Abstract
Introduction:
Centralized waiting lists (CWLs) are one solution to reduce the problematic number of patients without a regular primary care provider. This article describes different models of CWLs for unattached patients implemented in seven Canadian provinces and identifies common issues in the implementation of these CWLs.
Methods:
Logic models of each province's intervention were built after a grey literature review, 42 semi-structured interviews and a validation process with key stakeholders were performed.
Results:
Our analysis across provinces showed variability and common features in the design of CWLs such as same main objective to attach patients to a primary care provider; implementation as a province-wide program with the exception of British Columbia; management at a regional level in most provinces; voluntary participation for providers except in two provinces where it was mandatory for providers to attach CWL patients; fairly similar registration process across the provinces; some forms of prioritization of patients either using simple criteria or assessing for vulnerability was performed in most provinces except New Brunswick.
Conclusion:
Despite their differences in design, CWLs implemented in seven Canadian provinces face common issues and challenges regarding provider capacity to address the demand for attachment, barriers to the attachment of more vulnerable and complex patients as well as non-standardized approaches to evaluating their effectiveness. Sharing experiences across provinces as CWLs were being implemented would have fostered learning and could have helped avoid facing similar challenges.
Abstract
Introduction:
Les listes d'attente centralisées (LAC) constituent une solution afin de réduire les problématiques reliées au taux de patients sans affiliation à un professionnel de première ligne. Cet article décrit divers modèles de LAC pour les patients non-affiliés qui ont été implantés dans sept provinces canadiennes et recense les enjeux communs liés à leur mise en œuvre.
Méthode:
Des modèles logiques pour chacune des interventions provinciales ont été élaborés suite à une revue de la littérature grise, à 42 entrevues semi-dirigées et à un processus de validation auprès d'acteurs concernés.
Résultats:
Notre analyse montre une variabilité et des caractéristiques communes dans la conception des LAC, notamment un même objectif principal visant la prise en charge des patients par un professionnel de première ligne; la mise en œuvre d'un programme pour l'ensemble de la province, à l'exception de la Colombie-Britannique; la gestion au niveau régional dans la plupart des provinces; la participation volontaire des professionnels, sauf dans deux provinces où ils ont l'obligation de prendre en charge les patients inscrits à la LAC; des processus d'inscription plutôt similaires d'une province à l'autre; une certaine forme de priorisation des patients, soit à l'aide de critères simples ou en évaluant leur vulnérabilité, et ce, dans la plupart des provinces sauf au Nouveau-Brunswick.
Conclusion:
Malgré les différences dans la conception, les LAC mis en œuvre dans sept provinces canadiennes font face à des enjeux et défis communs quant à la capacité de traiter les demandes de prise en charge, quant aux obstacles pour la prise en charge des patients plus vulnérables et dont l'état est complexe, et quant à la non standardisation des processus pour l'évaluation de l'efficacité. Le partage de l'expérience entre les provinces au moment de la mise en œuvre des LAC aurait favorisé l'apprentissage et aurait permis d'éviter de rencontrer des défis similaires.
Introduction
Routine and episodic access to the same individual or group of primary care providers is widely considered to be essential for realizing the benefits of primary care. Specifically, primary care nurse practitioners (NPs) or family physicians (FPs) can provide accessible, continuous and comprehensive care that is coordinated with other levels (e.g., secondary, tertiary) or types (e.g., social, community-based) of care. Patients who are “attached” to a regular primary care provider receive more preventive care (Grunfeld et al. 2006; Starfield et al. 2005), use emergency services less frequently (Burge et al. 2003) and have better care coordination (Bayliss et al. 2008; Fung et al. 2015), chronic disease management (Østbye et al. 2005) and health outcomes (Griffin et al. 2004; Oates et al. 2000) than those who are not.
In Canada, however, approximately 15% of the population reported not having a regular primary care provider, ranging from 8% in Ontario (ON) to 25% in Quebec (QC) (Commissaire à la santé et au bien être 2014). Canada's rate of unattached patients compared poorly to other Organisation for Economic Co-operation and Development (OECD) countries, such as France, Germany and Norway, where less than 5% of the population reported lacking a regular primary care provider, ranking Canada in the more poorly performing end of the list with countries such as the UK (19%) and the US (23%) (Commissaire à la santé et au bien être 2014; Schoen et al. 2007). To address this important concern, seven provinces, British Columbia (BC), Manitoba (MB), ON, QC, New Brunswick (NB), Prince Edward Island (PEI) and Nova Scotia (NS), have implemented centralized waiting lists (CWLs) for unattached patients in primary care (Table 1). These CWLs coordinate, in a single point of access, patients' demand for attachment to a primary care provider and match unattached patients to available primary care providers, in a given jurisdiction.
Table 1.
Centralized waiting lists for unattached patients implemented across Canada
| Province | Program name | Implementation year |
|---|---|---|
| Prince Edward Island | Patient Registry Program | 1998 |
| Quebec | Guichets d'accès à un médecin de famille | 2008 |
| Ontario | Health Care Connect | 2009 |
| Manitoba | Family Doctor Finder | 2013 |
| New Brunswick | Patient Connect NB | 2013 |
| British Columbia | A GP for Me | 2015 |
| Nova Scotia | Need a Family Practice | 2016 |
GP = general practitioner; NB = New Brunswick.
CWLs are implemented to improve access to care in contexts where there is asymmetry of supply and demand. The basic idea of a CWL is to have a single intake point to centralize patient demand for a given service and link patients to a provider from within a pool of providers. CWLs have been implemented in many fields of healthcare, notably in the management of wait for elective surgeries (Dew et al. 2005; Noseworthy et al. 2003). To our knowledge, there is no evidence of the use of CWLs in the context of primary care outside the Canadian context (Breton et al. 2015). Within Canada, CWLs for unattached patients are quite different in each province and there is limited knowledge exchange between provinces regarding these initiatives.
