Abstract
Objective:
This systematized literature review identified reports describing epilepsy misconceptions in the developed Western countries and research interventions focused on reducing these misconceptions.
Materials and Methods:
English language publications from January 2004 to January 2015 that described original research conducted in Europe, North/Central/South America or Australia on misconceptions about epilepsy among the general public.
Results:
81 publications were selected. Most studies were conducted in the Americas (N=30) and Europe (N=31). Misconceptions and attitudes about epilepsy were assessed among clinical providers (N= 9), family members of people with epilepsy (PWE, N=5), teachers (N= 11), students (N=22), and the general public (N= 25). Most studies used structured questionnaires, sometimes adding open-ended questions. Misconceptions reflected socially exclusionary attitudes directed at PWE, ignorance about treatment, and over-generalizations that are stigmatizing when applied to all PWE. Misconceptions were more prevalent in those with less education, lower socioeconomic status, and no exposure to PWE. There were only 12 intervention studies. While intervention studies were generally effective in improving attitudes, many were targeted to healthcare and education settings, were time intensive, and impractical for broad general population implementation. None incorporated newer technology-based strategies regarding effective health communication approaches.
Conclusions:
Types of epilepsy misconceptions were similar in reports published over the last decade, although most referred to misconceptions that have already been previously described. Existing questionnaires may fail to identify more subtle forms of current misconceptions and negative attitudes. Few interventional studies specifically target epilepsy stigma. Practical and broad scalable approaches to de-stigmatize epilepsy may help reduce misconceptions.
Keywords: epilepsy, seizures, stigma, misconceptions, health communication
Introduction
Throughout history, epilepsy has been a misunderstood and highly stigmatized disorder. The word itself comes from ancient Greek and refers to “being seized by forces from without,” a reference to the supposed supernatural origins of the disease.1 Divine retribution, demonic possession, and contagion have been common explanations for seizures, and until the late 1800s, people with epilepsy (PWE) were often incarcerated as “criminally insane.”
Over time, negative attitudes toward PWE have diminished,2 yet a significant proportion of the population remains uninformed and stigma is still a major source of stress and limitations for PWE. The Global Campaign Against Epilepsy (GCAE): Out of the Shadows, a joint venture from the World Health Organization, the International League Against Epilepsy, and the International Bureau of Epilepsy, was established in 1997 with the mission of improving acceptability, treatment, services, and prevention of epilepsy worldwide.3 Perhaps appropriately, the primary focus of the GCAE has been in the developing world, where the stigma and dearth of knowledge concerning epilepsy have been the most severe. There is a large literature on the subject and some improvements for PWE living in these regions of the world.
By comparison, in Western developed countries, the degree of misconceptions and stigmatizing attitudes is unclear, even with national laws such as the Americans with Disabilities Act (ADA) and Individuals with Disabilities Education Act (IDEA). Relatively less effort has focused on the myths and misconceptions surrounding epilepsy in modern Western society, the impact on PWE, and means to overcome these misconceptions and stigma.
The Institute of Medicine (IOM) highlighted epilepsy stigma as an important priority, stressing the continuing negative effects of stigma on PWE.4 Stigmatized PWE have lower self-esteem, greater social isolation, poorer psychological health, lower quality of life, and worse epilepsy control.5–10 The IOM noted some specific public health initiatives to reduce stigma associated with epilepsy and other conditions, but there is still substantial room for improvement and adaptation of other successful approaches, such as stigma reduction initiatives for mental health disorders need to be considered 11–13 Initiatives to reduce mental health stigma can potentially inform new strategies to change attitudes and facilitate a supportive, positive, and socially inclusive environment for PWE.
We sought to understand the recent literature on misconceptions and stigma surrounding epilepsy in Western societies and to identify key information relevant to understanding and modifying these misconceptions in order to limit stigma in our own society. To this end, we conducted a literature review focused on epilepsy stigma over the last decade and identified key epilepsy stigma themes in these studies. We were especially interested in research that evaluated epilepsy stigma reduction interventions and summarized the specific formats and health communication approaches in which the stigma-reduction interventions were delivered.
Materials and Methods
Our investigations involved three levels of literature review all focused on manuscripts published from 2004 to January 2015 to ensure contemporary relevance: 1) A survey of the original reports on epilepsy stigma with emphasis on country or region of the world of origin; 2) A systematic review of those original reports that addressed misconceptions and attitudes of the general public (people without epilepsy) toward PWE in Western countries; and 3) A focused assessment of articles presenting interventions specifically designed to reduce epilepsy stigma in Western settings.
1.1. Literature Review Search Strategy
PubMed, Web of Science and PsycINFO databases were searched for original research studies and reviews published in English between 2004 and January 2015. Search terms used were seizure*, epilepsy, myth*, misconception*, stigma, bias, restriction*, discrimination*, with keyword 1: epilepsy or seizure*, and keyword 2: myth* or misconception* or stigma or bias or restriction*or discrimination*; (*) was used as wildcard, to include several forms of the terms. A second search was done using Web of Science, with the same keywords, and intervention* or program* or education* as second keywords.
Another, less detailed search was done using Web of Science using keywords along with discrimination*, restriction*, myth* or stigma, as secondary keywords. Results from this search were used to identify articles based on the country or region of origin (where research was conducted) and the type of report (original, meta-analysis, review), in order to determine the geographical distribution of research projects on epilepsy myths and stigma. As much of this literature was combined with literature on health-related quality of life (HRQOL), HRQOL literature was included if it appeared to address stigma. Articles that addressed very specific situations (e.g. stress surrounding epilepsy surgery) were excluded.
1.1.1. Literature reflecting the Western world
Inclusion criteria were 1) Studies of misconceptions about epilepsy among people who did not have epilepsy in the general population or in subgroups defined by role or occupation (e.g. teachers, college students); 2) Original research (randomized controlled trials, prospective non-randomized controlled and uncontrolled studies); and 3) Published in English. Reviews on epilepsy stigma from Europe, the Americas, and Australia were also used to identify additional studies potentially missed in the initial search. We excluded studies focused on self-perceived stigma in PWE. Studies that reported on both PWE and those without epilepsy were only included if the non-epilepsy group misconceptions were reported separately. The search results used to illustrate the distribution of research projects on epilepsy myths and misconceptions included all countries and research on both felt and enacted stigma. This systematic review focused on stigma attitudes as reported in the general population and not stigma experienced or reported by PWE.
1.1.2. Interventional Studies
In order to help inform the planning of future intervention studies, each interventional study was assessed for the specific health communication strategies used to deliver anti-stigma messages. Because this team of investigators is developing a stigma reduction approach targeted to young adults in the general public, we flagged as a particular area of focus, those interventions targeted to a young adult audience.
1.2. Selection of publications
All abstracts were pre-screened by one reviewer for relevance, based on title and abstract information. Abstracts were then assessed by a five-member review team for inclusion. Initially, all reviewers evaluated a list of the same 20 abstracts to ensure consistent application of inclusion/exclusion criteria. Discrepancies were discussed until consensus was reached and inclusion/exclusion criteria were refined as necessary. Once the inclusion/exclusion criteria were finalized, all abstracts were reviewed by two independent reviewers to determine suitability for further in-depth review.
