Abstract
Background
U and H-type sacral fractures are under diagnosed injuries resulting from significant axial loading that are often associated with neurological deficits. No studies to date have compared two common methods of surgical fixation, iliosacral screw fixation (ISF) and lumbopelvic fixation (LPF).
Methods
Patients with sacral fractures from 2009–2015 at one level 1 trauma center were identified by current procedural terminology (CPT) code and imaging reviewed for U/H type sacral fractures.
Results
Four hundred and fifty-three sacral fractures were identified during the study period, of which sixteen patients met inclusion criteria for the study. Six patients had the presence of a documented neurological injury at the time of presentation, 9 patients had concurrent spine fractures and 10 patients had concurrent pelvic fractures. Eight patients underwent ISF and 8 patients underwent LPF. There was no significant difference between the two groups in regards to age, intensive care unit (ICU) requirement, length of stay, or estimated blood loss. There was a significant increase in surgical time in the LPF group (P=0.002). In addition, there was a significant difference between those patients that underwent ISF that were discharged to a rehab facility compared to those treated with LPF (P=0.04).
Conclusions
Patients with U/H type sacral fractures can be treated with ISF or LPF without an expected increase in hospital length of stay (LOS) or need for ICU. Treatment with LPF may increase operative time however; the patient is more likely to be discharged to home instead of a rehab facility.
Keywords: U-type sacral fractures, spinopelvic dissociation, iliosacral screws, lumbopelvic fixation (LPF)
Introduction
Sacral fractures are an under diagnosed injury that often occur in conjunction with pelvic ring fractures (1). Approximately 50% of sacral fractures are not identified on initial evaluation and that number rises to 75% in the setting of a normal neurological exam (2). Furthermore, studies have demonstrated that only 30% of sacral fractures are appropriately visualized on an anterior-posterior (AP) pelvis radiograph; a standard procedure for an initial trauma evaluation of a patient (3). In the absence of a neurological deficit, computed tomography (CT) is the imaging study of choice; otherwise, magnetic resonance imaging (MRI) may be required in order to assess the integrity of the thecal sac and sacral nerve roots.
The age at which sacral fractures occur has a bimodal distribution which is generally related to the mechanism of injury. In young healthy patients, sacral fractures occur as a result of high-energy mechanism such as MVCs or a fall from height (4). However, in elderly patients sacral fractures can occur as a result of a ground level fall, especially in the setting of poor bone mineral density. The most important predictive factor in the prognosis of a sacral fracture is the presence of a neurological deficit. These deficits include lower extremity motor or sensory deficits, as well as urinary, sexual and rectal dysfunction; many of which can also develop if a sacral fracture remains untreated. In addition, untreated sacral fractures can also result in progressive deformity and chronic pain (5).
One subset of sacral fractures that can have devastating complications is U and H type sacral fractures. They consist of approximately 4–5% of all sacral fractures and have both a vertical and transverse component. Initially termed the “suicide jumpers” fracture, or lumbopelvic dissociation, they occur with significant axial loading (1). There is a high incidence of associated injuries, most often being other orthopaedic injuries, especially pelvis and lower extremity; however, there is a 20% incidence of chest injuries and a 12% incidence of significant brain injury. Furthermore, this fracture pattern has a high association of neurological deficits, reported to be as high as 94% in one study (6). The Roy-Camille classification is based on whether it is a flexion or extension angulation as well as the direction of translation and with increasing Roy-Camille score there is increased risk for neurological injury (7).
The treatment options for U/H type sacral fractures are generally surgical, although some patients that present with sacral insufficiency fractures or are unable to tolerate surgery may be managed non-operatively. Surgical options include iliosacral screw fixation (ISF) (8), lumbopelvic fixation (LPF) (lumbar pedicle screws and pelvic screws) (9) and triangular osteosynthesis (combination of LPF with iliosacral screws. Cadaveric studies have demonstrated the latter to have the most biomechanically stable construct (4,10,11). At present, there is a paucity of data available comparing the outcomes of patients that have undergone surgical management of U/H type sacral fractures by various modalities. Thus, the aim of the current study is to compare surgical outcomes of U and H type sacral fractures with surgical management by either ISF or LPF .
