Abstract
Introduction
Suicide among military personnel and young Veterans remains a health concern. This study examined stateside distribution of suicides by U.S. county to help focus prevention efforts.
Methods
Using 2005–2012 National Violent Death Reporting System data from 16 states (963 counties, or county-equivalent entities), this study mapped the county-level distribution of suicides among current military and Veteran decedents aged 18–35 years. This study also compared incident circumstances of death between decedents in high-density counties (i.e., counties with the highest proportion of deaths) versus those in medium/low-density counties to better understand the precipitators of suicide in counties most affected. Last, this study identified potential military and Veteran Health Administration intervention sites. All analyses were conducted in 2015.
Results
Within the National Violent Death Reporting System participating states, an estimated 262 (33%) current military suicides occurred in just ten (1.0%) counties, and 391 (33%) Veteran suicides occurred in 33 (3.4%) counties. Mental health and intimate partner problems were common precipitating circumstances, and some circumstances differed between cases in high-versus those in medium/low-density counties. Multiple potential intervention sites were identified in high-density counties.
Conclusions
These findings suggest that military and Veteran suicides are concentrated in a small number of counties. Increased efforts at these locales might be beneficial.
Introduction
The suicide rate doubled among active duty military personnel1,2 during Operations Enduring Freedom and Iraqi Freedom, from 2001 to 2010. Suicide-related morbidity and mortality have become health concerns among current military personnel and young Veterans,3,4 thereby warranting suicide prevention strategies for these populations.3,5–11 Surveillance data are critical to locating areas with the greatest burden of these deaths.12
Epidemiologic studies compare suicide rates between populations or locales to identify at-risk groups or areas. However, states with high rates do not always account for the greatest proportion of suicides nationally. For example, the 2013 state suicide rates for the general population were highest in Montana (24/100,000 population); Alaska (23/100,000); Wyoming (21/100,000); Utah (21/100,000); and New Mexico (20/100,000). These states accounted for 1,553 deaths or 3.8% of all suicides nationally.13 The suicide rate in California was roughly half those at 10/100,000 population; however, because of the population size, suicides accounted for 2.5 times more deaths (n=4,025) than those five states combined and overall 10% of suicides nationally.13 As prevention efforts aim to eliminate suicides among current military and Veteran populations, another way surveillance data can focus strategies is by determining which U.S. counties account for the greatest proportion of military and Veteran suicide deaths. Exploring the type of nearby military and Veterans Health Administration (VHA) facilities available within counties bearing the greatest burden of suicides (hereafter referred to as “high-density counties”) might inform practitioners and researchers where to implement prevention strategies.
Also, though suicide risk factors vary,14 decedents in similar environments and in close proximity might have similar factors involved in their deaths.15 More-descriptive details on circumstances preceding suicide among current military personnel and Veterans in high-density counties might further focus strategies on the needs of communities most affected.
Given these surveillance needs, this study:
Examines suicides among current military personnel and young Veterans by county in 16 U.S. states
Identifies high-density counties
Compares suicide incidents in high-versus medium/low-density counties for each group; and
Identifies military and VHA facilities in high-density counties that might serve as intervention sites.
Methods
This study used National Violent Death Reporting System (NVDRS) data from 16 U.S. states (Alaska, Colorado, Georgia, Kentucky, Maryland, Massachusetts, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, Rhode Island, South Carolina, Utah, Virginia, and Wisconsin); therefore, case inclusion was limited to incidents in those states. Data years included 2005–2012. NVDRS captures details on decedent characteristics, the mechanisms/weapons involved, and the precipitating circumstances of violent deaths, including suicides, in multiple U.S. states.16 NVDRS data sources include law enforcement, coroner/medical examiner, and toxicology reports, as well as death certificates. All sources are linked by incident into a data repository. Coding is conducted by trained abstractors in each NVDRS state.16
Suicide decedents aged 18–35 years who “ever served in the military” were initially selected. This study examined young adult cases because young military personnel (enlisted ranks E1–E5) are at greatest risk of suicide within the military1,12,17 and young Veterans still transitioning to civilian life could be experiencing new life stresses along with potential post-traumatic stress (note: This Veteran sample could have initiated service during the Afghanistan/Iraq war period or during earlier conflicts since the Gulf War). Based on these criteria, this study identified 2,026 current military and Veteran decedents.
The 2,026 decedents were categorized as either “current military” or “Veterans” based on the NVDRS occupation fields provided by death certificates, law enforcement reports, and coroner/medical examiner reports. For these fields, occupation is written as open text with terms like “soldier” and “Army” (a previous NVDRS study discovered that a military occupation was clearly listed in at least one field for 93% of decedents known to currently be in the military).12 Those with military occupations were categorized as “current military” (n=803). Those with different occupations were considered “Veterans” (n=1,178). Those with “unknown” occupations were considered to=have an unknown discharge status (n=45). Three abstractors categorized the decedents (κ=0.878) and then reconciled differences. This study only presents findings on the current military and Veteran groups.
