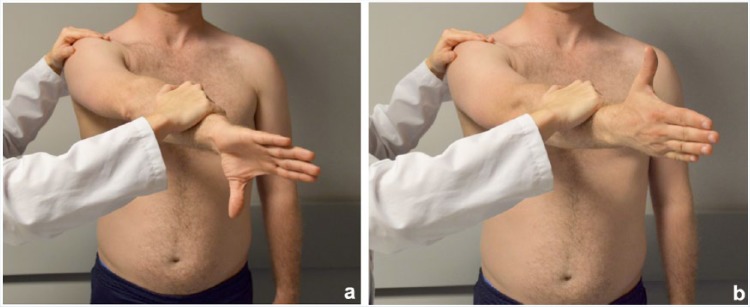
The O’Brien active compression test is another widely used examination maneuver to detect SLAP tears. With the patient in the standing position and the examiner behind the patient, the patient forward flexes the arm to 90°, adducts 10° to 15° medially with the elbow in full extension, and internally rotates the forearm such that the thumb is pointing toward the ground. The examiner then applies a downward-directed force on the anterior forearm. The same motion should be repeated but with the patient’s forearm now supinated such that the palm is facing up. The test is considered positive if pain is reproduced when the forearm is pronated and reduced or eliminated when the forearm is supinated (Figure 10).36 O’Brien et al36 reported a sensitivity of 100% and specificity of 98.5% for detecting labral pathology in their original article; however, numerous investigators have reported a wide-ranging sensitivity and specificity for the maneuver since its creation.11,15,22,38
Figure 10.
(a) The O’Brien active compression test. The examiner stabilizes the posterior shoulder with 1 hand and, with the patient flexing the right arm to 90° and adducting it approximately 30° with a pronated wrist, will ask the patient to supinate against resistance. (b) The patient has supinated against resistance of the examiner at the forearm. Elicitation of pain is considered a positive test.
Acromioclavicular Joint
The acromioclavicular (AC) joint is stabilized by the AC capsule, coracoclavicular ligaments, deltoid muscle, and trapezius muscle, but it is inherently unstable. Pathology of the AC joint, particularly in athletes, can generally be divided into 3 categories: AC separations, AC joint arthrosis, and distal clavicle osteolysis.41 Patients presenting with pathology of the AC joint will typically complain of superior shoulder pain or directly isolate the pain to the AC joint. Patients with acute pain will usually recall recent trauma to the shoulder or AC joint. Specific physical examination maneuvers have been described to identify AC joint pathology, including the O’Brien active compression test and the cross-body adduction sign (see Table 3). The O’Brien active compression test was previously described in this review to detect SLAP tears but can also identify AC joint pathology. The cross-body adduction test was first described by McLaughlin30 in 1951 to detect AC joint pathology. The test is performed by having the patient forward-flex their arm at the shoulder and adduct the arm across the body. The test is positive if it reproduces pain in the AC joint or superior shoulder. Authors have reported the cross-body adduction test to have a sensitivity of 77% and a specificity of 79% for AC joint pathology.10
Conclusion
The shoulder is a complex constellation of structures affording the greatest range of motion of any joint in the body. A thorough history and physical examination with specific examination maneuvers are key to creating a good differential diagnosis. Understanding the utility and limitations of these maneuvers is helpful in narrowing a differential diagnosis and therapeutic decision-making.
Footnotes
The following author declared potential conflicts of interest: Bernard R. Bach Jr, MD, receives royalties from SLACK Inc and research support from Tornier, Arthrex Inc, CONMED Linvatec, DJ Orthopaedics, Ossur, and Smith & Nephew.