1.2.1. Data collection, synthesis and reporting.
Reviewers used a structured data extraction form modeled on other systematic reviews and recommendations.14–17 Reports were also assessed to see whether they included 1) An active intervention to reduce epilepsy misconceptions or stigma, 2) A health communication approach, and 3) A focus on young adults aged 18–29 years.
Results
1.1. Literature Review
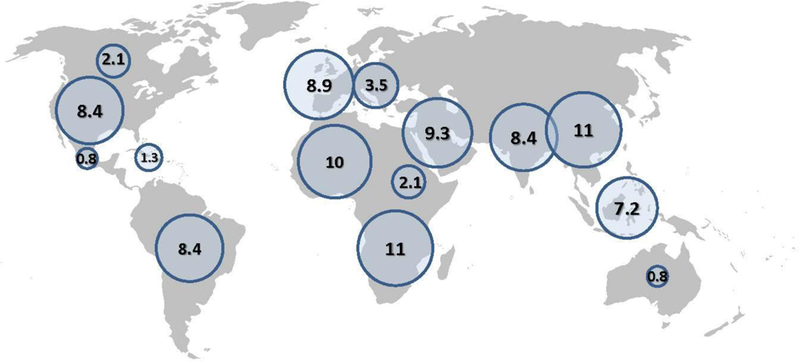
To understand the cultural and geographic emphasis on stigma in epilepsy research, we performed a Web of Science search for articles published between 2004 and 2015 referenced under the key word epilepsy or Seizure* combined with any of the words stigma, myth*, discrimination* or restriction*. After excluding duplicate references, references that were review papers, meta-analyses, editorials, or commentaries only without original data, and references that were very targeted to a very specific situation (e.g. epilepsy surgery), we identified 237 original research reports that examined stigma and related constructs. These included studies of attitudes of individuals in the general population as well as studies about felt stigma among PWE or their caregivers. We extracted information about the country or countries in which the research was performed based on the title when possible or review of the abstract. When necessary, we reviewed the methods section from the actual report. The countries were grouped by region of the world to demonstrate the relative amounts of research being performed in these different areas (Figure 2). Some studies did not fall into a single region (N=6) or where done based on on-line resources such as YouTube (N=4). They are not plotted but were included in the denominator.
Figure 2: Map of Epilepsy Research January 2004 – 2015.
1.2. Overall description of Western studies
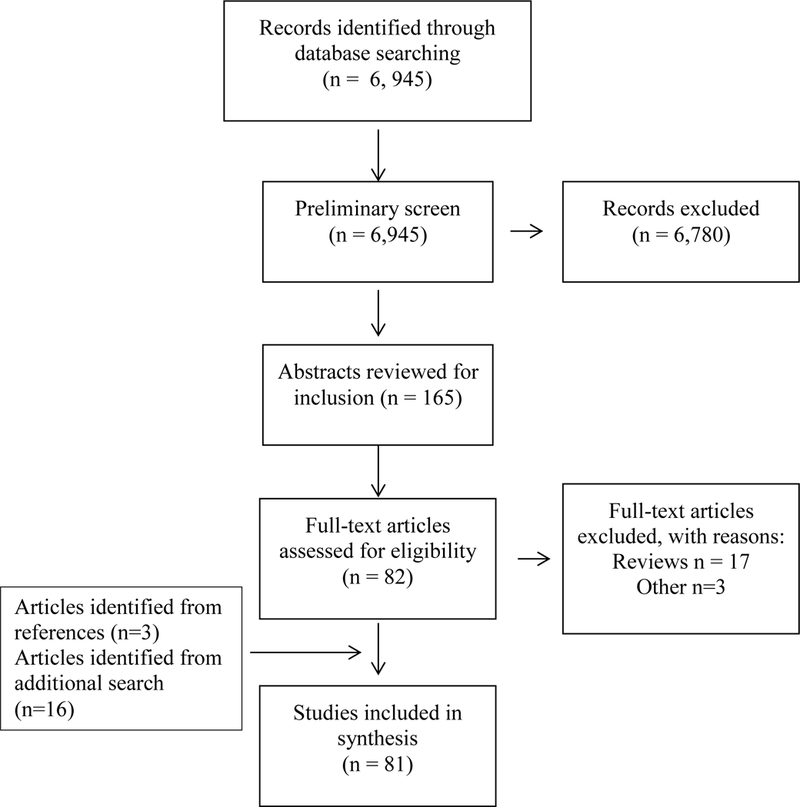
Eighty-one publications met inclusion criteria (Figure 1). Publication frequency is fairly uniform, except for a peak in 2007, which reflects several articles published by one group in Brazil (Figure 2). Most studies were from North America (N=27), Europe /Turkey, (N=32), and Central/South America (N=19). Two were from the Caribbean and one from Australia. The studies included assessment of misconceptions among clinical providers (N= 9), family members (N= 5), teachers (N= 11), students (elementary, secondary or professional schools, and universities) (N= 22), and the general public (N= 25). Eight studies analyzed social media content/sources including YouTube and Twitter. Studies were highly variable in format, design and quality.
Figure 1: Literature Review Flow Diagram.
Many studies combined assessment of knowledge and attitudes about epilepsy. Factual information about PWE was not always readily separated from some misconceptions; for example, while it is true that epilepsy does impose activity limitations (such as driving a car) for some PWE, it is not true that everyone with epilepsy is completely disabled.
1.3. Assessment of epilepsy misconceptions
Many studies used a structured, closed-ended questionnaire, either published previously by others or created by the authors, to assess epilepsy misconceptions, stigma or attitudes. A number of questionnaires were based on the surveys used by Caveness and Gallup.18,19–28 Bishop et al, developed a questionnaire based on the assessment of Antonak and colleagues.29–32 Fernandes et al, 33 developed the Stigma Scale of Epilepsy (SSE), which was used in a number of studies, often with some modifications. 34–40 Martiniuk et al, developed the “Thinking about epilepsy” questionnaire, which they used in a number of studies, 41–43 and Zanni et al, used the Brazilian version of The Epilepsy Beliefs and Attitudes Scale (EBAS).44
Only a handful of studies used open-ended, qualitative, or non-standardized formats for data collection. These provided some novel insights. A study from Mexico,45 which utilized in-depth interviews with patients, care-givers, and medical providers, indicated that if seizures were fully controlled, there was no epilepsy stigma, implying that patients might be to blame if their seizures were not adequately controlled.
1.4. Characterization of epilepsy misconceptions
1.4.1. Epilepsy misconception themes
Closed-ended instruments used to assess misconceptions tended to reflect beliefs or attitudes that have been previously well-established. Misconceptions (Table 1) fell into several categories: (A) Social status/integration; (B) Employment; (C) Associated conditions; (D) Restrictions and limitations; (E) Cause/Nature; (F) Treatment and prognosis; and (G) First Aid. There was a relatively high degree of similarity across studies that identified misconceptions, but given the diverse target populations and methodologies across studies, we could not compare how often these misconceptions occurred across various sub-groups.
