Abstract
Background
Functional performance tests are commonly utilized in screening for injury prevention, evaluating for athletic injuries, and making return-to-play decisions. Two frequently performed functional performance tests are the single leg squat and step-down tests.
Purpose
The purpose of this study was to systematically review the available psychometric evidence for use of the single leg squat and step-down tests for evaluating non-arthritic hip conditions and construct an evidence-based protocol for test administration.
Study Design
Review of the Literature
Materials/Methods
A search of the PubMed and SPORTSDiscus databases was performed. Psychometric evidence of reliability, validity, and responsiveness to support the use of the both tests were collected. The protocols used for administering these tests were extracted, summarized, and combined.
Results
Of the 3,406 articles that were reviewed, 56 total articles met the inclusion criteria and were included in the review. Evidence for reliability and validity was available to support the use of the single leg squat and step-down tests. Both tests assess for neuromuscular control of the hip and surrounding muscular structures. Evaluation of these functional movement patterns enable the clinician to assess for limitations that may cause an increase in hip pain and dysfunction.
Conclusions
The single leg squat and step-down tests can assess for kinematic and biomechanical deficiencies and may be useful in the evaluation process for individuals with non-arthritic hip pain. The authors of this review present a comprehensive evidence-based protocol for standardized performance of these tests.
Level of Evidence
2b
Keywords: Functional performance testing, non-arthritic hip pain, standardized protocol
INTRODUCTION
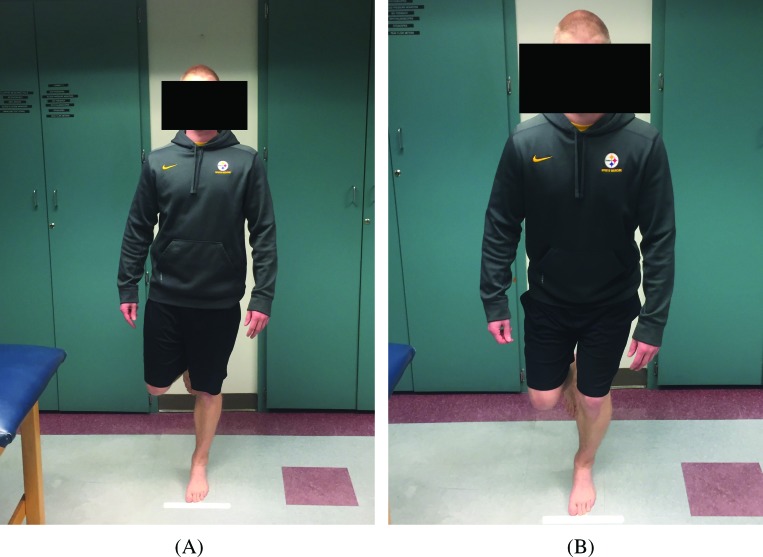
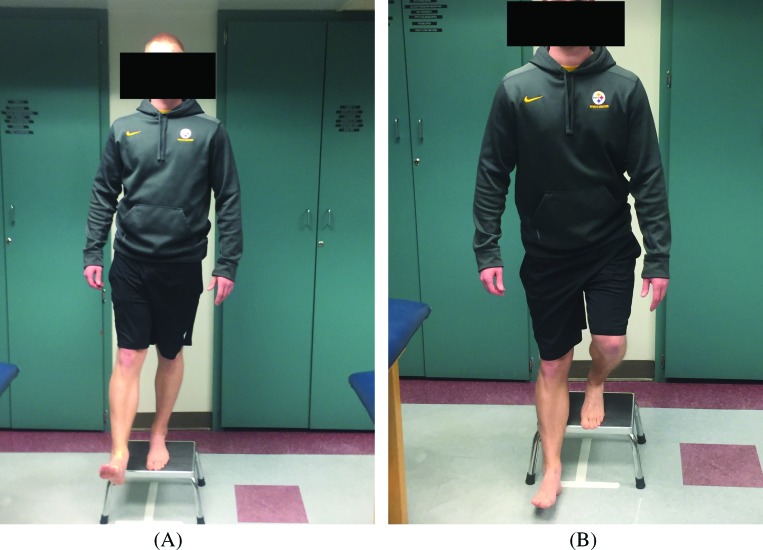
Functional performance tests are used to evaluate basic dynamic movement patterns that are commonly part of more complex activity. Such tests typically combine range of motion, strength, and proprioceptive assessment. They allow for the simultaneous evaluation of movement in all three (frontal, sagittal, and transverse) planes of motion. These functional performance tests can be useful in sports medicine to screen for injury prevention, evaluate athletic injuries, and help in return-to-play decisions.1-3 The single leg squat test (SLST) (Figure 1) and step-down test (SDT) (Figure 2) are two well-known tests described in the published literature and used in clinical practice.4,5 The SLST and SDT have been used in the evaluation of individuals with lower extremity dysfunction, most commonly among patients with knee pathology.6-15 However, these tests also assess for several deviations in hip, pelvis, and trunk performance that are considered important when assessing individuals with hip pain.16,17
Figure 1.
The Single Leg Squat Test. (A) – Initial test position. (B) – Squat position.
Figure 2.
The Step-Down Test. (A) – Initial test position. (B) – Step down position.
