Abstract
Purpose
To determine whether postpartum women (vaginal and Cesarean delivery) have deficits in trunk flexor strength, fatigability and steadiness, compared with nulligravid women, up to 26 weeks postpartum. We hypothesized that postpartum women would be weaker, more fatigable and have greater torque fluctuations than controls, with Cesarean delivery showing greater deficits than vaginal delivery.
Methods
22 control women (nulligravid) and 29 postpartum women (20-40 years, 19 who delivered via vaginal birth, 13 via Caesarian section) participated. Postpartum women were tested 8-10 and 24-26 weeks postpartum. Control women were tested 16-18 weeks apart. Maximal voluntary isometric contractions (MVC) were performed at multiple trunk positions with the trunk flexor muscles. To determine trunk flexor fatigability, subjects performed intermittent isometric contractions at 50% MVC (6-s contraction, 4-s rest) in upright sitting until task failure. An MVC was performed during the fatiguing task (one/min) and at 10 and 20 minutes of recovery.
Results
At 8 and 26 weeks, postpartum women (groups pooled) were weaker at all trunk angles (38% & 44% respectively, p<0.05) than controls despite no differences in handgrip strength. Postpartum women were more fatigable (71% & 52% respectively) and had greater torque fluctuations than controls (p<0.05). At 8 weeks postpartum, women who had a Cesarean delivery, were 59% more fatigable (p=0.004) than the vaginal-delivery group, with no difference between delivery types at 26 weeks postpartum.
Conclusions
Musculoskeletal recovery, including trunk flexor muscle strength and fatigability, is incomplete at 26 weeks postpartum. These findings provide a rationale for future studies to address outcomes of rehabilitation programs specifically targeted at improving strength and fatigability of the trunk flexor muscles after pregnancy and childbirth.
Keywords: abdominal muscles, muscle fatigue, steadiness, Cesarean delivery, vaginal delivery, women’s health
Introduction
Several physiological processes occur during pregnancy that impact the mother’s musculoskeletal system. The abdominal muscles experience substantial stretch and increased inter-recti distance (IRD) commonly occurs (1, 2). Hormones act on connective tissues throughout the mother’s body, resulting in joint laxity, particularly in the pelvis (3). The loss of passive lumbopelvic joint stabilization increases the importance and role of muscular stabilization, which is provided by the core muscles, including the abdominal muscles (4–6). Appropriate function of the abdominal muscles is critical for several life functions (5, 7). The ability to stabilize the pelvis against an external load was reported to be impaired during and after pregnancy (8). Despite the important daily and protective functions of the abdominal muscles, there is almost no understanding of the effects of pregnancy and mode of delivery on abdominal muscle function and recovery postpartum.
There are several other factors that may affect postpartum abdominal muscle function, including the mode of delivery and physical activity levels. Cesarean delivery involves profound disruption of the anterior abdominal wall and is associated with greater reports of postpartum pain and slower, more arduous recovery (9) than vaginal birth. Furthermore, physical activity, that can offset and protect against muscle dysfunction, is low for many mothers: approximately 60% of pregnant and 80% of postpartum women report a decline in their physical activity levels compared to pre-pregnancy activity (10). Given these factors and the reported changes in pain and recovery that suggest impairments in function of the core musculature in postpartum women, we investigated several aspects of abdominal muscle function including maximal strength at several trunk angles, fatigability, and force control (steadiness) during isometric trunk flexion.
Fatigability (often termed muscle fatigue) is an acute, activity-induced decline in the force or power of a muscle (11). It is often quantified as a reduction in the maximal force during or after a fatiguing task, but also can be quantified as the time to failure of a submaximal task (11). This metric of muscle function plays an important role in motor performance, injury prevention, and rehabilitation (11). However, fatigability of the abdominal muscles is rarely assessed clinically. Control of force, or steadiness of contraction, is also important for stabilization during movement and for limb muscles it is associated with functional tasks (12, 13). Steadiness is the ability to maintain a target force, and can be quantified as the fluctuations in force around a target force as the standard deviation (SD) of force or in relative terms as the coefficient of variation (CV) of force (14). In healthy men and nulligravid women, force fluctuations during trunk flexion contractions were 3-4 fold larger than that reported for limb muscles and were similar between the sexes (15). Whether this force control of the trunk flexor muscles is altered following childbirth, or impacted by mode of delivery, is unknown.
Currently, the musculoskeletal system is not assessed as part of standard care in pregnant or postpartum women (16–18), and musculoskeletal impairments are often dismissed as ‘normal’. Paid maternity leave in the United States, when available, is typically 6-8 weeks in duration (19) and often dictated by recovery of the smooth muscle of the uterus and perineal or surgical incision healing (16, 20). Thus, we assessed abdominal function in postpartum women at ~8 weeks postpartum, as well as at 26 weeks postpartum, to determine longer term recovery of the abdominal muscles.
The primary purpose of this study was to determine function of the abdominal muscles after vaginal and Cesarean delivery in postpartum women. The abdominal muscles are the primary movers during trunk flexion. Thus, maximal strength, fatigability and steadiness of the trunk flexor muscles in women 8-10 weeks and 24-26 weeks postpartum were compared with nulligravid controls. Given the large disruption to abdominal muscles during pregnancy and childbirth, particularly in women who delivered via Cesarean section, we hypothesized that 1) postpartum women (vaginal and Cesarean delivery pooled) would demonstrate significant deficits in maximal strength across a range of trunk angles, increased fatigability, and decreased steadiness of contraction of the trunk flexor muscles up to 26 weeks after delivery compared with healthy controls, and 2) women who underwent Cesarean delivery would have greater deficits in strength, fatigability, and steadiness than those who delivered vaginally. We also assessed the influence of physical activity on abdominal function in postpartum women. Thus, we compared the trunk flexor function between a subgroup of postpartum women at 8 weeks and control women who were matched for physical activity levels (estimated with accelerometer and questionnaire). We hypothesized that, even when matched for physical activity levels, postpartum women would demonstrate significant deficits in maximal strength, increased fatigability and less steady contractions compared with controls. As interpretive measures, we measured body composition, muscle thickness and inter-recti distance with ultrasonography, physical function, hand grip strength, and electromyography of the trunk flexor muscles during the fatiguing contraction.
Methods
Participants
All participants were females between 18 and 45 years old, not pregnant at the time of testing, free of chronic health conditions, did not smoke or use smokeless tobacco, had no known neurological impairment, did not take medications that impact neuromuscular excitability (including anti-depressants), and had no medical or orthopedic contraindications to exercise. Control women had never been pregnant. All participants provided written informed consent. This study was approved by the Institutional Review Boards at Marquette University and the Medical College of Wisconsin, and the Office of Clinical Research and Innovative Care Compliance at Froedtert Hospital.
Thirty-two postpartum women (vaginal delivery n=19, Cesarean delivery n=13) and 22 control women participated in the study. Some control women were also included in a previously published paper examining sex differences in trunk flexor function (15). Control women were also tested at two separate time points, separated by 16-18 weeks.
Variables and data sources/measurement
Trunk flexion torque
Maximal and submaximal trunk flexion torques were measured with a Biodex System 4 dynamometer (Biodex, Shirley, New York) using a Back Flexion-Extension attachment. Maximal voluntary isometric contractions (MVC) were assessed in six positions (upright sitting [0°]; 10°, 20°, 30°, and 40° of extension; 20°of flexion) to determine the strength of the trunk flexor muscles at different muscle lengths, in order to evaluate the impact of abdominal wall stretch during pregnancy on the torque-angle curve of the trunk flexor muscles following childbirth. Subjects were seated in the back flexion-extension attachment with the anterior superior iliac spine aligned with the axis of rotation of the device. The lower extremities and pelvis were secured with velcro straps, and two conjoined vertical straps on the anterior aspect of the shoulders restrained the trunk. Further details of device set up and subject positioning are described elsewhere (15). In brief, subjects performed trunk flexion, as if curling the shoulders toward the hips, without engaging the lower extremities. A study investigator (physical therapist) visually inspected all trunk flexion trials, and any trials with lower extremity involvement were excluded.
