Abstract
Background
Medial collateral ligament (MCL) injuries are one of the most commonly treated knee pathologies in sports medicine. The MCL serves as the primary restraint to valgus force. The large majority of these injuries do not require surgical intervention.
Case Subject Description
A 30-year-old professional wrestling athlete presented to the clinic with acute complaints of right medial knee pain resulting from a traumatic valgus force. Physical exam revealed Grade 3 MCL injury. Magnetic resonance imaging confirmed clinical diagnosis of a Grade 3 proximal MCL tear. This athlete had sustained a prior grade 3 ACL injury with Grade 3 distal MCL injury which required surgery to reconstruct the ACL and repair the MCL 13 months prior, in November of 2015.
Outcomes
The subject was successfully treated with a series of three sequential Leukocyte Rich Platelet Rich Plasma (LR-PRP) Injections spaced evenly one week apart in addition to an early physical therapy regimen. The total treatment time was cut down from an expected 35-49 days to 31 days.
Discussion
When paired with the appropriate rehabilitation treatment progression, the use of LR-PRP injections in the treatment of an isolated MCL tear was beneficial for this subject.
Conclusion
The results of this case report indicate that the use of LR-PRP and early rehabilitation shows promise in treating an acute grade 3 MCL injury. Future research utilizing randomized controlled trials are needed.
Level of Evidence
Case Report, 4
Keywords: Knee, Leukocyte-Rich PRP, medial collateral ligament
BACKGROUND
Medial collateral ligament (MCL) injuries are one of the most commonly treated knee pathologies in sports medicine.1,2 The MCL serves as the primary restraint to valgus force at both 5˚ (57.4%) and 25˚ (78.2%) knee flexion.3 The large majority of these injuries do not require surgical intervention. Furthermore, anatomically, a proximal injury is more favorable than a distal injury in regards to healing rate and regaining stability utilizing a conservative treatment approach.2 Shelbourne et al2 has classified these injuries as follows: Grade 1: No laxity with a solid endpoint, Grade 2: Some medial laxity and a firm endpoint, Grade 3: Complete disruption of the medial collateral ligament with substantial medial opening.2 Conservative care is the standard for grades 1 and 2 injuries. Treatment of grade 3 injuries remains controversial, however good outcomes have been reported with conservative care.5 Additionally, the treatment for distal versus proximal MCL injuries does vary based on the extent of the injury, with distal grade 3 often requiring surgery.2 Holden et al4 reported return after MCL injury in as early as 10 days for Grade 1, and four weeks for a Grade 2. Kim et al.5 reported a five to seven week recovery period for a Grade 3 injury. A general rule of thumb with MCL injury recovery is two weeks off per grade, although time lost from sport can vary significantly depending on lesion location, treatment progression, and demands of the sport.5,6
Platelet rich plasma (PRP) injections are becoming an increasingly popular adjunct to non-operative treatment protocols. PRP is autologous blood drawn with the intent to concentrate platelet levels higher than physiologic levels, in which, the concentration is typically three to five times higher than physiologic baseline.7 Growth factors and other molecules are contained within the alpha granules of platelets that are involved in tissue repair and pain modulation, among other functions.8-11 A few key factors found involved in tissue repair are transforming growth factor-beta 1 (TGF-B1), insulin-like growth factor (IGF), and, thrombospondin-1.11 PRP injections are initiated with intent to facilitate the healing cascade within the MCL due to the presence of growth factors they subsequently introduced to the site.12 The use of ultrasound to guide the PRP injection allows the physician performing the injection to evaluate the ligament as well as ensure that the PRP is injected within the site of ligament injury. The treatment hypothesis was that the use of a three-injection series of ultrasound guided leukocyte rich PRP (LR-PRP) injections in combination with an early physical therapy program would expedite the healing of the MCL and overall return to participation. The use of three injections was based on the non-invasive ability to monitor ligamentous healing via ultrasound imaging and the clinical expertise of the surgeon and physician performing the injections. The rehabilitation focused on immediate motion to facilitate collagen synthesis and alignment,13 preventing further quadriceps muscle atrophy, restoring lower extremity strength, as well as enhancing the neuromuscular stabilization of the knee and full body kinesthetic awareness. Bracing was used to in conjunction to help control valgus stress on the MCL outside of the clinic.