The overall movement pattern during descent for both the SLST and SDT include hip and knee flexion with anterior pelvic tilt, flexion at the trunk, and hip adduction with knee internal rotation and abduction.17-19 While these two tests are similar, they have been shown to produce different patterns of movement and stresses at the hip.20,21 Therefore, both the SLST and SDT could potentially be used to assess for kinematic and biomechanical deficiencies and be useful in the evaluation process of individuals with hip-related dysfunction. Static measures of range of motion performed standing or supine may not accurately depict the biomechanical demands of dynamic movements. It is currently unclear how the implementation of the SLST and SDT in clinical evaluation of non-arthritic hip patients is best accomplished, but there is promise regarding the potential of routine addition of these tests for advancing the understanding of non-arthritic hip dysfunction. Additional examination of strength, flexibility, and endurance could be necessary to specifically identify the underlying pathologies, however, the inclusion of the SLST and SDT in clinical practice may be particularly helpful in the examination of patients with non-arthritic sources of hip pain. There is a need for an evidence based standardized protocol for administering the SLST and SDT in individuals with non-arthritic hip pain.
The purpose of this study was to systematically review the literature to identify the psychometric evidence to support the use of and the best methods for administration of SLST and SDT in evaluation of patients with non-arthritic hip pain. The results of this study will allow for the development of a standardized protocol for administering the SLST and SDT in clinical practice and future research studies involving non-arthritic hip conditions.
METHODS
Search Strategy for Identification of Studies
A search of the PubMed and SPORTDiscus databases was performed to include articles from January 1997 to March 2017. Articles were identified that offered psychometric evidence for reliability, validity, and responsiveness regarding the administration of the SLST and SDT for examination of trunk and lower extremity function. The following key words were used in combination for searching the electronic databases: “single leg squat” AND “step down.” The primary author reviewed the abstracts of all references retrieved from the search and duplicates were removed. From this search, full length articles were retrieved and reference lists for these articles were also reviewed for additional relevant articles.
Research articles were included if they met the following criteria: 1) written in English, 2) published in a peer-reviewed journal after 1997, and 3) described the use of the SLST and/or SDT test in evaluation of strength, balance, postural control, or range of motion in the trunk, pelvis, hip, or knee. Studies were excluded if they assessed only the ankle or foot during performance of the tests, or the performance of testing was completed on patients with degenerative disorders (i.e. osteoarthritis).
Data Extraction – Reliability & Validity
Statistical analysis of reliability including test-retest, intra-rater, and inter-rater, and was recorded from each evaluated research article.2,22,23 Reliability was recorded as an interclass correlation coefficient (ICC) for interval or continuous data and the Cohen's Kappa statistic for categorical or nominal data.24-26 Both the ICC and Kappa coefficient are valued on a scale of 0.0 to 1.0, with values closer to 1 showing higher reliability.27 A value for either the ICC or Kappa that is equal to or greater than 0.75 is considered excellent, between 0.40 and 0.74 is considered moderate, and less than 0.40 is considered poor.24
Validity for the SLST and SDT was assessed by comparing the performance of individuals with a documented lower extremity condition to healthy individuals and/or comparing performance on another test that shares similar characteristics with the SLST and SDT.28 This relationship is commonly expressed through correlation coefficients, comparing the performance of each clinical test with other values, such as muscle strength and lower extremity range of motion.
RESULTS
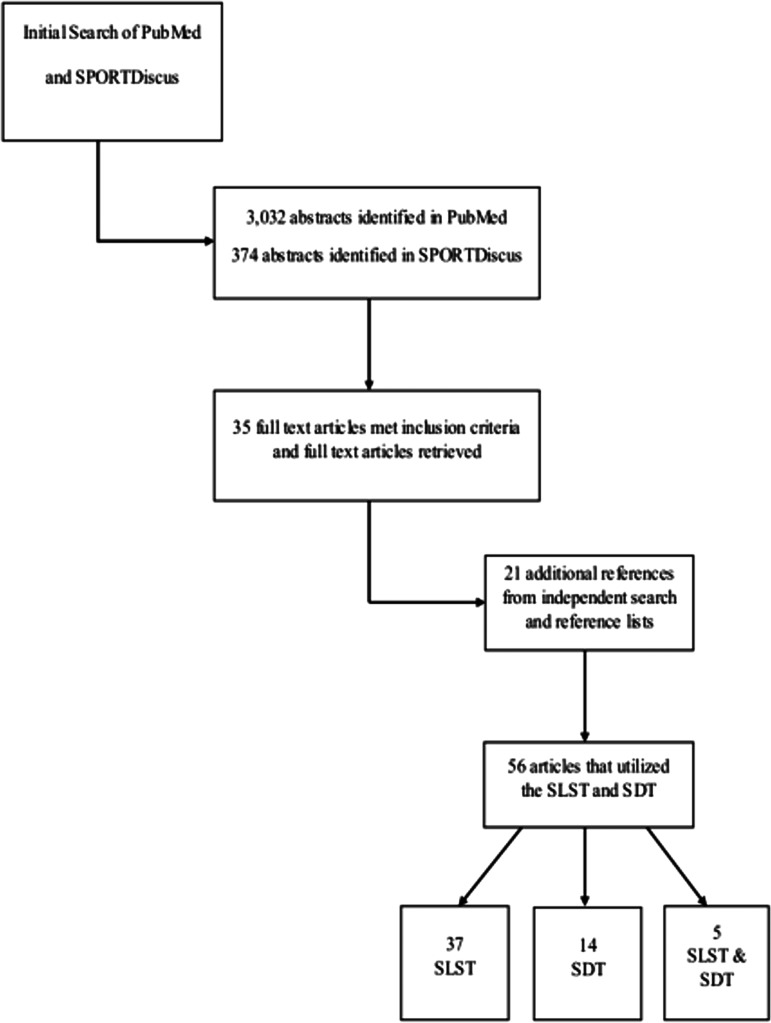
A total of 3,406 research articles were identified in the initial search. After applying the inclusion/exclusion criteria and subsequent evaluation of reference lists, a total of 56 studies were included in the review. Search results included 37 articles describing the SLST, 14 describing the SDT, and 5 articles describing a combination of the SLST and SDT as shown in Figure 3. A total of 27 articles addressed validity, 15 articles addressed reliability, and 14 addressed both reliability and validity. There were no articles that addressed the responsiveness of testing for either the SLST or SDT.