Table 1:
Misconceptions categories identified in studies on epilepsy
| Examples | |
|---|---|
| Social status / integration | Concern about socializing and befriending PWE Concern about close physical proximity (afraid to sit beside a PWE) PWE should be isolated PWE cannot have normal social roles / should not participate in social activities Objection to marriage for PWE Concern about PWE having children Concern about children with epilepsy associating with other children and attending regular school Concern that children with epilepsy may not succeed in life Perception that PWE may not be successful in specific professions Perception that epilepsy is more common in a lower socio-economic class / Religious people have lower risk of epilepsy PWE are responsible for their condition Idea that one can identify a PWE by appearance PWE may transmit the disease ( i.e. epilepsy is contagious) PWE are a danger to the public Being a PWE is a disgraceful condition |
| Employment | Concern about hiring PWE Co-workers’ concern about working with PWE Associate negative features to PWE as employees Concern for safety of PWE and others in the workplace |
| Associated Conditions (primarily cognitive and psychiatric) | PWE have poor cognitive capacity / lower IQ / are mentally retarded Children with epilepsy (CWE) almost always have mental or learning problems -and usually cannot be very good students PWE have impaired self-realization/lower self-confidence PWE have difficult personalities; aggressiveness, violence and behavioral disorders PWE have severe psychiatric disease PWE tend to develop and express criminal tendencies |
| Restrictions and limitations | PWE cannot work or number of suitable jobs for PWE is low PWE should not drive, operate heavy machinery PWE should not attend regular school PWE cannot participate in sports |
| Cause/nature of epilepsy | Excessive suffering in childhood Epilepsy is a blood disease / immune disease Epilepsy is a physical deficiency / sign of weakness Epilepsy is a form of madness or a mental disorder Epilepsy is caused by possession or a “spell” /supernatural disease/the devil/ moon cycles Epilepsy is punishment for past sins/past life PWE are fated by God to have epilepsy Is caused by bad thoughts, depression Epilepsy is a disease that can kill PWE have lower life expectancy |
| Treatment | PWE can be treated better in institutions Epilepsy drugs have to be taken for life Most PWE do not take epileptic drugs Epilepsy is not curable or controllable Treatments are teas and medicinal herbs Faith can heal epilepsy/ask for God’s help/talismans/prayers Acupuncture Herbal medicine doctor/healer |
| First aid for seizures | Smelling something strong can end a seizure / spread vinegar or alcohol on patient’s wrist PWE can swallow their tongue during a seizure, therefore try to pull out the tongue Place something between their teeth Hold the person down/try to contain, throw water at them Necessity for immediate medical intervention in the form of an ambulance crew to stop a seizure |
1.4.2. Public perception of how epilepsy affects PWE
Several studies noted that survey respondents who do not have epilepsy expressed positive attitudes towards PWE, but also felt that PWE experience discrimination from society and difficulties in relationships and work. Respondents noted they would conceal a diagnosis of epilepsy because of those concerns.19; 22; 40; 46 In a study24 of healthy people visiting medical centers in Greece, when asked “If a person close to you was to have a disease which one would you “prefer” it to be?” and given a choice of five chronic conditions, respondents ranked epilepsy fourth out of five, behind diabetes and chronic respiratory or cardiac problems. Only psychiatric problems ranked below epilepsy. In the workplace, negative attitudes towards PWE are also evident.5; 47 Jacoby5 reported that for employees, working with a PWE would cause great concern, second to working with a person suffering from stress or depression. Studies seemed to indicate that while the general population did not typically voice stigmatizing ideas or thoughts, their attitudes indicate recognition that stigma exists.46–48
1.4.3. General population sources of information on epilepsy
A number of studies assessed sources of information about epilepsy. Mass media appears a common source of information.36; 49–51 However, reliance on mass media is not universal, as Degirmenci46 reported that less than 20% of respondents (mostly adults) got information from television, radio, internet, brochures or newspapers and magazines.
Eight studies focused on the portrayal of epilepsy in the news media and social media.52–59 Caspermeyer58 reported that approximately 15% of stories about 11 different neurological conditions contained stigmatizing language. However, there was no breakdown by neurological disease and no specific examples given of stigmatizing language. Perhaps the most informative study was by McNeil59 who performed a content analysis of Tweets containing the word “seizure*” over a 7-day period. Less than half of the Tweets contained information (12%), personal accounts (31%), and people seeking advice (2%). The other comments were categorized as ridicule and jokes (9%), metaphorical references to seizures (32%), opinions (6%), and miscellaneous comments (6%). Derogatory comments were present in 41% of over 5,000 tweets analyzed.
1.4.4. Variables associated with misconceptions and stigma
Epilepsy stigma was most likely to occur in individuals with less education, lower socioeconomic status, minorities and those with no exposure to PWE.19; 24; 40; 60; 61 Individuals at the more extreme younger or older age ranges also had more misconceptions.19; 22; 60
1.5. Interventions to reduce epilepsy stigma
Only 12 studies included an intervention (Table 2), and of these, only one was conducted in the United States.62 The number of participants in studies varied widely, from 20 to over 1,300. Most studies (N=9)26; 28; 51; 78; 79; 80; 81; 82; 84 were non-controlled prospective trials, three were randomized control trials.34; 42; 83 Interventions targeted primary and elementary students42; 51; 83 (N=3), high school students34 (N=1) and college students26; 28 (N=2) as well as school teachers78; 79; 81; 84 (N=4) and health professionals80; 82 (N=2). Consistent with the pedagogical and clinical settings, interventions relied on communicating health information via lectures or other formal, lengthy curricula to train or educate their target audiences. Studies presented factual information regarding management of seizures, implications of epilepsy, and first aid for someone who had a seizure via videos, lectures, and simulation to allow for cognitive shaping of attitudes. A combination lectures, courses, or seminars were mostly commonly used communication approaches78; 79; 80; 81 (N=4). Combinations of seminars, lectures, trainings, and courses were all classified under the same approach because there were no distinguishing factors in the brief methods sections in these intervention papers. Another popular intervention strategy28; 42; 83 (N=3) was an audio visual mixed modality that included discussion and/or role playing. Next, lecture only82 (N=1) or lecture with discussion51 (N=1) were used. Other strategies included simulation34 (N=1), video only26 (N=1), and education session with education kits84 (N=1). Overall the studies noted an improvement in epilepsy knowledge and improved attitudes towards PWE.
