Abstract
Background
Medical professionals should be appropriately trained in the field of smoking cessation counseling and be familiar with related tobacco-control issues. Sadly, Canadian medical students receive little education regarding smoking cessation.
Methods
University of Ottawa medical students created Students Working Against Tobacco (SWAT), a program that provides its members with tobacco education and opportunities to discuss tobacco use, smoking prevention and cessation with elementary-school students. Surveys assessing student knowledge and confidence in addressing tobacco issues were administered to the participating students at the start of the program and following their delivery of a school presentation.
Results
Students initially lacked knowledge, skills and experience in addressing tobacco issues and discussing smoking prevention and cessation counselling. Following their involvement in the SWAT program, students’ smoking cessation counselling knowledge and skills improved, and they expressed confidence in becoming more engaged in this important preventive health issue.
Conclusion
Until smoking cessation is incorporated into undergraduate medical education programs, gaps will remain in the preparation of tomorrow’s physicians regarding the provision of effective smoking cessation counselling and their broader understanding of this important health issue. Currently, there are constraints limiting the number of medical undergraduates that SWAT is able to involve and influence.
Introduction
Smoking is the leading cause of preventable disease, disability and death worldwide. If smoking rates do not significantly decline, almost 1 billion deaths secondary to tobacco use will have occurred by the end of the 21st century.1
Currently 18% of Canadians smoke,2,3 with the majority beginning in their youth.4,5 Among adolescents, 24% have tried a cigarette, 28% have tried a tobacco product and 4% are current smokers.5 There is no national Canadian data describing the use of e-cigarettes by youth, but 10% of grade 9 students in a representative cohort have tried electronic cigarettes.6
A large number of smokers attempt cessation each year, but only 5% are successful.7 With the provision of brief advice, healthcare workers can have a positive impact on smoking cessation;8-10 with specific assistance and appropriate support, physicians can obtain higher cessation rates.11 It is important, therefore, that physicians are appropriately trained to promote smoking cessation.4,9,10,12,13
Unfortunately, Canadian medical students receive little education regarding smoking cessation.9,14,15 An assessment of 11 of the 17 Canadian medical schools revealed that 64% of those schools provide less than three hours of smoking cessation education, 64% do not examine their students on smoking cessation and 73% do not provide an opportunity to rehearse cessation counselling skills.14 This lack of training is reflected in the attitudes of graduating medical students from one university: only half of them felt capable of counselling and treating patients for smoking cessation. Surprisingly, one-third did not view smoking cessation as being a healthcare priority.15 Multiple studies have demonstrated the positive association between decreased physician knowledge about tobacco cessation and likelihood of addressing the smoking behaviour of their patients.4,10,12,16
At the time of this study, the University of Ottawa, medical students received only a two-hour lecture on smoking and tobacco products as part of a course addressing psycho-social issues in medicine. To address this shortcoming, medical students created an interest group: Students Working Against Tobacco (SWAT). The goals of the organization are to improve future physicians’ tobacco education and counselling skills while familiarizing them with the importance of addressing Canada’s leading cause of preventable disease, disability and death.
Herein, we describe the possible effect of an extracurricular anti-tobacco advocacy and education program on the knowledge of medical students regarding tobacco and health, their comfort in addressing smoking cessation, and the acquisition of counselling skills.
Methods
Learning opportunities for medical students through SWAT
During the academic year, SWAT student-leaders organize frequent, relevant, presentations by health care professionals familiar with tobacco control and smoking cessation issues. Topics include: nicotine addiction; the nature of tobacco products including e-cigarettes and shisha; socio-economic correlates of smoking behaviour; co-existing substance use; patient perspectives on cessation; cessation techniques and programs; smoking cessation advocacy; and, community cessation resources. Each talk is delivered during a lunch hour period and provides students with knowledge not currently provided in any part of the University of Ottawa medical school curriculum. In the 2015-16 year, 140 students joined SWAT and an average of 19 students attended each of the seven talks. Membership in SWAT was similar to that of most other special interest groups in the University of Ottawa Faculty of Medicine.