Measures
The NVDRS provides details on decedent demographics, incident characteristics (e.g., location of death, weapons/mechanisms involved), and precipitating circumstances of death. Precipitating circumstances come from law enforcement and coroner/medical examiner investigator reports. To gather this information, investigators process forensic evidence and interview family members, friends, and others associated with the decedent as well as witnesses to the death.18 Precipitating factors included current/recent depressed mood or mental health problem, alcohol dependence or suspected intoxication at the time of death, other substance abuse problems, intimate partner problems, other relationship problems, criminal/civil legal problems, job problems, financial problems, and any recent crisis (within 2 weeks of death). These factors have been cited elsewhere as risk factors for suicide.19–28 Additionally, other preceding circumstances were examined such as whether decedents disclosed suicide intent or left suicide notes, which suggest premeditation or desire to communicate intentions and motives either pre- or post-event. Circumstance-variable definitions are provided in the Appendix (available online).16
Statistical Analysis
For each study group, counties within the NVDRS states were ranked from high to low according to the total number of suicides; therefore, two lists were generated. According to census records, there were 963 counties and county-equivalent entities in this study. Most NVDRS states initiate records by electronically importing death certificate data within their territories, which minimizes the impact of counties not reporting suicides to NVDRS. For each list, counties were then partitioned into three categories:
“high-density,” which accounted for the top 33% of the suicides
“medium-density,” which accounted for the next 33% of suicides; and
“low-density,” which accounted for the remaining suicides.
Counties are displayed according to density for each group. This study also used a case comparison design to describe incidents in high-versus those in outside (i.e., medium/low-density) counties for each group to identify incident characteristics associated with concentrated areas where interventions might be focused. Comparisons were made with multivariable logistic regression accounting for all variables. Prevalence AORs and 95% CIs are presented.
Last, the military installations and VHA facilities located in the high-density counties for both groups are presented. Types of facilities included military installations, VHA outpatient clinics, VHA hospitals, and other VHA centers. All analyses were conducted in 2015.
Results
Samples were refined based on county residency. This analysis excluded 42 (3.5%) of the 1,178 Veteran decedents who died in nonresident counties. Part of this analysis aimed to identify VHA facilities in high-density counties that might serve as intervention sites. VHA facilities located in counties with many nonresident decedents might not be ideal sites. Therefore, this Veteran suicide analysis only included decedents who died in their residential county. By contrast, the current military group included both county residents and nonresidents. Nonresidents (n=70, 8.7%) were included in this group because these decedents were most likely affiliated with the local military installation, the potential intervention site, and were not stationed long enough to declare county residency. Finally, this study excluded 32 (4%) of the 803 military decedents and 2 (0.2%) of the 1,136 Veteran decedents who did not have county of death information. The total mapped samples included 771 current military and 1,134 Veteran decedents.
For the second analysis (i.e., characterizing decedents, incidents, and precipitating circumstances), the samples were limited to cases with known law enforcement or coroner/medical examiner circumstance information, which included 640 of 771 (83%) current military decedents and 1,042 of 1,134 (92%) Veteran decedents (Appendix Figure 1, available online).
Figures 1 and 2 display the burden of suicide by county from 2005 to 2012 for current military personnel and Veterans aged 18–35 years among 16 NVDRS states. Both maps show that suicides were concentrated in a small proportion of counties. An estimated 262 (33%) current military suicide deaths occurred in only 10 (1%) of the 963 NVDRS counties. Total deaths in these counties ranged from 12 to 51, and these counties were considered “high-density” counties. They were located in six of the 16 NVDRS states (North Carolina, Colorado, Virginia, Georgia, Alaska, and Oklahoma; Figure 1). Roughly another third (36%) of the current military suicide deaths occurred in 55 (6%) of the 963 counties; these counties had a range of three to 11 deaths and were considered “medium-density” counties. The remaining counties in NVDRS were considered “low-density” and accounted for the rest of the current military suicides.
Figure 1.

Suicides among current military personnel of ages 18–35 years, National Violent Death Reporting System, 16 states, 2005–2012.
Figure 2.
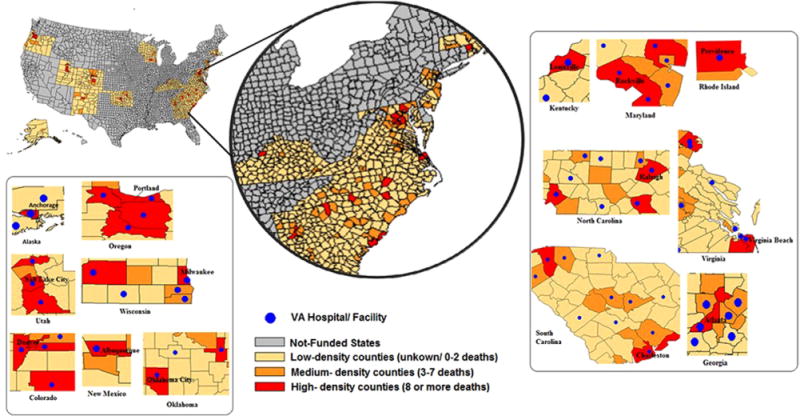
Suicides among Veterans of ages 18–35 years, National Violent Death Reporting System, 16 states, 2005–2012.
For the Veteran group, an estimated 391 (33%) suicides occurred in 33 (3.4%) counties (Figure 2). Total deaths in these “high-density” counties ranged from 8 to 27 deaths. Another third of the suicides occurred in 93 (10%) of the 963 counties. These counties had a range of three to seven deaths and were considered “medium-density.” The remaining “low-density” counties accounted for the rest of the Veteran suicides.
A description of the study groups is provided in Table 1 for decedents with known circumstance information. For current military suicide decedents aged 18–35 years, most were men (95%) and non-Hispanic whites (75%). More than half (54%) of these decedents were aged 18–25 years and 56% were either currently or previously married. An estimated 67% of the current military decedents died in their home, and 68% died by firearm use.
Table 1.