Figure 3.
Results of Literature Search for Single Leg Squat and Step-Down Tests. SLST – single leg squat test; SDT – step-down test.
There was no evidence of reliability in administration or evaluation procedures for either the SLST or SDT specifically in patients with documented hip dysfunction. Evidence of reliability for the visual assessment of overall quality of movement for both the SLST and SDT in both healthy subjects and those with documented knee injuries is shown in Table 1. Both the SLST and SDT were found to be reliable when the evaluation was based on the evaluators overall impression of test performance as well as evaluation of specific biomechanical deviations for posture and/or movement of the trunk, pelvis, hip, and knee.29-32
Table 1.
Studies offering evidence of reliability in overall quality of movement for SLST and SDT
| Study | Test | Evidence of Reliability | Normative Values for Evaluation of Participants |
|---|---|---|---|
| Crossley (2011) | SLST | Inter-rater (Kappa = 0.6 – 0.8, 73% - 87% agreement) Intra-rater (Kappa = 0.61 -0.8, 73%-87% agreement) |
Quality of movement rated as “poor”, “fair” or “good”, based on 5-point criteria |
| Junge (2012) | SLST | Inter-rater (Kappa = 0.54 – 0.86, 86%-97% agreement) | Postural orientation of knee, hip, and trunk, based on a 4-point scale |
| Kennedy (2010) | SLST | Intra-rater (ICC = 0.85 & 0.95, 0.74-0.97; Kappa = 0.31 & 0.53) Inter-rater (ICC = 0.8 & 0.92, 0.71-0.95; Kappa = 0.37 & 0.26) |
Evaluation of trunk, hip, knee, lower leg, and overall pattern on repetitions (ICC) and limiting factor (Kappa) for left and right leg. |
| Loudon (2002) | SDT | Intra-rater (ICC = 0.94, SEM = 0.53) | Overall quality of movement |
| Park (2013) | SDT | Inter-rater (Kappa = 0.80, 85% agreement) | Quality of movement based on 5-point criteria |
| Piva (2006) | SDT | Inter-rater (Kappa = 0.67, 80% agreement) | Quality of movement based on 5-point criteria |
| Rabin (2014) | SDT | Inter-rater Overall (Kappa = 0.81, 0.68 – 0.94) Trunk (Kappa = 0.72, 0.57 – 0.87) Pelvis (Kappa = 0.71, 0.52 – 0.90) Knee (Kappa = 0.87, 0.75 – 0.99) |
Overall quality of movement & individual rating criteria for trunk, pelvis, and knee rated as “good” or “moderate” |
| Herman (2016) | SDT | Inter-rater Overall (ICC = 0.61, 73.83% agreement) <1 year (ICC = 0.61, 66.67% agreement) 1 -5 years (ICC = 0.59, 78.33% agreement) >5 years (ICC = 0.59, 73.40% agreement) |
Overall quality of movement rated as “good”, “fair”, “poor” for a cohort of physical therapists with varying levels of experience. |
| Chmielewski (2007) | SLST/SDT | Inter-rater (Overall method) SLST (Kappa = 0.01, (-0.27) – 0.25) SDT (Kappa = 0.19, (-0.15) – 0.53) Inter-rater (Specific method) SLST (Kappa = 0.18, 0.04 – 0.32) SDT (Kappa = 0.22, 0.07– 0.36) |
Overall vs. specific methods for quality of movement |
SLST – single leg squat test; SDT – step-down test; ICC – intraclass correlation coefficient; Kappa = Cohen's Kappa; 95% Confidence Interval
There was no evidence of validity in administration of the SDT specifically in patients with documented hip dysfunction. One study for the SLST demonstrated evidence of validity in administration for patients with hip dysfunction.16 Both tests demonstrated evidence of validity in kinematic and muscle function assessment in healthy patients. Table 2 presents the evidence related to validity in evaluation of hip function for both the SLST and SDT.
Table 2.