Table 2:
Research studies testing an intervention intended to improve epilepsy misconceptions or stigma
| Study | Country | Study Population & Design | Intervention Description |
Health Communication Approach |
Outcome Instrument and Results |
|---|---|---|---|---|---|
| Bekiroglu, Ozkan, et al. (2004)78 | Turkey | Primary school teachers (N= 346) Prospective, uncontrolled trial |
Seminars included 1. Four lectures about epilepsy causes and consequences as well as social, professional, and legal aspects of epilepsy 2. Training on attitude toward students with epilepsy and management of seizures. 3. Videos were used to show common types of epileptic seizures. Given by member of the Committee of Education of the Turkish League Against Epilepsy |
Seminars that included lectures, trainings, and videos | Developed own questionnaire measuring attitude toward epilepsy Improved awareness, knowledge, and attitudes, decreased misperceptions Post-seminar survey, no follow up |
| Aydin, Yildiz (2007)79 |
Turkey | Primary public school teachers (N=275) Prospective, uncontrolled trial |
45 minutes education program including a seminar on causes and consequences of epilepsy, social, professional, and legal implications of epilepsy, as well as instruction about attitudes toward students with epilepsy and first-aid management for seizures. Given by a pediatric neurologist |
Education program including seminar and instructions | Developed own questionnaire measuring perception of epilepsy (knowledge, attitude, and practice) Improved knowledge and attitudes and a positive change in epilepsy perception at one month follow-up |
| Fernandes, Noronha, et al. (2007)80 | Brazil | Physicians, health professionals (Module 1 N=194 in the pre-test, N= in both pre and post-test Module 2 N= 484 pre-test, 147 both pre and post-test) Prospective, uncontrolled trial |
Training consisting of three separate modules for different health professionals: Module 1. 8 hour information courses for physicians Module 2. 3 hour course for health professionals and community leader Module 3. “Training the trainers” course for physicians to help them deliver information about epilepsy to other health care providers in their communities |
Informational, multi-hour courses | Developed own questionnaire Improved knowledge, attitudes, and perceptions for both Modules 1 and 2 six months after courses |
| Fernandes, P. T., A. L. Noronha, et al. (2007)81
|
Brazil | Elementary education teachers (N=20, training course completers) Prospective, uncontrolled trial |
20 hour training course “Epilepsy and Health” with 8 hours about epilepsy and 12 hours about educational methods to use in class on the theme of epilepsy. |
Training course | Developed own questionnaire Improved knowledge, attitudes and perception at up to 2 years follow-up |
| Martiniuk, Speechley, et al. (2007)42 | Canada | Grade 5 students (N=783) Cluster randomized, controlled trial, with schools as unit of randomization |
A 30-minute ‘Thinking about Epilepsy’ educational program, using posters, photographs, a television commercial, a puppet show, and role playing |
Posters, photos, television commercial, puppet show, role play | Developed own questionnaire Improved knowledge and attitudes at 1 month follow-up |
| Reno, Fernandes, et al. (2007)34 | Brazil | Students of first year of high school (N= 182 pre/86 post) Randomized controlled trial |
Two groups were shown a simulation of a tonic-clonic seizure: one group was shown how to respond correctly; another group was shown incorrect response. A third group was the control that did not see a simulation and received no information about epilepsy. All subjects completed a questionnaire. |
Simulation | Used Stigma Scale of Epilepsy (SSE) plus three questions Improved attitudes in group given correct information |
| Smith, Siddarth, et al. (2007)82 | US | Pediatric neurologists (N=18) Pediatricians (N=17) Prospective, uncontrolled trial |
50 minute lecture on cognitive and behavioral impact of pediatric epilepsy as well as bio-psycho-social factors Information presented by a pediatric neuropsychiatrist with clinical and research experience in pediatric epilepsy |
Lecture | Developed own questionnaire Improved knowledge about impact of epilepsy in children |
| Tedrus, Fonseca, et al. (2007)28 | Brazil | University students in health sciences (N= 285 pre; N=116 post) Prospective, uncontrolled trial |
2 hour presentation of audio-visual material about biological and psychosocial aspects of epilepsy, followed by a brief discussion. Audio-visual material produced by the Brazilian League of Epilepsy |
Audio-visual material | Developed questionnaire based on Caveness and other surveys Improved knowledge and attitudes |
| Bozkaya, Arhan et al. (2010)51 | Turkey | Primary school students (N=851) Prospective, uncontrolled trial |
Lecture and discussion session presenting information on epilepsy. Educational strategies used included practice with a simulated patient, case-based discussion, and videos of seizures. |
Lecture and discussion | Developed own questionnaire Improved knowledge and attitudes improved |
| Roberts, Farhana (2010)26 | Australia | Undergraduate psychology students (N=131) Prospective, uncontrolled trial |
10 minute informational first aid video including testimonials, based on previous educational videos and national guidelines. Development by the Epilepsy Tasmania Association |
Video | Developed questionnaire based on Caveness and on DiIorio (ABLE) Improved knowledge and attitudes |
| Brabcova, Lovasova, et al. (2013)83 | Czech Republic | Elementary school students (N=1,342) Randomized (school level), controlled trial |
20 minute video (group 1) or interactive drama (group 2) with a narrative approach where one main character had epilepsy. Control group with no intervention (group 3) |
Video and interactive drama with narrative approach | Developed own questionnaire Improved knowledge and attitudes in interventions compared to control |
| Mecarelli, Messina, et al. (2015)84 | Italy | Primary school teachers (N= 582 pre; N=317 post) Prospective, uncontrolled trial |
Education session on epilepsy. Educational kits to share with the students. |
Education session and educational kits containing brochures, story (fairy tale), poster | Developed own questionnaire Improved knowledge but not attitudes |
In the literature on health communication strategies for epilepsy interventions, there was a focus on providing factual information/education. Outcomes suggested improved epilepsy knowledge and attitudes for various timeframes post-intervention (immediate to two years). However, these intervention studies did not assess whether this additional knowledge or change in attitude translated into measurable behavioral changes in real-world settings. Furthermore, how epilepsy stigma was addressed is not consistently obvious in the health communication interventions.
Discussion
Findings from this literature review on epilepsy stigma and stigma-reduction efforts suggests that although there is a substantial literature on misconceptions, negative attitudes, and stigma surrounding epilepsy from developing and non-Western countries, there is a relative paucity of recent information from the Americas, Europe and Australia, and a very limited literature on stigma-reduction strategies in these settings. Most of the literature relies on responses to the same kinds of questions from decades ago, which reflect what we would today consider unacceptable forms of negative attitudes, especially in our post-ADA society. Notably, we found relatively little utilization of qualitative methods to elicit new information that could then be used in innovative intervention programs. Key findings of this literature review and implications for future work are noted in Figure 3.
Figure 3: Key findings and research implications from a synthesis of a systematized literature review on epilepsy stigma.
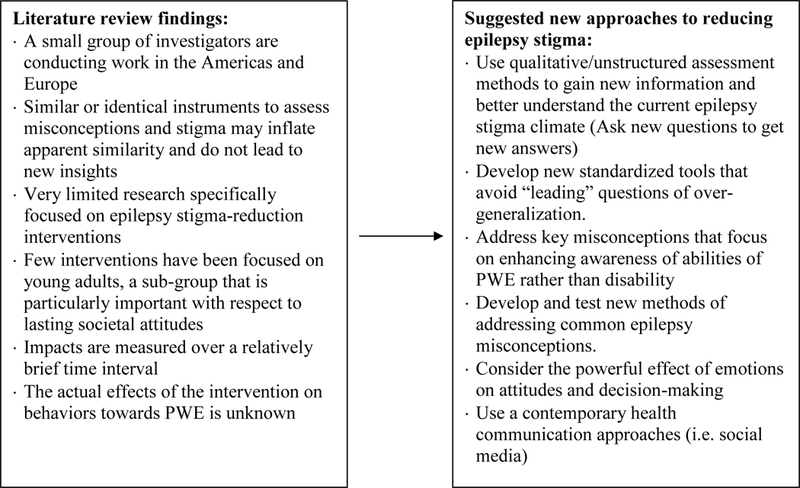
Key epilepsy misconception themes in the research literature over the past decade include limitations on normal social roles (socializing with PWE, marriage, children, employment), conditions associated with epilepsy (cognitive and behavioral difficulties and disabilities), personal characteristics of PWE (unreliable, dangerous), restrictions placed on activities (driving, sports), and inaccurate beliefs regarding the causes, treatment, and prognosis of epilepsy. Unfortunately, we could not compare the frequency and nature of misconceptions across population subgroups because of extensive variability in study design and methods.