A minimum of three trials of MVCs were performed at each position, with 1 minute of rest between trials, until two trials were within 5% of each other. The maximum torque value was considered the MVC. Torque was recorded online using a Power 1401 A-D converter and Spike2 software [Cambridge Electronics Design (CED), Cambridge, UK]. Torque signals were digitized at 500 Hz and displayed on a monitor in front of the participant.
Hand Grip Strength
To determine the strength of a muscle group that is not typically affected by pregnancy and childbirth, and that is not dependent on the abdominal muscles or stability of the pelvic joints for function, bilateral handgrip strength was assessed as a control muscle group. Strength was measured with a JAMAR handgrip dynamometer (Patterson Medical, Warrenville, IL) with the arm positioned fully extended at the side. Three trials were performed bilaterally, and the highest value for each hand was used.
Fatigability
Fatigability of the trunk flexor muscles was assessed as the time to failure of an intermittent, submaximal isometric fatiguing task, and the reduction in MVC torque during the task. Subjects performed repeated trunk flexion contractions in upright sitting (0°) in the Biodex attachment at 50% MVC (target line displayed on a monitor) for 6 seconds, followed by 4 seconds of rest. A 6-second MVC was performed every minute (in lieu of 50% MVC), followed by 4 seconds of rest. Strong verbal encouragement was provided to continue until failure. Task failure was identified as torque <50% MVC for ≥ 3 seconds of the 6-second contraction or an MVC of <50% of baseline MVC. The fatiguing protocol always ended with an MVC. Recovery of maximal strength was assessed with an MVC at 10 minutes and 20 minutes after task failure.
Steadiness (Force Fluctuations)
Steadiness of the trunk flexor muscles was quantified as the coefficient of variation (CV) of torque during a 6-s isometric contraction at four contraction intensities (5, 10, 20, and 70% of MVC) while the participant sat upright (0°) in the Biodex attachment. The CV allows comparison of steadiness across target intensities or between individuals of varying strength levels. A target line was displayed on a monitor in front of the participant, who was cued to trace the line as steadily as possible for the 6 seconds. Two trials were performed at each intensity with adequate rest provided between trials. CV of torque [(standard deviation of torque/mean torque produced)*100] was calculated from the middle 3 s interval (1.5-4.5 s) of each 6 s trial, and the CV of the two trials at each intensity was averaged (14).
Steadiness was also assessed during the submaximal contractions (50% MVC) performed during the fatiguing exercise task; the middle 3 s interval was assessed from three submaximal contractions and averaged at the beginning and end of the fatiguing exercise task.
Electromyography (EMG)
EMG signals were recorded from the right rectus abdominis, left external oblique, and right rectus femoris using two 8-mm silver chloride surface recording electrodes (Coulbourn Instruments, Whitehall, PA) arranged in a bipolar configuration and with recommended placements (21). EMG signals were amplified (1000x) and band-pass (13-1000 Hz) and Notch (60 Hz) filtered (Coulbourn Instruments, Allentown, PA). Signals were recorded online using a Power 1401 A-D converter (CED) and were digitized at 2000 Hz. EMG signals for the rectus abdominis and external oblique during the submaximal contractions of the fatiguing exercise protocol were normalized to the maximum RMS EMG of each respective muscle recorded during baseline trunk flexion MVCs. EMG signals for the rectus femoris muscle during the submaximal trunk flexion contractions during the fatiguing protocol were normalized to the maximum RMS EMG of the rectus femoris recorded during knee extension MVCs (obtained with a strap around the shank of the right lower extremity) prior to the fatiguing protocol of the trunk flexor muscles.
Inter-recti distance (IRD) and rectus abdominis muscle thickness
Real-time ultrasound (GE Vivide; 8 LRS linear probe) was used to assess IRD and thickness of the rectus abdominis muscles while the participant was supine. Measurement of IRD was made 4 cm below the umbilicus, because increased IRD below the umbilicus is usually more severe than increased IRD above the umbilicus (1). Muscle thickness measurements of the right rectus abdominis were taken 2.5 cm above and below the umbilicus.
Physical activity
Physical activity levels were quantified with accelerometry and questionnaire. Physical activity during a 4-day time period at each time point of testing was quantified with ActiGraph accelerometers (ActiGraph Corp, Pensacola, Florida) worn around the waist. Average minutes/day of moderate intensity exercise was quantified using ActiLife analysis software (ActiGraph). Self-reported physical activity was also estimated with a questionnaire, which estimated the metabolic cost (METs) and the weekly metabolic equivalents (MET∙hour∙week−1) of activities performed over the previous year (22).
Body composition
Dual x-ray absorptiometry (DXA) was used to estimate fat mass (GE Lunar Idxa, GE Healthcare, Little Chalfont, United Kingdom).
Functional mobility
The six-minute walk test (23) was performed on an indoor course to quantify the maximal walk distance in six minutes.
Statistical methods
Differences between groups (postpartum and control) were determined for subject characteristics, pre-exercise MVC torque, IRD, and time-to-task failure (fatigability) using independent samples t-tests. Differences between groups for torque-angle curve, recovery of MVC torque following fatiguing exercise, EMG during fatiguing exercise, CV of the force fluctuations (steadiness) at multiple contraction intensities, and steadiness during fatiguing exercise were assessed using repeated measures analysis of variance (ANOVA) with group as a between-subjects factor. Impact of method of delivery (Cesarean vs vaginal) was assessed for subject characteristics, pre-exercise MVC torque, IRD, and time-to-task failure (fatigability) using independent samples t-tests. Differences between delivery types for torque-angle curve, recovery of MVC torque following fatiguing exercise, EMG during fatiguing exercise, CV of the force fluctuations (steadiness) at multiple contraction intensities, and steadiness during fatiguing exercise were assessed using repeated measures analysis of variance (ANOVA) with delivery type as a between-subjects factor.
A subgroup of participants were matched for physical activity at the initial time point (8 weeks postpartum) using both questionnaire and accelerometer estimations of physical activity levels. Differences between activity-matched controls and postpartum women were determined with similar methods to between group (postpartum and control) differences. Physical activity matching was not possible at the follow up time point (26 weeks postpartum) due to very low numbers of activity matched individuals, resulting in insufficient statistical power.
Pearson correlation was used to examine relationships between scale level variables that demonstrated a linear relationship. Spearman correlation was used to examine relationships between variables that had a curvilinear relationship and/or were ordinal level data. Significance was set as p<0.05. Missing data was excluded analysis by analysis. Statistical analyses were performed with SPSS version 24 software (IBM, Armonk, NY, USA).
Results
Participants
Twenty-nine postpartum women (Vaginal delivery n=18, Cesarean delivery n=11) and 15 control women completed initial (8-10 weeks postpartum) testing. Twenty-eight postpartum women (Vaginal delivery n=17, Cesarean delivery n=11) and 14 control women completed testing at follow up (24-26 weeks postpartum). Eight control women and 26 postpartum women (Vaginal delivery n=17, Cesarean delivery n=9) had complete data sets at both time points. Loss of follow up for seven control women and two women from the Cesarean group was due to schedule conflicts. One woman from the vaginal group did not complete follow up testing due to another pregnancy. Two women from the Cesarean group completed testing only at 24-26 weeks postpartum.
