Abstract
The treatment of highly migrated lumbar disc herniation (LDH) is a challenge for percutaneous endoscopic lumbar discectomy (PELD). The purpose of this study was to determine the feasibility and efficacy of PELD for highly migrated LDH via the adjacent interlaminar space. We performed PELD via the adjacent interlaminar space in three patients with radiculopathy caused by highly migrated LDH using a full-endoscopic system (diameter of working channel: 4.1 mm, outer diameter: 6.9 mm). One case had a large interlaminar bone window that did not require enlargement. Enlargement of the bone window in other cases was performed with a 3.5-mm diameter high-speed drill. After the operation, we confirmed pain relief and evacuation of migrated LDH on magnetic resonance imaging in all patients. The mean operative time was 75.3 min, and no complication was observed. PELD via the adjacent interlaminar space is an appropriate operative approach for highly down-migrated LDH. Minimal laminectomy using a high-speed drill is conductive to this approach.
Keywords: Percutaneous endoscopic lumbar discectomy (PELD), lumbar disc herniation (LDH), highly migrated, interlaminar approach (ILA), minimally invasive
Introduction
Percutaneous endoscopic lumbar discectomy (PELD) is one of the most sophisticated operative procedures for the treatment of lumbar disc herniation (LDH) (1-3). However, the treatment of highly migrated LDH still remains a challenge for PELD.
Several modifications of PELD have been developed for the treatment of highly migrated LDH (4-13). Among these, Choi et al. described successful treatment of highly down-migrated L4/5 LDH through an L5/S1 interlaminar approach (ILA) (13). In this technical note, the author emphasized the limitation of a narrow interlaminar window. Although a 2.7-mm working channel endoscope (outer diameter 5.8 mm) was used in the report, a larger working channel endoscope (diameter 4.1 mm, outer diameter 6.9 mm, Richard Wolf GmbH, Knittlingen, Germany) is widely used in Japan. Therefore, a narrow interlaminar window is more challenging with use of a larger working channel endoscope. On the other hand, the larger working channel enables the use of a larger operative instrument such as a high-speed drill (14,15). To overcome the limitation of the interlaminar window, we used a high-speed drill to enlarge the window. We successively treated three patients using this new technique, and further discuss modification of the ILA for the treatment of highly migrated LDH.
Case presentation (Figures 1-5)
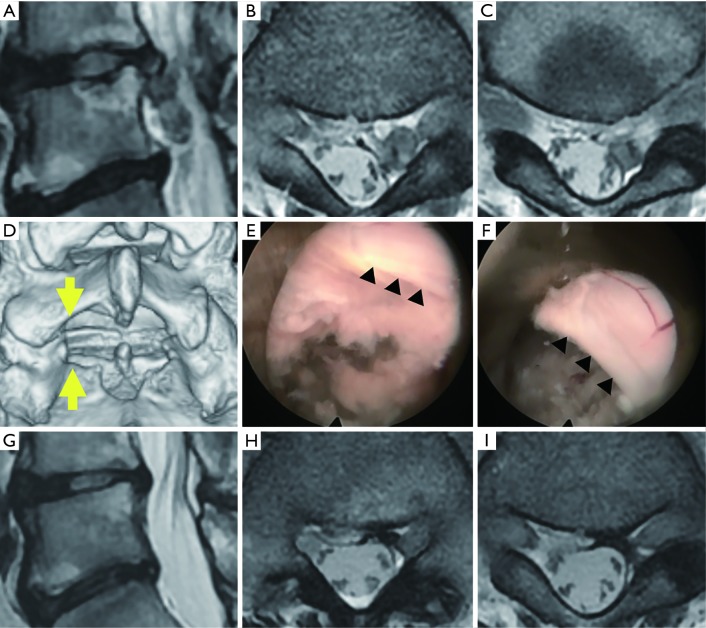
Figure 1.
Pre- and postoperative radiographic and intraoperative findings in a patient with highly down-migrated lumbar disc herniation (case 1). (A-C,G-I) Pre- (A-C) and postoperative (G-I) magnetic resonance imaging findings: sagittal (A,G) and axial (B,C,H,I) views of the T2-weighted image; (D) three-dimensional computed tomography: arrows indicate insertion area of the endoscope at L5/S1 interlaminar bone window; (E,F) intraoperative photographs: before (E) and after (F) the removal of the sequestrated nucleus. Arrowheads indicate left margin of the dural sac.