Studies offering evidence of validity for kinematic evaluation of the trunk, pelvis, hip, and knee
| Study | Test | Evidence of Validity |
|---|---|---|
| Claiborne (2006) | SLST | Hip abduction and internal rotation strength are strong predictors for control of valgus motion at the knee. |
| Crossley (2011) | SLST | Individuals graded as “good” on test performance had greater hip abduction torque and trunk side flexion force in comparison to those graded as “poor.” |
| DiMattia (2005) | SLST | Weak, positive correlation between hip-abduction strength and hip-adduction angle during test performance. |
| Hatton (2014) | SLST | Individuals with documented hip chondropathy had decreased balance during test performance. Increased range of motion for hip external rotation may predict balance impairments. |
| Hollman (2014) | SLST | Individuals graded as “good” had less hip flexion and adduction during test performance than those graded as “poor” performers. Increased medial hip rotation and adduction occurred with an increased knee valgus angle. |
| Khuu (2016) | SLST | Mechanics of the trunk, pelvis, and lower extremity during test performance was affected by the positioning of the non-stance leg. The SLST-Back positioning caused the most kinematic changes at the hip and pelvis during testing. |
| Mauntel (2013) | SLST | Increased hip abductor and external rotator strength influences decreasing medial knee deviation during test performance. |
| Shirey (2012) | SLST | The intentional core activation of individuals during test performance had significantly smaller hip frontal plane displacement (p=0.01) and a larger angle of knee flexion (p=0.009). |
| Stickler (2015) | SLST | The hip abductors, external rotators, extensors, and core musculature have an impact on the frontal plane projection angle of the knee during test performance. Specifically, strength of the hip abductors was the greatest indicator of valgus deviation at the knee. |
| Burnham (2016) | SDT | Hip abduction, external rotation, and extension strength, as well as trunk endurance were positively correlated with repetitions of SDT. |
| Hollman (2009) | SDT | Recruitment of the gluteus maximus muscle may have a greater effect on test performance than muscle strength. Hip adduction is positively correlated to knee valgus in the frontal plane. |
| Oliver (2016) | SDT | Both the hamstring and gluteus medius muscles were classified as “strong” during test performance. |
| Hatfield (2016) | SLST & SDT | The SDT and SLST were shown to have similar kinematic requirements with high hip flexion and adduction muscle impulses. The SDT was shown to have a higher hip adduction angle as well as frontal plane excursion angle of the hip. |
| Lewis (2015) | SLST & SDT | The SLST and SDT were kinematically different with the SLST having less hip adduction but more hip external rotation and knee abduction (p ≤ 0.03) than the SDT. |
SLST – single leg squat test; SDT – step-down test
Results attained from studies on the SLST2,18,29,33-41 (Table 3) and SDT6,13,29,33,39,40,42-44 (Table 4) were used to create a standardized protocol and scoring criteria for both functional performance tests for use in examination of individuals with non-arthritic hip pain. Evaluation for the proposed protocol was based on an overall impression of the trials (including balance and evaluation of the arm strategy), posture or movement of the trunk, posture of the pelvis, hip joint movement and posture, and knee joint movement and posture.29-32
Table 3.
Single Leg Squat Test Protocol
| Each individual must wear shorts that enables the evaluator to observe their knee position throughout the entire SLST. A “T” (6” horizontal and 10” vertical) will be marked with 1 ½” white athletic tape on the floor. Patients will be instructed to stand barefoot with both legs shoulder width apart and parallel to each other, with arms positioned at their side. They are instructed to place their unaffected foot on the long axis of the “T” shape with the second metatarsal aligned perpendicular to the stem but not touching the line. The individuals will then transition to a single leg-stance on the unaffected leg with the non-stance knee flexed to 90 ° and thigh vertically aligned with the stance leg. While maintaining a straight trunk the participants are then instructed to squat down until they can no longer see the line in front of their toes (∼45-60 degrees of flexion), while maintaining a balanced and controlled motion at a rate of 1 squat per 2 seconds. After completion of each repetition the individuals will return to their original standing position before beginning another squat. The SLST will be performed a total of 3 times. The participants then will complete 3 repetitions on the affected side. A single investigator will demonstrate the entire procedure before the participation of an individual. |
| The evaluator assessed the overall test performance of the individuals affected side. Along with an overall impression, each repetition was graded as “positive” or “negative” for the five criteria listed below. For the individual to pass, the evaluator must first grade the overall impression of test performance as passing. Second, a total of 4 out of the 5 specific criteria must be negative for deviation. A passing grade of at least 1 out of the 3 tests are needed for evaluation. Therefore, failing 2 out of 3 tests still elicits a passing assessment. |
|
Scoring Criteria Overall impression (balance, gross arm deviation, ability to perform test)
|
SLST – single leg squat test
Table 4.
Step-Down Test Protocol
| Each individual must wear shorts that enable the evaluator to observe their knee position throughout the entire SDT. They are instructed to stand barefoot with both legs shoulder width apart and parallel to each other with arms positioned at their side on a standardized step that is 20-25 cm high. They are then asked to transition to a single leg-stance on the unaffected leg with the non-stance knee extended out from the step and foot in dorsiflexion. The stance leg is positioned so that the toes are even with the front edge of the step. While maintaining a straight trunk, individuals are then instructed to bend their knee on the stance leg until the heel of the contralateral leg touches the floor. Without putting weight on the heel, they must return to the starting position at a rate of 1 squat per 2 seconds. After completion of each repetition the participants will return to their original standing position before beginning the next repetition. Individuals will perform the SDT a total of 3 times. They will then complete 3 repetitions on the affected side. A single investigator will demonstrate the entire test performance before the participation of an individual. |
| The evaluator assessed the overall test performance of the individuals affected side. Along with an overall impression, each repetition was graded as “positive” or “negative” for the five criteria listed below. For the individual to pass, the evaluator must first grade the overall impression of test performance as passing. Second, a total of 4 out of the 5 specific criteria must be negative for deviation. A passing grade of at least 1 out of the 3 tests are needed for evaluation. Therefore, failing 2 out of 3 tests still elicits a passing assessment. |
|
Scoring Criteria Overall impression (balance, balance or acceleration provided by heel contact, gross arm deviation, ability to perform test) 1. Trunk movement (forward lean, lateral rotation, lateral flexion, thoracic rotation) 2. Posture of the pelvis (tilt or rotation) 3. Posture of the hip joint (adduction or internal rotation) 4. Posture of the knee (knee valgus or tremor) 5. Depth of squat (inability to contact heel to ground) |
SDT – step-down test
DISCUSSION
This literature review identified evidence of reliability and validity for the SLST and SDT, with a large proportion of the literature determining these psychometric properties in the healthy population. While there was only one study that offered evidence of validity for the SLST in individuals with non-arthritic hip pain, there was evidence that both tests may be useful in evaluating for range of motion, strength, and proprioceptive deficiencies of the hip and surrounding muscular structures. These tests assess for several deviations in trunk, pelvis, and hip performance that are considered important when assessing individuals with non-arthritic hip pain. From the identified articles, a standardized protocol and scoring criteria was created for administering the SLST and SDT based on the best available evidence.