CASE DESCRIPTION
A 30-year-old professional male wrestling athlete presented to the clinic 1/31/17 with acute complaints of right medial knee pain resulting from a traumatic valgus force that occurred the previous night 1/30/17. The subject of this case report also trained aggressively with weight lifting exercises, cardiovascular exercise, and in Crossfit. The subject had a pertinent past medical history of a right ACL reconstruction with patellar tendon autograft, medial meniscus repair, and distal MCL repair with suture anchor fixation performed in November of 2015. The subject was ambulating with a modified three point gait utilizing bilateral axillary crutches with antalgia and weight bearing as tolerated in a hinged knee brace locked at 0˚. Clinical exam revealed an active range of motion from 5-120˚, 2 cm of swelling measured at the joint line, a negative Lachman's exam with firm end feel, and a grade 2+/3 positive valgus stress test at 5˚ and 30˚ of knee flexion. Strength testing and functional testing were deferred due to the acuity of the injury. The magnetic resonance imaging (MRI) depicted a proximal Grade 3 MCL tear in isolation. Due to the proximal location of the isolated injury, non-operative treatment, via an early physical therapy program, was chosen. In combination with the early physical therapy program, serial LR-PRP injections were performed, timed a week apart for three weeks total under the guidance of ultrasound.
TREATMENT PROGRAM
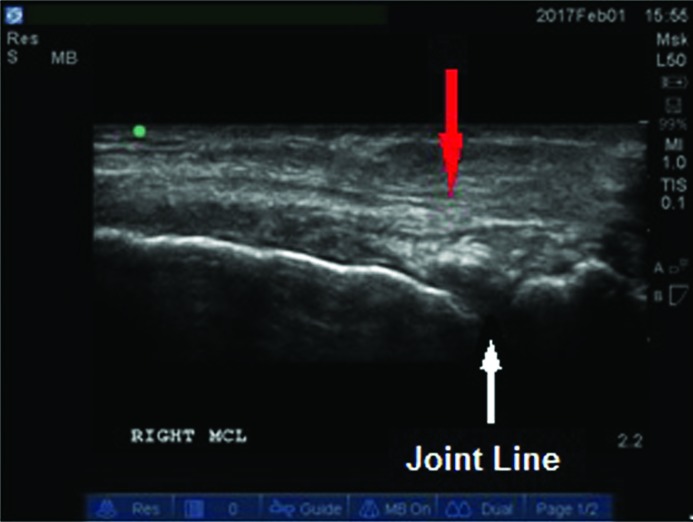
The initial LR-PRP injection was performed on 2/1/17. Figure 1 depicts the soft tissue integrity of the MCL at the time of the initial LR-PRP injection (Figure 1). Immediately following the LR-PRP injection the rehabilitation process began in physical therapy. Weight bearing activity in the clinic was performed under the supervision of the physical therapist (PT) without bracing. Weight bearing activity outside of therapy took place in a hinged knee brace locked at 0˚ until adequate quad control was demonstrated during ambulation, without knee buckling.
Figure 1.
Right MCL soft tissue integrity at the time of initial Leukocyte Rich-Platelet Rich Plasma injection on 2/1/17. The red arrow pointing towards MCL fibers in disarray.
The rehabilitation program was separated into three phases, the acute phase, the intermediate, and, the advanced phase. The first three days post-injection consisted of the acute phase rehabilitation (Table 1). The acute phase rehabilitation consisted of ice for pain relief, passive range of motion (PROM) performed on the right knee by the physical therapist (PT). Initial passive range of motion was performed 10-110˚. Neuromuscular electrical stimulation (NMES) was used during quadriceps setting, straight leg raises, and 90-40˚ knee extensions via a hand trigger that allowed the patient to maintain constant muscle stimulus throughout the duration of each exercise repetition. Straight leg adduction raises were avoided in this phase to decrease valgus stress at the knee. Weight shifting was performed in a staggered stance, shifting in an anterolateral and posterolateral direction on each leg. Partial squats were initiated on a force plate with visual biofeedback to emphasize symmetrical lower extremity loading. Class IV therapeutic laser treatment was also utilized each session for seven minutes at 13.5 Watts (LiteCure,Dover,DE). On day four post-injection, the intermediate phase was initiated for three more days. During this phase the subject was progressed to upright stationary bicycling, isotonic multi-hip machine hip abduction and extension strengthening exercises, seated hip internal and external rotation with elastic band resistance, hip bridging, double leg dynamic balance on an unstable foam surface, and double leg balance on a rocker board with light perturbations (Table 2).
