To the Editor
The disease course of acute pancreatitis (AP) is not well defined with most studies focusing on mortality.1,2 Improved ICU care and aggressive management have improved mortality rates,3 potentially increasing the risk for recurrent and chronic pancreatitis.4 Detailed information of the natural disease course is important to treat patients before these irreversible damage occurs. The recent development of the Pancreatitis Activity Scoring System (PASS) can assess disease activity at any given time during an episode of AP,5 and its individual components give more information beyond mortality.
The objective of this study was to evaluate the variations of AP disease course based on etiology using the newly described PASS.
METHODS
A retrospective review of patients from January 2014 to December 2014 at Cedars-Sinai Medical Center (approved by the Institutional Review Board, IRB #38294) was performed using discharge diagnosis International Classification and Diagnosis (ICD-9) code 577.0. Manual chart review confirmed patients met criteria for AP.7 Transfers from outside hospitals were excluded.
Pancreatitis Activity Scoring System and its individual components were modeled using a Generalized Linear Mixed Model (GLMM).
RESULTS
One hundred seventy five patients qualified for this study: 30 (17%) alcohol, 64 (37%) gallstones, 81 (46%) idiopathic. The median baseline PASS for alcohol, gallstones, and idiopathic were 237.5, 160, and 215, respectively; the median discharge PASS for the three groups were 90, 65.6, and 80 (Table 1).
TABLE 1.
Demographic Data for the Different Etiologies of AP
| Alcohol (n = 30) | Gallstone (n = 64) | Idiopathic (n = 81) | |
|---|---|---|---|
| Age, median (IQR), y | 42 (30-56) | 57 (42-76) | 58 (38-68) |
| Sex, female, n (%) | 8 (27) | 42 (66) | 46 (57) |
| Length of stay, median (IQR), d | 3 (3-5) | 4 (3-5) | 4 (2-6) |
| BMI on admission, median (IQR), kg/m2 | 23.8 (21.6-28.3) | 28.3 (25.1-32.9) | 24.8 (20.3-29.6) |
| Readmission within 60 days, n (%) | 1 (3) | 2 (3) | 3 (4) |
| ICU admission during hospital stay, n (%) | 6 (20) | 5 (8) | 4 (5) |
| Baseline PASS, median (IQR) | 237.5 (148.8-266.3) | 160 (125-220) | 215 (145-295) |
| Discharge PASS, median (IQR) | 90 (52.5-123.1) | 65.6 (38.1-100.6) | 80 (45-125) |
IQR indicates interquartile range; BMI, body mass index.
Organ failure, change in morphine usage, and ability to tolerate solid diet were similar among the three groups. The alcoholic group had a higher average abdominal pain score compared to the gallstone and idiopathic groups (P < 0.0067, P < 0.0003) for patients with length of stay of 5 days.
For patients with length of stay of 3 and 5 days, the alcoholic group had a larger baseline SIRS compared to the gallstone group (P < 0.0104, P < 0.0134, respectively) (Fig. 1). The alcoholic group also had a larger baseline SIRS compared to the idiopathic group for patients with length of stay of 5 days (P < 0.0086). The SIRS at day 5 for patients with length of stay of 5 days was higher in the alcoholic group compared to the gallstone group (P < 0.0071) and the idiopathic group (P < 0.0029).
FIGURE 1.
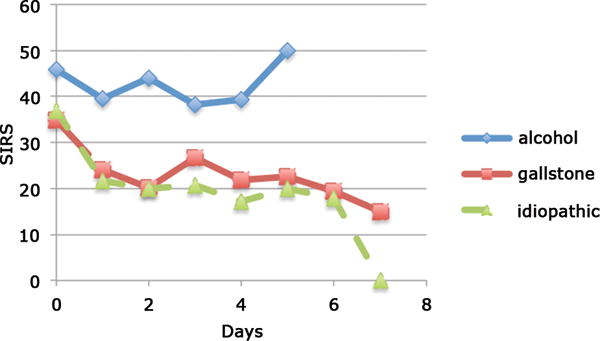
Weighted SIRS component for the different etiologies. Weighted scale is number of SIRS Criteria × 25.
DISCUSSION
This study describes in detail, the disease course of AP stratified by etiology using the recently validated PASS. We found patients with alcoholic pancreatitis had a higher baseline and discharge PASS; alcoholic pancreatitis had a higher level of baseline and discharge SIRS; and higher abdominal pain score for patients with higher length of stays. The SIRS trend was also interesting; while both gallstone and idiopathic groups showed improvement throughout, the alcohol group showed minimal improvement, and worsened after day 4. Alcoholic pancreatitis is thought to have a more severe form of AP and increased risk for recurrent acute pancreatitis and chronic pancreatitis,7 which can potentially be explained by the diffuse negative effects of alcohol throughout the body.8
The small sample size and the retrospective nature of the study are limitations of this study. Future studies should be performed with larger cohorts in a prospective manner.
Footnotes
There are no financial interests or conflicts to disclose.
References
- 1.Gloor B, Müller CA, Worni M, et al. Late mortality in patients with severe acute pancreatitis. Br J Surg. 2001;88:975–979. doi: 10.1046/j.0007-1323.2001.01813.x. [DOI] [PubMed] [Google Scholar]
- 2.Mofidi R, Duff MD, Wigmore SJ, et al. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br J Surg. 2006;93:738–744. doi: 10.1002/bjs.5290. [DOI] [PubMed] [Google Scholar]
- 3.Mutinga M, Rosenbluth A, Tenner SM, et al. Does mortality occur early or late in acute pancreatitis? Int J Pancreatol. 2000;28:91–95. doi: 10.1385/IJGC:28:2:091. [DOI] [PubMed] [Google Scholar]
- 4.Lew D, Afghani E, Pandol S. Chronic Pancreatitis: Current Status and Challenges for Prevention and Treatment. Dig Dis Sci. 2017;62:1702–1712. doi: 10.1007/s10620-017-4602-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu BU, Batech M, Quezada M, et al. Dynamic measurement of disease activity in acute pancreatitis: the Pancreatitis Activity Scoring System (PASS) Am J Gastroenterol. 2017;112:1144–1152. doi: 10.1038/ajg.2017.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis — 2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 7.Zerem E. Treatment of severe acute pancreatitis and its complications. World J Gastroenterol. 2014;20:13879–138892. doi: 10.3748/wjg.v20.i38.13879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burnham EL, Moss M, Martin GS. The Effect of Alcohol Consumption on Risk for Sepsis and ARDS. In: Vincent JL, editor. Intensive Care Medicine. New York, NY: Springer; 2003. [Google Scholar]