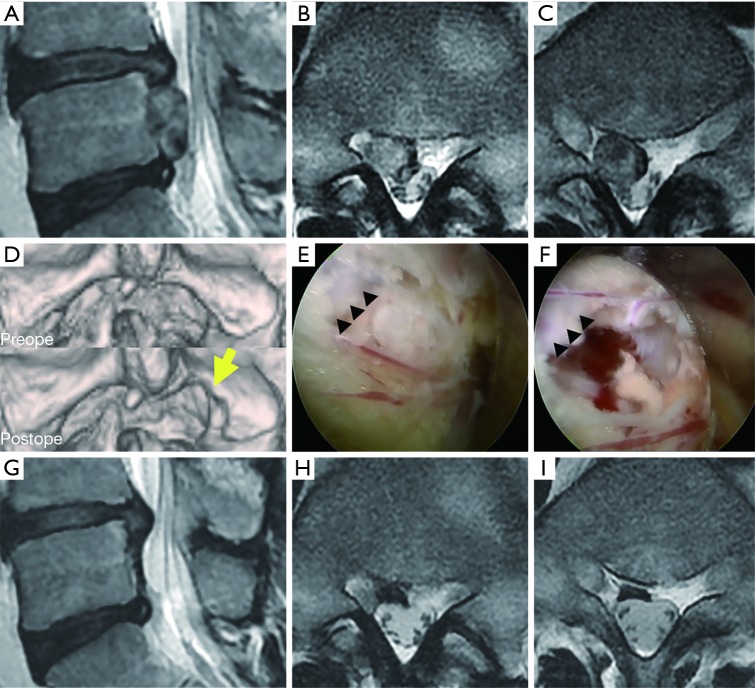
Figure 2.
Measurement of cranio-caudal length of the interlaminar space. (A,C,E) Axial computed tomography at L5/S1 disc level: solid yellow lines indicate the sagittal plane for measurement of cranio-caudal length of the interlaminar space. Note that the lines are located outside the lateral border of the dural sac; (B,D,F) sagittal computed tomography at corresponding solid yellow line: yellow dotted line indicates the cranio-caudal length. This line starts at the angle change point on the inner surface of the L5 vertebral laminae and ends at the cranial margin of the sacral bone. (A,B), (C,D), and (E,F) indicate cases 1, 2, and 3, respectively.
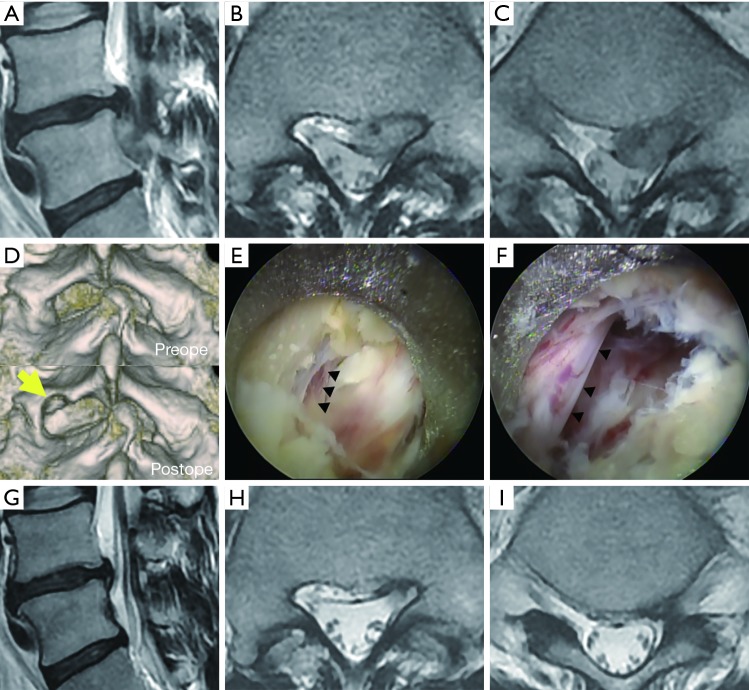
Figure 3.