References
- 1. Andrews JR, Wilcox CL. Decision making in the throwing athlete. Sports Med Arthrosc. 2014;22:130-136. [DOI] [PubMed] [Google Scholar]
- 2. Bahk M, Keyurapan E, Tasaki A, Sauers EL, McFarland EG. Laxity testing of the shoulder: a review. Am J Sports Med. 2007;35:131-144. [DOI] [PubMed] [Google Scholar]
- 3. Bartsch M, Greiner S, Haas NP, Scheibel M. Diagnostic values of clinical tests for subscapularis lesions. Knee Surg Sports Traumatol Arthrosc. 2010;18:1712-1717. [DOI] [PubMed] [Google Scholar]
- 4. Beighton P. Hypermobility scoring. Br J Rheumatol. 1988;27:163. [DOI] [PubMed] [Google Scholar]
- 5. Bhattacharyya R, Edwards K, Wallace AW. Does arthroscopic sub-acromial decompression really work for sub-acromial impingement syndrome: a cohort study. BMC Musculoskelet Disord. 2014;15:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609-613. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS, Morgan CD. The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy. 1998;14:637-640. [DOI] [PubMed] [Google Scholar]
- 8. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part III. The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19:641-661. [DOI] [PubMed] [Google Scholar]
- 9. Castoldi F, Blonna D, Hertel R. External rotation lag sign revisited: accuracy for diagnosis of full thickness supraspinatus tear. J Shoulder Elbow Surg. 2009;18:529-534. [DOI] [PubMed] [Google Scholar]
- 10. Chronopoulos E, Kim TK, Park HB, Ashenbrenner D, McFarland EG. Diagnostic value of physical tests for isolated chronic acromioclavicular lesions. Am J Sports Med. 2004;32:655-661. [DOI] [PubMed] [Google Scholar]
- 11. Cook C, Beaty S, Kissenberth MJ, Siffri P, Pill SG, Hawkins RJ. Diagnostic accuracy of five orthopedic clinical tests for diagnosis of superior labrum anterior posterior (SLAP) lesions. J Shoulder Elbow Surg. 2012;21:13-22. [DOI] [PubMed] [Google Scholar]
- 12. Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20-26. [DOI] [PubMed] [Google Scholar]
- 13. Garrett WE, Jr, Swiontkowski MF, Weinstein JN, et al. American board of orthopaedic surgery practice of the orthopaedic surgeon: part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660-667. [DOI] [PubMed] [Google Scholar]
- 14. Gross ML, Distefano MC. Anterior release test. A new test for occult shoulder instability. Clin Orthop Relat Res. 1997;339:105-108. [DOI] [PubMed] [Google Scholar]
- 15. Guanche CA, Jones DC. Clinical testing for tears of the glenoid labrum. Arthroscopy. 2003;19:517-523. [DOI] [PubMed] [Google Scholar]
- 16. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151-158. [DOI] [PubMed] [Google Scholar]
- 17. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46:964-978. [DOI] [PubMed] [Google Scholar]
- 18. Jia X, Ji JH, Petersen SA, Freehill MT, McFarland EG. An analysis of shoulder laxity in patients undergoing shoulder surgery. J Bone Joint Surg Am. 2009;91:2144-2150. [DOI] [PubMed] [Google Scholar]
- 19. Jobe FW, Jobe CM. Painful athletic injuries of the shoulder. Clin Orthop Relat Res. 1983;173:117-124. [PubMed] [Google Scholar]
- 20. Jobe FW, Kvitne RS, Giangarra CE. Shoulder pain in the overhand or throwing athlete. The relationship of anterior instability and rotator cuff impingement. Orthop Rev. 1989;18:963-975. [PubMed] [Google Scholar]
- 21. Kibler WB. Specificity and sensitivity of the anterior slide test in throwing athletes with superior glenoid labral tears. Arthroscopy. 1995;11:296-300. [DOI] [PubMed] [Google Scholar]
- 22. Kibler WB, Sciascia A. Current practice for the diagnosis of a SLAP lesion: systematic review and physician survey. Arthroscopy. 2015;31:2456-2469. [DOI] [PubMed] [Google Scholar]
- 23. Kibler WB, Sciascia AD, Hester P, Dome D, Jacobs C. Clinical utility of traditional and new tests in the diagnosis of biceps tendon injuries and superior labrum anterior and posterior lesions in the shoulder. Am J Sports Med. 2009;37:1840-1847. [DOI] [PubMed] [Google Scholar]
- 24. Kim TK, Queale WS, Cosgarea AJ, McFarland EG. Clinical features of the different types of SLAP lesions: an analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am. 2003;85-A:66-71. [PubMed] [Google Scholar]