The objective of this paper is to describe the different models of CWLs for unattached patients implemented in seven Canadian provinces and to identify common issues in the implementation of these CWLs.
Methods
Design: This paper presents the results of the first step of a logic analysis. Logic analysis is a theory-based evaluation that is conducted in three steps: (1) build logic models of the interventions; (2) develop a conceptual framework based on scientific knowledge; and (3) compare the logic models to the conceptual framework (Brousselle and Champagne 2011).
In this first step, logic modelling is used to represent how the interventions' inputs and processes are intended to lead to the desired outcomes, drawing on information from documents and key informants' interviews (Brousselle and Champagne 2011). Once the logic models are built, stakeholders are consulted to identify issues (e.g., implementation difficulties) to be explored in detail in the subsequent steps of the logic analysis.
Data collection and analysis: Our data collection and analysis protocol are detailed elsewhere (Breton et al. 2017). Briefly, we first searched for documents describing the main components of each province's CWL by applying systematic search strategies to the grey literature (Godin et al. 2015). We conducted searches in grey literature databases (Canadian Research Index, TRIP database, Des Libris – The Canadian Electronic Library), Google and on targeted websites (e.g., national and provincial government websites, medical association websites, provincial newspapers, health institutions' websites). In addition, we used snowballing and asked key stakeholders in each province to identify other relevant documents. The 73 identified documents were analyzed to prepare a description of the components of the CWLs in each province. To gain a more accurate understanding of our CWL descriptions, we conducted 42 semi-structured interviews with 3–8 key stakeholders per province (BC = 3, MB = 8, ON = 8, QC = 7, NB = 4, PEI = 4 and NS = 8) in person or by telephone. The interview guide was based on the logic model components. Participants were sampled purposively based on their knowledge of CWLs for unattached patients. Participants included CWL managers and staff as well as, in ON and QC, primary care providers who attached CWL patients. Variations in the number of stakeholders interviewed per province reflect differences in the number of stakeholders involved in implementing CWLs. In BC, because CWLs were implemented only by certain Divisions of Family Practice (i.e., community-based groups of FPs in the same geographic area) rather than provincially, interviews were conducted with stakeholders in two divisions. These divisions were chosen in partnership with provincial-level BC stakeholders. Although both CWLs were similar, for the development of the logic models, only one division was studied as the information was more complete. Issues stated from stakeholders from both divisions were integrated.
Interviews were conducted between May and December 2016 in all provinces but NS, which was not originally included in our study because the CWL was still in the early stages of implementation. In response to interest from provincial stakeholders, we added NS to our study, conducting interviews between October and December 2017. Prior to the interviews, participants were provided with the preliminary description of the CWL in their province, based on the grey literature review. Interviews were conducted by an investigator from the corresponding province because of their knowledge of the provincial context. All interviews were audio recorded and transcribed.
The data were analyzed with NVivo version 11, using a codebook based on Mitchell and Lewis's logic model (Mitchell and Lewis 2003) and adapted to reflect the general components of CWLs (Figure 1). This particular model offers a simple diagram of the main components of a unique intervention and is widely used in research on primary care interventions in Canada (Haggerty et al. 2014). Two independent team members coded the data to ensure repeatability and reliability of the process. Data from each province were summarized and a logic model for each province was built. To increase trustworthiness, the logic models were member-checked (Laperrière 1997; Mays and Pope 1995) with key stakeholders and investigators from each province during a video conference. In addition, interviews were analyzed thematically to identify common issues in the implementation of CWLs raised by stakeholders.
Figure 1.
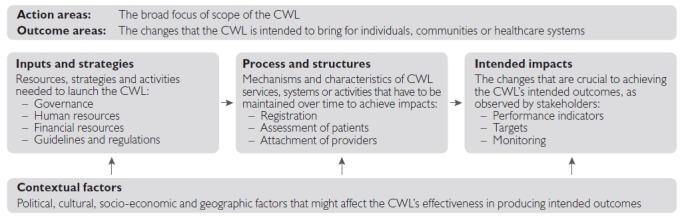
Logic model
CWL = centralized waiting list.
The design of CWLs was compared and contrasted by the research team to examine similarities and differences. Moreover, issues with CWLs raised during interviews with stakeholders were summarized. At a pan-Canadian symposium in February 2017, 20 stakeholders (CWL managers, providers, decision-makers) and investigators from six provinces discussed and added to the comparative analysis of the CWLs. NS stakeholders did not participate in the symposium because they joined the study later.
Results
A comparison of the CWLs' key characteristics is presented based on each dimension of the logic model, followed by a summary of the common issues identified by the stakeholders. The seven CWL logic models can be found in Appendix 1 (available at: Appendix 1).
Action areas and outcome areas
The seven CWLs were implemented in the action area of improving access to primary healthcare. CWLs were implemented in every province with the primary aim of making sure that every patient in the province is attached to a primary care provider. NS stakeholders emphasized that they had implemented a “registry” rather than a formal waiting list. From their point of view, the registry was different than a waiting list as it did not guarantee that patients would be attached to a primary care provider quickly. As stated by stakeholders, the absence of formal guarantee of attachment in NS was reportedly misunderstood by the public, which created expectations from the population to be attached to a provider through the list.