Pre- and postoperative radiographic and intraoperative findings in a patient with highly down-migrated lumbar disc herniation (case 2). (A-C,G-I) Pre- (A-C) and postoperative (G-I) magnetic resonance imaging findings: sagittal (A,G) and axial (B,C,H,I) views of the T2-weighted image; (D) three-dimensional computed tomography: arrows indicate minimal laminectomy of the caudal margin of the right L5 vertebral laminae; (E,F) intraoperative photographs before (E) and after (F) the removal of the sequestrated nucleus. Arrowheads indicate right margin of the dural sac covering with epidural fat.
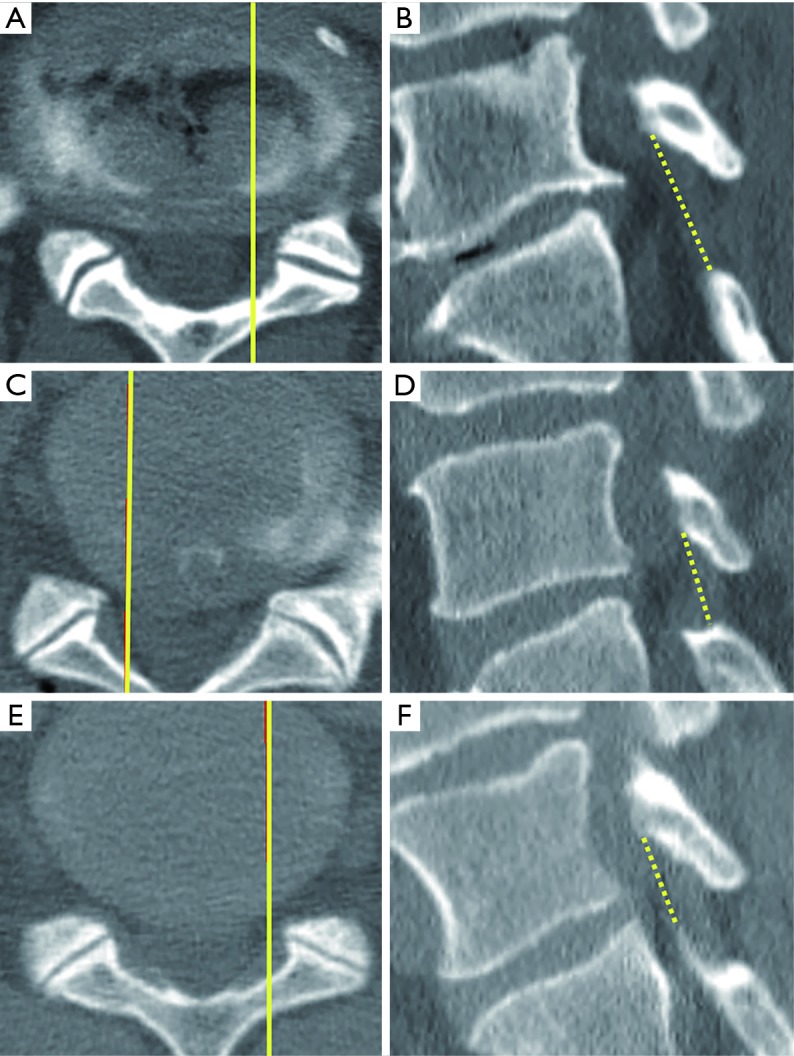
Figure 4.
Pre- and postoperative radiographic and intraoperative findings in a patient with highly down-migrated lumbar disc herniation (case 3). (A-C,G-I) Pre- (A-C) and postoperative (G-I) magnetic resonance imaging findings: sagittal (A,G) and axial (B,C,H,I) views of the T2-weighted image; (D) three-dimensional computed tomography: arrows indicate minimal laminectomy of the caudal margin of the left L5 vertebral laminae; (E,F) intraoperative photographs before (E) and after (F) the removal of the sequestrated nucleus. Arrowheads indicate caudal margin of the left L5 nerve root.
Figure 5.