Table 1.
Acute Phase rehabilitation following LR-PRP injection to the knee medial collateral Ligament
| PROM: | Modalities: | Exercises: (3 sets of 10 repetitions) Resistance progressed based on subject's ability Brace not utilized during rehabilitation |
|---|---|---|
| •Subject seated •Performed by PT 10-110˚ |
•Cryotherapy/Ice (Pre/Post) 20 minutes •Class IV Laser: 13.5 Watts 7 minutes •EMPI Portable NMES Unit with Hand trigger |
•With EMPI NMES Unit: •Quad Sets •Straight Leg Raises •Flexion and Abduction •Seated 90-40˚ knee extensions •Partial Squats 0-30˚ on force plate with biofeedback •Weight shifting in staggered stance: •Anterolateral •Posterolateral |
LR-PRP = Leukocyte rich, platelet rich plasma
Table 2.
Intermediate Phase rehabilitation following LR-PRP injection to the knee medial collateral Ligament
| PROM: | Modalities: | Exercises: (3 sets of 10 repetitions) Resistance progressed based on subject's ability Brace not utilized during rehabilitation |
|---|---|---|
| •Subject seated •Performed by PT 10-110˚ |
•Cryotherapy/Ice (Pre/Post) 20 minutes •Class IV Laser: 13.5 Watts 7 minutes •EMPI Portable NMES Unit with Hand trigger |
•With EMPI NMES Unit: •Quad Sets •Straight Leg Raises •Flexion and Abduction •Seated 90-40˚ knee extensions •Upright stationary bicycling •Partial Squats 0-60˚ on force plate with biofeedback •Weight shifting in staggered stance: •Anterolateral •Posterolateral •Seated Hip Internal and External Rotation with elastic band resistance •Hip Bridging •Balance: •Partial Squats on foam •Single leg balance on firm surface/foam •Partial Squats on rocker board with light perturbation |
LR-PRP = Leukocyte rich, platelet rich plasma
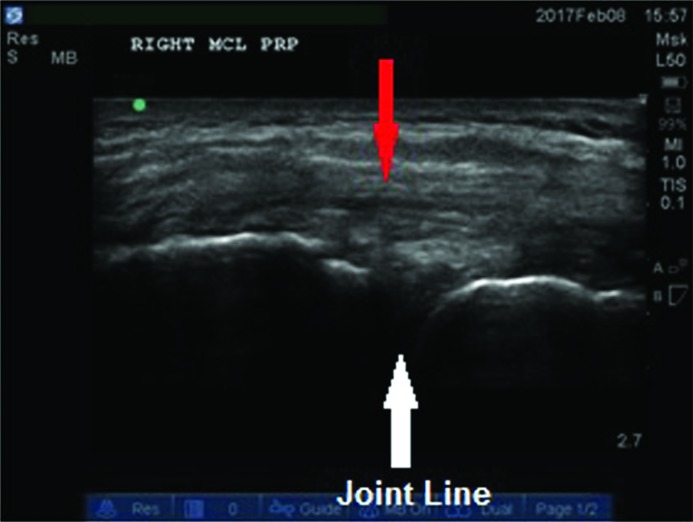
A second injection was performed seven days later (2/8/17) with simultaneous re-assessment of soft tissue integrity with the use of ultrasound imaging (Figure 2). Once again this was followed by the acute phase rehabilitation for three days and again followed by a progression to the intermediate phase rehabilitation up until the next injection. The final injection of the series was performed seven days after (2/15/17) the second injection, with final visual assessment of the MCL (Figure 3). The final injection was followed by the acute phase rehabilitation for three days, then the intermediate phase rehabilitation for five days, followed by a gradual progression into the advanced phase rehabilitation began on day six after the third injection was completed.
Figure 2.
Right MCL soft tissue integrity at the time of the second Leukocyte Rich-Platelet Rich Plasma injection on 2/8/17, The red arrow pointing to signs of tissue remodeling.
Figure 3.
Right MCL soft tissue integrity at the time of the third and final Leukocyte Rich-Platelet Rich Plasma injection on 2/15/17. The arrow pointing to further signs of tissue remodeling.