Incident, Precipitating, and Other Preceding Circumstances of 18–35 Year Old Adult Suicide Decedents, Current Military Personnel or Veterans
| Variable | Current military personnel (N=640) | Veterans (N=1,042) | ||||||
|---|---|---|---|---|---|---|---|---|
| Total,a n (%) | High density (≥33%ile), n (%) | Medium-low density, n (%) | AOR (95% CIs)b | Total, n (%) | High density (>33%ile), n (%) | Medium-low density, n (%) | AOR (95% CIs)b | |
| Demographic | ||||||||
| Sex | ||||||||
| Female | 31 (4.8) | 8 (4.0) | 23 (5.2) | ref | 78 (7.5) | 33 (9.1) | 45 (6.6) | ref |
| Male | 609 (95.2) | 191 (96.0) | 418 (94.8) | 1.2 (0.5, 2.9) | 964 (92.5) | 329 (90.9) | 635 (93.4) | 0.7 (0.4, 1.2) |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 478 (74.7) | 142 (71.4) | 336 (76.2) | ref | 800 (76.8) | 264 (72.9) | 536 (78.9) | ref |
| Non-Hispanic black | 92 (14.4) | 29 (14.6) | 63 (14.3) | 1.0 (0.6, 1.7) | 123 (11.8) | 49 (13.5) | 74 (10.9) | 1.4 (0.9, 2.2) |
| Non-Hispanic other | 36 (5.6) | 14 (7.0) | 22 (5.0) | 1.4 (0.7, 3.0) | 55 (5.3) | 23 (6.4) | 32 (4.7) | 1.4 (0.8, 2.5) |
| Hispanic | 34 (5.3) | 14 (7.0) | 20 (4.5) | 1.8 (0.8, 3.7) | 63 (6.1) | 26 (7.2) | 37 (5.4) | 1.3 (0.7, 2.2) |
| Age (years) | ||||||||
| 18–25 | 345 (53.9) | 118 (59.3) | 227 (51.5) | ref | 302 (29.0) | 95 (26.2) | 207 (30.4) | ref |
| 26–35 | 295 (46.1) | 81 (40.7) | 214 (48.5) | 0.7 (0.5,1.0) | 740 (71.0) | 267 (73.8) | 473 (69.6) | 1.3 (0.9, 1.8) |
| Marital status | ||||||||
| Never married, single unspecified | 280 (43.75) | 75 (37.7) | 205 (46.5) | ref | 510 (48.9) | 189 (52.2) | 321 (47.2) | ref |
| Married | 269 (42.0) | 100 (50.3) | 169 (38.3) | 2.0 (1.3,3.0) | 317 (30.4) | 95 (26.2) | 222 (32.7) | 0.7 (0.5, 1.0) |
| Divorced | 56 (8.8) | 15 (7.5) | 41 (9.3) | 1.2 (0.6, 2.5) | 174 (16.7) | 68 (18.8) | 106 (15.6) | 1.0 (0.7, 1.4) |
| Married but separated | 23 (4.0) | 6 (3.0) | 17 (3.4) | 1.3 (0.5, 3.7) | 28 (2.7) | –e | 25 (3.7) | 0.2 (0.1, 0.6) |
| Widowed | 7 (1.0) | –e | 5 (1.1) | 1.2 (0.2, 6.8) | 5 (0.5) | –e | –e | 2.9 (0.5, 18.0) |
| Incident characteristics | ||||||||
| Location of death | ||||||||
| Died outside of home | 213 (33.3) | 58 (29.2) | 155 (35.2) | ref | 330 (31.7) | 104 (28.7) | 226 (33.2) | ref |
| Died at home | 427 (66.7) | 141 (70.9) | 286 (64.9) | 1.3 (0.9, 2.0) | 712 (68.3) | 258 (71.3) | 454 (66.8) | 1.2 (0.9, 1.6) |
| Weapon involved | ||||||||
| Firearm | 436 (68.1) | 143 (71.9) | 293 (66.4) | ref | 613 (58.8) | 211 (58.3) | 402 (59.1) | ref |
| Sharp instrument | 5 (0.8) | –e | –e | 1.3 (0.2, 8.4) | 16 (1.5) | 7 (1.9) | 9 (1.3) | 1.2 (0.4, 3.4) |
| Poisoning | 43 (6.7) | 10 (5.0) | 33 (7.5) | 0.7 (0.3, 1.4) | 119 (11.4) | 47 (12.9) | 72 (10.6) | 1.2 (0.8, 1.8) |
| Hanging | 125 (19.5) | 34 (17.1) | 91 (20.6) | 0.8 (0.5, 1.3) | 260 (25.0) | 82 (22.7) | 178 (26.2) | 0.8 (0.6, 1.1) |
| Other | 31 (4.8) | 10 (5.0) | 21 (4.8) | 1.4 (0.6, 3.2) | 34 (3.3) | 15 (4.1) | 19 (2.8) | 1.7 (0.8, 3.5) |
| Precipitating circumstancesc | ||||||||
| Health relatedd | ||||||||
| Current depressed mood or mental health problem | 334 (52.2) | 102 (51.3) | 232 (52.6) | 1.1 (0.8, 1.6) | 648 (62.2) | 238 (65.7) | 410 (60.3) | 1.1 (0.9, 1.5) |
| Alcohol dependence, or suspected intoxication | 259 (40.5) | 80 (40.2) | 179 (40.6) | 1.0 (0.7, 1.5) | 403 (38.7) | 153 (42.3) | 250 (36.8) | 1.2 (0.9, 1.6) |
| Other substance abuse | 54 (8.4) | 11 (5.5) | 43 (9.8) | 0.6 (0.3, 1.2) | 162 (15.5) | 63 (17.4) | 99 (14.6) | 1.2 (0.8, 1.8) |
| Life-stressd | ||||||||
| Intimate partner problems | 332 (51.9) | 104 (52.3) | 228 (51.7) | 0.9 (0.6, 1.3) | 509 (48.9) | 179 (49.5) | 330 (48.5) | 1.3 (1.0, 1.8) |
| Other relationship problems | 48 (7.5) | 15 (7.5) | 33 (7.5) | 1.2 (0.6, 2.4) | 124 (11.9) | 50 (13.8) | 74 (10.9) | 1.2 (0.8, 1.8) |
| Criminal and civil legal problems | 96 (15.0) | 22 (11.1) | 74 (16.8) | 0.7 (0.4, 1.2) | 198 (19.0) | 72 (19.9) | 126 (18.5) | 1.2 (0.8, 1.7) |
| Job problems | 140 (21.9) | 41 (20.6) | 99 (22.5) | 1.0 (0.6, 1.6) | 167 (16.0) | 77 (21.3) | 90 (13.2) | 1.7 (1.2, 2.4) |