Methods
Study population
Sacral fractures were identified by CPT code at one level 1 trauma center from 2004 until 2015. Inclusion criteria were U and H-type sacral fractures. Exclusion criteria included other types of sacral fractures and those U/H type sacral fractures managed non-operatively. Our outcomes measures included patient demographics, mechanism of injury, concurrent fractures, Roy-Camille classification, surgical variables such as surgical duration and estimated blood loss, length of hospital stay, discharge disposition and post-operative complications. Choice of procedure performed was based on surgeon preference (see Figure 1). Placement of iliosacral screws were performed by two fellowship-trained orthopaedic traumatologists, while LPF was performed by a single fellowship trained orthopaedic spine surgeon. The ISF procedure involved placement of bilateral iliosacral screws with fluoroscopic guidance. LPF involved placement of L4 and L5 pedicle screws, bilateral iliac screws and sacral decompression where appropriate. Post-operatively patients underwent CT to assess for fracture union prior to removal of hardware. The protocol for the current study was performed with approval from our institutional review board.
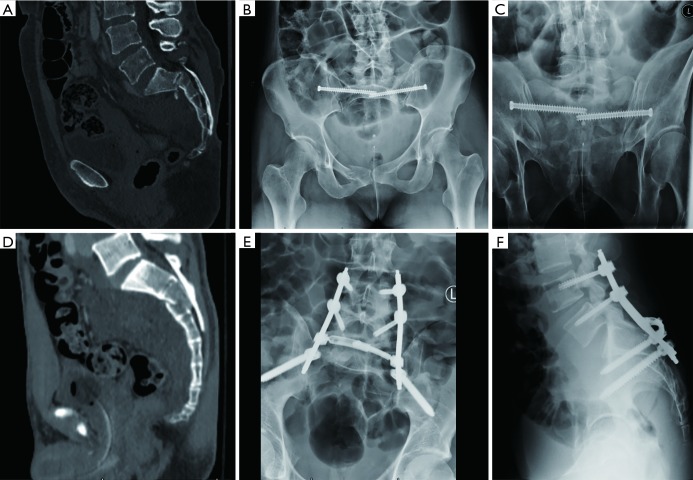
Figure 1.
(A) Sagittal CT cut and (B,C) post-operative inlet and outlet X-rays of a 51-year-old woman who underwent iliosacral screw fixation after sustaining a U-type sacral fracture after falling from a horse; (D) sagittal CT cut and (E,F) post-operative AP and lateral X-rays of a 26-year-old man who underwent lumbopelvic fixation after sustaining a U-type sacral fracture after sustaining a fall from a 30 ft roof. CT, computed tomography.
Statistics
An unpaired Student’s t-test was performed to assess for statistical differences between to two surgical treatments when appropriate (Graphpad Prism La Jolla, CA, USA). A Fisher’s exact test was used for determining the significant of categorical data. Differences were considered significant when P<0.05.
Results
Patient and fracture demographics
Of the 453 sacral fractures identified by CPT code between 2004 and 2015, 18 were found to be U or H type sacral fractures. One patient was excluded due to non-operative management and a second patient underwent decompression without instrumentation, resulting in 16 patients for the current study. The mean age at the time of injury was 46.5 (range, 16–80) years with a mean follow-up of 18 months [range, 1–52 months (see Table 1)]. Seven of the nine patients who were injured in a high-energy mechanism (MVC, fall from height, etc.) occurred in those patients under the age of 41 (range, 16–65) years. On the other hand, all 4 patients who were injured from low energy mechanisms (ground level falls, etc.) were over the age of 64.