The advanced phase rehabilitation was comprised of a progression into increased dynamic functional activity and strengthening. Cone marching drills were performed going forward, backwards and laterally. Running in the Alter G treadmill (Alter G, Fremont, CA) was introduced, initially with one minute intervals of work and two minutes of rest, to continuous running. A progression of weight resisted single leg strengthening was initiated in this phase along with a progression of dynamic single leg balance on unstable surfaces. Finally, lower extremity vertical and lateral plyometrics were also introduced during this phase (Table 3.)
Table 3.
Advanced Phase rehabilitation following LR-PRP injection to the knee medial collateral ligament
| PROM: | Modalities: | Exercises: (3 sets of 10 repetitions) Resistance progressed based on subject's ability Brace not utilized during rehabilitation |
|---|---|---|
| •Subject prone •Performed by PT, full range of motion to subject tolerance |
•Moist Heat (pre) 20 minutes •Cryotherapy/Ice (post) 20 minutes •Class IV Laser: 13.5 Watts 7 minutes •Hinged brace utilized for sporting activity outside of the clinic |
•Upright stationary bicycling •Multi Hip Machine:•Abduction •Adduction •Extension •Weighted Wall Sits (0-70˚) •Weighted front step downs •Prone Hamstring Curls •Cone Marching: •Forward/backward •Lateral •Romanian Deadlifts •Seated Hip Internal and External Rotation with elastic band resistance •Clamshells with elastic band resistance •Alter G treadmill running •Interval to continuous •Lateral plyometric hops with sport cord resistance: •Lateral •Diagonal •Onto unstable surface •Vertical Plyometrics: •Box Jumps •Double leg to single leg •Box Drops •Double leg to single leg •Balance: • •Single leg balance on foam with dynamic reaching •Single leg balance on BOSU ball with ball toss •Single leg balance on rocker board with perturbation |
LR-PRP = Leukocyte rich, platelet rich plasma
Cessation of treatment was determined by a clinical exam, which included improved valgus stability with firm end point, return of normal strength, completion of a functional rehabilitation program, satisfactory physical performance during dynamic functional activity, and close communication between the subject, the referring physician, and the physical therapist.
OUTCOMES
The final range of motion measurements were 5-0-140˚ on the right knee (affected knee) compared to 5-0-145˚ on the left knee (uninvolved knee). In total, treatment spanned 31 days, with the subject being discharged 32 days after the initial injury. The total treatment time was cut down from the average expected duration of 35 to 49 days5 before return to full activity, to 31 days. The subject demonstrated a non-antalgic symmetrical walking and running gait, negative valgus stress tests at both 5˚ and 30˚, weight bearing symmetry with squatting, and the ability to perform vertical and lateral plyometric jumps and hops without pain or apprehension. The subject was able to return to professional wrestling full time, unrestricted weightlifting, and training for Crossfit competition.
DISCUSSION
MCL injuries are a commonly treated musculoskeletal pathology seen in orthopedic and sports medicine clinics. A Grade 3 MCL injury is commonly associated with an absence from sport or full athletic participation for five to seven weeks as cited in the literature.5 When paired with the appropriate rehabilitation treatment progression, the use of LR-PRP injections in the treatment of an isolated MCL tear appears to have been beneficial for this subject. In the elite professional athlete, return to participation 4 to 18 days sooner than expected, the cost effectiveness of LR-PRP injections could be significant when lost wages, lost ticket sales, lost advertising costs, lost merchandise sales, and the cost of prolonged treatment are considered. This is the second published case report to the authors’ knowledge examining the use of a series of three, evenly spaced, sequential injections.14 This is the first case report to outline the post-injection rehabilitation. The authors believe the expedited complete recovery of this subject back to high level sport activity was achieved due to several key treatment interventions. It is believed the use of LR-PRP, with laser therapy15-17 and immediate motion created an optimal environment for healing. In addition, early lower extremity muscle strengthening diminished muscle atrophy, and the use of hip/core control exercises in combination with proprioception and neuromuscular dynamic stabilization drills promoted dynamic joint stability.
Limitations of this case report include, a joint opening measurement, via ultrasound imaging, was not obtained pre or post-treatment to provide further objective evidence of benefit. A validated patient reported outcome questionnaire was not utilized to track progression through rehabilitation. Strength testing via handheld dynamometry was not conducted. A specific return to activity battery of tests such as Biodex testing, single leg press tests, and hop tests were not performed. Finally, this case report reflects a sample size of one and the results cannot be generalized.