Three provinces (BC, QC and ON) had an objective of prioritizing vulnerable patients, generally defined in these provinces as those with higher health needs, in the attachment to a primary care provider. In QC, vulnerable patients were defined as those having at least one of 19 health conditions (e.g., active cancer, mental health problem, addiction, diabetes) based on self-reported information and health insurance data, or being over 70 years old and patients with more urgent health needs (e.g., palliative care, active cancer) were prioritized. In ON, patients were considered to be vulnerable if they had one or more co-morbidities or were considered frail, based on self-reported health status, chronic conditions, disability, mental status and body mass index. In BC, there were no formal definitions of vulnerable patients, but certain patients who were considered by the CWL coordinator to have complex conditions or for whom attachment could be most beneficial were prioritized and priorities were based on the community's needs. In addition, QC, PEI and NS created and used CWLs as a tool to monitor the number of unattached patients. NS used the information from the CWL to document problems regarding the geographic distribution of primary care providers and planned the allocation of additional resources based on this information.
Inputs and strategies
The main characteristics of the inputs and strategies are presented in Table 2. In all provinces except BC, the CWLs were implemented as a province-wide program, supported by staff and provincial governance structures. In BC, as part of a temporary provincial initiative called A GP for Me (General Practice Services Committee 2015) that aimed to help attach patients to providers and improve access to care for vulnerable populations, only certain Divisions of Family Practice chose to implement CWLs.
Table 2.
Characteristics of the inputs and strategies in the seven provinces
| Inputs and strategies | BC | MB | ON | QC | NB | PEI | NS |
|---|---|---|---|---|---|---|---|
| Governance | |||||||
| Province-wide implementation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Management at regional level | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| CWL implemented as a permanent measure | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Human resources | |||||||
| CWL care connectors at regional level | ✓ | ✓ | ✓ | ✓ | |||
| Patients can be attached to nurse practitioners | ✓ | ✓ | ✓ | ✓ | |||
| Financial resources, guidelines and regulations | |||||||
| Financial incentives to attach CWL patients | ✓ | ✓ | ✓ | ||||
| Mandatory attachment of CWL patients for certain providers | ✓ | ✓ | |||||
BC = British Columbia; CWL = centralized waiting list; MB = Manitoba; NB = New Brunswick; NS = Nova Scotia; ON = Ontario; PEI = Prince Edward Island; QC = Quebec.
In BC and NB, CWLs were implemented as temporary programs, as opposed to other provinces where CWLs had been implemented as permanent measures. In NB, the CWL was planned to be replaced by another initiative by 2020. In BC, funding from the aforementioned A GP for Me program had come to an end at the time of data collection and strategies were being discussed to secure alternate funding to sustain regional CWLs in the future. In NS, the Department of Health and Wellness had reallocated human and financial resources, from within their existing resources, for the CWL's operations, rather than having a dedicated provincial budget for the CWL. Stakeholders in this province noted that the absence of dedicated managers or resources for managing and operating the CWL posed a risk for the success of its implementation.
Two provinces had a formal attachment, meaning that a patient's attachment to a primary care provider was formally recorded in the provincial health insurance database. In QC, patients and FPs had to sign an agreement officialising attachment. In ON, formalization of attachment varied according to FPs' compensation models. For instance, under capitation (e.g., in Family Health Teams – a team-based model of primary healthcare), providers were required to formally attach patients.
In all provinces, CWL patients were mainly attached to FPs. In QC and MB, patients were not eligible to be attached to an NP, and in PEI, it was reported that only one NP had her own patient panel and, consequently, used the CWL. In NS, NPs in team-based practices were considered as resources to increase capacity, allocated to the group after attaching a target number of patients and, hence, could not attach patients themselves, as opposed to NPs in solo practices who could have their own panel.
In four provinces (MB, ON, QC and NS), CWLs were regionally managed and operated, although they were implemented province-wide. General guidelines for CWL operations, financial incentives (if any), regulations and monitoring were generally defined provincially in these provinces, while human resources, such as care connectors, were employed at the regional level to operate the CWLs. Care connectors were described as professional staff, usually nurses, who were responsible for the CWLs' activities, namely from registration to attachment. Care connectors were also generally involved in developing relationships with providers and facilitating their participation in CWLs at a regional level. Other provinces (NB, BC and PEI) had smaller-scale programs involving fewer human resources and were governed, managed and operated at a provincial level. In PEI, one full-time clerk and one part-time manager worked in the CWL. In NB, the program was embedded with the provincial health information phone line. In BC, at the regional level, a medical office assistant coordinated the CWL.
In all provinces, except for certain FPs in NB and PEI, primary care providers participated in CWLs on a voluntary basis; that is, it was not mandatory for providers to attach patients from the CWLs, and providers could, for instance, choose to attach patients they had seen at walk-in clinics rather than through the CWLs. In NB, a provincial policy mandated new FPs to attach 600 patients from the CWL in their first year of practice. In PEI, participation was mandatory for contract and salaried FPs, meaning that they had an obligation to attach patients from the CWL.
Financial incentives had been used to increase FPs' participation in CWLs in ON, QC, NB and PEI. For example, in QC, FPs received a one-time financial incentive for every patient attached through the CWL modulated by the degree of medical vulnerability, from $23 for a healthy patient to $300 for a patient with mental health or substance abuse problems. For FPs who had been practising for over four years, the financial incentives were limited to the first 150 newly attached patients (i.e., added to their existing patient panel) from the CWL, per year. In contrast, an unlimited number of patients could be attached from the CWL for an FP with less than four years of practice. In PEI, FPs receive a bonus of $150 for each new patient attached after reaching a target panel of 1,200 patients, while NPs did not receive this incentive. Stakeholders expressed concern regarding the potential for providers to use the system for individual benefit (i.e., gaming the system), namely in terms of financial gain. Such behaviour was reported to have an impact on costs and led to cherry picking/creaming (e.g., selecting less complex patients for attachment), which in turn may have affected the equity of attachment to primary care providers (Breton et al. 2015; Rudoler et al. 2015a; Rudoler et al. 2015b). ON reportedly ceased the allocation of financial incentives for the attachment of patients through the CWL and observed a decrease in providers' use of the CWL to attach patients following this decision. NB also saw a reduction in FPs' use of the CWL when financial incentives were changed.