At the initial time point (8 weeks postpartum), 9 control women and 9 postpartum women were matched for physical activity levels.
Descriptive data
Group characteristics, including body composition, handgrip strength, muscle thickness, distance walked in six minutes, and physical activity, are presented for controls vs postpartum women in Table 1 and vaginal delivery vs Cesarean delivery in Table 2. Postpartum women were older, weighed more, had greater body fat, and were less physically active than controls at both time points (p<0.05). Hand grip strength was similar between control and postpartum women at both time points (p>0.05). There were no differences in age, number of pregnancies, body composition, hand grip strength, or physical activity between delivery types at either 8 weeks or 26 weeks postpartum (p>0.05).
Table 1.
Subject characteristics: Control vs Postpartum.
| Variable | INITIAL (8wks Postpartum) | FOLLOW UP (26 wks Postpartum) | ||
|---|---|---|---|---|
| Control (n=15) | Postpartum (n=29) | Control (n=14) | Postpartum (n=28) | |
| Age (years) | 25.5 ± 5.3 | 31.4 ± 5.2* | 25.8 ± 6.1 | 32.0 ± 5.1* |
| Weight (kg) | 63.6 ± 12.7 | 74.4 ± 13.4* | 62.7 ± 7.8 | 71.4 ± 14.0* |
| Height (cm) | 166.6 ± 7.1 | 164.1 ± 4.6 | 166.9 ± 8.4 | 164.1 ± 4.8 |
| BMI (kg/m2) | 22.7 ± 3.8 | 27.6 ± 5.0* | 22.4 ± 1.8 | 26.9 ± 5.1* |
| Body Fat (%) | 31.0 ± 5.4 | 38.5 ± 6.9* | 31.8 ± 4.6 | 36.7 ± 8.4* |
| Thickness of right rectus abdominis muscle belly (2.5 cm above umbilicus) (cm) | 1.0 ± 0.2 | 0.8 ± 0.2* | 1.0 ± 0.1 (n=13) | 0.8 ± 0.2* |
| Thickness of right rectus abdominis muscle belly (2.5 cm below umbilicus) (cm) | 1.0 ± 0.2 | 0.8 ± 0.2* | 0.9 ± 0.1 (n=13) | 0.8 ± 0.2 |
| Average minutes/day of moderate intensity physical activity | 47.8 ± 23.4 (n=9) | 18.8 ± 18.8* (n=20) | 31.2 ± 14.0 (n=7) | 16.7 ± 10.5* (n=13) |
| Self-reported physical activity over the previous 12 months (MET·hours·week−1) | 43.0 ± 28.3 (n=14) | 22.2 ± 19.2* (n=27) | 34.0 ± 25.1 | 14.9 ± 17.3* (n=25) |
| Distance walked in 6 minutes (m) | 686.2 ± 58.7 | 640.0 ± 64.8* | 693.3 ± 58.2 | 652.7 ± 65.1 |
| Hand grip maximal strength, right hand (kg) | 33.4 ± 6.7 | 33.1 ± 5.9 | 34.2 ± 5.3 | 34.1 ± 6.5 (n=27) |
| Hand grip maximal strength, left hand (kg) | 31.4 ± 5.9 | 31.1 ± 4.9 | 30.8 ± 4.5 | 32.3 ± 5.6 (n=27) |
| Change in MVC torque at end of fatiguing exercise protocol (% MVC) | -26.2 ± 15.9 | -14.6 ± 32.4 | -30.0 ± 13.4 | -24.0 ± 18.8 |
| External Oblique EMG at beginning of fatigue task (%MVC) | 48.3 ± 33.7 | 54.2 ± 23.9 | 46.6 ± 16.4 | 50.3 ± 23.0 |
| External Oblique EMG at end of fatigue task (%MVC) | 50.2 ± 32.5 | 60.6 ± 20.8 | 56.6 ± 17.4 | 56.2 ± 23.0 |
| Rectus Femoris EMG at beginning of fatigue task (%MVC) | 12.8 ± 27.6 | 4.5 ± 2.4 | 4.7 ± 3.7 | 6.4 ± 6.0 |
| Rectus Femoris EMG at end of fatigue task (%MVC) | 12.4 ± 26.9 | 4.5 ± 2.4 | 4.8 ± 3.8 | 6.5 ± 6.0 |
Indicates p<0.05. kg=kilograms; cm=centimeters; m=meters; MET=metabolic equivalents; MVC=maximal voluntary contraction
Table 2.
Subject Characteristics: Vaginal vs Cesarean Delivery
| Variable | 8 weeks Postpartum | 26 weeks postpartum | ||
|---|---|---|---|---|
| Vaginal (n=18) | Cesarean (n=11) | Vaginal (n=17) | Cesarean (n=11) | |
| Age (years) | 30.6 ± 6.0 | 32.8 ± 3.5 | 31.4 ± 5.8 | 33.0 ± 4.0 |
| Weeks postpartum | 9.4 ± 1.1 | 9.3 ± 0.5 | 26.1 ± 1.6 | 26.2 ± 0.6 |
| Total Number of Pregnancies | 2.1 ± 1.2 (n=17) | 3.0 ± 1.9 (n=10) | 2.1 ± 1.1 (n=15) | 3.0 ± 2.1 (n=9) |
| Duration of Most Recent Pregnancy (weeks) | 39.3 ± 1.0 (n=14) | 38.1 ± 1.2* (n=10) | 39.3 ± 1.0 (n=12) | 38.3 ± 1.4 (n=9) |
| Weight (kg) | 74.3 ± 14.4 | 74.2 ± 12.2 | 70.9 ± 15.3 | 72.4 ± 12.4 |
| Height (cm) | 164.6 ± 4.3 | 163.1 ± 5.3 | 165.1 ± 4.8 | 162.6 ± 4.8 |
| BMI (kg/m2) | 27.5 ± 5.4 | 27.8 ± 4.3 | 26.4 ± 5.6 | 27.5 ± 4.3 |
| Body Fat % | 39.0 ± 7.0 | 37.7 ± 7.0 | 36.1 ± 8.8 | 37.7 ± 8.2 |
| Thickness of right rectus abdominis muscle belly (2.5 cm above umbilicus) (cm) | 0.8 ± 0.2 | 0.8 ± 0.1 | 0.8 ± 0.2 | 0.8 ± 0.1 |
| Thickness of right rectus abdominis muscle belly (2.5 cm below umbilicus) (cm) | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.8 ± 0.3 | 0.8 ± 0.2 |
| Average minutes/day of moderate intensity physical activity | 17.1 ± 19.1 (n=10) | 20.4 ± 19.4 (n=10) | 16.8 ± 11.2 (n=10) | 13.1 ± 4.9 (n=3) |
| Self-reported physical activity over the previous 12 months (MET·hours·week−1) | 22.0 ± 16.3 (n=17) | 22.6 ± 24.3 (n=10) | 15.4 ± 20.8 (n=15) | 14.3 ± 11.3 (n=10) |
| Distance walked in 6 minutes (m) | 645.0 ± 62.0 | 631.8 ± 71.3 | 663.4 ± 60.8 | 636.1 ± 70.9 |
| Hand grip maximal strength, right hand (kg) | 33.4 ± 5.9 | 32.5 ± 6.1 | 34.9 ± 6.5 | 32.7 ± 6.6 (n=10) |
| Hand grip maximal strength, left hand (kg) | 31.7 ± 5.2 | 30.2 ± 4.6 | 33.2 ± 5.9 | 30.7 ± 4.9 (n=10) |
| Change in MVC torque at end of fatiguing exercise protocol (% MVC) | −12.0 ± 27.4 (n=16) | −18.4 ± 39.7 | −22.9 ± 21.0 | −25.8 ± 15.4 |
| External Oblique EMG at beginning of fatigue task (%MVC) | 52.2 ± 26.7 (n=14) | 57.4 ± 19.7 (n=9) | 46.8 ± 22.6 | 55.7 ± 23.7 |
| External Oblique EMG at end of fatigue task (%MVC) | 59.4 ± 23.5 (n=14) | 62.3 ± 16.9 (n=9) | 49.2 ± 16.8 | 67.0 ± 27.6 |
| Rectus Femoris EMG at beginning of fatigue task (%MVC) | 4.3 ± 2.1 (n=14) | 4.8 ± 2.9 (n=9) | 5.9 ± 5.1 | 7.3 ± 7.4 |
| Rectus Femoris EMG at end of fatigue task (%MVC) | 4.3 ± 2.1 (n=14) | 4.9 ± 2.9 (n=9) | 6.0 ± 5.2 | 7.3 ± 7.4 |
Indicates p<0.05. kg=kilograms; cm=centimeters; m=meters; MET=metabolic equivalents; MVC=maximal voluntary contraction
Maximal Torque Across Different Positions (Torque-Angle Curve)
Postpartum women were weaker than controls across all trunk positions at 8 weeks (39.6 ± 22.6 Nm vs 65.8 ± 29.2 Nm, respectively, p<0.001; Figure 1A) and 26 weeks (36.5 ± 19.8 Nm vs 54.3 ± 24.2 Nm, p=0.001; Figure 1B) postpartum. The shape of the torque-angle curve was similar between groups at both time points (8 weeks: position × group, p=0.927; 26 weeks: position × group, p=0.766), with both control and postpartum women generating greatest trunk flexion MVC torque at 40 degrees of extension (effect of position, p<0.001 at both time points).