| Financial problems | 55 (8.6) | 16 (8.0) | 39 (8.8) | 1.0 (0.5, 1.9) | 120 (11.5) | 52 (14.4) | 68 (10.0) | 1.3 (0.9, 2.0) |
| Recent crisis | 227 (35.5) | 67 (33.7) | 160 (36.3) | 0.9 (0.6, 1.3) | 366 (35.1) | 124 (34.3) | 242 (35.6) | 0.8 (0.6, 1.1) |
| Other preceding circumstancesd | ||||||||
| Disclosed intent | 176 (27.5) | 41 (20.6) | 135 (30.6) | 0.6 (0.4, 1.0) | 313 (30.0) | 121 (33.4) | 192 (28.2) | 1.2 (0.9, 1.6) |
| Left a note | 195 (30.5) | 54 (27.1) | 141 (32.0) | 0.9 (0.6, 1.3) | 336 (32.3) | 124 (34.3) | 212 (31.2) | 1.2 (0.9, 1.6) |
| Total | 640 (100.0) | 199 (100.0) | 441 (100.0) | 1042 (100) | 362 (100) | 680 (100) | ||
Note: Analysis stratified by suicide-case county density, National Violent Death Reporting System, 16 states, 2005–2012. Boldface indicates statistical significance (p<0.05).
Unknown values are not presented. Unknown values never exceeded 1% for any variable.
Adjusted for all demographic variables (i.e., age, sex, race/ethnicity, marital status) and all other incident, precipitating, and preceding circumstances.
AII circumstances are not mutually exclusive.
Reference groups for these circumstances were those who did not have the circumstance identified.
Values suppressed to prevent identifiability.
The five most common precipitating circumstances discovered among current military decedents with known circumstance information were a current depressed mood or mental health problem (52%); intimate partner problems (52%); alcohol dependence or suspected intoxication (41%); a recent or impending crisis (36%); and job problems (22%) (Table 1). Among the 334 decedents identified as having a current depressed mood or mental health problems, 203 decedents had specified mental health diagnoses. The most common were major depressive disorder (72%) and post-traumatic stress disorder (33%) (Appendix Table 1, available online). Thirty-one percent of the current military decedents left notes and 28% disclosed intent. Compared with current military decedents in medium/low-density counties, military decedents in high-density counties were of younger age and more commonly married versus never married (Table 1).
Veteran suicide decedents aged 18–35 years also consisted mostly of men (93%) and non-Hispanic whites (77%) (Table 1). Most were aged 26–35 years (71%), and half were either currently or previously married (50%). An estimated 68% of the Veteran decedents died in their homes, and 59% died by firearm use.
Veteran suicide decedents also commonly had a current depressed mood or mental health problem (62%); intimate partner problems (49%); alcohol dependence or suspected intoxication (39%); a recent or impending crisis (35%); and job problems (16%). Additionally, 19% of Veteran suicide decedents had precipitating criminal/civil legal problems. There were 391 decedents with specified mental health diagnoses: 74% had major depression and 18% had post-traumatic stress disorder (Appendix Table 1, available online). Thirty-two percent of Veteran decedents left notes and 30% disclosed suicidal intent. Compared with Veteran decedents in medium/low-density counties, Veteran decedents in high-density counties more commonly had precipitating job problems and were less commonly married (or married but separated) versus never married.
For current military decedents, military installations were identified in high-density counties (Table 2; note: This study could not confirm most decedents’ branch of service and therefore was unable to connect them to the appropriate installation in counties with multiple installations). U.S. Army installations were in seven of ten high-density counties. The U.S. Air Force had installations in four high-density counties. Navy or Marine bases were in three high-density counties. Coast Guard and Reserves installations were each found in one high-density county. All ten current military suicide high-density counties also had VHA facilities that might help support military suicide prevention efforts.
Table 2.