Most published studies on epilepsy misconceptions and stigma used standardized instruments that relied upon closed-ended questions. Some epilepsy misconception questions in published reports were worded such that they invited over-generalization of items that can be true for some individuals and turned them into blanket statements about all PWE. For example, saying “epilepsy can kill” is an important message for PWE who are at risk of Sudden Unexpected Death in Epilepsy (SUDEP).63 However, portraying epilepsy as a lethal condition is unlikely to reduce stigma. For example, one could imagine that employers might be less likely to hire PWE if they think a person can die while having a seizure at work. Although PWE can have a variety of cognitive difficulties, most of these are relatively subtle and can be managed with appropriate compensatory approaches. Few studies used open-ended or qualitative methods that might provide a finer-grained understanding of current misconceptions and stigma. To arrive at different answers, it is important to ask new questions.
In the Americas, Australia, and Europe only a dozen interventional studies have been reported over the past decade targeting the general population which does not have epilepsy. Although the interventions in the 12 studies examined in this review improved attitudes about epilepsy, interventions were limited to healthcare and education settings and were time intensive and impractical to implement for the broad population.
This review suggests that published evidence on ways to best reduce epilepsy stigma in the general population is extremely limited. Summary findings demonstrate that both epilepsy knowledge and epilepsy attitudes can be improved with directed effort. While nearly all interventions appeared effective in improving epilepsy knowledge and attitudes in their respective target population, interventions mainly were intended for use in classroom or healthcare settings and used didactic delivery approaches that would not be expected to be practical or scale-able for the general population. Most importantly, their enduring impact was not assessed.
Given the paucity of evidence-based epilepsy stigma-reduction interventions, it may be reasonable to look at other stigmatizing disorder as to how future research might be operationalized. A mental illness stigma intervention protocol 64 suggests anti-stigma interventions should examine the effect on stigma and discrimination of people with mental illness as well as their caregivers. A similar research protocol would be applicable for research on stigma among people with epilepsy.
In marked contrast to the limited number of published research studies that tested interventions to address epilepsy stigma, there has been extensive work, most notably conducted by advocacy groups such as the Epilepsy Foundation (EF) and government agencies such as the Centers for Disease Control and Prevention (CDC), to implement public awareness campaigns that broadly address epilepsy awareness 65; 66 and which are intended to improve understanding, promote social inclusion, and reduce stigma. Subsequent to our literature review, Price and colleagues published a comprehensive summary of multi-faceted public education awareness campaigns that have been implemented in the U.S. from 2001–2013.65; 67 Targeted educational efforts by CDC and EF support groups such as school nurses, first responders, school staff, and adult day-care personnel.68
Consistent with recommendations by Corrigan69 suggesting that stigma reduction is most likely to be effective when it is targeted toward specific populations, has local relevance, and uses people from the targeted population to deliver the message, the EF and CDC campaigns targeted important subgroups including Tweens, African-Americans, Hispanic-Americans and Asian-Americans using communication approaches that leveraged the strength of mass and social media and included multiple formats such as audio and video release, celebrity endorsement and community events. A key feature of the public campaigns implemented thus far is their extraordinary reach. For example, the “26 Days of Epilepsy Awareness and Action” campaign in 2012–213 was delivered to more than 3 million individuals, including 1.9 million Asian-Americans. However, an important limitation of these public awareness efforts is that impact data mainly consisted of process outcomes that provided information on reach or uptake of the information (number of website visits, attendance, etc.) rather than specific effects of these efforts on epilepsy misconceptions and stigma.65
Health communication approaches used in interventions identified in this review used mainly lectures and videos. However, information provided through these means does not extend beyond the audience directly receiving the information. Effective health communication approaches need to engage individuals and communities in formats that are easily accessible and ideally without cost. Mass and multi-media health information can be delivered and shared at a rapid pace and potentially a larger audience. Future efforts to specifically target and reduce epilepsy stigma will almost certainly need to use technology-based approaches such as social media which might be expected to appeal to younger audiences. Novel communication technologies, including social network sites, text messaging, podcasts, blogs, and videos uploaded by organizations and Internet users are all potentially fruitful areas of investigation.70 The ease of user “sharing” of web-based content allows for the continual spread of information. Since none of the epilepsy intervention studies in this review used novel health communication mediums, these new mediums need to be tested.
In addition to the format of communication channels utilized, it is important to consider the message being communicated. Protest against stigma, which involves identifying instances of incorrect ideas or discrimination and speaking out against them, can result in worse discrimination because of the increased focus on instances where it occurs.69 Additionally, both cognitive beliefs (what a person believes is true/not true about PWE) and emotional responses that include fears about safety or risk can influence intentions for behavior that may result in avoiding PWE. 71; 72 Decision Theory posits that people have difficulty refuting negative information. Instead, correct positive information should be provided. 73 As an example, the statement “people with epilepsy aren’t stupid” plants the connection of epilepsy with stupidity in the listener’s mind. A preferred approach is to remain positive and avoid negative connections such as the statement “Most people with epilepsy are bright, engaged, and living full lives.” Emotions are potent drivers of decision-making74; 75 and positive emotional content, such as health communication approaches that emphasize caring, inclusiveness and altruism are known to be effective in shaping attitudes. 76; 77
Limitations
Our literature search was focused on studies published in 2004–2015. As with any search, we may not have identified all pertinent articles, and our search and review strategy may have introduced some bias. Furthermore, while we identified similar themes across studies, findings from non-U.S. studies might not generalize to the U.S. population. A limitation common to most of the studies we reviewed is “social desirability bias,” meaning that respondents may provide answers that they feel are socially appropriate, but not necessarily reflective of true attitudes and behavior. This could explain some of the subtle discrepancies among answers within the same questionnaire, such as the fact that individuals endorsed having positive attitudes towards PWE, but would still not disclose having epilepsy if they themselves had epilepsy. There are only a limited number of epilepsy stigma-reduction interventions and the relatively narrow audience focus of the existing interventions limits an approximation of how they might perform in general population samples.