An important component of the program is the opportunity for medical students to deliver tobacco presentations in local elementary schools. Each year, SWAT leaders contact Ottawa schools, offering the presentations to supplement the schools’ health curriculum. Additionally, SWAT leaders prepare and provide an annotated slide set and a mandatory training session to SWAT members prior to school visits. The training session includes detailed explanations of the presentation material as well as tips on engaging children. The presentation addresses the design and composition of a cigarette, the health impacts of smoking, the financial costs of tobacco addiction, e-cigarettes, the stigma and psychological impact of smoking behaviour, and the marketing strategies used by tobacco companies.
Evaluation of the SWAT program
In the 2015-2016 school year, SWAT members completed a self-assessment survey at the start of their training session and, ultimately, following the completion of a school presentation. The initial survey evaluated the students’ baseline tobacco cessation knowledge and counselling skills. The survey was repeated to evaluate any subsequent changes in knowledge and skills. The primary objective was to assess the SWAT program’s effectiveness in developing medical students’ clinical counselling and teaching skills and their comfort level in addressing smoking cessation and prevention. The survey also assessed students’ attitudes regarding the role of health care professionals in assisting with cessation.
The survey consisted of 24 questions and was based on questionnaires used in recent studies examining health care professionals’ tobacco use and cessation practices.17-19 The size of our sample did not permit inferential statistical analysis; our results are descriptive only. No incentive was offered for completing the survey.
Results
In the past 5 years, 53 pre-clerkship medical students have given presentations to 38 classes of children in grades 4-10, in both French and English. During the 2015-16 academic year, 13 pre-clerkship medical students underwent training; six medical students delivered four presentations.
Participants
The characteristics of the participating medical students are displayed in Table 1. Only one student had ever smoked or was smoking at the time. All six students who completed a school presentation were female and in their second year of medical school. Five of the six students completed the post-presentation survey.
Table 1.
Demographic characteristics of SWAT training session participants
| Number/Total | |
|---|---|
| Gender | |
| Male | 4/13 |
| Female | 9/13 |
| Medical School Year | |
| Year 1 | 4/13 |
| Year 2 | 9/13 |
| Smoker (Current or Ever) | 1/13 |
Students’ Baseline
Prior to training, all 13 SWAT members stated they had either no experience (4/13) or were somewhat experienced (9/13) in educating others about tobacco (Figure 1). Almost half were not at all comfortable or somewhat comfortable advising patients about smoking cessation and teaching youth about tobacco (6/13, Figure 2).
Figure 1.

University of Ottawa SWAT members’ pre-training (top) and post-presentation (bottom) amount of experience with public tobacco education
Figure 2.

University of Ottawa medical students’ pre-training (A) and post-presentation (B) comfort level with discussing smoking cessation
Students were asked about their skill set regarding smoking cessation counselling. The results are summarized in Figure 3. The majority of students reported having no skills or being only somewhat skilled in: counselling a child or adolescent regarding smoking prevention (10/13); asking about smoking at every patient interaction (6/13); advising all smokers to quit (9/13); assessing patient willingness to quit (10/13); assisting a patient with a quit plan (12/13); arranging follow-up (9/13); and, recommending nicotine replacement therapy (11/13).
Figure 3.

University of Ottawa medical students’ pre-training (A) and post-presentation (B) smoking cessation and prevention skills
A summary of the perceived effectiveness of commonly used approaches to youth tobacco prevention is provided in Figure 4. All students considered the approaches as somewhat, moderately or very effective, with the exception of two students who believed discussing tobacco company marketing strategies as not at all effective.
Figure 4.
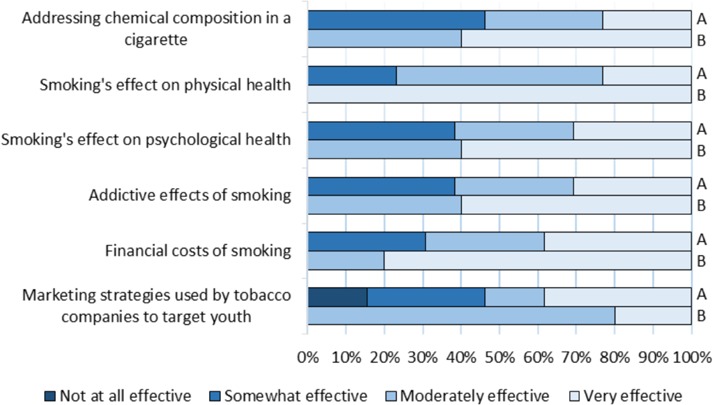
University of Ottawa medical students’ pre-training (A) and post-presentation (B) opinion on effective strategies for youth tobacco prevention and cessation
When asked whether they agreed with various belief statements regarding the role of the health care provider in patient smoking cessation, many students reported that they disagreed or felt neutral that healthcare workers: can increase a patient’s chance of quitting (6/13); should routinely ask patients about tobacco use (2/13); should routinely help patients to quit using tobacco (2/13); and, should set a good example by not using tobacco (4/13) (Figure 5).