Intraoperative video in a patient with highly down-migrated lumbar disc herniation (case 3): after minimal laminectomy, we could insert the endoscope into the spinal canal (16). Available online: http://www.asvide.com/article/view/25604
Case 1
A 61-year-old man presented with lower back pain (LBP) and left leg pain (both L5 and S1 dermatomes) that started 3 months before visiting our outpatient clinic. Although neurological examination revealed a positive straight-leg rising sign (SLR) at 20° on the left side, no apparent muscle weakness was observed. His symptoms were resistant to medical treatment (pregabalin 225 mg) and nerve root block. Lumbar magnetic resonance imaging (MRI) revealed an extremely down-migrated LDH at the L4/5 disc level. The caudal end of the sequestrated fragment reached to the lower endplate of the L5 vertebra and was located in the axillary area (between the L5 nerve root and dural sac) (Figure 1A,B,C). Three-dimensional (3D) computed tomography (CT) demonstrated a large L5/S1 interlaminar bone window (cranio-caudal length of the interlaminar space was 24 mm) (Figures 1D,2A,B; Table 1). We thought that the sequestrated nucleus could be extracted through this bone window and performed PELD-ILA. After insertion to the shoulder area of the left S1 nerve root, the endoscope (diameter of working channel: 4.1 mm, outer diameter: 6.9 mm) was tilted toward the L4/5 disc space and the sequestrated nucleus was pulled out (Figure 1E,F). Immediately after the operation, the leg pain improved. Postoperative MRI revealed complete disappearance of the extremely down-migrated LDH (Figure 1G,H,I).
Table 1. Clinical features of the three cases.
| Case no. | Age (years) /sex | Location | Width of interlaminar space (mm)* | Cranio-caudal length of interlaminar space (mm)** | mJOA score | Recovery rate (%) | NRS score | Partial laminectomy | Operation time (min) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level | R/L | Preoperative | Postoperative | Preoperative | Postoperative | |||||||
| 1 | 61/M | L4/5 | L | 28 | 24 | 14 | 22 | 88.9 | 3 | 0 | (−) | 61 |
| 2 | 44/M | L4/5 | R | 28 | 18 | 7 | 18 | 56.3 | 5 | 1 | (+) | 72 |
| 3 | 34/M | L4/5 | L | 27 | 16 | 9 | 17 | 57.1 | 5 | 0 | (+) | 93 |
*, width of the interlaminar space was calculated as in our previous manuscript; **, cranio-caudal length of the interlaminar space was calculated according to the legend for Figure 2. mJOA, modified Japanese Orthopaedic Association scale; NRS, Numerical Rating Scale.
Case 2
A 44-year-old man presented with LBP and right leg pain (both L5 and S1 dermatomes) that started 2 months before visiting our outpatient clinic. Neurological examination revealed a positive SLR at 30° on both sides and apparent muscle weakness [extensor hallucis longus (EHL) 5/4, flexor hallucis longus (FHL) 5/4]. His symptoms were resistant to medical treatment (celecoxib 200 mg). Lumbar MRI revealed extremely down-migrated LDH at the L4/5 disc level. The caudal end of the sequestrated fragment reached to the lower endplate of the L5 vertebra and was located in the axillary area (between the L5 nerve root and dural sac) (Figure 3A,B,C). 3D-CT demonstrated a shorter cranio-caudal length (18 mm) than that in Case 1 (Table 1, Figures 2C,D,3D preoperative). We attempted PELD-ILA via the L5/S interlaminar bone window. As it was difficult to insert the endoscope to the shoulder area of the right S1 nerve root, we removed a small part of the caudal margin of the L5 vertebral laminae using a 3.5-mm diameter high-speed drill (Figure 3D postoperative). Subsequently, the endoscope was inserted and tilted toward the L4/5 disc space and the sequestrated nucleus was pulled out (Figure 3E,F). Immediately after the operation, the leg pain improved. Postoperative MRI revealed a small residual fragment but compression of the nerve root and dural sac disappeared (Figure 3G,H,I).