Conclusions
As our review findings illustrate, types of epilepsy misconceptions were similar in reports published over the last decade, although most referred to misconceptions that have already been previously described. While some factors associated with stigmatizing misconceptions are non-modifiable, having no familiarity or exposure to a PWE appears associated with more misconceptions and may be an avenue for intervention within specific subgroups. There are remarkably few published research studies which specifically tested epilepsy stigma-reduction efforts. Techniques that re-frame stigmatizing beliefs, create positive affective reactions and can be implemented on a broad and easily-accessible population-level should be incorporated into the next generation of approaches to reduce epilepsy stigma.
Acknowledgements
This project was supported by a grant from the Centers for Disease Control and Prevention (1U48DP005030 SIP008). The authors would like to acknowledge the helpful suggestions of Rosemarie Kobau, Matthew Zack and Wanjun Cui from the Centers for Disease Control and Prevention (CDC).
This project was supported by a grant from the Centers for Disease Control and Prevention (1U48DP005030 SIP008).
Footnotes
Disclosures
As of March 2016, M Sajatovic is or has been (within the past 3 years) supported by the following research grants: Pfizer, Merck, Ortho-McNeil Janssen, Janssen, Reuter Foundation, Woodruff Foundation, Reinberger Foundation, National Institute of Health (NIH), and the Centers for Disease Control and Prevention (CDC). She is a consultant for Bracket, Prophase, Otsuka, Pfizer, and Sunovion. She also receives royalties from Springer Press, Johns Hopkins University Press, Oxford Press, UpToDate, and Lexicomp. All other authors have nothing to disclose. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Contributor Information
Lynn K. Herrmann, Northern Illinois University, College of Health and Human Sciences, DeKalb, Illinois.
Elisabeth Welter, Case Western Reserve University School of Medicine and Neurological and Behavioral Outcomes Center, University Hospitals Case Medical Center, Cleveland, Ohio
Anne T. Berg, Ann & Robert H. Lurie Children’s Hospital of Chicago, Epilepsy Center, and Northwestern Feinberg School of Medicine, Dept. Pediatrics. Chicago, Illinois.
Adam T. Perzynski, Center for Health Care Research and Policy. Case Western Reserve University, MetroHealth Medical Center, Cleveland, Ohio.
James Van Doren, Case Western Reserve University School of Medicine and Neurological and Behavioral Outcomes Center, University Hospitals Case Medical Center, Cleveland, Ohio.
Martha Sajatovic, Department of Psychiatry and of Neurology, Case Western Reserve University School of Medicine, Neurological and Behavioral Outcomes Center, University Hospitals Case Medical Center, Cleveland, Ohio.
References:
- 1.Temkin O The falling sickness: A history of epilepsy from the Greeks to the beginnings of modern neurology. Johns Hopkins University Press: Baltimore; 1994. [Google Scholar]
- 2.Caveness WF, Merritt HH, Gallup GH Jr. A survey of public attitudes toward epilepsy in 1974 with an indication of trends over the past twenty-five years. Epilepsia 1974;15:523–536. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization, International Bureau for Epilepsy. ILAE/IBE/WHO Global Campaign against Epilepsy. Out of the Shadows., 2003. Available at: http://www.who.int/mental_health/management/en/GcaeBroEn.pdf?ua=1.
- 4.Institute of Medicine. Committee on the Public Health Dimensions of the Epilepsies. EPILEPSY across the SPECTRUM. Promoting Health and Understanding. The National Academies Press; Washington, DC; 2012. [PubMed] [Google Scholar]
- 5.Jacoby A, Gorry J, Gamble C, et al. Public knowledge, private grief: a study of public attitudes to epilepsy in the United Kingdom and implications for stigma. Epilepsia 2004;45:1405–1415. [DOI] [PubMed] [Google Scholar]
- 6.Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurol 2005;4:171–178. [DOI] [PubMed] [Google Scholar]
- 7.Jacoby A, Austin JK. Social stigma for adults and children with epilepsy. Epilepsia 2007;48:6–9. [DOI] [PubMed] [Google Scholar]
- 8.A. Jacoby Stigma, epilepsy, and quality of life. Epilepsy Behav 2002;3:10–20. [DOI] [PubMed] [Google Scholar]
- 9.Bandstra NF, Camfield CS, Camfield PR. Stigma of epilepsy. Canadian Journal of Neurological Sciences 2008;35:436–440. [DOI] [PubMed] [Google Scholar]
- 10.Whatley AD, DiIorio CK, Yeager K. Examining the relationships of depressive symptoms, stigma, social support and regimen-specific support on quality of life in adult patients with epilepsy. Health Educ Res 2010;25:575–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins RL, Wong E, Cerully J, et al. Interventions to Reduce Mental Health Stigma and Discrimination.A Literature Review to Guide Evaluation of California’s Mental Health Prevention and Early Intervention Initiative In Editor (Ed)^(Eds) Book Interventions to Reduce Mental Health Stigma and Discrimination.A Literature Review to Guide Evaluation of California’s Mental Health Prevention and Early Intervention Initiative.; 2012. [PMC free article] [PubMed] [Google Scholar]
- 12.Yamaguchi S, Mino Y, Uddin S. Strategies and future attempts to reduce stigmatization and increase awareness of mental health problems among young people: A narrative review of educational interventions. Psychiatry Clin Neurosci 2011;65:405–415. [DOI] [PubMed] [Google Scholar]
- 13.Substance Abuse and Mental Health Services Administration. Available at: http://www.samhsa.gov/prevention.
- 14.Higgins J, Green Se. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. .