The SLST demonstrated moderate to excellent reliability for evaluation of test performance. Visual assessment of overall quality of movement for the SLST showed a 73-87% agreement for inter-rater and intra-rater reliability (Kappa = 0.61 – 0.80) based on a five-point scoring criteria.29 Moderate to excellent reliability was also present in the inter-tester evaluation of adolescent trunk, hip, and knee postural orientation utilizing a four-point scoring criteria (Kappa = 0.54 – 0.86).45 Visual observation of dynamic knee valgus and frontal plane projection angle (FPPA) was also shown to be reliable in evaluation of asymptomatic patients during performance of the SLST.4,35,46-49 While the SLST test has been shown effective in the pass/fail evaluation of an individual's trunk, hip, knee, and lower leg movement patterns, a more objective set of criteria is necessary for reliable identification of specific biomechanical deficiencies in multiple planes.30 Kinematic evaluation of the trunk, pelvis, hip, and knee utilizing an electromagnetic tracking system demonstrated excellent intra-rater, intrasession reliability (ICC = 0.83 – 1.00) and intra-rater, intersession reliability (ICC = 0.82 – 0.96).50
In addition to evidence of reliability, the SLST was valid in the evaluation of dynamic lower extremity control and hip muscle function.16,29,51 Individuals with documented hip chondropathy were shown to have an overall decrease in balance, as determined by the amplitude and velocity of center of pressure movement when performing the SLST compared to healthy individuals.16 Increased hip external rotation range of motion may also predict balance impairments for those with non-arthritic hip pathologies.16 Moderate, negative correlations between test performance and muscle function of the hip abductors (r = –0.37, p < 0.05).53 Hip abduction (r = 0.466, p = 0.002), hip external rotation (r = 0.464, p = 0.003), hip extension (r = 0.396, p = 0.012) and core musculature (r = 0.426, p = 0.006) were shown to have moderate, positive correlations to the frontal plane projection angle during performance of the SLST.54 Individuals who were graded as having a “poor” SLST showed weakness and slower activation of the hip abductors specifically the gluteus medius as measured by electromyographic activity,29 with an increase in hip adduction and flexion motions compared to those that were graded as “good” based on visual observation56 Greater strength in the hip abductors and an increase in depth of knee flexion was shown to be related to a decrease in the valgus motion of the knee during the SLST.53 The increase in coactivation of gluteal and hip adductor muscles was shown to also cause a decrease in valgus motion of the knee during the SLST as measured by electromyographic activity and an electromagnetic motion tracking system.57,58 The SLST was shown to induce less hip adduction but more hip external rotation and knee abduction compared to the SDT.17
Although the evidence for reliability and validity of the SDT is less than that for the SLST, the SDT was shown to have moderate to excellent reliability for test performance. The SDT showed excellent interrater reliability for overall quality of movement (Kappa = 0.81, 0.68 – 0.94), as well as moderate to excellent interrater reliability for trunk alignment (Kappa = 0.72, 0.57 – 0.87), pelvic plane (Kappa = 0.71, 0.52 – 0.90), and knee positioning (Kappa = 0.87, 0.75 – 0.99) during performance in individuals with patellofemoral pain.59,60 Intra-rater reliability for SDT performance in individuals with patellofemoral pain syndrome and healthy subjects was also shown to be excellent (ICC = 0.94, SEM = 0.53).6 The overall movement quality of the SDT has been shown to have moderate (Kappa = 0.67, 80% agreement)43 to excellent inter-tester reliability (Kappa = 0.80, 85% agreement)31 based on a five point scoring criteria in healthy individuals.43 Moderate inter-rater reliability for the SDT was even shown amongst 142 physical therapists who evaluated 15 healthy subjects on a three level rating criteria (ICC = 0.61, 74% agreement).61 Kinematic evaluation of the trunk, pelvis, hip, and knee utilizing an electromagnetic tracking system demonstrated excellent intra-rater, intrasession reliability (ICC = 0.83 – 1.00) and intra-rater, intersession reliability (ICC = 0.82 – 0.97).50
The available studies demonstrated evidence of validity for evaluation of hip and trunk muscle function. Hip abduction (r = 0.446, p<0.001) and external rotation (r = 0.448, p<0.001) strength were positively correlated with performance of the SDT.42 Those evaluated as having “good” movement quality had significantly stronger hip abductors, increased knee active range of motion, and increased hip adduction range of motion than those with “moderate” movement quality.31 “Moderate” quality of movement patterns also had an increased contralateral pelvic drop (p = 0.01) and increased knee external rotation (p = 0.04) compared to those that were evaluated as “good.”62 The SDT was found to be more biomechanically demanding when compared to the SLST, however, the differences between the two were not statistically significant (p range = 0.36 – 1.00).19 Although similar in performance, when compared to the SLST the SDT demonstrated significantly greater knee flexion (p<0.001), as well as hip flexion and adduction (p≤0.013) during test performance.17,19 The frontal plane projection angle of the hip was also significantly higher during the SDT than in the SLST (p<.001) as observed with 3-D imaging, surface electromyographic activity, and ground reaction forces.19 Examination of test performance for both functional tests have shown an increase in hip abductor strength and degree of knee flexion to have a significant effect on decreasing hip adduction and valgus motion at the knee.17,54 The SLST and SDT are beneficial in evaluating patients through visual observation of pelvic tilt and rotation as well as trunk stability.42,50,52
This literature review was used to assimilate current evidence to construct standardized protocols for administering the SLST and SDT for use during the examination of individuals with non-arthritic hip pain. The proposed protocols for both the SLST and SDT reflect the authors’ interpretations of best available evidence of reliability and validity extracted from the current peer-reviewed literature. Evaluation was based on an overall impression of each repetition (including balance and evaluation of the arm strategy), posture or movement of the trunk, positioning of the pelvic plane, hip joint movement and positioning, and knee joint movement and posture.29-32
The accumulation of procedures utilized for both the SLST and SDT were extracted and analyzed by the authors from the current peer-reviewed literature in order to assess for reliability and validity. These results were summarized and combined to create a recommended protocol and evaluation procedure for clinical utilization of the SLST and SDT in individuals with non-arthritic hip pain. The standardized protocol and scoring criteria for both the SLST and SDT can be found in Table 3 and Table 4, respectively.