Figure 5.

University of Ottawa medical students’ pre-training (A) and post-presentation (B) attitudes on patient smoking cessation
Students’ improvement
Following the completion of a school presentation, students’ comfort and skills regarding smoking cessation improved. They felt moderately experienced in public tobacco education (3/5), very comfortable teaching youth about the topic (4/5) and very comfortable advising patients (2/5) (Figures 1, 2). Students reported substantial improvement in terms of their smoking cessation and prevention counselling abilities (Figure 3). All students agreed the commonly used tobacco prevention and cessation strategies were moderately or very effective (Figure 4).
A change in the student perception of the role of a physician in smoking cessation also occurred; all students agreed or strongly agreed that a healthcare worker plays an important role in the identification, assessment, and treatment of smokers. One student remained neutral on whether patients want healthcare providers to recommend quitting (Figure 5).
Discussion
It has already been noted that a significant proportion of graduating Canadian medical students from one university felt they had not received enough education in smoking cessation.15 Although there were few participants, our results may indicate University of Ottawa pre-clerkship medical students may lack knowledge, skills, and experience in smoking cessation counselling. Astonishingly, many were skeptical about the role of a physician in helping patients to quit despite abundant evidence that suggests otherwise.8-11 Furthermore, students were unaware of evidence-based approaches to smoking prevention, with some skeptical that industry denormalization is influential, when in fact, it has demonstrated significant effectiveness in addressing and preventing tobacco use among youth.20
SWAT was originally created to increase student exposure and education in tobacco cessation. The development of SWAT has augmented learning and led to greater engagement in addressing this important healthcare issue. Self-assessments were the fundamental tool employed in our study. They have been identified as a reliable method in evaluating competence and are seen as possessing utility in the assessment of educational programs.21 Unfortunately, the small number of participants in the cohort study negated the possibility of statistical analysis to more accurately demonstrate the impact of the SWAT program. Further and more rigorous research is needed.
Conclusion
The importance of smoking cessation training should be reflected in the Canadian medical schools’ curricula. Sadly, the dangers of tobacco and the approaches to cessation appear to be unacknowledged in medical education. That such matters are seemingly absent is ironic given the human and financial costs incurred as a direct consequence of tobacco addiction. Smokers lose a decade of life expectancy from nicotine addiction and smoking cessation is the most important of all preventive initiatives.22
Building on their experience, SWAT leaders at the University of Ottawa have worked with leading Canadian experts to create an evidence-based clinical skills development tutorial on smoking cessation for medical students. A trial of this initiative was recently concluded. It is hoped that it will be incorporated into the medical curriculum in the near future. The magnitude of the global tobacco epidemic and the stated desire to reduce smoking in Canada to “less than 5% by 2035” require that tomorrow’s medical practitioners are able to assist with smoking cessation.23
Footnotes
Conflicts of interest: There are no conflicts of interest for any of the authors.
References
- 1.Eriksen M, Mackay J, Schluger N, Gomeshtapeh FI, Drope J. The Tobacco Atlas. 5th ed. Atlanta, United States of America: American Cancer Society, Inc., 2015:14-25. [Google Scholar]
- 2.Allin S, Veillard J, Wang L, Grignon M. How Can Health System Efficiency Be Improved in Canada? Healthcare Policy. 2015;11(1):33–45. [PMC free article] [PubMed] [Google Scholar]
- 3.Smokers, by sex, provinces and territories. Statistics Canada, 2014. [Internet]. Available at: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/health74b-eng.htm [Accessed July 10, 2016].