Figure 1. Torque-Angle Curve.

Torque-angle curve for the trunk flexor muscles at the initial and follow up time points for postpartum vs control [A & B] and vaginal vs Cesarean delivery [C & D]. Negative numbers indicate positions of trunk extension, upright sitting is 0°, and positive numbers indicate positions of trunk flexion. Postpartum women had lower maximal trunk flexion torque across all positions at both time points compared to control. However, the torque-angle curve shape was similar for all groups. There were no differences between delivery types (vaginal vs Cesarean). *= group difference at the time point (postpartum vs control).
Mode of Delivery
There was no difference in the torque-angle curve between delivery types at 8 weeks (position: p<0.001; position × delivery type: p=0.169; delivery type: p=0.058; Figure 1C) or 26 weeks (position: p<0.001, position × delivery type: p=0.964, delivery type: p=0.485; Figure 1D).
Comparison across matched activity levels
Despite being matched for physical activity levels, postpartum women demonstrated decreased torque production compared to controls at all trunk positions (p=0.002). The shape of the torque-angle curve was similar for both groups (position: p=0.001, position × group: p=0.826).
Fatigability
Time to Task Failure
Postpartum women had a shorter time to task failure (i.e. greater fatigability) than control women at 8 weeks postpartum (189 ± 156 s vs 644 ± 327 s, respectively; p<0.001; Figure 2A). By 26 weeks, postpartum women demonstrated longer time-to-task failure (i.e. improved fatigability) vs 8 weeks postpartum (p=0.015), but were still more fatigable than control women (288 ± 167 s vs 605 ± 396 s; group, p=0.011; Figure 2B).
Figure 2. Fatigability and Recovery.

A-B: Time-to-task failure for the intermittent isometric submaximal trunk flexion fatiguing exercise at time points for postpartum (pooled), control, vaginal delivery, and cesarean delivery at 8-10 weeks postpartum [A] and 24-26 weeks postpartum[B]. *=group difference at the time point (postpartum vs control); γ=improvement compared to initial timepoint; #=delivery group difference at the time point (vaginal vs Cesarean). C-D: MVC torque before (baseline), immediately after (task failure, TF), and 10 minutes (R10) and 20 minutes (R20) after fatiguing trunk flexor exercise for controls vs postpartum women at 8-10 weeks [C] and 24-26 weeks [D]. Postpartum women generate lower maximal torque than control women at all time points. Postpartum women demonstrate impaired recovery of MVC strength up to 10 weeks postpartum [C], but show a similar recovery pattern to control women at 26 weeks postpartum [D]. *=group difference at the time point (postpartum vs control); δ=different from baseline MVC. E-F: No statistical difference is present between modes of delivery at either time point [E & F]. Postpartum women demonstrate a decline in baseline MVC strength from 8-26 weeks, driven by a loss of strength for women in the vaginal delivery group. δ=different from baseline MVC.
Mode of Delivery
At 8 weeks postpartum, the Cesarean delivery group demonstrated a shorter time-to-task failure (greater fatigability) than the vaginal delivery group (99 ± 58 s vs 244 ± 173 s; p=0.004; Figure 2A). By 26 weeks postpartum, there was no difference in time-to-task failure between delivery groups (262 ± 168 s vs 304 ± 169 s; p=0.523; Figure 2B). The vaginal delivery group showed no change in time-to-task failure from 8 to 26 weeks (p=0.306), but the Cesarean delivery group demonstrated improvement in time-to-task failure (p=0.005).
Comparison across matched activity levels
In this subgroup, the postpartum women continued to demonstrate increased trunk flexor fatigability compared with controls (195.2 ± 183.7 s vs 618.7 ± 332.1 s, respectively; p=0.004; Table 3).
Table 3.
Physical Activity Matched Participants at Initial Time Point (8 weeks postpartum)
| Variable | Control (n=9) | Postpartum (n=9) |
|---|---|---|
| Age (years) | 23.3 ± 1.8 | 31.6 ± 4.9* |
| Weight (kg) | 63.9 ± 10.5 | 70.0 ± 12.3 |
| Body Fat % | 29.9 ± 4.3 | 36.7 ± 6.7* |
| BMI (kg/m2) | 22.5 ± 1.5 | 26.2 ± 5.1 |
| Rectus Abdominis muscle thickness (above umbilicus) (cm) | 1.1 ± 0.2 | 0.8 ± 0.2* |
| Rectus Abdominis muscle thickness (below umbilicus) (cm) | 1.1 ± 0.1 | 0.7 ± 0.2* |
| Sedentary time (average minutes/day) | 531.0 ± 118.9 | 494.8 ± 80.1 |
| Light physical activity (average minutes/day) | 240.0 ± 34.2 | 276.5 ± 52.4 |
| Moderate physical activity (average minutes/day) | 50.5 ± 25.9 | 24.3 ± 29.3 |
| Vigorous physical activity (average minutes/day) | 13.9 ± 7.0 | 7.5 ± 9.2 |
| Average Steps/day | 11509.0 ± 2850.5 | 6649.5 ± 4292.4 |
| Distance walked in six minutes (m) | 697.0 ± 39.9 | 657.6 ± 78.9 |
| Self-reported physical activity over the previous 12 months (MET·hours·week−1) | 57.3 ± 25.1 | 45.4 ± 13.5 |
| Time-to-task failure on the intermittent, isometric trunk flexion fatiguing exercise protocol (s) | 618.7 ± 332.1 | 195.2 ± 183.7* |
| Pre-exercise MVC (Nm) | 55.5 ± 28.9 | 26.9 ± 14.2* |
| CV of torque at beginning of fatigue task (%) | 5.2 ± 2.0% | 11.9 ± 6.6%* |
| CV of torque at end of fatigue task (%) | 8.4 ± 4.1 | 12.3 ± 4.5%* |
Indicates p<0.05. kg=kilograms; cm=centimeters; m=meters; MET=metabolic equivalents; MVC=maximal voluntary contraction; Nm= Newton meters
Maximal Trunk Flexion Torque Before and After the Fatiguing Task
Trunk flexion MVC torque was less for the postpartum women than control women at both 8 weeks (28.6 ± 12 Nm vs 46.5 ± 26.1 Nm; p=0.022; Figure 2C) and 26 weeks postpartum (24.6 ± 10.1 Nm vs 44.1 ± 16.6 Nm; p=0.001; Figure 2D).