Case 3
A 34-year-old man presented with LBP and left leg pain (both L5 and S1 dermatomes) that started 1 month before visiting our outpatient clinic. Neurological examination revealed a positive SLR at 60° on both sides and apparent muscle weakness [tibialis anterior (TA) 5/4, EHL 5/4]. His symptoms were resistant to medical treatment (loxoprofen 180 mg, Neurotropin 4 tablets, celecoxib 200 mg). Lumbar MRI revealed extremely down-migrated LDH at the L4/5 disc level. The caudal end of the sequestrated fragment reached to the lower endplate of the L5 vertebra and was located in the axillary area (between the L5 nerve root and dural sac) (Figure 4A,B,C). 3D-CT demonstrated a shorter cranio-caudal length (16 mm) than that in cases 1 and 2 (Table 1, Figures 2E,F,4D preoperative). We preoperatively planned to enlarge the L5/S1 interlaminar window and successfully pulled out the sequestrated nucleus (Figures 4E,F,5). Immediately after the operation, the leg pain improved. Postoperative MRI revealed complete disappearance of extremely down-migrated LDH (Figure 4G,H,I).
Discussion
PELD has an anatomical limitation for endoscope insertion, and there are three different operative approaches: interlaminar, transforaminal, and posterolateral. Several investigators have evaluated the PELD technique for highly migrated LDH (4-12), most studies described modifications of the transforaminal approach (4,6,7,9,11,12). Endoscope insertion using the transforaminal approach is a blind procedure, but can be safely performed via Kambin’s triangular working zone. In contrast, PELD-ILA has no such safety zone, and the entry to the spinal canal is performed under endoscopic visualization. We have found in many cases that the cranial side of the spinal canal as observed in PELD-ILA was wider than we had expected. We therefore designed an operative approach for highly down-migrated LDH through this wide visual field.
The direction of endoscope insertion is from caudal to cranial along the inner surface of the L5 vertebral laminae. The angle between the endoscope and caudal vertebral terminal plate of L5 is approximately 30–45°. This angle is narrower than that in conventional PELD-ILA. When tilting the endoscope, the cranio-caudal length of the interlaminar space is important to consider. Choi et al. proposed that a 7-mm-wide superior-inferior interlaminar space on the anteroposterior view was considered the minimum allowable width (13). As endoscopic insertion should be performed through the lateral side of the dural sac, we measured the more lateral side of the interlaminar window (Figure 2). In addition, as endoscopic insertion should also be performed along the inner surface of the L5 vertebral laminae, we defined the change point of the angle as the cranial starting point for measurement. Using this measurement, we confirmed that a shorter cranio-caudal length of the interlaminar space indicates the necessity for minimal laminectomy. Case 1 had a longer cranio-caudal length (Table 1, Figure 2A,B), due to a hypoplastic sacral bone at the cranial margin. Therefore, enlargement of the interlaminar bone window was not necessary. As Cases 2 and 3 had a shorter length (Table 1, Figure 2C,D,E,F), minimal laminectomy of the lateral caudal L5 vertebral laminae was required (Figures 3D,4D, arrows). The combination of a full endoscopic system and use of a high-speed drill through a long and narrow endoscopic lumen has created options for minimally invasive spinal surgery for highly migrated LDH.
Conclusions
We successfully treated three cases of highly down-migrated L4/5 LDH with PELD-ILA via the adjacent interlaminar space. The narrow interlaminar window was overcome with the use of a high-speed drill. The extent of laminectomy was minimal compared with that in conventional laminectomy. Although the presented cases are relatively rare, this new technique may also be applied to L3/4 LDH via L4/5 with a large interlaminar window and highly up-migrated L5/S LDH.
Acknowledgements
None.