Military Installations and Veteran Health Administration Facilities in High-Density Counties of Suicides Among Current Military Personnel and Veterans of Ages 18–35 Years
| State | County | Number of suicides | Cumulative number (%)a | Military installations | VHA facilities | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| USA | USMC | USAF | USN | USCG | Reserves | Hospital | Outpatient centers and clinics | Veterans center | ||||
| Current military personnel | ||||||||||||
| NC | Cumberland | 51 | 51(6) | × | × | × | × | × | ||||
| NC | Onslow | 47 | 98 (12) | × | × | × | ||||||
| CO | El Paso | 36 | 134 (17) | × | × | × | × | |||||
| VA | Norfolk City | 26 | 160 (20) | × | × | × | ||||||
| VA | Virginia Beach City | 26 | 186 (23) | × | × | |||||||
| GA | Liberty | 19 | 205 (26) | × | × | |||||||
| AK | Anchorage | 18 | 223 (28) | × | × | × | × | |||||
| OK | Oklahoma | 14 | 237 (30) | × | × | × | × | × | × | |||
| GA | Chatham | 13 | 250 (31) | × | × | |||||||
| GA | Muscogee | 12 | 262 (33) | × | × | × | ||||||
| Veterans | ||||||||||||
| CO | El Paso | 27 | 27 (2) | × | × | × | × | |||||
| OK | Oklahoma | 23 | 50 (4) | × | × | × | × | × | × | |||
| WI | Milwaukee | 18 | 68 (6) | × | × | × | × | |||||
| UT | Salt Lake | 17 | 85 (7) | × | × | × | ||||||
| NM | Bernalillo | 16 | 101 (9) | × | × | × | ||||||
| AK | Anchorage | 16 | 117 (10) | × | × | × | × | |||||
| OK | Tulsa | 15 | 132 (11) | × | × | |||||||
| NC | Wake | 14 | 146 (12) | × | × | × | ||||||
| CO | Denver | 14 | 160 (14) | × | × | × | × | |||||
| UT | Utah | 13 | 173 (15) | × | × | |||||||
| VA | Virginia Beach City | 12 | 185 (16) | × | × | |||||||
| OR | Washington | 12 | 197 (17) | × | ||||||||
| UT | Weber | 11 | 208 (18) | × | × | × | ||||||
| NC | Mecklenburg | 11 | 219 (19) | × | × | |||||||
| MD | Baltimore | 11 | 230 (20) | × | × | × | × | |||||
| KY | Jefferson | 11 | 241 (20) | × | × | × | ||||||
| CO | Jefferson | 11 | 252 (21) | |||||||||
| CO | Arapahoe | 11 | 263 (22) | × | × | × | × | |||||
| VA | Fairfax | 10 | 273 (23) | × | ||||||||
| NC | Cumberland | 10 | 283 (24) | × | × | × | × | × | ||||
| MD | Prince Georges | 10 | 293 (25) | × | × | × | × | |||||
| WI | Dane | 9 | 302 (26) | × | × | × | ||||||
| GA | Fulton | 9 | 311 (26) | × | ||||||||
| VA | Chesapeake City | 8 | 319 (27) | × | × | |||||||
| SC | Charleston | 8 | 327 (28) | × | × | × | ||||||
| SC | Greenville | 8 | 335 (28) | × | × | |||||||
| RI | Providence | 8 | 343 (29) | × | × | |||||||
| OR | Clackamas | 8 | 351 (30) | × | ||||||||
| OR | Marion | 8 | 359 (30) | × | ||||||||
| OR | Multnomah | 8 | 367 (31) | × | × | × | ||||||
| OK | Cleveland | 8 | 375 (32) | × | × | × | × | × | × | |||
| MD | Montgomery | 8 | 383 (33) | × | × | |||||||
| CO | Boulder | 8 | 391 (33) | × | ||||||||
Cumulative percent is among the total number of suicide deaths captured in the NVDRS states and study years selected for this study. There were 771 total suicides among current affiliates and 1,134 suicides among Veterans.
USA, U.S. Army; USAF, U.S. Air Force; USCG, U.S. Coast Guard; USMC, U.S. Marine Corps; USN, U.S. Navy; VFIA, Veterans Flealth Administration.
For Veterans, 28 of 33 Veteran suicide high-density counties had VHA facilities (Table 2). In total, 13 of these counties had VHA hospitals, 21 had VHA outpatient clinics, and 26 had other VHA centers.
Discussion
As suggested by data from the 16 NVDRS states, military and Veteran suicides are concentrated in a small number of counties; therefore, prevention strategies may not have to be scaled to national or even statewide levels to benefit these populations. Select states including North Carolina, Georgia, and Virginia may be NVDRS states of interest with regard to military suicides because they had multiple high-density counties with local military installations that could potentially serve as intervention sites. For Veteran suicide, almost all NVDRS states had at least one high-density county with nearby VHA clinics that could potentially support Veteran suicide prevention efforts.
As expected, this study found that suicides commonly involved firearms12,17,29 and were frequently precipitated by depressed mood/mental health conditions,8,30,31 intimate partner problems,28,32,33 job-related problems,29 or a recent crisis.12,29 Additionally, among current military decedents, decedents in high-density counties were younger and more commonly married than those in less concentrated areas. Among Veteran decedents, being single and having job problems were more common characteristics for those in high-versus medium/low-density areas. Many decedents had a history of alcoholism or were suspected of being intoxicated at the time of death, which has also been previously reported.1,34 Also, at least one fifth of decedents disclosed suicide intent to others who might not have known how to respond. Collectively, these findings suggest that prevention efforts for these populations must not only focus on risks in relation to individual health but also on those associated with social norms and one’s social environment.35
The U.S. Air Force developed a suicide prevention program aimed to reduce risk factors, strengthen social support and social skills, and modify social norms to encourage help-seeking.36 This program established an Integrated Delivery System and Community Action Information Board to provide assistance with financial, child care, mental health, and legal services. It also trained staff on identifying warning signs of suicidality and changed policies to ensure that Airmen who accessed mental health treatment received increased confidentiality privileges. Knox et al.37 evaluated the Air Force program and found it to be associated with a 33% reduction in the suicide rate. Efforts to sustain this program are needed to ensure a long-standing positive impact; however, this program exemplifies a public health approach to suicide prevention and might be enhanced with the latest research.