At task failure, the postpartum and control women had a similar reduction in MVC torque, at both the 8-week and 26-week time points (Table 1). At 8 weeks, the MVC torque of postpartum women was below pre-exercise MVC at 20 minutes following fatiguing exercise, while the MVC torque of control women had recovered by 10 minutes post-exercise (time, p<0.001; time × group, p<0.001; group, p=0.001; Figure 2C). At 26 weeks, postpartum women demonstrated a recovery (increase) of MVC torque post-exercise that was similar to control women, though postpartum women demonstrated lower MVC torque than control women at all time points before and after exercise (time, p<0.001; time × Group, p=0.463; group, p<0.001; Figure 2D).
Mode of Delivery
There were no differences between vaginal and Cesarean delivery for pre-exercise MVC strength at 8 weeks (31.4 ± 13.0 Nm vs 24.0 ± 8.8 Nm, respectively, p=0.106, Figure 2E) nor at 26 weeks (24.9 ± 11.4 Nm vs 24.3 ± 8.1 Nm, respectively, p=0.886, Figure 2F). There was also no difference in MVC torque recovery following fatiguing exercise at 8 weeks (time, p=0.775; time × delivery type, p=0.592; delivery type, p=0.829; Figure 2E) and 26 weeks (time, p=0.006; time × delivery type, p=0.163; delivery type, p=0.386; Figure 2F).
Comparison across matched activity levels
In the subgroup of physical activity-matched women, postpartum women continued to demonstrate decreased trunk flexor strength compared to control women at 8 weeks postpartum (26.9 ± 14.2 Nm vs 55.5 ± 28.9 Nm, respectively; p=0.021; Table 3). Despite being matched for physical activity levels, postpartum women continued to demonstrate impaired recovery of MVC strength following fatiguing exercise (time, p=0.027; time × group, p=0.019; group, p=0.013), with MVC strength at 20 minutes post-exercise still below baseline MVC.
Steadiness of contraction at 5, 10, 20, and 70% of MVC
At 8 weeks postpartum, the CV of torque at four intensities was quantified for 22 postpartum women and 13 control women. CV of torque decreased as contraction intensity increased for both postpartum and control women (intensity, p<0.001; intensity × group, p=0.068; Figure 3A). Postpartum women however, had larger CV of torque than controls (group, p=0.013), particularly at low contraction intensities. At 26 weeks postpartum, CV of torque was obtained for 25 postpartum women and 15 control women. As was seen at initial testing (8 week postpartum), CV of torque decreased as contraction intensity increased for both groups (intensity, p<0.001; intensity × group, p=0.219; Figure 3B). Postpartum women continued to have larger CV of torque than controls at 26 postpartum (group, p=0.039), with the greatest difference between groups at low contraction intensities.
Figure 3. Steadiness.
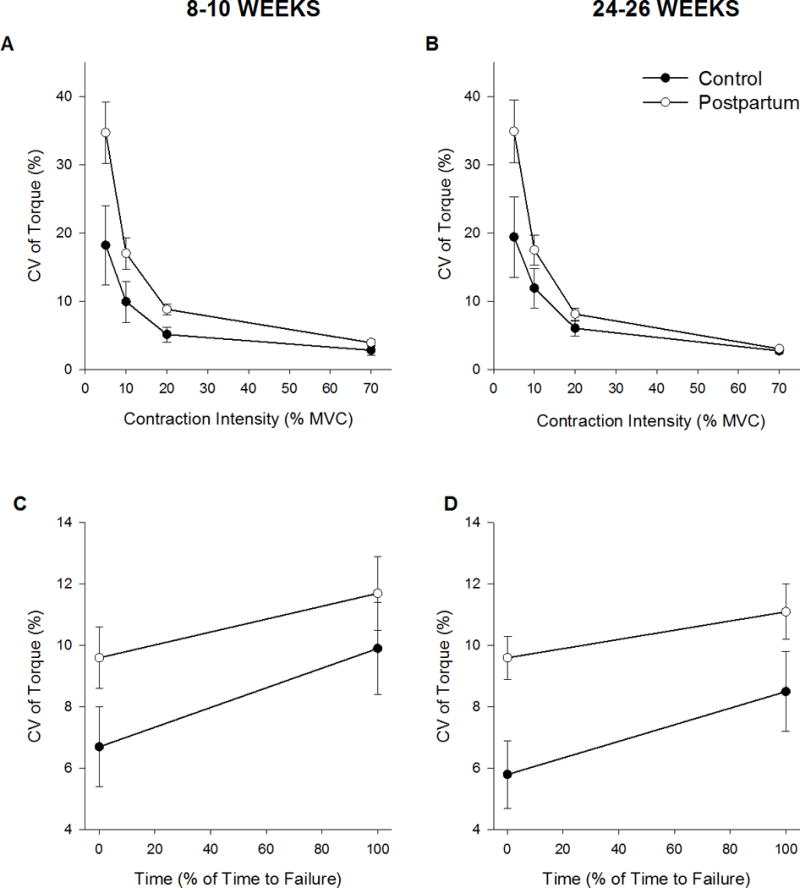
A-B: Steadiness (CV of torque) of trunk flexor contractions at four intensities (5, 10, 20, & 70% MVC) for control vs postpartum women at 8-10 weeks [A] and 24-26 weeks [B] postpartum. Postpartum women have greater torque fluctuations than controls at both time points, particularly at low contraction intensities. *=group difference at the time point (postpartum vs control). C-D: CV of torque during submaximal (50% MVC) contractions during fatiguing exercise is represented for controls vs postpartum women at 8-10 weeks [C] and 24-26 weeks [D]. Both groups demonstrated increased force fluctuations from the beginning to end of fatiguing exercise at both time points. CV of torque is similar between groups at 8-10 weeks postpartum [C], but postpartum women have greater fluctuations in torque than controls at 24-26 weeks postpartum [D]. *=group difference at the time point (postpartum vs control).
Comparison across matched activity levels
CV of torque at four intensities was quantified for 8 control and 8 postpartum women who were matched for physical activity levels. CV of torque decreased as contraction intensity increased (intensity p<0.001). Postpartum women had greater fluctuations in torque than controls (group, p=0.020) despite being matched for physical activity levels. However, the decrease in CV with higher contraction intensity was greater in postpartum women than controls (intensity × group, p=0.049) because postpartum women had a significantly higher CV at 5% MVC but not the higher contraction intensities.
Method of Delivery
At 8 weeks postpartum, CV was quantified at four intensities for 13 women who had a vaginal delivery and nine women who delivered via Cesarean section. CV of torque decreased as intensity increased for both delivery types (intensity p<0.001, intensity × delivery type p=0.202). CV of torque was similar between delivery types (delivery type p=0.846). At 26 weeks postpartum (n = 15 vaginal delivery, n = 10 Cesarean delivery), the CV of torque decreased as contraction intensity increased (intensity, p<0.001; intensity × delivery type, p=0.206) but was similar between delivery types (delivery type, p=0.637).