Informed Consent: Informed consent was obtained from the patients for publication of this manuscript and any accompanying images.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Choi G, Lee SH, Deshpande K, et al. Working channel endoscope in lumbar spine surgery. J Neurosurg Sci 2014;58:77-85. [PubMed] [Google Scholar]
- 2.Sairyo K, Egawa H, Matsuura T, et al. State of the art: Transforaminal approach for percutaneous endoscopic lumbar discectomy under local anesthesia. J Med Invest 2014;61:217-25. 10.2152/jmi.61.217 [DOI] [PubMed] [Google Scholar]
- 3.Yeung AT. The Evolution and Advancement of Endoscopic Foraminal Surgery: One Surgeon's Experience Incorporating Adjunctive Techologies. SAS J 2007;1:108-17. 10.1016/S1935-9810(07)70055-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu X, Fan G, Guan X, et al. Percutaneous Endoscopic Lumbar Discectomy for Far-Migrated Disc Herniation through Two Working Channels. Pain Physician 2016;19:E675-80. [PubMed] [Google Scholar]
- 5.Du J, Tang X, Jing X, et al. Outcomes of percutaneous endoscopic lumbar discectomy via a translaminar approach, especially for soft, highly down-migrated lumbar disc herniation. Int Orthop 2016;40:1247-52. 10.1007/s00264-016-3177-4 [DOI] [PubMed] [Google Scholar]
- 6.Ying J, Huang K, Zhu M, et al. The Effect and Feasibility Study of Transforaminal Percutaneous Endoscopic Lumbar Discectomy Via Superior Border of Inferior Pedicle Approach for Down-Migrated Intracanal Disc Herniations. Medicine (Baltimore) 2016;95:e2899. 10.1097/MD.0000000000002899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JS, Choi G, Lee SH. Percutaneous endoscopic lumbar discectomy via contralateral approach: a technical case report. Spine (Phila Pa 1976) 2011;36:E1173-8. 10.1097/BRS.0b013e3182264458 [DOI] [PubMed] [Google Scholar]
- 8.Hu QF, Pan H, Fang YY, et al. Percutaneous endoscopic lumbar discectomy for high-grade down-migrated disc using a trans-facet process and pedicle-complex approach: a technical case series. Eur Spine J 2017. [Epub ahead of print]. 10.1007/s00586-017-5365-3 [DOI] [PubMed] [Google Scholar]
- 9.Choi KC, Lee DC, Park CK. A Novel Combination of Percutaneous Endoscopic Lumbar Discectomy and Epiduroscopic Laser Neural Decompression for Down-migrated Disc Herniation. Pain Physician 2017;20:E605-9. [PubMed] [Google Scholar]
- 10.Xin Z, Liao W, Ao J, et al. A Modified Translaminar Osseous Channel-Assisted Percutaneous Endoscopic Lumbar Discectomy for Highly Migrated and Sequestrated Disc Herniations of the Upper Lumbar: Clinical Outcomes, Surgical Indications, and Technical Considerations. Biomed Res Int 2017;2017. Available online: https://doi.org/ 10.1155/2017/3069575 [DOI] [PMC free article] [PubMed]
- 11.Liu C, Chu L, Yong HC, et al. Percutaneous Endoscopic Lumbar Discectomy for Highly Migrated Lumbar Disc Herniation. Pain Physician 2017;20:E75-84. [PubMed] [Google Scholar]
- 12.Ahn Y, Jang IT, Kim WK. Transforaminal percutaneous endoscopic lumbar discectomy for very high-grade migrated disc herniation. Clin Neurol Neurosurg 2016;147:11-7. 10.1016/j.clineuro.2016.05.016 [DOI] [PubMed] [Google Scholar]
- 13.Choi G, Prada N, Modi HN, et al. Percutaneous endoscopic lumbar herniectomy for high-grade down-migrated L4-L5 disc through an L5-S1 interlaminar approach: a technical note. Minim Invasive Neurosurg 2010;53:147-52. 10.1055/s-0030-1254145 [DOI] [PubMed] [Google Scholar]
- 14.Koga H, Inanami H. Minimal laminectomy using the interlaminar approach for percutaneous endoscopic lumbar discectomy. Mini-invasive Surg 2017;1:56-62. 10.20517/2574-1225.2017.04 [DOI] [Google Scholar]
- 15.Koga H. Improved percutaneous endoscopic translaminar approach for lumbar foraminal stenosis at L5/S1. Mini-invasive Surg 2017;1:3-5. 10.20517/2574-1225.2016.07 [DOI] [Google Scholar]
- 16.Inomata Y, Oshima Y, Inoue H, et al. Intraoperative video in a patient with highly down-migrated lumbar disc herniation (case 3): after minimal laminectomy, we could insert the endoscope into the spinal canal. Asvide 2018;5:595. Available online: http://www.asvide.com/article/view/25604