In recent years, clinical research on military populations has advanced knowledge of suicide screening and risk assessment,9,38–40 mental health conditions linked to suicide,7,8,31 treatments tailored to address suicidality,6 and telemedicine and teletherapeutic tools used in treating deployed soldiers.3,17 These advancements can be incorporated into comprehensive strategies and help address mental health problems. For example, Warner and colleagues40 reported that pre-deployment mental health screening can be feasibly connected to ongoing mental health support during deployment. Rudd et al.6 found that brief cognitive behavioral therapy versus treatment as usual was associated with a 60% decline in suicide attempts among military personnel who reported having suicidal ideation.
Programs aimed to strengthen intimate partner relationships exist for current/former military personnel but have not been examined with respect to suicide-related outcomes. These programs might significantly help comprehensive prevention strategies considering the prevalence of intimate partner conflicts that precipitate suicide. Such programs can improve coping skills for relationship-related stress, increase awareness of suicide warning signs among partners, and provide guidance on how to act when someone in the family discloses suicide intent. One program, Strength at Home Couples, uses couples therapy to improve intimate partner relationships among soldiers, particularly those who suffer from post-traumatic stress disorder. This program has been shown to prevent intimate partner conflicts and aggression,41,42 but more exploration into how it impacts suicide is still needed.
Last, this is another study documenting that suicide among current military and Veteran populations is largely committed with firearms.12,17 It is important to evaluate safe storage practices and other prevention strategies around lethal means as part of a comprehensive approach. Suicide can be an impulsive act. Simon and colleagues43 found that 24% of a group aged 13–34 years who survived nearly lethal suicide attempts spent fewer than 5 minutes contemplating the act. Safe storage of firearms (e.g., keeping firearms unloaded, locked, and secured) might prevent impulsive suicides. Campaigns, such as “Lok-it-up” or the U.S. Department of Veterans Affairs’ Gun Safety Lock Program, increase awareness of safe storage options.44–46 Safe storage practices have been associated with lower risk of suicidal behavior,47–49 making them important strategies to evaluate with military populations.
Limitations
This study had some limitations. First, it was not nationally representative. Second, this study could not describe the military characteristics of current military decedents (e.g., branch of service). One database, the Department of Defense Suicide Event Reports, contains such details. NVDRS data have been linked to Department of Defense Suicide Event Reports data in the past12,29; however, the linked data did not cover this study period and therefore were excluded. Such linked data would enhance this analysis in future iterations. Third, although NVDRS is comprehensive, it did not capture some demographic characteristics that might be of interest (e.g., sexual orientation) in the entire study period and therefore were excluded. Fourth, misclassification of current military personnel as Veterans could have occurred if a military occupation was not listed in NVDRS. Fifth, county-level risk could not be assessed. County-level risk assessment is challenging because of the difficulties with estimating stable county-level rates for these populations (gathering appropriate denominator data, small numbers of suicides). The high density of cases in a county may simply be related to large populations. Nevertheless, the focus of this study was to display where cases are concentrated and installations that can reach these areas. Last, characteristics of high-versus low-density counties regarding local policies/laws and population characteristics were not described. Future efforts are planned to perform these analyses.
Conclusions
The distribution of suicide incidents among these populations largely occur in a small proportion of U.S. counties. Suicide prevention strategies that are comprehensive and focused by county might be beneficial. Future studies may also consider replicating this analysis with non-fatal attempts to further understand the burden of suicidal outcomes across U.S. counties.
Supplementary Material
Acknowledgments
Publication of this article was supported by the Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Appendix Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2016.06.001.
Footnotes
This article is part of the supplement issue titled National Violent Death Reporting System: Analyses and Commentary. 0749-3797/$36.00 http://dx.doi.org/10.1016/j.amepre.2016.06.001
No financial disclosures were reported by the authors of this paper.