Process and structures
We present CWLs' processes and structures based on three sequential activities from the logic models: registration on the CWL, assessment of patients and attachment to a primary care provider.
Registration on the CWL
Characteristics of the CWLs' registration process varied across provinces (Table 3). In most provinces, being unattached was an eligibility criterion for patients to register on the CWL. In the two provinces (ON and QC) where attachment was formally recorded, patients with a provider wishing to register on the CWL (e.g., because they wanted to change providers or because they were moving to another region) had to withdraw from their current attachment, a complex process that stakeholders described as a barrier to registration. QC stakeholders also mentioned that some patients were unaware that they were already attached to a provider, which could lead to additional difficulties for patients when trying to register on the CWL. In NS, the only attached patients who were eligible for registration on the CWL were those who were moving and who wanted a provider in their new location. In MB and NB, all patients were eligible to register; however, unattached patients were prioritized over patients who wanted to change providers.
Table 3.
Characteristics of the registration process in the seven provinces
| Processes and structures | BC | MB | ON | QC | NB | PEI | NS |
|---|---|---|---|---|---|---|---|
| Eligibility criteria for registering on CWL | |||||||
| Registration limited to unattached patients | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Ways to register on CWL | |||||||
| Patients can register by telephone | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Patients can register online | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| Information collected upon registration to CWL | |||||||
| Demographic information is collected | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Medical information is collected | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Patient can state their preferences for providers | ✓ | ✓ | ✓ | ✓ | |||
| Patients' registration information update while waiting for attachment | |||||||
| Information updated with an automatic process | ✓ | ✓ | ✓ | ||||
| Information is manually verified with patients | ✓ | ✓ | ✓ | ||||
BC = British Columbia; CWL = centralized waiting list; MB = Manitoba; NB = New Brunswick; NS = Nova Scotia; ON = Ontario; PEI = Prince Edward Island; QC = Quebec.
Patients could register on the CWL by telephone and online in every province except in BC where registration was only by telephone. In addition to demographic information, patients could state their preferences regarding a provider (e.g., preference for an NP or FP, sex and region of primary care provider, preferred language); in BC, MB, NB and PEI, these were taken into account in the attachment process. Patients' medical information was collected through a self-reported questionnaire in QC, ON, BC, PEI and NB. In NS, this information was not collected and in MB, it was documented only if mentioned by the patient.
An important challenge arising in some provinces (ON, QC and NB) was the large influx of patients registering on the CWL when FPs retired. Many stakeholders reported that the CWLs were being used to manage the turnover of providers (e.g., new providers, retirement), which had led to difficulties in managing the influx of patients and increased healthcare system costs. For example, stakeholders explained that, when retiring, some providers detached all their patients and had them register on the CWL, instead of directly transferring their panel to new providers as would have been the case before CWLs were implemented. To address these issues, ON and QC had implemented measures to avoid massive registration. In QC, for example, FPs had to advise their patients of their upcoming retirement two years in advance and patients from a retiring FP then became eligible to register on the CWL without having to go through the detachment process. In NB, at the time of data collection, a new program for retirement was planned to partially replace the CWL.
Five provinces (ON, QC, NB, PEI and NS) had implemented processes to verify and update patients' information. In NB and NS, there were automated phone calls to patients waiting on the list on a quarterly basis with options to update information if needed. In PEI, temporary staff was hired to call patients on the list, validate their unattached status and update their information. In QC, because the list was linked to the provincial health insurance database, patients' information was automatically and regularly updated.
Assessment of patients
The assessment of patients registered on the CWLs differed across the provinces (Table 4). All provinces but NB gave certain patients priority over others; however, some provinces prioritized certain groups of patients based on a few simple criteria, such as being unattached (MB and NS), being referred by a hospital (MB and PEI), having urgent needs (PEI), being a newborn/new mother or having cancer (MB). Within these CWLs, patients were attached to a provider in the order of their date of registration with the exception of patients meeting the simple prioritization criteria, who were moved forward on the list.
Table 4.
Characteristics of the assessment process in the seven provinces
| Assessment | BC | MB | ON | QC | NB | PEI | NS |
|---|---|---|---|---|---|---|---|
| Prioritization of patients for attachment | |||||||
| No prioritization – attachment based on date of registration | ✓ | ||||||
| Simple prioritization – certain groups of patients prioritized for attachment | ✓ | ✓ | ✓ | ||||
| Prioritization of complex/vulnerable patients – patients assessed as complex/vulnerable are prioritized for attachment | ✓ | ✓ | ✓ | ||||
| Alternative or transitional services during wait for attachment | |||||||
| Patient can receive transitional care (during wait) | ✓ | ✓ | |||||
BC = British Columbia; MB = Manitoba; NB = New Brunswick; NS = Nova Scotia; ON = Ontario; PEI = Prince Edward Island; QC = Quebec.