- 15.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Finding What Works in Health Care: Standards for Systematic Reviews. The National Academies Press: Washington, DC; 2011. [PubMed] [Google Scholar]
- 17.Berg AT, Shinnar S. Relapse Following Discontinuation of Antiepileptic Drugs - a Metaanalysis. Neurology 1994;44:601–608. [DOI] [PubMed] [Google Scholar]
- 18.Caveness WF, Gallup GH Jr. A survey of public attitudes toward epilepsy in 1979 with an indication of trends over the past thirty years. Epilepsia 1980;21:509–518. [DOI] [PubMed] [Google Scholar]
- 19.Bagic A, Bagic D, Zivkovic I. First population study of the general public awareness and perception of epilepsy in Croatia. Epilepsy & Behavior 2009;15:170–178. [DOI] [PubMed] [Google Scholar]
- 20.Bagic A, Bagic D, Zivkovic I. First population study of the general public awareness and perception of epilepsy in Bosnia and Herzegovina. Epilepsy & Behavior 2009;14:154–161. [DOI] [PubMed] [Google Scholar]
- 21.Bagic D, Mastilica M, Bagic A. A five-year follow-up study of the general public awareness and perception of epilepsy in Croatia. Epilepsy & Behavior 2012;25:200–207. [DOI] [PubMed] [Google Scholar]
- 22.Chung K, Ivey SL, Guo WT, et al. Knowledge, attitudes, and practice toward epilepsy (KAPE): A survey of Chinese and Vietnamese adults in the United States. Epilepsy & Behavior 2010;17:221–227. [DOI] [PubMed] [Google Scholar]
- 23.Demirci S, Donmez CM, Gundogar D, et al. Public awareness of, attitudes toward, and understanding of epilepsy in Isparta, Turkey. Epilepsy & Behavior 2007;11:427–433. [DOI] [PubMed] [Google Scholar]
- 24.Diamantopoulos N, Kaleyias J, Tzoufi M, et al. A survey of public awareness, understanding, and attitudes toward epilepsy in Greece. Epilepsia 2006;47:2154–2164. [DOI] [PubMed] [Google Scholar]
- 25.Gzirishvili N, Kasradze S, Lomidze G, et al. Knowledge, attitudes, and stigma towards epilepsy in different walks of life: a study in Georgia. Epilepsy Behav 2013;27:315–318. [DOI] [PubMed] [Google Scholar]
- 26.Roberts RM, Farhana HS. Effectiveness of a first aid information video in reducing epilepsy-related stigma. Epilepsy Behav 2010;18:474–480. [DOI] [PubMed] [Google Scholar]
- 27.Spatt J, Bauer G, Baumgartner C, et al. Predictors for negative attitudes toward subjects with epilepsy: a representative survey in the general public in Austria. Epilepsia 2005;46:736–742. [DOI] [PubMed] [Google Scholar]
- 28.Tedrus GM, Fonseca LC, Vieira AL. Knowledge and attitudes toward epilepsy amongst students in the health area: intervention aimed at enlightenment. Arq Neuropsiquiatr 2007;65:1181–1185. [DOI] [PubMed] [Google Scholar]
- 29.Bishop M, Slevin B. Teachers’ attitudes toward students with epilepsy: results of a survey of elementary and middle school teachers. Epilepsy & Behavior 2004;5:308–315. [DOI] [PubMed] [Google Scholar]
- 30.Bishop M, Boag EM. Teachers’ knowledge about epilepsy and attitudes toward students with epilepsy: Results of a national survey. Epilepsy & Behavior 2006;8:397–405. [DOI] [PubMed] [Google Scholar]
- 31.Antonak RF. Psychometric Analysis and Validation of the Scale of Attitudes toward Persons with Epilepsy. Journal of Epilepsy 1990;3:11–16. [Google Scholar]
- 32.Antonak RF, Livneh H. Development, Psychometric Analysis, and Validation of an Error-Choice Test to Measure Attitudes toward Persons with Epilepsy. Rehabil Psychol 1995;40:25–38. [Google Scholar]
- 33.Fernandes PT, Salgado PCB, Noronha ALA, et al. Stigma Scale of Epilepsy: Validation process. Arq Neuropsiquiatr 2007;65:35–42. [DOI] [PubMed] [Google Scholar]
- 34.Reno BA, Fernandes PT, Bell GS, et al. Stigma and attitudes on epilepsy - A study with secondary school students. Arq Neuropsiquiatr 2007;65:49–54. [DOI] [PubMed] [Google Scholar]
- 35.Youssef FF, Dial S, Jaggernauth N, et al. Knowledge of, attitudes toward, and perceptions of epilepsy among college students in Trinidad and Tobago. Epilepsy Behav 2009;15:160–165. [DOI] [PubMed] [Google Scholar]
- 36.Otte WM, Meeuwesse E, Kafiluddin E, et al. Knowledge and beliefs about epilepsy among people with and without epilepsy in urban Suriname. Epilepsy Behav 2013;29:128–132. [DOI] [PubMed] [Google Scholar]
- 37.Fernandes PT, Salgado PCB, Noronha ALA, et al. Epilepsy stigma perception in an urban area of a limited-resource country. Epilepsy & Behavior 2007;11:25–32. [DOI] [PubMed] [Google Scholar]
- 38.Fernandes PT, Noronha AL, Sander JW, et al. Stigma scale of epilepsy: the perception of epilepsy stigma in different cities in Brazil. Arq Neuropsiquiatr 2008;66:471–476. [DOI] [PubMed] [Google Scholar]
- 39.Fernandes PT, de Barros NF, Li LM. Stop saying epileptic. Epilepsia 2009;50:1280–1283. [DOI] [PubMed] [Google Scholar]
- 40.Bruno E, Bartoloni A, Sofia V, et al. Epilepsy-associated stigma in Bolivia: A community‐based study among the Guarani population: An International League Against Epilepsy/International Bureau for Epilepsy/World Health Organization Global Campaign Against Epilepsy Regional Project. Epilepsy & Behavior 2012;25:131–136. [DOI] [PubMed] [Google Scholar]
- 41.Martiniuk AL, Secco M, Speechley KN, et al. Development and evaluation of an Epilepsy Education Program for Grade 5 Students: a cluster randomized trial. J Neurol Sci 2005;238:S133–S133. [DOI] [PubMed] [Google Scholar]
- 42.Martiniuk ALC, Speechley KN, Secco M, et al. Evaluation of an epilepsy education program for Grade 5 students: A cluster randomized trial. Epilepsy & Behavior 2007;10:604–610. [DOI] [PubMed] [Google Scholar]
- 43.Martiniuk A, Secco M. Evaluating effect of a TV commercial about epilepsy. Epilepsia 2007;48:41–41.17910580 [Google Scholar]
- 44.Zanni KP, Matsukura TS, Maia Filho Hde S. Beliefs and Attitudes about Childhood Epilepsy among School Teachers in Two Cities of Southeast Brazil. Epilepsy Res Treat 2012;2012:819859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Espínola-Nadurille M, Crail-Melendez D, Sánchez-Guzmán MA. Stigma experience of people with epilepsy in Mexico and views of health care providers. Epilepsy & Behavior 2014;32:162–169. [DOI] [PubMed] [Google Scholar]
- 46.Degirmenci Y, Karaman HIO, Bakar C. Perceptions of epilepsy of three different groups in Turkey. Epilepsy & Behavior 2010;19:315–+. [DOI] [PubMed] [Google Scholar]
- 47.Dorota T, Witkowska M, Michalak M. Attitudes of employees of service and trading companies towards people with epilepsy and their professional activity in Poland. Seizure-European Journal of Epilepsy 2014;23:178–183. [DOI] [PubMed] [Google Scholar]
- 48.Labuz-Roszak B, Pierzchala K, Kapinos M, et al. Knowledge and attitudes towards epilepsy among inhabitants of Silesia. A questionnaire study. Neurol Neurochir Pol 2011;45:107–114. [DOI] [PubMed] [Google Scholar]
- 49.Jajić S, Vila A, Ivanović S, et al. KNOWLEDGE AND OPINIONS OF SCHOOL CHILDREN ABOUT EPILEPSY. Acta medica Medianae 2013;52. [Google Scholar]