Table 1. Patient demographics.
| Variables | n ± SD [range] |
|---|---|
| No. of patients | 16 |
| Age at time of injury (years) | 46.5±20.4 [16–80] |
| Male:female ratio | 5:11 |
| BMI (kg/m2) | 24.4±4.5 [18.7–35] |
| Duration of follow-up (mo) | 18±14.5 [1–52] |
| Mean hospital stay (days) | 16.8±10.9 [6–45] |
| Roy Camille classification | |
| 3 | 2 |
| 2 | 9 |
| 1 | 5 |
| Presence of neuro injury | |
| Paresthesias | 4 |
| Bowel/bladder injury | 2 |
| Cauda equina (or “impending”) | 3 |
| Concurrent injuries | |
| Spine fractures | 9 (56%) |
| Pelvic fractures | 10 (63%) |
| Mechanism of injury | |
| Fall from height | 6 |
| Motor vehicle collision | 3 |
| Ground level fall | 3 |
| Fall from horse | 1 |
| Snow mobile collision | 1 |
| Tractor accident | 1 |
| Low energy fall | 1 |
The majority of fractures were classified as type 2 using the Roy-Camille classification (56%) and presented with concurrent spine or pelvic fractures (56% and 63%, respectively). Six patients presented with a documented neurological changes (4 had lower extremity paresthesias, 2 had bowel or bladder incontinence) and two patients were found to have symptoms concerning for cauda equina syndrome with an additional patient was noted to have “impending” cauda equina syndrome. There was no pre-operative neurological exam documented for 2 patients due to altered mental status and concurrent head injury.
Comparison of ISF and LPF
There were eight patients that underwent ISF and eight patients that underwent LPF. LPF consisted of bilateral L4 and L5 pedicle screws and bilateral iliac screws. Of those who underwent LPF, seven of them also underwent sacral decompression and seven patients had their instrumentation removed within 12 months. One patient expired of unrelated causes prior to 12 months. There was a trend towards a younger age in those that underwent LPF (P=0.13; Table 2). The BMI was significantly lower in those patients that underwent LPF (26.9 vs. 21.5, P=0.03). There was a trend towards a higher Roy-Camille classification in those patients that underwent LPF (2.1 vs. 1.5, P=0.053). Those that underwent LPF had a significantly higher operative time, likely due to the concurrent sacral decompression at the time of surgery (326 vs. 89 min, P=0.0017). There was no significant difference between estimated blood loss between the two groups. However, two patients that underwent ISF also underwent additional pelvic procedures. One underwent simultaneous open reduction internal fixation (ORIF) of the acetabulum and another patient underwent simultaneous debridement of a sacral non-union and harvest of an iliac crest bone graft. Removal of these two patients from analysis resulted in a mean estimated blood loss of the ISF group to 25 mL, significantly lower than those that underwent LPF (P=0.01). There were two complications in the ISF group, one deep vein thrombosis (DVT) and one patient who developed a sacral non-union that ultimately underwent LPF. There were three complications in the LPF group—an intra-operative broken pelvic screw, a superficial wound infection requiring a return to the OR for irrigation and debridement and persistent bladder dysfunction. The majority of patients that presented with documented neurological symptoms improved post-operatively; however, one ISF patient with subjective numbness in her foot had a persistent foot drop that was treated with an ankle foot orthosis (AFO). One patient who had a delayed presentation (~6 weeks) with bowel and bladder dysfunction continued to report disturbances in bladder function at her most recent follow up (18 months post-surgery).