In BC, ON and QC, patients were prioritized based on the assessment of their complexity or vulnerability. The assessment of vulnerability and reasons for completing this assessment differed across provinces, which also led to differences in what was defined as vulnerability between provinces. In ON, there was an automated prioritization process with an algorithm based on patients' answers to a self-reported health questionnaire. Within this system, based on a score from 0 to 10, patients were labelled not vulnerable or “complex vulnerable.” In BC and QC, the management process involved assigning patients to a category of priority. In QC, in addition to a self-reported questionnaire, the CWL was directly linked with the provincial health insurance system, and so, previous diagnoses automatically appeared in patients' files. If requested by patients upon registration, a health assessment could be conducted over the phone by a nurse. In QC, there are five formally defined categories of priority from the most urgent health conditions to the least urgent with recommended target wait times. For example, the highest category of priority (A) is for patients with urgent health conditions (target time of 7 days) such as active cancer, palliative care, psychotic state, suicidal ideas and pregnancy. In BC, based on collected information, the coordinator responsible for the CWL assigned a category of priority. The criteria for assigning patients to each category were not formally defined; however, complex and vulnerable patients were reported to be prioritized by the coordinator. In MB, care connectors in some regions undertook their own assessment of patients' vulnerability, not for prioritization, but rather to better match patients with a suitable provider.
Additionally, to providing information to CWL patients on existing services such as health information phone lines (e.g., 8-1-1) and walk-in clinics, two provinces (BC and NB) offered transitional care to vulnerable or complex patients while they waited on the CWL. In BC, vulnerable patients were seen in access clinics with a multidisciplinary team to stabilize their chronic medical conditions, before being attached to a primary care provider. In NB, there were special clinics named “Patient Registry Clinics” in two urban centres where, on a temporary basis, care was provided to vulnerable unattached patients until they were attached to a provider.
Attachment to a provider
The attachment process varied from one province to another. Three provinces (BC, ON and PEI) had processes in place to allow for family members to be attached to the same provider. Some provinces formally (ON) or informally (MB) asked providers about their preferences in types of patients. Stakeholders in several provinces mentioned the difficulty of finding providers willing to accept patients with certain conditions, notably substance abuse and mental health issues.
Some stakeholders stated issues regarding contacting patients for their first appointment with their new provider, particularly when an appointment was necessary to confirm attachment and to remove the patient from the CWL. NB, for example, had implemented a maximum period of two weeks for the first contact between the patients and their new provider, which was identified by stakeholders as too short of a period and, consequently, a barrier to attachment.
The distance between patients' residence and providers' practice was considered to be an important issue. For example, in QC, a policy on maximum distance between patients and providers had been implemented province-wide and had led to issues in urban areas where the maximum distance was considered too long and in rural areas where it was too short. To address this issue, it was decided that criterion related to distance was to be determined by regional management so it could be adapted to regional contexts. In all provinces except BC, patients could refuse attachment to the provider with whom they had been matched through the CWL and could return on the CWL with their original registration date. In BC, stakeholders reported that the CWL did not have the capacity to have patients unsatisfied with their attachment return to the CWL. However, it was reported that in these cases the coordinator could provide support to patients and providers to help improve their communication and relationship.
Intended impacts
Stakeholders identified intended impacts linked with the outcome area of the CWLs. Every CWL had the intended impact of having more patients attached to a primary care provider. Some provinces had the supplemental aim of attaching patients within a recommended wait time (MB, ON and QC) and used the average wait time as an indicator of performance. Stakeholders in MB and QC envisioned the CWL becoming the main way to meet ongoing demand for attachment to a primary care provider.
To monitor CWLs, provinces produced weekly (PEI), monthly (BC, MB, ON, NB and NS) or quarterly (QC) reports of CWL activities. Provinces used different indicators to monitor their CWLs. For example, QC monitored information such as wait times, number of patients registered, number of patients still waiting on the list, number of vulnerable and non-vulnerable patients, while ON used information such as patients' registration date, age and distance from the assigned provider as well as the number of complex and vulnerable patients. Some provinces also used this information to identify areas with specific resource needs (MB and NS) or provider availability to attach new patients (NB). ON and NS reported the proportion of patients attached through their CWL on a public website. According to the performance data reported by stakeholders, CWL performance appeared to vary widely across provinces as well as across regions within provinces. In MB, it was reported that the CWL reliably attached over 80% of unattached patients to a provider within 30 days; in PEI, typical wait times were 6–8 months in rural areas and 2–5 years in urban areas. QC reported that target wait times for each category of priority were not being reached, and 350,000 patients remained on the CWL, waiting for attachment.
Contextual factors
Most provinces had multiple paths for patient attachment; CWLs were not the sole point of entry. Stakeholders noted that providers' decision to use the CWL may be influenced by considerations of financial gain, workload, and the credibility and reputation of the CWL. For example, some stakeholders mentioned that certain providers avoid the CWL because the patients on the CWL are thought to be more complex; in contrast, other stakeholders noted that personalized contact with care connectors increased providers' trust in the CWL in knowing that the patients they would attach would not all be inordinately complex.
In five provinces (MB, ON, QC, NB and NS), stakeholders reported that provincial policies had influenced providers' use of CWL for the attachment of patients. Reforms in MB, QC and NB notably included targets of attached patients for certain providers or team practices. For example, in QC, FPs received inferior fee-for-service amounts when they had fewer than 500 attached patients and received the regular amount when this target number of attached patients was reached.
It was reported that geographical factors also had influenced the CWLs' effectiveness in increasing attachment to primary care providers. In BC, having developed the CWL in a small division was reported to be a factor that had led to the program's success. However, because the CWL was implemented at the Division of Family Practice level rather than the provincial level, not all divisions in BC had attachment policies. This was reported to be difficult to navigate for patients, as they were often unware of the attachment policies in their division.
Also, the unequal distribution of supply of primary care providers among regions was reported as a key determinant of the success of CWLs. In PEI's urban areas, the low provider-to-population ratio was reported as a factor leading to higher wait times compared to other areas of the province. In MB, the regions that had struggled to meet the target wait time of 30 days were rural or remote communities that lacked local providers able to attach new patients. BC stakeholders also noted that providers whose panels were full were unlikely to use the CWL, even if willing to do so in theory.