Steadiness of contraction during fatiguing exercise
CV of torque during the fatiguing exercise protocol (50% MVC) was quantified at the initial time point (8 weeks postpartum) in 15 control women and 23 postpartum women. CV of torque increased similarly across time for both control and postpartum women (time, p<0.001; time × group, p=0.316; Figure 3C) with no group differences (group, p=0.180). At the follow up time point (26 weeks postpartum), 14 control women and 28 postpartum women were included in analysis. CV of torque increased across time for both groups (time, p<0.001; time × group, p=0.122; Figure 3D), but postpartum women were less steady (large CV of torque) than control women (group, p=0.026).
Comparison across matched activity levels
CV of torque during the fatiguing task (n = 9 control, n = 6 postpartum women) increased with time for both groups (time, p=0.036; time × group, p=0.088). Despite being matched for physical activity levels, postpartum women were less steady (larger CV of torque) than controls (group, p=0.028) at the beginning of the fatiguing task (11.9 ± 6.6% Vs 5.2 ± 2.0%, respectively) and the end of the fatiguing task (12.3 ± 4.5% Vs 8.4 ± 4.1%, respectively) (Table 3).
Method of Delivery
At 8 weeks postpartum, 14 women who delivered vaginally and 9 women who delivered via Cesarean section were included in analysis. CV of torque increased across time (time, p=0.001), with women who underwent Cesarean delivery demonstrating a greater increase in CV of torque across time (time × delivery type, p=0.032). CV of torque was similar between delivery types (delivery type, p=0.146).
At 26 weeks postpartum (n = 17 vaginal delivery and n = 11 Cesarean delivery), CV of torque increased across time for both delivery types (time p<0.001; time × delivery type, p=0.929) and was similar between delivery types (delivery type, p=0.511).
EMG during fatiguing exercise (%MVC)
EMG activity (%MVC) of the external oblique and rectus abdominis increased over time for both postpartum and control women (external oblique: time, p=0.025; time × group, p=0.229; rectus abdominis: time, p=0.037; time × group, p=0.283) with both groups demonstrating similar activation of both muscles at the initial time point ie 8 weeks postpartum (group, p=0.361 for external oblique, p=0.380 for rectus abdominis; Table 1).
At the follow up time point (26 weeks postpartum), external oblique EMG increased over time for both groups (time, p=0.003, time × group, p=0.409), with no difference in relative EMG between control and postpartum women (group p=0.800; Table 1). Rectus abdominis EMG did not change over time for either group (time, p=0.138, time × group, p=0.231), and relative rectus abdominis EMG was similar between control and postpartum women (group p=0.188).
At both time points (8 & 26 weeks postpartum), rectus femoris EMG did not change across time during the fatiguing task in the control or postpartum women (8 weeks: time p=0.351, time × group p=0.376; 26 weeks: time p=0.410, time × group p=0.725), and both groups demonstrated similar rectus femoris activation (8 weeks: group p=0.164; 26 weeks: group p=0.328; Table 1).
Method of delivery
At both time points (8 and 26 weeks postpartum) there were no differences in relative EMG between vaginal and Cesarean delivery groups for any muscle groups tested (time × group, p>0.05, group, p>0.05 for all muscles).
Inter-recti distance
Postpartum women demonstrated greater IRD 4 cm below the umbilicus than controls at 8 weeks (1.4 ± 1.1 cm vs 0.4 ± 0.2 cm, p<0.001) and 26 weeks (1.3 ± 1.1 cm vs 0.3 ± 0.2 cm, p<0.001).
Comparison across matched activity levels
Postpartum women demonstrated greater IRD than activity-matched controls (1.2 ± 0.8 cm vs 0.4 ± 0.2 cm, respectively; p=0.019; Table 3).
Mode of delivery
There was no difference in IRD between vaginal and Cesarean delivery types at 8 weeks (1.2 ± 1.1 cm vs 1.8 ± 1.2 cm, respectively, p=0.271) or 26 weeks (1.2 ± 1.0 cm vs 1.5 ± 1.3 cm, respectively, p=0.431).
Associations (postpartum and control)
Trunk flexor MVC torque was associated with fatigability (8 weeks: r=0.602, p<0.001 & 26 weeks: r=0.415, p=0.006), thickness of the rectus abdominis muscle belly 2.5 cm above the umbilicus (8 weeks: r=0.311, p=0.040 & 26 weeks: r=0.388, p=0.012), self-reported physical activity (8 weeks: r=0.430, p=0.005) and the six-minute walk (8 weeks: r=0.306, p=0.044 and 26 weeks: r=0.449, p=0.003). Thus, stronger women had a longer time-to-task failure, greater rectus abdominis thickness, were more active, and walked further in six minutes.
Fatigability was associated with IRD (8 weeks: rs=−0.548, p<0.001 & 26 weeks: rs=−0.484, p=0.002), such that women with greater IRD were more fatigable.
Discussion
The novel findings are that the trunk flexor muscles of postpartum women were weaker, more fatigable, and demonstrated greater fluctuations in torque during isometric contractions than nulligravid women (controls), and that these impairments in trunk flexor muscle function persisted at 6 months (26 weeks) after childbirth. The strength deficits do not appear to impact muscle groups throughout the body, because there was no difference in hand grip strength between controls and postpartum women. Fatigability of the trunk flexor muscles was greater in postpartum women at 8 weeks postpartum, even when matched with the control women for physical activity levels. Furthermore, mode of delivery impacted abdominal muscle function: women whom had a Cesarean delivery were more fatigable, and had a greater increase in force fluctuations during the fatiguing trunk flexor exercise, at 8 weeks postpartum compared with women who delivered vaginally. Greater trunk flexor strength was associated with lower fatigability and greater functional mobility. Thus, trunk flexor muscle function was substantially lower in postpartum women than healthy controls, with limited recovery by 6 months.
This is the first study to establish that postpartum women demonstrate impaired strength, fatigability, and torque steadiness of core muscles, which are important to many daily activities, even at 6 months postpartum. The strength deficits in postpartum women, relative to controls, were 38% at 8 weeks, and 44% at 26 weeks; long past when women have returned to work (~8 weeks postpartum). The strength deficits occurred at all trunk angles, so that the stretch experienced by the abdominal muscles during pregnancy did not alter the torque angle curve. The highest torque occurred at the −40° position for both postpartum and control women, a position close to full extension as occurs in upright standing and where the abdominal muscle fibers must be close to the optimal overlap of actin and myosin in the sarcomere and optimal force production (24). Furthermore, strength deficits in postpartum women in this study were localized to the trunk flexor muscles because the handgrip strength of the postpartum and control women was similar.
Postpartum women (both vaginal and Caesarean delivery groups) were also more fatigable (shorter time to task failure) than controls by 71% at 8 weeks and by 52% at 26 weeks postpartum. Another metric of fatigability was the reduction in the MVC which occurred more rapidly for the postpartum women than the control women during the fatiguing task: the reduction in MVC torque was similar between groups, but the time to failure was considerably briefer in the postpartum women than controls Furthermore, at 20 mins of recovery from the fatiguing task at 8 weeks after delivery, the MVC differed between groups, with postpartum women demonstrating impaired recovery of maximal strength. In contrast, control women had returned to baseline strength 10 minutes after exercise. This prolonged reduction in maximal strength may increase risk of injury when performing repetitive tasks, such as lifting and carrying.
Method of delivery was a contributing factor to the increased fatigability of postpartum women at 8 weeks after delivery, with a briefer time to failure for the Cesarean delivery group compared with vaginal delivery (Figure 2A). The recovery of the MVC torque did not differ with delivery mode. These results are in part consistent with our hypothesis and support that the surgical damage to the abdominal muscles and the surrounding fascia slow recovery of abdominal muscle function, particularly for activities involving repeated contractions and fatiguing exercise. Fatigability was also greater in women matched for physical activity levels indicating that the abdominal muscle endurance was still lower independent of physical activity.