References
- 1.Bachynski KE, Canham-Chervak M, Black SA, et al. Mental health risk factors for suicides in the U.S. Army, 2007-2008. Inj Prev. 2012;18(6):405–412. doi: 10.1136/injuryprev-2011-040112. [DOI] [PubMed] [Google Scholar]
- 2.Schoenbaum M, Kessler RC, Gilman SE, et al. Predictors of suicide and accident death in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS): results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71(5):493–503. doi: 10.1001/jamapsychiatry.2013.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castro CA. The U.S. framework for understanding, preventing, and caring for the mental health needs of service members who served in combat in Afghanistan and Iraq: a brief review of the issues and the research. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.24713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castro CA, Kintzle S. Suicides in the military: the post-modern combat veteran and the Hemingway effect. Curr Psychiatry Rep. 2014;16(8):460. doi: 10.1007/s11920-014-0460-1. [DOI] [PubMed] [Google Scholar]
- 5.Ilgen MA, Jain A, Lucas E, Moos RH. Substance use-disorder treatment and a decline in attempted suicide during and after treatment. J Stud Alcohol Drugs. 2007;68(4):503–509. doi: 10.15288/jsad.2007.68.503. [DOI] [PubMed] [Google Scholar]
- 6.Rudd MD, Bryan CJ, Wertenberger EG, et al. Brief cognitive-behavioral therapy effects on post-treatment suicide attempts in a military sample: results of a randomized clinical trial with 2-year follow-up. Am J Psychiatry. 2015;172(5):441–449. doi: 10.1176/appi.ajp.2014.14070843. [DOI] [PubMed] [Google Scholar]
- 7.Kessler RC, Heeringa SG, Stein MB, et al. Thirty-day prevalence of DSM-IV mental disorders among nondeployed soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71(5):504–513. doi: 10.1001/jamapsychiatry.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nock MK, Stein MB, Heeringa SG, et al. Prevalence and correlates of suicidal behavior among soldiers: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014;71(5):514–522. doi: 10.1001/jamapsy-chiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conner KR, Simons K. State of innovation in suicide intervention research with military populations. Suicide Life Threat Behav. 2015;45(3):281–292. doi: 10.1111/sltb.12130. [DOI] [PubMed] [Google Scholar]
- 10.Luxton DD, Thomas EK, Chipps J, et al. Caring letters for suicide prevention: implementation of a multi-site randomized clinical trial in the U.S. military and Veteran Affairs healthcare systems. Contemp Clin Trials. 2014;37(2):252–260. doi: 10.1016/j.cct.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Bush NE, Dobscha SK, Crumpton R, et al. A virtual hope box smartphone app as an accessory to therapy: proof-of-concept in a clinical sample of veterans. Suicide Life Threat Behav. 2015;45(1):1–9. doi: 10.1111/sltb.12103. [DOI] [PubMed] [Google Scholar]
- 12.Logan JE, Skopp NA, Reger MA, et al. Precipitating circumstances of suicide among active duty U.S. Army personnel versus U.S. civilians, 2005-2010. Suicide Life Threat Behav. 2015;45(1):65–77. doi: 10.1111/sltb.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Web-based injury statistics query and reporting system (WISQARS) www.cdc.gov/injury/wisqars/dataandstats.html. Accessed July 23, 2015.
- 14.Logan JE, Hall J, Karch DL. Suicide categories by patterns of known risk factors: a latent class analysis. Arch Gen Psychiatry. 2011;68(9):935–941. doi: 10.1001/archgenpsychiatry.2011.85. [DOI] [PubMed] [Google Scholar]
- 15.Joiner T. The clustering and contagion of suicide. Curr Dir Psychol Sci. 1999;8(3):89–92. doi: 10.1111/1467-8721.00021. [DOI] [Google Scholar]
- 16.Centers for Disease Control and Prevention (CDC) National Violent Death Reporting System (NVDRS) Web Coding Manual Version 5.1. National Center for Injury Prevention and Control, CDC; Atlanta, GA: www.cdc.gov/violenceprevention/pdf/nvdrs_web_codingmanual.pdf. Accessed October 10, 2015. [Google Scholar]
- 17.Bush NE, Reger MA, Luxton DD, et al. Suicides and suicide attempts in the U.S. Military, 2008-2010. Suicide Life Threat Behav. 2013;43(3):262–273. doi: 10.1111/sltb.12012. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Department of Justice, Office of Justice Programs, National Institute of Justice. Death scene investigation: a guide for the scene investigator. www.ncjrs.gov/pdffiles/167568.pdf Accessed August 15, 2015.
- 19.Allen JP, Cross G, Swanner J. Suicide in the Army: a review of current information. Mil Med. 2005;170(7):580–584. doi: 10.7205/MILMED.170.7.580. [DOI] [PubMed] [Google Scholar]
- 20.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Kung HC, Pearson JL, Liu X. Risk factors for male and female suicide decedents ages 15-64 in the United States. Results from the 1993 National Mortality Followback Survey. Soc Psychiatry Psychiatr Epidemiol. 2003;38(8):419–426. doi: 10.1007/s00127-003-0656-x. [DOI] [PubMed] [Google Scholar]
- 22.Mahon MJ, Tobin JP, Cusack DA, et al. Suicide among regular-duty military personnel: a retrospective case-control study of occupation-specific risk factors for workplace suicide. Am J Psychiatry. 2005;162(9):1688–1696. doi: 10.1176/appi.ajp.162.9.1688. [DOI] [PubMed] [Google Scholar]
- 23.Miller M, Mogun H, Azrael D, et al. Cancer and the risk of suicide in older Americans. J Clin Oncol. 2008;26(29):4720–4724. doi: 10.1200/JCO.2007.14.3990. [DOI] [PubMed] [Google Scholar]
- 24.Moscicki EK. Epidemiology of suicide. Int Psychogeriatr. 1995;7(2):137–148. doi: 10.1017/S1041610295001931. [DOI] [PubMed] [Google Scholar]
- 25.Moscicki EK. Epidemiology of suicidal behavior. Suicide Life Threat Behav. 1995;25(1):22–35. [PubMed] [Google Scholar]