Table 2. Iliosacral fixation (ISF) vs. lumbopelvic fixation (LPF).
| Variables | ISF | LPF | P value |
|---|---|---|---|
| No. patients | 8 | 8 | |
| Age (years) | 54.5 | 38.5 | 0.13 |
| BMI (kg/m2) | 26.9 | 21.5 | 0.03 |
| Roy-Camille classification (mean) | 1.5 | 2.1 | 0.053 |
| EBL (mL) | 371 | 325 | 0.83 |
| Surgical time (min) | 89 | 326 | 0.0017 |
| ICU stay required | 3 | 2 | 1.00 |
| Length of hospital stay (days) | 17.4 | 19.6 | 0.74 |
| SNF placement | 7 | 2 | 0.04 |
| Complications | |||
| Non-union | 1 | 0 | |
| Persistent urinary dysfunction | 0 | 1 | |
| Wound infections | 0 | 1 | |
| Broken hardware | 0 | 1 | |
| DVT | 1 | 0 |
SNF, skilled nursing facility; DVT, deep vein thrombosis.
There was no significant difference in requirement of an intensive care unit (ICU) stay or overall length of stay for those treated with ISF or LPF. Five patients, overall, were admitted to the ICU upon presentation, 3 were due to a traumatic head injury and two for a higher level of care due to multiple traumatic injuries. However, there was a significant difference in the discharge disposition of the patients between the two groups. The majority of patients that underwent ISF were discharged to a skilled nursing facility, while the majority of patients that underwent LPF were discharged to home (P=0.04).
Discussion
A number of studies have examined the outcomes of U/H type sacral fractures that are currently available in the literature, however these have generally been in the setting of case reports, case series and small retrospective studies (reviewed in Konig et al.) (4). More recently, Mirzashahi et al. have reported the surgical treatment of sacral fractures using either ISF or LPF; however, the study included all sacral fractures, and only five of the 27 sacral fractures identified would be classified as U/H type sacral fractures, all of which underwent LPF (12). The present study is the first to retrospectively compare surgical outcomes with two different methods of operative management of U/H type sacral fractures.
The present study identified 18 U/H type sacral fractures, which is approximately 4% of all sacral fractures, a prevalence similar to that observed in previous studies; 16 of which satisfied inclusion criteria (1,3). We observed a bimodal distribution of injuries and ages—those that occurred in younger patients were more likely to be a result of a high-energy mechanism. As expected, a majority of patients had concomitant pelvic or spine fractures and alterations in neurological status at presentation. There was no significant difference in age, length of hospital stay or admission to the ICU with treatment of either ISF or LPF. However, there was a significant increase in operative time and estimated blood loss in the setting of an isolated sacral injury in the LPF group and a higher likelihood that those patients would be discharged to home instead of a skilled nursing facility.
There are a few studies currently in the literature that have examined outcomes in the surgical management of U/H-type sacral fractures; however, these have been limited to one type of surgical fixation. Nork et al. provided a retrospective review of 13 patients with U/H-type sacral fractures treated by ISF revealing that all patients demonstrated radiographic healing of their fracture, improvement in neurological function without significant changes in the degree of sacral kyphosis (8). On the other hand, Schildhauer et al. and Bellabarba et al. retrospectively examined patients with U/H-type sacral fractures treated with sacral decompression and LPF (9,13). Their study revealed that LPF also provides a stable construct for fixation in which all patients were radiographically healed with a significant improvement in the degree of kyphosis and a majority of their patients demonstrating neurological improvement post-operatively. The percentage of patients demonstrating neurological improvement in the latter study was lower than that observed in the study by Nork et al., however the initial degree of kyphosis was less than that observed in the study by Schildhauer et al. (27 vs. 43 degrees) (8,9,13). There are no current studies, to our knowledge, that have directly compared surgical outcomes of LPF and ISF in the treatment of U/H-type sacral fractures. Our methodology of LPF also differed than that of Schildhauer’s study given that our patients underwent decompression without arthrodesis in order to allow for fracture healing and removal of instrumentation at a future date. On CT imaging all fractures had healed uneventfully and instrumentation was removed 6 to 12 months post-operatively.