Fatigability did not differ with delivery mode by 26 weeks because the women who had undergone Cesarean delivery had improved abdominal muscle endurance to similar levels as the vaginal delivery group. In another study, women who had a Cesarean delivery reported a more difficult postpartum recovery than women who delivered vaginally, along with greater pain reports in the immediate postpartum period (37). We showed here that trunk flexor strength did not differ at 8 weeks postpartum between Cesarean and vaginal delivery, so fatigability may be a more sensitive test of abdominal muscle recovery, at least at 8 weeks postpartum. No differences exist, however, in the length of paid maternity leave based on delivery method (3). This research suggests that women who undergo Cesarean delivery require a longer period of time to recover from the musculoskeletal deficits experienced from pregnancy and childbirth than women who experience a vaginal delivery. Given our findings and the severe deficits in abdominal function of postpartum women in general, it appears all postpartum women, regardless of delivery method, would benefit from rehabilitative interventions; however, this rehabilitation may be even more crucial in the immediate postpartum period for women who deliver by Cesarean section.
Electromyographic (EMG) activity (% MVC) of the trunk flexor muscles was similar throughout the fatiguing contraction between postpartum and control women, suggesting similar muscle activation between groups. Similarly, EMG was not different between vaginal and Cesarean delivery during the fatiguing contraction. Rectus femoris activation was low for all groups (4-13%) and did not change during the fatiguing exercise task, indicating that the rectus femoris was not contributing to the observed trunk flexion torque or compensating during the fatiguing contraction. Activation of the abdominal muscles (rectus abdominis and external oblique) increased from the beginning to the end of the fatiguing exercise bout, which is expected, and likely represents an increase in motor unit recruitment and altered discharge rates as the active muscle fibers become fatigued (25, 26). Despite the shorter time to failure of the postpartum women, the relative muscle activity at task failure was similar to controls, and EMG was similar between delivery types. These results suggest that, for the rectus abdominis and external oblique muscles, the activation of the motor neuron pool in postpartum women was similar to controls at task end. Hence, impaired muscle activation probably did not contribute significantly to the difference in fatigability between the postpartum and control women. Alternatively, muscular mechanisms likely played a greater role than neural mechanisms for the increased fatigability of the postpartum women in this study, although this requires confirmation.
Postpartum women also demonstrated larger fluctuations in trunk flexor torque (lower steadiness) than control women, with women who underwent Cesarean delivery exhibiting a greater increase in force fluctuations during fatiguing exercise than women who delivered vaginally. Steadiness can be impacted by several factors, including common drive to the motor neuron pool (14, 27, 28), physical activity (14), and stress (29). The trunk flexor muscles are innervated by multiple spinal levels (4), which may contribute to higher force fluctuations during trunk flexion contractions than those observed in limb muscles, as has been shown in healthy men and nulligravid women (15). Low physical activity levels during and after pregnancy (10) may also impact force steadiness in this population; however, postpartum women continued to demonstrate greater force fluctuations than controls even when matched for physical activity levels, suggesting that physical activity is not the sole mechanism behind the impaired force control observed during trunk flexion contractions after pregnancy and childbirth. Furthermore, perturbations to the connective tissue of the anterior abdominal wall during pregnancy and childbirth, such as thinning and widening of the linea alba (1, 2), may compromise the transfer of force generated by the abdominal muscles (30, 31). Large fluctuations in abdominal muscle force may lead to significant fluctuations in intra-abdominal pressure, and thus stability of the lumbar spine and pelvis (5), making further research of force control and its impact on lumbopelvic stability important in postpartum women.
Trunk flexor strength appears to be a critical factor in musculoskeletal function after pregnancy and childbirth. Stronger women were less fatigable and demonstrated better functional mobility, as evidenced by performance on the six-minute walk test. The association between strength and fatigability of the abdominal muscles has also been observed in healthy young men and women (15), supporting the importance of core strength. Strength was also associated with thickness of the rectus abdominis muscle and with self-reported physical activity over the previous year. Thus, our results suggest that lower physical activity levels in postpartum women may have contributed to lower trunk flexor strength. Physical activity levels of postpartum women were significantly lower than those of control women, and self-reported physical activity over the previous 12 months declined even further between 8 and 26 weeks postpartum. In addition, postpartum women did not meet the recommended average of 30 minutes per day of moderate intensity physical activity (32). These results provide a rationale for prescription of individualized exercise for postpartum women to offset the strength decrements, and thus the impairments in fatigability and functional mobility, seen in this study.
However, the strength, fatigability and torque steadiness deficits after pregnancy and childbirth do not appear to be mediated solely by decreased physical activity levels in the postpartum group, as physical activity matching continued to show that postpartum women were weaker, more fatigable, with reduced control of torque during isometric contractions than control women. In this activity-matched subgroup, the postpartum women continued to demonstrate greater IRD and thinner rectus abdominis muscle thickness than controls, suggesting that the significant stretch experienced by the abdominal muscles during pregnancy and the changes in fascial integrity in postpartum women may contribute to the deficits in abdominal muscle function observed in this population. This highlights the critical need for further research into the mechanisms responsible for impaired strength, fatigability, and steadiness, especially of the trunk flexor muscles, following pregnancy and childbirth.
One limitation of this study is that the postpartum women in this study were statistically older than the women in the control group; however, it has been well documented that age-related changes in muscular strength typically are not apparent until after age 50 (28). As the mean age of both groups is in the mid-20s and early 30s (~5-6 years difference), age was probably not a significant contributing factor to the differences in strength, fatigability and steadiness between nulligravid and postpartum women. Another limitation is that we only assessed one muscle group outside of the trunk flexors (hand grip muscles). Further research is needed to determine if other major muscle groups, such as the knee extensors, also experience impairments in strength/fatigability in a postpartum population.
Conclusion
Postpartum women had larger deficits in trunk flexor strength, muscle endurance and steadiness of contraction, up to 6 months postpartum, and that could not be fully accounted for by lower levels of physical activity, at least at 8 weeks after childbirth. Furthermore, women who delivered by Cesarean section had even greater trunk flexor deficits in fatigability and torque steadiness than those who had a vaginal delivery. These large deficits in trunk flexor strength, fatigability and steadiness in postpartum women in this study support the need for skilled assessment of the musculoskeletal system by health care providers who have expertise in the examination, diagnosis, and treatment of musculoskeletal disorders. Incorporating health care professionals such as physiatrists and physical therapists in the standard care of pregnant and postpartum women may offset some of the neuromuscular impairments seen in this study, and may improve the incidence and severity of other pregnancy-related musculoskeletal disorders, such as low back pain, pelvic girdle pain, and incontinence. Further research is needed to determine the mechanisms for the large deficits in abdominal muscle function postpartum, and the impact of exercise and rehabilitation on the musculoskeletal health of pregnant and postpartum women.
Acknowledgments
Grant Support: Women’s Health Research Program Grant, Department of Obstetrics & Gynecology, Medical College of Wisconsin; American Dissertation Fellowship, American Association of University Women; National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Numbers UL1TR001436 and 1TL1TR001437.
Footnotes
The authors thank the following individuals for their contributions to this project:
Ms. Jordan Lemens, Marquette University, Exercise Science Intern, for assistance with data collection and analysis.
Ms. Sarah Nisivaco, Marquette University, Honors Program Summer Research Program, for assistance with data analysis.
Dr. Anna McCormick, Medical College of Wisconsin, for assistance with subject recruitment.
Dr. Ruta Brazauskas, Medical College of Wisconsin, for statistical analysis.
The authors report no conflicts of interest. The results of this study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The results of this study do not constitute endorsement by ACSM, are solely the responsibility of the authors, and do not necessarily represent the official views of the NIH.