- 26.Moscicki EK. Identification of suicide risk factors using epidemiologic studies. Psychiatr Clin North Am. 1997;20(3):499–517. doi: 10.1016/S0193-953X(05)70327-0. [DOI] [PubMed] [Google Scholar]
- 27.Thoresen S, Mehlum L. Suicide in peacekeepers: risk factors for suicide versus accidental death. Suicide Life Threat Behav. 2006;36(4):432–442. doi: 10.1521/suli.2006.36.4.432. [DOI] [PubMed] [Google Scholar]
- 28.Skopp NA, Trofimovich L, Grimes J, et al. Relations between suicide and traumatic brain injury, psychiatric diagnoses, and relationship problems, active component, U.S. Armed Forces, 2001-2009. MSMR. 2012;19(2):7–11. [PubMed] [Google Scholar]
- 29.Logan J, Skopp NA, Karch D, et al. Characteristics of suicides among U.S. Army active duty personnel in 17 U.S. states from 2005 to 2007. Am J Public Health. 2012;102(suppl 1):S40–S44. doi: 10.2105/AJPH.2011.300481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nock MK, Deming CA, Fullerton CS, et al. Suicide among soldiers: a review of psychosocial risk and protective factors. Psychiatry. 2013;76(2):97–125. doi: 10.1521/psyc.2013.76.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nock MK, Ursano RJ, Heeringa SG, et al. Mental disorders, comorbidity, and pre-enlistment suicidal behavior among new soldiers in the U.S. Army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) Suicide Life Threat Behav. 2015;45(5):588–599. doi: 10.1111/sltb.12153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alexander CL, Reger MA, Smolenski DJ, Fullerton NR. Comparing U.S. Army suicide cases to a control sample: initial data and methodological lessons. Mil Med. 2014;179(10):1062–1066. doi: 10.7205/MILMED-D-13-00574. [DOI] [PubMed] [Google Scholar]
- 33.Hyman J, Ireland R, Frost L, Cottrell L. Suicide incidence and risk factors in an active duty U.S. military population. Am J Public Health. 2012;102(suppl 1):S138–S146. doi: 10.2105/AJPH.2011.300484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LeardMann CA, Powell TM, Smith TC, et al. Risk factors associated with suicide in current and former U.S. military personnel. JAMA. 2013;310(5):496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention (CDC) The social-ecological model: a framework for prevention. www.cdc.gov/violenceprevention/overview/social-ecologicalmodel.html. Accessed August 11, 2015.
- 36.The Air Force Suicide Prevention Program. A description of program initiatives and outcomes. AFPAM 44-160. https://dmna.ny.gov/suicideprevention/AFPAM44.160.pdf Accessed October 2, 2015.
- 37.Knox KL, Litts DA, Talcott GW, et al. Risk of suicide and related adverse outcomes after exposure to a suicide prevention programme in the U.S. Air Force: cohort study. BMJ. 2003;327(7428):1376. doi: 10.1136/bmj.327.7428.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haney EM, O’Neil ME, Carson S, et al. Suicide Risk Factors and Risk Assessment Tools: A Systematic Review. Washington, DC: Department of Veterans Affairs; 2012. [PubMed] [Google Scholar]
- 39.McCarthy JF, Bossarte RM, Katz IR, et al. Predictive modeling and concentration of the risk of suicide: implications for preventive interventions in the U.S. Department of Veterans Affairs. Am J Public Health. 2015;105(9):1935–1942. doi: 10.2105/AJPH.2015.302737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Warner CH, Appenzeller GN, Parker JR, et al. Effectiveness of mental health screening and coordination of in-theater care prior to deployment to Iraq: a cohort study. Am J Psychiatry. 2011;168(4):378–385. doi: 10.1176/appi.ajp.2010.10091303. [DOI] [PubMed] [Google Scholar]
- 41.Hayes M, Gallagher M, Gilbert K, et al. Targeting relational aggression in Veterans: the Strength at Home friends and family intervention. J Clin Psychiatry. 2015;76(6):774–778. doi: 10.4088/JCP.14m09155. [DOI] [PubMed] [Google Scholar]
- 42.Taft C, Macdonald A, Creech S, et al. A randomized controlled clinical trial of the Strength at Home Men’s Program for partner violence in military veterans. J Clin Psychiatry. doi: 10.4088/jcp.15m10020. In press. [DOI] [PubMed]
- 43.Simon OR, Swann AC, Powell KE, et al. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(1 suppl):49–59. doi: 10.1521/suli.32.1.5.49.24212. [DOI] [PubMed] [Google Scholar]
- 44.Suicide Prevention Resource Center. Suicide prevention toolkit for rural primary care. www.sprc.org/for-providers/primary-care-tool-kit-book-resources-providers. Accessed October 2, 2015.
- 45.King County. LOK-IT-UP: promoting the safe storage of firearms. Public Health’s 2015 Safe Storage Saves Lives Campaign. www.kingcounty.gov/healthservices/health/injury/lokitup.aspx. Accessed October 2, 2015.
- 46.U.S. Department of Veterans Affairs. Michael E. DeBakey VA Medical Center-Houston, Texas. Veteran family safety: free gun locks. www.houston.va.gov/pressreleases/Veteran_Family_Safety_Free_Gun_Locks.asp. Accessed November 20, 2015.
- 47.Grossman DC, Mueller BA, Riedy C, et al. Gun storage practices and risk of youth suicide and unintentional firearm injuries. JAMA. 2005;293(6):707–714. doi: 10.1001/jama.293.6.707. [DOI] [PubMed] [Google Scholar]
- 48.Reisch T, Steffen T, Habenstein A, Tschacher W. Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 “Army XXI” reform. Am J Psychiatry. 2013;170(9):977–984. doi: 10.1176/appi.ajp.2013.12091256. [DOI] [PubMed] [Google Scholar]
- 49.Anglemyer A, Horvath T, Rutherford G. The accessibility of firearms and risk for suicide and homicide victimization among household members: a systematic review and meta-analysis. Ann Intern Med. 2014;160(2):101–110. doi: 10.7326/M13-1301. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