CONCLUSION
The use of LR-PRP injections is becoming more common place in the orthopedic and sports medicine practice. In this case report, the use of three serial LR-PRP injections in combination with an early rehabilitation program was shown to be beneficial for the treatment of an isolated Grade 3 MCL injury. Optimal timing of LR-PRP injections, dosing, and long term efficacy remains in question as well as the optimal timing and dosing of the rehabilitation regimen. Future research utilizing LR-PRP should investigate and outline both the injection protocol as well as the rehabilitation protocol used.
REFERENCES
- 1.Roach CJ Haley CA Cameron KL Pallis M Svoboda SJ Owens BD., The epidemiology of medial collateral ligament sprains in young Athletes. Am J Sports Med. 2014;42(5):1103-1109. [DOI] [PubMed] [Google Scholar]
- 2.Shelbourne KD Patel DV, Management of Combined Injuries of the Anterior Cruciate and Medial Collateral Ligaments, Instruc Course Lect. 1996;45:275-280 [PubMed] [Google Scholar]
- 3.Grood ES, Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees., Bone Joint Surg. 1981;63(8):1257-1269. [PubMed] [Google Scholar]
- 4.Holden DL Eggert AW Butler JE. The nonoperative treatment of grade I and II medial collateral ligament injuries to the knee. Am J Sports Med. 1983;11:340-344. [DOI] [PubMed] [Google Scholar]
- 5.Kim C Chase PM Taylor DC, Return to play after medial collateral ligament injury, Clin Sports Med. 2016;35(4)679-696. [DOI] [PubMed] [Google Scholar]
- 6.Marchant Jr. MH Tibor LM Sekiya JK Hardaker Jr. WT Garrett Jr WE Taylor DC, Management of medial-sided knee injuries, part 1. Am J Sports Med 2011;39(5)1102-1112. [DOI] [PubMed] [Google Scholar]
- 7.Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dentistry. 2001;10:225-22. [DOI] [PubMed] [Google Scholar]
- 8.Toumi H Best T. The inflammatory response: friend or enemy for muscle injury? British J Sports Med. 2003;37:284-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blair P Flaumenhaft R. Platelet α-granules: basic biology and clinical correlates. Blood Reviews. 2009;23:177-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leslie M. Beyond clotting: the powers of platelets. Science. 2010;328:562-564. [DOI] [PubMed] [Google Scholar]
- 11.Leitner G Gruber R Neumüller J, et al. Platelet content and growth factor release in platelet–rich plasma: a comparison of four different systems. Vox sanguinis. 2006;91:135-13. [DOI] [PubMed] [Google Scholar]
- 12.LaPrade RF Geeslin AG Murray IR Musahl V Zlotnicki, Petrigliano F Mann BJ, Biologic treatments for sports Injuries II think tank-current concepts, future research, and barriers to advancement, part 1. biologics overview, ligament injury, tendionpathy, Am J Sports Med. 44(12):3270-3283. [DOI] [PubMed] [Google Scholar]
- 13.Frank C Woo SL Amiel D Harwood F Gomez M Akeson W, Medical collateral healing: a multidisciplinary assessment in rabbits, Am J Sports Med 1983;11(6)379-389. [DOI] [PubMed] [Google Scholar]
- 14.Eirale C Mauri E Hamilton B, Use of platelet rich plasma in an isolated complete medial collateral ligament lesion in a professional football (soccer) player: a case report Asian J Sports Med. 2013. 4(2):158-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allahverdi A Sharifi D Takhtfooladi MA Hesaraki S Khansari M Dorbeh S, Evaluation of low-level laser therapy, platelet-rich plasma, and their combination of achilles tendon in rabbits, Lasers Med Sci. 201. DOI:10.1007/s10103-015-1733-6. [DOI] [PubMed] [Google Scholar]
- 16.Reddy GK Stehno-Bittel L Enwemeka CS, Laser photostimulation of collagen production in healing rabbit achilles tendon, Lasers Surg Med. 1998;22:281-287. [DOI] [PubMed] [Google Scholar]
- 17.Tumilty ST Munn J McDonough S Hurley DA Basford JR Baxter D, Low level laser treatment of tendinopathy: a systematic review with meta-analysis. Photomed Laser Surg. 2010;28:3-16. [DOI] [PubMed] [Google Scholar]