- 50.Mecarelli O, Voti PL, Vanacore N, et al. A questionnaire study on knowledge of and attitudes toward epilepsy in schoolchildren and university students in Rome, Italy. Seizure 2007;16:313–319. [DOI] [PubMed] [Google Scholar]
- 51.Bozkaya İO, Arhan E, Serdaroglu A, et al. Knowledge of, perception of, and attitudes toward epilepsy of school children in Ankara and the effect of an educational program. Epilepsy & Behavior 2010;17:56–63. [DOI] [PubMed] [Google Scholar]
- 52.An S, Kang H. Stigma-reducing components in direct-to-consumer prescription ads: onset controllability, offset controllability, and recategorization. Health Commun 2011;26:468–478. [DOI] [PubMed] [Google Scholar]
- 53.Brigo F, Otte WM, Igwe SC, et al. Clearly written, easily comprehended? The readability of websites providing information on epilepsy. Epilepsy Behav 2015;44C:35–39. [DOI] [PubMed] [Google Scholar]
- 54.Kerson TS. Epilepsy postings on YouTube: exercising individuals’ and organizations’ right to appear. Soc Work Health Care 2012;51:927–943. [DOI] [PubMed] [Google Scholar]
- 55.Preston SM, Shihab N, Volk HA. Public perception of epilepsy in dogs is more favorable than in humans. Epilepsy & Behavior 2013;27:243–246. [DOI] [PubMed] [Google Scholar]
- 56.Wong VSS, Stevenson M, Selwa L. The presentation of seizures and epilepsy in YouTube videos. Epilepsy & Behavior 2013;27:247–250. [DOI] [PubMed] [Google Scholar]
- 57.Lo AS, Esser MJ, Gordon KE. YouTube: A gauge of public perception and awareness surrounding epilepsy. Epilepsy & Behavior 2010;17:541–545. [DOI] [PubMed] [Google Scholar]
- 58.Caspermeyer JJ, Sylvester EJ, Drazkowski JF, et al. Evaluation of stigmatizing language and medical errors in neurology coverage by US newspapers. Mayo Clin Proc 2006;81:300–306. [DOI] [PubMed] [Google Scholar]
- 59.McNeil K, Brna PM, Gordon KE. Epilepsy in the Twitter era: a need to re-tweet the way we think about seizures. Epilepsy Behav 2012;23:127–130. [DOI] [PubMed] [Google Scholar]
- 60.Rafael F, Dubreuil CM, Burbaud F, et al. Knowledge of epilepsy in the general population based on two French cities: implications for stigma. Epilepsy Behav 2010;17:82–86. [DOI] [PubMed] [Google Scholar]
- 61.Mecarelli O, Capovilla G, Romeo A, et al. Past and present public knowledge and attitudes toward epilepsy in Italy. Epilepsy & Behavior 2010;18:110–115. [DOI] [PubMed] [Google Scholar]
- 62.Smith GM, Ferguson P, Wagner J, et al. Stigma and self-efficacy in persons with epilepsy. Epilepsia 2007;48:238–238.17295616 [Google Scholar]
- 63.Bellon M, Panelli RJ, Rillotta F. Epilepsy-related deaths: An Australian survey of the experiences and needs of people bereaved by epilepsy. Seizure 2015;29:162–168. [DOI] [PubMed] [Google Scholar]
- 64.Buechter R, Pieper D, Ueffing E, et al. Interventions to reduce experiences of stigma and discrimination of people with mental illness and their caregivers. The Cochrane Library; 2013. [Google Scholar]
- 65.Price P, Kobau R, Buelow J, et al. Improving understanding, promoting social inclusion, and fostering empowerment related to epilepsy: Epilepsy Foundation public awareness campaigns-2001 through 2013. Epilepsy & Behavior 2015;44:239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Epilepsy Foundation. Available at: http://www.epilepsy.com/.
- 67.Buelow J, Gattone P, Giles W, et al. Epilepsy foundation public awareness campaigns−−2001 through 2013. Epilepsy Behav 2015;44:238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention. Available at: http://www.cdc.gov/epilepsy/professionals.htm.
- 69.Corrigan PW. Best practices: Strategic stigma change (SSC): five principles for social marketing campaigns to reduce stigma. Psychiatr Serv 2011;62:824–826. [DOI] [PubMed] [Google Scholar]
- 70.Schiavo R Health Communication: From Theory to Practice. Jossey-Bass: San Francisco, CA; 2014. [Google Scholar]
- 71.Kobau R, DiIorio CA, Anderson LA, et al. Further validation and reliability testing of the Attitudes and Beliefs about Living with Epilepsy (ABLE) components of the CDC Epilepsy Program Instrument on Stigma. Epilepsy Behav 2006;8:552–559. [DOI] [PubMed] [Google Scholar]
- 72.DiIorio CA, Kobau R, Holden EW, et al. Developing a measure to assess attitudes toward epilepsy in the US population. Epilepsy & Behavior 2004;5:965–975. [DOI] [PubMed] [Google Scholar]
- 73.Lewandowsky S, Ecker UKH, Seifert CM, et al. Misinformation and Its Correction: Continued Influence and Successful Debiasing. Psychological Science in the Public Interest 2012;13:106–131. [DOI] [PubMed] [Google Scholar]
- 74.Loewenstein G, Lerner JS. THe role of affect in decision making. Oxford University Press; 2003. [Google Scholar]
- 75.Lerner JS, Li Y, Valdesolo P, et al. Emotion and decision making. Annu Rev Psychol 2015;66:799–823. [DOI] [PubMed] [Google Scholar]
- 76.Aronson ID, Bania TC. Race and emotion in computer-based HIV prevention videos for emergency department patients. AIDS Educ Prev 2011;23:91–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.D’Alessandro AM, Peltier JW, Dahl AJ. The impact of social, cognitive and attitudinal dimensions on college students’ support for organ donation. Am J Transplant 2012;12:152–161. [DOI] [PubMed] [Google Scholar]
- 78.Bekiroglu N, Ozkan R, Gurses C, et al. A study on awareness and attitude of teachers on epilepsy in Istanbul. Seizure-European Journal of Epilepsy 2004;13:517–522. [DOI] [PubMed] [Google Scholar]
- 79.Aydin K, Yildiz H. Teachers’ perceptions in central Turkey concerning epilepsy and asthma and the short-term effect of a brief education on the perception of epilepsy. Epilepsy & Behavior 2007;10:286–290. [DOI] [PubMed] [Google Scholar]
- 80.Fernandes PT, Noronha ALA, Sander JW, et al. Training the trainers and disseminating information - A strategy to educate health professionals on epilepsy. Arq Neuropsiquiatr 2007;65:14–22. [DOI] [PubMed] [Google Scholar]
- 81.Fernandes PT, Noronha ALA, Araújo U, et al. Teachers perception about epilepsy. Arq Neuropsiquiatr 2007;65:28–34. [DOI] [PubMed] [Google Scholar]
- 82.Smith K, Siddarth P, Zima B, et al. Unmet mental health needs in pediatric epilepsy: Insights from providers. Epilepsy & Behavior 2007;11:401–408. [DOI] [PubMed] [Google Scholar]
- 83.Brabcova D, Lovasova V, Kohout J, et al. Improving the knowledge of epilepsy and reducing epilepsy-related stigma among children using educational video and educational drama-A comparison of the effectiveness of both interventions. Seizure 2013;22:179–184. [DOI] [PubMed] [Google Scholar]
- 84.Mecarelli O, Messina P, Capovilla G, et al. An educational campaign about epilepsy among Italian primary school teachers. 2. The results of a focused training program. Epilepsy Behav 2015;42:93–97. [DOI] [PubMed] [Google Scholar]