- 25. King JJ, Wright TW. Physical examination of the shoulder. J Hand Surg Am. 2014;39:2103-2112. [DOI] [PubMed] [Google Scholar]
- 26. Lesniak BP, Baraga MG, Jose J, Smith MK, Cunningham S, Kaplan LD. Glenohumeral findings on magnetic resonance imaging correlate with innings pitched in asymptomatic pitchers. Am J Sports Med. 2013;41:2022-2027. [DOI] [PubMed] [Google Scholar]
- 27. Lintner SA, Levy A, Kenter K, Speer KP. Glenohumeral translation in the asymptomatic athlete’s shoulder and its relationship to other clinically measurable anthropometric variables. Am J Sports Med. 1996;24:716-720. [DOI] [PubMed] [Google Scholar]
- 28. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000;9:299-301. [DOI] [PubMed] [Google Scholar]
- 29. McFarland EG, Campbell G, McDowell J. Posterior shoulder laxity in asymptomatic athletes. Am J Sports Med. 1996;24:468-471. [DOI] [PubMed] [Google Scholar]
- 30. McLaughlin HL. On the frozen shoulder. Bull Hosp Joint Dis. 1951;12:383-393. [PubMed] [Google Scholar]
- 31. Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90:1898-1903. [DOI] [PubMed] [Google Scholar]
- 32. Moulton SG, Greenspoon JA, Millett PJ, Petri M. Risk factors, pathobiomechanics and physical examination of rotator cuff tears. Open Orthop J. 2016;10:277-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murrell GA, Walton JR. Diagnosis of rotator cuff tears. Lancet. 2001;357:769-770. [DOI] [PubMed] [Google Scholar]
- 34. Neer CS., 2nd Impingement lesions. Clin Orthop Relat Res. 1983;173:70-77. [PubMed] [Google Scholar]
- 35. Neer CS, 2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. A preliminary report. J Bone Joint Surg Am. 1980;62:897-908. [PubMed] [Google Scholar]
- 36. O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med. 1998;26:610-613. [DOI] [PubMed] [Google Scholar]
- 37. Owens BD, Campbell SE, Cameron KL. Risk factors for anterior glenohumeral instability. Am J Sports Med. 2014;42:2591-2596. [DOI] [PubMed] [Google Scholar]
- 38. Parentis MA, Glousman RE, Mohr KS, Yocum LA. An evaluation of the provocative tests for superior labral anterior posterior lesions. Am J Sports Med. 2006;34:265-268. [DOI] [PubMed] [Google Scholar]
- 39. Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87:1446-1455. [DOI] [PubMed] [Google Scholar]
- 40. Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ. Dead men and radiologists don’t lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006;88:116-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med. 2008;27:763-788. [DOI] [PubMed] [Google Scholar]
- 42. Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63:863-872. [PubMed] [Google Scholar]
- 43. Schwartzberg R, Reuss BL, Burkhart BG, Butterfield M, Wu JY, McLean KW. High prevalence of superior labral tears diagnosed by MRI in middle-aged patients with asymptomatic shoulders. Orthop J Sports Med. 2016;4: 2325967115623212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Silliman JF, Hawkins RJ. Classification and physical diagnosis of instability of the shoulder. Clin Orthop Relat Res. 1993;291:7-19. [PubMed] [Google Scholar]
- 45. Tzannes A, Murrell GA. Clinical examination of the unstable shoulder. Sports Med. 2002;32:447-457. [DOI] [PubMed] [Google Scholar]
- 46. van Kampen DA, van den Berg T, van der Woude HJ, Castelein RM, Terwee CB, Willems WJ. Diagnostic value of patient characteristics, history, and six clinical tests for traumatic anterior shoulder instability. J Shoulder Elbow Surg. 2013;22:1310-1319. [DOI] [PubMed] [Google Scholar]
- 47. Walch G, Boulahia A, Calderone S, Robinson AH. The ‘dropping’ and ‘hornblower’s’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80:624-628. [DOI] [PubMed] [Google Scholar]
- 48. Winter SB, Hawkins RJ. Comprehensive history and physical examination of the throwing shoulder. Sports Med Arthrosc. 2014;22:94-100. [DOI] [PubMed] [Google Scholar]
- 49. Yoon JP, Chung SW, Kim SH, Oh JH. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg. 2013;22:1186-1192. [DOI] [PubMed] [Google Scholar]