In the present study, there was a significant difference in BMI and a trend towards a significant decrease in age in those treated with LPF compared to those treated with ISF. However, the difference in age observed is likely confounded by the higher likelihood of a high-energy mechanism of injury. In addition there was a trend towards treatment of more severe injuries (or those with a higher classification in the Roy-Camille classification system) with LPF. As expected, there was a significantly higher operative time and a higher estimated blood loss with treatment with LPF compared to an isolated ISF procedure. These differences are attributed to the concurrent sacral decompression that occurred in the majority of patients undergoing LPF. It is difficult to fully assess any significant differences in complication rates given the small size of the study; the present study had five documented complications overall (DVT, superficial wound infection, broken instrumentation, persistent urinary dysfunction and a sacral non-union). These complications are similar to that which has been previously published where wound infection was the most common complication found in patients (14%), however a number of case reports examined previously did not report complications (4,13).
Of the 14 patients in the current study that were able to give an appropriate neurological assessment pre-operatively, six were found to have either bowel or bladder dysfunction, paresthesias or symptoms concerning for cauda equina syndrome. The majority of these patients had resolution of their neurological symptoms post-operatively whether treated with ISF or LPF. The incidence of pre-operative neurological injury in the present study is somewhat lower that what has been observed in similar sized retrospective studies (70–100%) (8,9,13). However, this is likely due to the fact that many of the patients in the present study have a lower degree of kyphosis (Roy-Camille type 1 and 2) than those in the above-mentioned studies and thus would be less likely to present with a neurological deficit. Despite differing incidences of pre-operative neurological dysfunction, this study is in agreement with others in that the majority of patients have demonstrated improvement in post-operative neurological function (8,9,13).
There was no significant difference between the ISF and LPF groups regarding admission to the ICU stay or overall length of stay. On the other hand, there was a significant difference in the discharge of patients to a skilled nursing facility; the majority of patients that underwent LPF were discharged to home or a psychiatric facility while the majority of patients that underwent ISF were discharged to a skilled nursing facility. At our institution, patients that undergo ISF for U- or H-shaped sacral fractures are restricted from bearing weight on their bilateral lower extremities for 12 weeks, while those undergoing LPF are allowed to immediately weight bear on bilateral lower extremities, initially with a walker for assistance. These restrictions are similar to those observed in other studies (8,9). The significant difference in discharge disposition observed in the present study is likely due these differences in weight bearing statuses with the two procedures. In line with this theory, one of the two LPF patients discharged to a skilled nursing facility had additional lower extremity injuries (calcaneus and foot fractures) that required restricted weight bearing of bilateral lower extremities for 6–8 weeks.
The current study provides important data regarding the outcomes of surgical treatment of U/H-type sacral fractures and can aid in the clinical management of these injuries. There is ongoing controversy as to whether the best management of these fractures would fall under the care of orthopaedic traumatologists or spine surgeons (14). In the current study, one fellowship-trained spine surgeon performed all LPF procedures, while two fellowship-trained traumatologists performed the ISF procedures. However, there was communication between the two specialties to determine the optimal treatment for these patients. The direct comparison of the two surgical treatments in the current study may also suggest important patient characteristics that aid in the decision-making process for the treatment of these patients given that a gold standard algorithm does not exist. For example, despite a longer operative time, the benefits of immediate weight bearing with LPF may be important in the setting of patients with concurrent injuries that would leave them at an elevated risk of pneumonia or other pulmonary complications. On the other hand, patients with significant lower extremity injuries that require fixation and resultant non-weight bearing status may be better suited for treatment with ISF if there is concern that the patient may not tolerate the increased operative time and blood loss.
There are a number of limitations to the present study—there is a small sample size due to the rarity of the fracture. However, our incidence in the setting of overall sacral fractures does mirror that which was published previously (1). Furthermore, the study is retrospective and thus has the limitations inherent to retrospective analysis. In addition, there were multiple surgeons involved in the study and the procedure performed was based on clinical preference and judgment. Finally, given its retrospective nature, patient reported outcomes are not available and thus it remains unknown whether there are differences in functional status following both procedures with validated methods of comparison.