- 4.Pbert L, Farber H, Horn K, Lando HA, Muramoto M. State-of-the-Art Office-Based Interventions to Eliminate Youth Tobacco Use: The Past Decade. Pediatrics. 2015;135(4):734-47. [DOI] [PubMed] [Google Scholar]
- 5.Youth Smoking Survey Health Canada, 2012-2013 [Internet]. Available at: http://healthycanadians.gc.ca/publications/healthy-living-vie-saine/youth-smoking-survey-tables-2012-2013-tableaux-enquete-jeunes-tabagisme/index-eng.php [Accessed July 10, 2016].
- 6.Khoury M, Manlhiot C, Fan C-PS, et al. Reported electronic cigarette use among adolescents in the Niagara region of Ontario. CMAJ. 2016;188(11):794-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaiton M, Diemert L, Cohen JE, et al. Estimating the number of quit attempts it takes to quit smoking successfully in a longitudinal cohort of smokers. BMJ. 2016;6:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stead L, Buitrago D, Preciado N, Sanchez G, Lancaster T. Physician advice for smoking cessation (Review). Cochrane Database Syst Rev. 2013;(5):1-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vogt F, Hall S, Marteau TM. General practitioners’ and family physicians’ negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction. 2005;100:1423–31. [DOI] [PubMed] [Google Scholar]
- 10.Carson KV, Verbiest MEA, Crone MR, et al. Training health professionals in smoking cessation (Review). Cochrane Database Syst Rev. 2012;(5):1-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pisinger C, Vestbo J, Borch-Johnsen K, Jørgensen T. It is possible to help smokers in early motivational stages to quit. The Inter99 study. Prev Med. 2005;40(3):278–84. [DOI] [PubMed] [Google Scholar]
- 12.Toll BA, Rojewski AM, Duncan L, et al. “Quitting Smoking Will Benefit Your Health”: The Evolution of Clinician Messaging to Encourage Tobacco Cessation. Clin Cancer Res. 2015;20(2):301–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warren GW, Marshall JR, Cummings KM, et al. Practice Patterns and Perceptions of Thoracic Oncology Providers on Tobacco Use and Cessation in Cancer Patients. J Thorac Oncol. 2014;8(5):543–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loranger M, Simms K, Pipe A. Smoking cessation counselling training in the pre-clerkship curriculum of Canadian medical school: A national survey. CMEJ. 2018;9(2):7-12. [PMC free article] [PubMed] [Google Scholar]
- 15.Vanderhoek AJ, Hammal F, Chappell A, Wild TC, Raupach T, Finegan BA. Future physicians and tobacco: an online survey of the habits, beliefs and knowledge base of medical students at a Canadian University. Tob Induc Dis. 2013;11(9):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorzkowski JA, Whitmore RM, Kaseeska KR, Brishke JK, Klein JD. Pediatrician Knowledge, Attitudes, and Practice Related to Electronic Cigarettes. J Adolesc Heal. 2016;59(1):81–6. [DOI] [PubMed] [Google Scholar]
- 17.Prucha MG, Fisher SG, McIntosh S, et al. Health Care Workers’ Knowledge, Attitudes and Practices on Tobacco Use in Economically Disadvantaged Dominican Republic Communities. Int J Environ Res Public Health. 2015;12(4):4060–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geller AC, Brooks DR, Powers CA, et al. Tobacco cessation and prevention practices reported by second and fourth year students at US medical schools. J Gen Intern Med. 2008;23(7):1071–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou S, Van Devanter N, Fenstermaker M, Cawkwell P, Sherman S, Weitzman M. A Study of the Use, Knowledge, and Beliefs About Cigarettes and Alternative Tobacco Products Among Students at One U.S. Medical School. Acad Med. 2015;90(12):1713–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borland T, Schwartz R. The Next Stage: Delivering Tobacco Prevention and Cessation Knowledge through Public Health Networks. Ontario Tobacco Research Unit, 2010. [Google Scholar]
- 21.D’Eon MF, Trinder K. Evidence fr the validity of grouped self-assessments in measuring the outcomes of educational programs. Eval Health Prof. 2014;37(4):457-69. [DOI] [PubMed] [Google Scholar]
- 22.Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341-50. [DOI] [PubMed] [Google Scholar]
- 23.A Tobacco Endgame for Canada. Kingston, Ontario: Queen’s University Endgame Summit Background paper, 2016. [Internet]. Available at: http://www.queensu.ca/gazette/sites/default/files/assets/attachments/EndgameSummit-Backgroundpaper%20.pdf [Accessed November 27, 2017]. [Google Scholar]