Discussion
CWLs are tools readily available in many Canadian provinces that can be used to assist patients in finding a regular primary care provider or to help providers build their patient panels by centralizing the demand in a single-entry point. One major contribution of this paper is the use of logic modelling to describe the different models of CWLs for unattached patients and to identify common issues in the implementation of these CWLs.
Firstly, this approach allowed us to describe the characteristics of each CWL in a form that could easily be compared and contrasted across the seven provinces. This highlighted that while all seven provinces similarly aimed to increase attachment of patients to primary care providers through CWLs, there were large variations in their design.
All provinces, except BC and NS, had a provincially funded CWL to attach patients to FPs as well as, in the majority of the provinces, to NPs. Most were operated at the regional level by care connectors – who were mostly nurses. Incentives were provided for attaching patients from the CWL in QC, NB and PEI, but only to FPs, not NPs. Finally, only two provinces (NB and PEI) required primary care providers to attach patients from the CWL, whereas participation was on a voluntary basis in other provinces. The registration process was fairly similar across provinces. Demographic, contact information and medical information are collected in every province except in MB and NS, which did not systematically collect patients' medical information. All provinces except NB did some form of patient prioritization using either simple criteria (MB, PEI and NS) or assessing for vulnerability (BC, ON and QC). The assessment criteria for prioritization varied from province to province. While all provinces provided some information on existing programs such as walk-in clinics or health information phone lines to meet patients' healthcare needs while waiting on the CWLs, temporary primary care was offered to certain patients on the CWL in some regions of BC and NB.
Secondly, by using logic modelling, we were able to summarize the characteristics of each province's CWL in a way that allowed us to both validate our understanding of the CWL with stakeholders and to engage stakeholders from different provinces in an exchange about the common challenges they face. Three main common challenges were identified by stakeholders: (1) shortage of capacity in primary care; (2) issue of attaching complex or vulnerable patients; and (3) the non-standardized approach to evaluating the effectiveness of CWLs.
Capacity shortage in terms of providers to meet the demand for attachment was identified as a major issue. In a simple manner, CWLs were implemented to address the large demand from patients to be attached to a primary care provider, but often there was a limited number of providers available to attach new patients. Several stakeholders proposed strategies to address the primary care capacity issue such as increasing the possibilities of attaching patients with NPs or investing resources in interdisciplinary primary healthcare teams. BC, MB, ON, QC and NS had implemented team practices where patients had access to various types of primary healthcare providers such as nurses, social workers and dietitians within the practice. In addition, in QC and NS, team-based practices received additional professional resources, namely more nurses, when reaching a target number of patients attached to the team's FPs. Although this was proposed by stakeholders as a strategy to address the capacity shortage, there is little evidence in the literature that supports team-based approaches as a way to increase attachment (Muldoon et al. 2012).
The attachment of patients with certain complex conditions, such as substance abuse, mental health issues and multiple chronic diseases, was described as challenging across provinces. According to several stakeholders, providers may be demotivated from attaching patients from CWLs if they lack information about patients' conditions as they may fear unknowingly attaching very complex and time-consuming patients. Conversely, when providers are aware of patients' conditions, a form of cherry-picking or creaming may occur as shown by a recent study conducted in QC that found patients with certain conditions such as mental health problems waited longer to be attached through CWLs (Smithman et al. 2017). As previously mentioned, two provinces (NB and BC) provided temporary care to patients while they waited for attachment. In BC, this strategy helped to stabilize vulnerable patients and was reported to be a facilitating factor for the attachment of vulnerable patients as they had a more stable condition and it was therefore easier to find a provider willing to attach them.
A third challenge lays in the lack of a common framework to evaluate the effectiveness of CWLs, their inputs and strategies, structures and processes, on the intended impacts (i.e., attaching patients to primary care providers and increasing access). Although all the provinces implemented CWLs to address the same objective, namely patients' need for attachment to a primary care provider, every province implemented a different model of CWL. Our findings show, although different in design, CWLs share similar challenges. An important observation from this study is that there has been little learning between provinces, in part, due to the fact that most CWLs were developed independently and that no common framework or methods were used to evaluate the intended impact of CWLs. The lack of a common or standardized approach makes it difficult to measure and compare the effectiveness of the different CWLs as provinces do not monitor and report the same indicators (e.g., not all provinces monitored and reported wait times for attachment) and similar indicators are often measured differently.
In summary, this study was the first of a three-step logic analysis. This article highlighted key components of CWLs across seven Canadian provinces. The study was conducted in collaboration with stakeholders in each province to address a concern for the large number of unattached patients. One limitation is the small number of stakeholders who participated in some provinces; however, we note that all key stakeholders identified as having in-depth knowledge of the CWL's design in each province were recruited and participated in this study. Also, in order to support the validity of our findings in the context of limited participation, we used grey literature from every province and we validated our findings with stakeholders. A second limitation is that we did not solicit the perspectives of patients (e.g., those attached, or waiting to be attached, through CWLs) as the focus was to describe the design of the CWL; future evaluation of CWLs' effectiveness should include patients. Finally, an important limitation is that this study only aimed to describe CWLs' design and implementation challenges; data collection on the actual impacts of these models will be a crucial component of future research.
Conclusion
CWLs are widely used in many fields of healthcare to better coordinate the demand and supply of care. To our knowledge, CWLs to attach patients to primary care providers have only been implemented in Canada. The findings of our study showed that CWLs have been implemented in seven Canadian provinces to attach patients to a primary care provider, with large variations in the design of CWLs between provinces. Comparing logic models of these CWLs allowed us to compare their design and helped us identify common challenges in their implementation. Although contextual factors may have influenced the design of CWLs in each province, engaging stakeholders in sharing experiences may foster cross-jurisdictional learning and may help more newly implemented CWLs avoid facing the same challenges.