There are limitations present in the current review that need to be considered when interpreting the results and recommendations. The proposed protocols for administration of the SLST and SDT are based on the authors interpretation of the current peer-reviewed literature. These recommendations may not be the only viable options for administration of the SLST and SDT during assessment of individuals with non-arthritic hip pain. Different techniques for test performance as well as differing landmarks for the visual evaluation criteria could be utilized with effectiveness. Other functional performance tests may be beneficial in the evaluation of individuals with intra-articular conditions of the hip. Caution should also be exercised when generalizing the results of the current review to other populations. Future studies are needed to demonstrate the diagnostic accuracy of the SLST and SDT in evaluation of individuals with non-arthritic hip pain. The use of three-dimensional motion analysis technology and electromyographic assessment could also add quantitative analysis to validate the use of the SLST and SDT in this population.
CONCLUSIONS
Evidence was available to support the reliable and valid use of the SLST and SDT. Both tests have been utilized to assess quality of movement in the hip and surrounding structures. These tests are indicative of the weight-bearing demands and dynamic muscular control needed for sports related movements. The best procedures used during research to assess reliability and validity of the tests were extracted, analyzed, summarized, and combined in order to create suggestions for practical, clinical procedures for utilization during administration of the SLST and SDT in examination of individuals with non-arthritic hip pain.
REFERENCES
- 1.Bird SP Markwick WJ. Musculoskeletal screening and functional testing: Considerations for basketball athletes. Int J Sports Phys Ther. 2016;11(5):784-802. [PMC free article] [PubMed] [Google Scholar]
- 2.Kivlan BR Martin RL. Functional performance testing of the hip in athletes: a systematic review for reliability and validity. Int J Sports Phys Ther. 2012;7(4):402-412. [PMC free article] [PubMed] [Google Scholar]
- 3.Ardern CL Glasgow P Schneiders A, et al. 2016 Consensus statement on return to sport from the first world congress in sports physical therapy, Bern. Br J Sports Med. 2016;50(14):853-864. [DOI] [PubMed] [Google Scholar]
- 4.Ugalde V Brockman C Bailowitz Z Pollard CD. Single leg squat test and its relationship to dynamic knee valgus and injury risk screening. Phys Med Rehabil. 2015;7(3):229-235; quiz 235. [DOI] [PubMed] [Google Scholar]
- 5.Kline PW Johnson DL Ireland ML Noehren B. Clinical predictors of knee mechanics at return to sport after acl reconstruction. Med Sci Sports Exerc. 2016;48(5):790-795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loudon JK Wiesner D Goist-Foley HL Asjes C Loudon KL. Intrarater reliability of functional performance tests for subjects with patellofemoral pain syndrome. J Athl Train. 2002;37(3):256-261. [PMC free article] [PubMed] [Google Scholar]
- 7.Kulas AS Hortobagyi T DeVita P. Trunk position modulates anterior cruciate ligament forces and strains during a single-leg squat. Clin Biomech. 2012;27(1):16-21. [DOI] [PubMed] [Google Scholar]
- 8.Mascal CL Landel R Powers C. Management of patellofemoral pain targeting hip, pelvis, and trunk muscle function: 2 case reports. J Orthop Sports Phys Ther. 2003;33(11):647-660. [DOI] [PubMed] [Google Scholar]
- 9.Beutler AI Cooper LW Kirkendall DT Garrett WE Jr. Electromyographic analysis of single-leg, closed chain exercises: implications for rehabilitation after anterior cruciate ligament reconstruction. J Athl Train. 2002;37(1):13-18. [PMC free article] [PubMed] [Google Scholar]
- 10.Nakagawa TH Moriya ET Maciel CD Serrao FV. Trunk pelvis, hip, and knee kinematics hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012;42(6):491-501. [DOI] [PubMed] [Google Scholar]
- 11.Nakagawa TH Serrao FV Maciel CD Powers CM. Hip and knee kinematics are associated with pain and self-reported functional status in males and females with patellofemoral pain. Int J Sports Med. 2013;34(11):997-1002. [DOI] [PubMed] [Google Scholar]
- 12.Anderson G Herrington L. A comparison of eccentric isokinetic torque production and velocity of knee flexion angle during step down in patellofemoral pain syndrome patients and unaffected subjects. Clin Biomech. 2003;18(6):500-504. [DOI] [PubMed] [Google Scholar]
- 13.Souza RB Powers CM. Differences in hip kinematics muscle strength, and muscle activation between subjects with and without patellofemoral pain. J Orthop Sports Phys Ther. 2009;39(1):12-19. [DOI] [PubMed] [Google Scholar]
- 14.Lee SP Souza RB Powers CM. The influence of hip abductor muscle performance on dynamic postural stability in females with patellofemoral pain. Gait Posture. 2012;36(3):425-429. [DOI] [PubMed] [Google Scholar]
- 15.Levinger P Gilleard W Coleman C. Femoral medial deviation angle during a one-leg squat test in individuals with patellofemoral pain syndrome. Phys Ther Sport. 2007;8(4):163-168. [Google Scholar]