References
- 1.Boissonnault JS, Blaschak MJ. Incidence of Diastasis Recti Abdominis during the Childbearing Year. Physical Therapy. 1988;68(7):1082–6. doi: 10.1093/ptj/68.7.1082. [DOI] [PubMed] [Google Scholar]
- 2.Coldron Y, Stokes MJ, Newham DJ, Cook K. Postpartum characteristics of rectus abdominis on ultrasound imaging. Manual therapy. 2008;13(2):112–21. doi: 10.1016/j.math.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Kristiansson P, Svardsudd K, von Schoultz B. Reproductive hormones and aminoterminal propeptide of type III procollagen in serum as early markers of pelvic pain during late pregnancy. American Journal of Obstetrics and Gynecology. 1999;180(1):128–34. doi: 10.1016/s0002-9378(99)70162-6. [DOI] [PubMed] [Google Scholar]
- 4.Neumann DA. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. Third. St Louis, MO: Mosby Elsevier; 2016. [Google Scholar]
- 5.Hodges PW, Kaigle Holm A, Holm S, Ekström L, Cresswell A, Hansson T, et al. Intervertebral stiffness of the spine is increased by evoked contraction of transversus abdominis and the diaphragm: in vivo porcine studies. Spine (Phila Pa 1976) 2003;28(23):2594–601. doi: 10.1097/01.BRS.0000096676.14323.25. [DOI] [PubMed] [Google Scholar]
- 6.Stokes IA, Gardner-Morse MG, Henry SM. Abdominal muscle activation increases lumbar spinal stability: analysis of contributions of different muscle groups. Clin Biomech (Bristol, Avon) 2011;26(8):797–803. doi: 10.1016/j.clinbiomech.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee DG, Lee LJ, McLaughlin L. Stability, continence and breathing: The role of fascia following pregnancy and delivery. Journal of Bodywork and Movement Therapies. 2008;12:333–48. doi: 10.1016/j.jbmt.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Gilleard WL, Brown JMM. Structure and Function of the Abdominal Muscles in Primigravid Subjects During Pregnancy and the Immediate Postbirth Period. Journal of the American Physical Therapy Association. 1996;76(7):750–62. doi: 10.1093/ptj/76.7.750. [DOI] [PubMed] [Google Scholar]
- 9.Lobel M, DeLuca RS. Psychosocial sequelae of cesarean delivery: Review and analysis of their casues and implications. Social Science & Medicine. 2007;64:2272–84. doi: 10.1016/j.socscimed.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 10.Gutke A, Lundberg M, Ostgaard HC, Oberg B. Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms. European Spine Journal. 2011;20(3):440–8. doi: 10.1007/s00586-010-1487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hunter SK. Performance Fatigability: Mechanisms and Task Specificity. Cold Spring Harb Perspect Med. 2017 doi: 10.1101/cshperspect.a029728. Epub 2017/05/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Almuklass AM, Price RC, Gould JR, Enoka RM. Force steadiness as a predictor of time to complete a pegboard test of dexterity in young men and women. J Appl Physiol (1985) 2016;120(12):1410–7. doi: 10.1152/japplphysiol.01051.2015. [DOI] [PubMed] [Google Scholar]
- 13.Marmon AR, Pascoe MA, Schwartz RS, Enoka RM. Associations among strength, steadiness, and hand function across the adult life span. Med Sci Sports Exerc. 2011;43(4):560–7. doi: 10.1249/MSS.0b013e3181f3f3ab. [DOI] [PubMed] [Google Scholar]
- 14.Enoka RM, Christou EA, Hunter SK, Kornatz KW, Semmler JG, Taylor AM, et al. Mechanisms that contribute to differences in motor performance between young and old adults. J Electromyogr Kinesiol. 2003;13(1):1–12. doi: 10.1016/s1050-6411(02)00084-6. [DOI] [PubMed] [Google Scholar]
- 15.Deering R, Senefeld J, Pashibin T, Neumann DA, Hunter S. Muscle Function and Fatigability of Trunk Flexors in Males and Females. Biology of Sex Differences. 2017;8:12. doi: 10.1186/s13293-017-0133-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Borders N. After the Afterbirth: A Critical Review of Postpartum Health Relative to Method of Delivery. The Journal of Midwifery & Women’s Health. 2006;51(4):242–8. doi: 10.1016/j.jmwh.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Liddle SD, Pennick V. Interventions for preventing and treating low-back and pelvic pain during pregnancy (Review) Cochrane Database of Systematic Reviews. 2015;(9):1–116. doi: 10.1002/14651858.CD001139.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng CY, Fowles ER, Walker LO. Continuing education module: postpartum maternal health care in the United States: a critical review. J Perinat Educ. 2006;15(3):34–42. doi: 10.1624/105812406X119002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vahratian A, Johnson TR. Maternity leave benefits in the United States: today’s economic climate underlines deficiencies. Birth. 2009;36(3):177–9. doi: 10.1111/j.1523-536X.2009.00330.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Archuleta K. In: Handbook on Leave and Workplace Flexibilities for Childbirth, Adoption, and Foster Care. Management USOoP, editor. 2015. pp. 9–18. [Google Scholar]
- 21.Cram JR. Cram’s Introduction to Surface Electromyography. 2nd. Sudbury, Massachusetts: Jones and Bartlett; 2011. p. 412. [Google Scholar]
- 22.Kriska AM, Knowler WC, LaPorte RE, Drash AL, Wing RR, Blair SN, et al. Development of questionnaire to examine relationship of physical activity and diabetes in Pima Indians. Diabetes Care. 1990;13(4):401–11. doi: 10.2337/diacare.13.4.401. [DOI] [PubMed] [Google Scholar]
- 23.Ross RM, Murthy JN, Wollak ID, Jackson AS. The six minute walk test accurately estimates mean peak oxygen uptake. BMC Pulm Med. 2010;10:31. doi: 10.1186/1471-2466-10-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hunter SK. Muscle: the Primary Stabilizer and Mover of the Skeletal System. In: Neumann DA, editor. Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. Third. Mosby Elsevier; 2016. pp. 47–76. [Google Scholar]
- 25.Riley ZA, Maerz AH, Litsey JC, Enoka RM. Motor unit recruitment in human biceps brachii during sustained voluntary contractions. J Physiol. 2008;586(8):2183–93. doi: 10.1113/jphysiol.2008.150698. 10.1113/jphysiol.2008.150698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpentier A, Duchateau J, Hainaut K. Motor unit behaviour and contractile changes during fatigue in the human first dorsal interosseus. J Physiol. 2001;534(Pt 3):903–12. doi: 10.1111/j.1469-7793.2001.00903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farina D, Negro F. Common synaptic input to motor neurons, motor unit synchronization, and force control. Exerc Sport Sci Rev. 2015;43(1):23–33. doi: 10.1249/JES.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 28.Hunter SK, Pereira HM, Keenan KG. The Aging Neuromuscular System and Motor Performance. J Appl Physiol (1985) 2016 doi: 10.1152/japplphysiol.00475.2016. jap.00475.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hunter SK. Sex differences in human fatigability: mechanisms and insight to physiological responses. Acta Physiol (Oxf) 2014;210(4):768–89. doi: 10.1111/apha.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown SHM, McGill SM. Transmission of Muscularly Generated Force and Stiffness Between Layers of the Rat Abdominal Wall. Spine. 2009;34(2):E70–E5. doi: 10.1097/BRS.0b013e31818bd6b1. [DOI] [PubMed] [Google Scholar]
- 31.Gracovetsky S, Farfan H, Lamy C. A mathematical model of the lumbar spine using an optimized system to control muscles and ligamets. Orthop Clin North Am. 1977;8(1) [PubMed] [Google Scholar]
- 32.Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]