Acknowledgements
This study was approved by the Centre de recherche – Centre Hospitalier de l'Université de Sherbrooke, University of British Columbia Behavioural Research Ethics Board, Comité d'éthique de la recherche avec les êtres humains de l'Université de Moncton, Health PEI Research Ethics Board, Queen's University Health Sciences and Affiliated Teaching Hospitals Research Ethics Board, University of Manitoba Health Ethics Research Board and the Nova Scotia Health Authority Research Ethics Board.
This study was supported by a grant from the Canadian Institutes of Health Research (CIHR, #360866). The authors are grateful to the Fonds de Recherche du Québec – Santé (FRQS), which funded Mylaine Breton's young researcher fellowship (J2) and Mélanie Ann Smithman's doctoral fellowship; to the Michael Smith Foundation for Health Research, which funded Valorie A. Crooks and Jason Sutherland's Scholar Award; to the CIHR, which funded Damien Contandriopoulos' Canada Research Chair in Policies, Knowledge and Health (Pocosa / Politiques, Connaissances, Santé) and Valorie A. Crooks' Canada Research Chair in Health Service Geographies; to Research Manitoba for the funding of Sara Kreindler's Chair in Health System Innovation and Community Health Sciences; as well as to the Clinical Teachers' Association of Queen's University for the funding of Michael Green's Chair in Applied Health Economics/Health Policy. We would also like to thank other research team colleagues Audrey Vandesrasier and Eliot Frymire who were of great help at different stages of this research. Finally, we want to thank all the stakeholders involved in the research project: Marilyn Barrett, Katrina Bepple, Serge Dulude, Phil Graham, Yves-Alain Hémon, Andrew Posen, Michelle Turnbulland and Richard Yampolsky.
Contributor Information
Mylaine Breton, Associate Professor, Department of Community Health Sciences, Université, de Sherbrooke, Chairwoman, Canadian Research Chair in Clinical Governance on Primary Health Care, Longueuil, QC.
Sabrina T. Wong, Professor, School of Nursing and Centre for Health Services and Policy Research, University of British Columbia, Co-Director, BC Primary Care Sentinel Surveillance Network, Vancouver, BC.
Mélanie Ann Smithman, Doctoral Student, Université, de Sherbrooke, Longueuil, QC.
Sara Kreindler, Assistant Professor, Department of Community Health Sciences, University of Manitoba, Manitoba Research Chair in Health System Innovation and Community Health Sciences, Winnipeg, MB.
Jalila Jbilou, Professor and Researcher, Centre de formation médicale, du Nouveau-Brunswick and École de psychologie, Université, de Moncton, Moncton, NB.
Jason Sutherland, Associate Professor, Centre for Health Services and Policy Research, University of British Columbia, Scholar, Michael Smith Foundation for Health Research, Vancouver, BC.
Astrid Brousselle, Director and Professor, School of Public Administration, University of Victoria, Victoria, BC.
Jay Shaw, Scientist, Institute for Health System Solutions and Virtual Care, Women's College Research Institute, Women's College Hospital, Assistant Professor, Institute of Health Policy, Management and Evaluation, University of Toronto, Toronto, ON.
Valorie A. Crooks, Professor, Department of Geography, Simon Fraser University, Scholar, Michael Smith Foundation for Health Research, Canada Research Chair in Health Service Geographies, Burnaby, BC.
Damien Contandriopoulos, Professor, School of Nursing, University of Victoria, Chairman, Research Chair Policies, Knowledge and Health (Pocosa/Politiques, Connaissances, Santé), Victoria, BC.
Martin Sasseville, Research professional, Centre de recherche –, Hôpital Charles-Le Moyne –, Université, de Sherbrooke, Longueuil, QC.
Michael Green, Associate Professor, Departments of Family Medicine and Public Health Sciences, Queen's University, CTAQ Chair in Applied Health Economics/Health Policy, Director, Centre for Health Services and Policy Research, Associate Director, Centre for Studies in Primary Care, Adjunct Scientist, Institute for Clinical Evaluative Sciences, Kingston, ON.
References
- Bayliss E.A., Edwards A.E., Steiner J.F., Main D.S. 2008. “Processes of Care Desired by Elderly Patients with Multimorbidities.” Journal of Family Practice 25(4): 287–93. 10.1093/fampra/cmn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breton M., Brousselle A., Boivin A., Roberge D., Pineault R., Berbiche D. 2015. “Who Gets a Family Physician through Centralized Waiting Lists?” BMC Family Practice 16(1): 10. 10.1186/s12875-014-0220-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breton M., Green M., Kreindler S., Sutherland J., Jbilou J., Wong S.T. et al. 2017. “A Comparative Analysis of Centralized Waiting Lists for Patients without a Primary Care Provider Implemented in Six Canadian Provinces: Study Protocol.” BMC Health Services Research 17(1): 60. 10.1186/s12913-017-2007-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brousselle A., Champagne F. 2011. “Program Theory Evaluation: Logic Analysis.” Evaluation and Program Planning 34: 69–78. [DOI] [PubMed] [Google Scholar]
- Burge F., Lawson B., Johnston G. 2003. “Family Physician Continuity of Care and Emergency Department Use in End-of-Life Cancer Care.” Medical Care 41(8): 992–1001. [DOI] [PubMed] [Google Scholar]
- Commissaire à la santé et au bien être. 2014. “Perception et expériences de la population : le Québec comparé – résultats de l'enquête internationale sur les politiques de santé du Commonwealth Fund.” Retrieved May 15, 2017. <http://www.csbe.gouv.qc.ca/fileadmin/www/2013/CWF/CSBE_Rapport_Commonwealth_Fund_2013.pdf>.