Conclusions
The study presented here demonstrates that U/H type sacral fractures can be treated with either LPF or ISF without an expected difference in length of stay or need for ICU. On the other hand, treatment with LPF increases overall operative time and estimated blood loss if it is an isolated sacral fracture. However, it also allows for immediate weight bearing and thus is more likely to result in a discharge home instead of to a skilled nursing facility.
Acknowledgements
None.
Ethical Statement: The protocol for the current study was performed with approval from our institutional review board.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Mehta S, Auerbach JD, Born CT, et al. Sacral fractures. J Am Acad Orthop Surg 2006;14:656-65. 10.5435/00124635-200611000-00009 [DOI] [PubMed] [Google Scholar]
- 2.Hunt N, Jennings A, Smith M. Current management of U-shaped sacral fractures or spino-pelvic dissociation. Injury 2002;33:123-6. 10.1016/S0020-1383(00)00179-0 [DOI] [PubMed] [Google Scholar]
- 3.Yi C, Hak DJ. Traumatic spinopelvic dissociation or U-shaped sacral fracture: a review of the literature. Injury 2012;43:402-8. 10.1016/j.injury.2010.12.011 [DOI] [PubMed] [Google Scholar]
- 4.Konig MA, Jehan S, Boszczyk AA, et al. Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J 2012;21:829-36. 10.1007/s00586-011-2125-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gribnau AJ, van Hensbroek PB, Haverlag R, et al. U-shaped sacral fractures: surgical treatment and quality of life. Injury 2009;40:1040-8. 10.1016/j.injury.2008.11.027 [DOI] [PubMed] [Google Scholar]
- 6.Lehman RA, Jr, Kang DG, Bellabarba C. A new classification for complex lumbosacral injuries. Spine J 2012;12:612-28. 10.1016/j.spinee.2012.01.009 [DOI] [PubMed] [Google Scholar]
- 7.Roy-Camille R, Saillant G, Gagna G, et al. Transverse fracture of the upper sacrum. Suicidal jumper's fracture. Spine (Phila Pa 1976) 1985;10:838-45. 10.1097/00007632-198511000-00011 [DOI] [PubMed] [Google Scholar]
- 8.Nork SE, Jones CB, Harding SP, et al. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 2001;15:238-46. 10.1097/00005131-200105000-00002 [DOI] [PubMed] [Google Scholar]
- 9.Schildhauer TA, Bellabarba C, Nork SE, et al. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma 2006;20:447-57. 10.1097/00005131-200608000-00001 [DOI] [PubMed] [Google Scholar]
- 10.Schildhauer TA, Josten C, Muhr G. Triangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma 1998;12:307-14. 10.1097/00005131-199806000-00002 [DOI] [PubMed] [Google Scholar]
- 11.Schildhauer TA, Ledoux WR, Chapman JR, et al. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma 2003;17:22-31. 10.1097/00005131-200301000-00004 [DOI] [PubMed] [Google Scholar]
- 12.Mirzashahi B, Farzan M, Sadat M, et al. Surgical Treatment of Sacral Fractures: A Case Series Study. J Orthop Trauma 2015;1:e2061. [Google Scholar]
- 13.Bellabarba C, Schildhauer TA, Vaccaro AR, et al. Complications associated with surgical stabilization of high-grade sacral fracture dislocations with spino-pelvic instability. Spine (Phila Pa 1976) 2006;31:S80-8; discussion S104. [DOI] [PubMed]
- 14.Lindtner RA, Bellabarba C, Firoozabadi R, et al. Should Displaced Sacral Fractures Be Treated by an Orthopedic Traumatologist or a Spine Surgeon? Clin Spine Surg 2016;29:173-6. 10.1097/BSD.0000000000000385 [DOI] [PubMed] [Google Scholar]