- 16.Hatton AL Kemp JL Brauer SG Clark RA Crossley KM. Impairment of dynamic single-leg balance performance in individuals with hip chondropathy. Arthritis Care Res. 2014;66(5):709-716. [DOI] [PubMed] [Google Scholar]
- 17.Lewis CL Foch E Luko MM Loverro KL Khuu A. Differences in lower extremity and trunk kinematics between single Leg squat and step down tasks. PLoS One. 2015;10(5):e0126258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khuu A Foch E Lewis CL. Not all single leg squats are equal: a biomechanical comparison of three variations. Int J Sports Phys Ther. 2016;11(2):201-211. [PMC free article] [PubMed] [Google Scholar]
- 19.Hatfield GL Charlton JM Cochrane CK, et al. The biomechanical demands on the hip during progressive stepping tasks. J Strength Cond Res. 2016. [DOI] [PubMed] [Google Scholar]
- 20.Chinkulprasert C Vachalathiti R Powers CM. Patellofemoral joint forces and stress during forward step-up, lateral step-up, and forward step-down exercises. J Orthop Sports Phys Ther. 2011;41(4):241-248. [DOI] [PubMed] [Google Scholar]
- 21.Luque-Seron JA Medina-Porqueres I. Anterior cruciate ligament strain in ivo: systematic review. Sports Health. 2016;8(5):451-455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim HY. Statistical notes for clinical researchers: Evaluation of measurement error 2: dahlberg's error bland-altman method, and kappa coefficient. Restor Dent Endod. 2013;38(3):182-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim HY. Statistical notes for clinical researchers: Evaluation of measurement error 1: using intraclass correlation coefficients. Restor Dent Endod. 2013;38(2):98-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andersen EM. Criteria for Assessing the Tools of Disability Outcomes Research. Arch Phys Med Rehabil. 2000;81(Suppl 2 ):S15-S20. [DOI] [PubMed] [Google Scholar]
- 25.Zaki R Bulgiba A Nordin N Azina Ismail N. A systematic review of statistical methods used to test for reliability of medical instruments measuring continuous variables. Iran J Basic Med Sci. 2013;16(6):803-807. [PMC free article] [PubMed] [Google Scholar]
- 26.Kwiecien R Kopp-Schneider A Blettner M. Concordance analysis: part 16 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2011;108(30):515-521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bruton A CJ Holgate ST. Reliability: What is it and how is it measured? Physiotherapy 2000;86(2):94-99. [Google Scholar]
- 28.Karras DJ. Statistical methodology: II. Reliability and validity assessment in study design, Part B. Acad Emerg Med. 1997;4(2):144-147. [DOI] [PubMed] [Google Scholar]
- 29.Crossley KM Zhang WJ Schache AG Bryant A Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866-873. [DOI] [PubMed] [Google Scholar]
- 30.Kennedy MD Burrows L Parent E. Intrarater and interrater reliability of the single-leg squat test. Athl Ther Today. 2010;15(6):32-36. [Google Scholar]
- 31.Park KM Cynn HS Choung SD. Musculoskeletal predictors of movement quality for the forward step-down test in asymptomatic women. J Orthop Sports Phys Ther. 2013;43(7):504-510. [DOI] [PubMed] [Google Scholar]
- 32.Herman G Nakdimon O Levinger P Springer S. Agreement of an evaluation of the forward-step-down test by a broad cohort of clinicians with that of an expert panel. J Sport Rehabil. 2016;25(3):227-232. [DOI] [PubMed] [Google Scholar]
- 33.Chmielewski TL Hodges MJ Horodyski M Bishop MD Conrad BP Tillman SM. Investigation of clinician agreement in evaluating movement quality during unilateral lower extremity functional tasks: a comparison of 2 rating methods. J Orthop Sports Phys Ther. 2007;37(3):122-129. [DOI] [PubMed] [Google Scholar]
- 34.Weeks BK Carty CP Horan SA. Kinematic predictors of single-leg squat performance: a comparison of experienced physiotherapists and student physiotherapists. BMC Musculoskelet Disord. 2012;13:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ageberg E Bennell KL Hunt MA Simic M Roos EM Creaby MW. Validity and inter-rater reliability of medio-lateral knee motion observed during a single-limb mini squat. BMC Musculoskelet Disord. 2010;11:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stensrud S Myklebust G Kristianslund E Bahr R Krosshaug T. Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. Br J Sports Med. 2011;45(7):589-595. [DOI] [PubMed] [Google Scholar]
- 37.Graci V Van Dillen LR Salsich GB. Gender differences in trunk, pelvis and lower limb kinematics during a single leg squat. Gait Posture. 2012;36(3):461-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bremander AB Dahl LL Roos EM. Validity and reliability of functional performance tests in meniscectomized patients with or without knee osteoarthritis. Scand J Med Sci Sports. 2007;17(2):120-127. [DOI] [PubMed] [Google Scholar]
- 39.Tijssen M van Cingel RE Staal JB Teerenstra S de Visser E Nijhuis-van der Sanden MW. Physical therapy aimed at self-management versus usual care physical therapy after hip arthroscopy for femoroacetabular impingement: study protocol for a randomized controlled trial. Trials. 2016;17:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agresta CE Church C Henley J Duer T O’Brien K. Single leg squat performance in active ddolescents age 8 to 17 years. J Strength Cond Res. 2017;31(5):1187-1191. [DOI] [PubMed] [Google Scholar]