- Dew K., Cumming J., McLeod D., Morgan S., McKinlay E., Dowell A., Love T. 2005. “Explicit Rationing of Elective Services: Implementing the New Zealand Reforms.” Health Policy 74(1): 1–12. [DOI] [PubMed] [Google Scholar]
- Fung C.S., Wong C.K., Fong D.Y., Lee A., Lam C.L. 2015. “Having a Family Doctor Was Associated with Lower Utilization of Hospital-Based Health Services.” BMC Health Services Research 15(1): 42. 10.1186/s12913-015-0705-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- General Practice Services Committee. 2015. “Innovations – A GP for Me.” Retrieved March 26, 2018. <http://www.gpscbc.ca/what-we-do/innovations/a-gp-for-me>.
- Godin K., Stapleton J., Kirkpatrick S.I., Hanning R.M., Leatherdale S.T. 2015. “Applying Systematic Review Search Methods to the Grey Literature: A Case Study Examining Guidelines for School-Based Breakfast Programs in Canada.” Systematic Reviews 4(1): 138. 10.1186/s13643-015-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin S.J., Kinmonth A.-L., Veltman M.W.M., Gillard S., Grant J., Stewart M. 2004. “Effect on Health-Related Outcomes of Interventions to Alter the Interaction between Patients and Practitioners: A Systematic Review of Trials.” Annals of Family Medicine 2(6): 595–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunfeld E., Levine M.N., Julian J.A., Coyle D., Szechtman B., Mirsky D. et al. 2006. “Randomized Trial of Long-Term Follow-Up for Early-Stage Breast Cancer: A Comparison of Family Physician Versus Specialist Care.” Journal of Clinical Oncology 24(6): 848–55. [DOI] [PubMed] [Google Scholar]
- Haggerty J., Tamblyn R., Boileau L., Levesque J., Katz A., Russell G. 2014. “Building Systems-Level Evidence from the Mosaic of 12 Research Programs in the CIHR Signature Initiative on Community Based Primary Health Care.” Paper presented at the Canadian Association of Health Services and Policy Research Conference, Montreal, QC. [Google Scholar]
- Laperrière A. 1997. “Les critères de scientificité des méthodes qualitatives.” In Poupart J., Deslauriers J.-P., Groulx L.-H., Laperrière A., Mayer R., Pires A.P. (Eds.), La recherche qualitative : enjeux épistémologiques et méthodologiques (pp. 365–89). Montréal, QC: Gaëtan Morin Éditeur. [Google Scholar]
- Mays N., Pope C. 1995. “Rigour and Qualitative Research.” BMJ 311(6997): 109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell P., Lewis V. 2003. “A Manual to Guide the Development of Local Evaluation Plans.” Retrieved March 26, 2018. <https://yeah.org.au/wp-content/uploads/2014/07/evaluationplanmanual.pdf>.
- Muldoon L., Dahrouge S., Russell G., Hogg W., Ward N. 2012. “How Many Patients Should a Family Physician Have? Factors to Consider in Answering a Deceptively Simple Question.” Healthcare Policy 7(4): 26. [PMC free article] [PubMed] [Google Scholar]
- Noseworthy T.W., McGurran J.J., Hadorn D.C. 2003. “Waiting for Scheduled Services in Canada: Development of Priority-Setting Scoring Systems.” Journal of Evaluation in Clinical Practice 9(1): 23–31. 10.1046/j.1365-2753.2003.00377.x. [DOI] [PubMed] [Google Scholar]
- Oates J., Weston W.W., Jordan J. 2000. “The Impact of Patient-Centered Care on Outcomes.” Journal of Family Practice 49(9): 796–804. [PubMed] [Google Scholar]
- Østbye T., Yarnall K.S.H., Krause K.M., Pollak K.I., Gradison M., Michener J.L. 2005. “Is There Time for Management of Patients with Chronic Diseases in Primary Care?” Annals of Family Medicine 3(3): 209–14. 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudoler D., Deber R., Barnsley J., Glazier R.H., Dass A.R., Laporte A. 2015a. “Paying for Primary Care: The Factors Associated with Physician Self-Selection into Payment Models.” Health Economics 24(9): 1229–42. 10.1002/hec.3221. [DOI] [PubMed] [Google Scholar]
- Rudoler D., Laporte A., Barnsley J., Glazier R.H., Deber R.B. 2015b. “Paying for Primary Care: A Cross-Sectional Analysis of Cost and Morbidity Distributions across Primary Care Payment Models in Ontario Canada.” Social Science and Medicine 124: 18–28. 10.1016/j.socscimed.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Schoen C., Osborn R., Doty M.M., Bishop M., Peugh J., Murukutia N. 2007. “Toward Higher-Performance Health Systems: Adults' Health Care Experiences in Seven Countries, 2007.” Health Affairs 26(6): w717–34. 10.1377/hlthaff.26.6.w717. [DOI] [PubMed] [Google Scholar]
- Smithman M.A., Breton M., Berbiche D., Touati N., Loignon C., Côté-Boileau É. et al. 2017. “They Will Get a Family Physician Sooner or Later: Wait Time Inequalities in Centralized Waiting Lists for Unattached Patients.” Paper presented at the North American Primary Care Research Group Annual Meeting, Montreal, QC Retrieved March 26, 2018. <http://www.napcrg.org/Conferences/AnnualMeeting/EducationEvents/SearchEducationalSessions?language=en-US&m=0&s=smithman&p=0>. [Google Scholar]
- Starfield B., Shi L., Macinko J. 2005. “Contribution of Primary Care to Health Systems and Health.” Milbank Quarterly 83(3): 457–502. 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