- 41.Perrott MA Pizzari T Opar M Cook J. Development of clinical rating criteria for tests of lumbopelvic stability. Rehabil Res Pract. 2012;2012:803637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burnham JM Yonz MC Robertson KE, et al. Relationship of hip and trunk muscle function with single leg step-down performance: implications for return to play screening and rehabilitation. Phys Ther Sport. 2016;22:66-73. [DOI] [PubMed] [Google Scholar]
- 43.Piva SR Fitzgerald K Irrgang JJ, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Disord. 2006;7:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rabin A Kozol Z. Measures of range of motion and strength among healthy women with differing quality of lower extremity movement during the lateral step-down test. J Orthop Sports Phys Ther. 2010;40(12):792-800. [DOI] [PubMed] [Google Scholar]
- 45.Junge T Balsnes S Runge L Juul-Kristensen B Wedderkopp N. Single leg mini squat: an inter-tester reproducibility study of children in the age of 9-10 and 12-14 years presented by various methods of kappa calculation. BMC Musculoskelet Disord. 2012;13:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Poulsen DR James CR. Concurrent validity and reliability of clinical evaluation of the single leg squat. Physiother Theory Pract. 2011;27(8):586-594. [DOI] [PubMed] [Google Scholar]
- 47.Raisanen A Pasanen K Krosshaug T Avela J Perttunen J Parkkari J. SinglelLeg squat as a tool to evaluate young athletes' frontal plane knee control. Clin J Sport Med. 2016;26(6):478-482. [DOI] [PubMed] [Google Scholar]
- 48.Almeida GP Silva AP Franca FJ Magalhaes MO Burke TN Marques AP. Relationship between frontal plane projection angle of the knee and hip and trunk strength in women with and without patellofemoral pain. J Back Musculoskelet Rehabil. 2016;29(2):259-266. [DOI] [PubMed] [Google Scholar]
- 49.Tate J Dale B Baker C. Expert versus novice interrater and intrarater reliability of the frontal plane projection angle during a single-leg squat. Int J Athl Ther Train. 2015;20(4):23-27. [Google Scholar]
- 50.Nakagawa TH Moriya ET Maciel CD Serrao FV. Test-retest reliability of three-dimensional kinematics using an electromagnetic tracking system during single-leg squat and stepping maneuver. Gait Posture. 2014;39(1):141-146. [DOI] [PubMed] [Google Scholar]
- 51.Charlton PC Bryant AL Kemp JL Clark RA Crossley KM Collins NJ. Single-leg squat performance is impaired 1 to 2 years after hip arthroscopy. Phys Med Rehabil. 2016;8(4):321-330. [DOI] [PubMed] [Google Scholar]
- 52.Dingenen B Malfait B Vanrenterghem J Verschueren SM Staes FF. The reliability and validity of the measurement of lateral trunk motion in two-dimensional video analysis during unipodal functional screening tests in elite female athletes. Phys Ther Sport. 2014;15(2):117-123. [DOI] [PubMed] [Google Scholar]
- 53.Claiborne TL Armstrong CW Gandhi V Pincivero DM. Relationship between hip and knee strength and knee valgus during a single leg squat. J Appl Biomech. 2006;22(1):41-50. [DOI] [PubMed] [Google Scholar]
- 54.Stickler L Finley M Gulgin H. Relationship between hip and core strength and frontal plane alignment during a single leg squat. Phys Ther Sport. 2015;16(1):66-71. [DOI] [PubMed] [Google Scholar]
- 55.Shirey M Hurlbutt M Johansen N King GW Wilkinson SG Hoover DL. The influence of core musculature engagement on hip and knee kinematics in women during a single leg squat. Int J Sports Phys Ther. 2012;7(1):1-12. [PMC free article] [PubMed] [Google Scholar]
- 56.Hollman JH Galardi CM Lin IH Voth BC Whitmarsh CL. Frontal and transverse plane hip kinematics and gluteus maximus recruitment correlate with frontal plane knee kinematics during single-leg squat tests in women. Clin Biomech. 2014;29(4):468-474. [DOI] [PubMed] [Google Scholar]
- 57.Mauntel TC Begalle RL Cram TR, et al. The effects of lower extremity muscle activation and passive range of motion on single leg squat performance. J Strength Cond Res. 2013;27(7):1813-1823. [DOI] [PubMed] [Google Scholar]
- 58.Mauntel TC Frank BS Begalle RL Blackburn JT Padua DA. Kinematic differences between those with and without medial knee displacement during a single-leg squat. J Appl Biomech. 2014;30(6):707-712. [DOI] [PubMed] [Google Scholar]
- 59.Rabin A Kozol ZVI Moran U Efergan A Geffen Y Finestone AS. Factors associated with visually assessed quality of movement during a lateral step-down test among individuals with patellofemoral pain. J Orthop Sports Phys Ther. 2014;44(12):937-946. [DOI] [PubMed] [Google Scholar]
- 60.Rabin A Portnoy S Kozol Z. The association of ankle dorsiflexion range of motion with hip and knee kinematics during the lateral step-down test. J Orthop Sports Phys Ther. 2016;46(11):1002-1009. [DOI] [PubMed] [Google Scholar]
- 61.Herman G Nakdimon O Levinger P Springer S. Agreement of an evaluation of the forward-step-down test by a broad cohort of clinicians with that of an expert panel. J Sport Rehabil. 2016;25(3):227-232. [DOI] [PubMed] [Google Scholar]
- 62.Rabin A Portnoy S Kozol Z. The association between visual assessment of quality of movement and three-dimensional analysis of pelvis, hip, and knee kinematics during a lateral step down test. J Strength Cond Res. 2016;30(11):3204-3211. [DOI] [PubMed] [Google Scholar]