Abstract
Purpose
The purpose of this study is to assess the feasibility and usefulness of time-resolved magnetic resonance angiography (TR-MRA) for follow-up of visceral artery aneurysms (VAAs) after embolotherapy.
Material and methods
Twenty-one VAAs (11 splenic, six renal, three internal iliac, and one superior pancreaticoduodenal artery aneurysms) in 18 patients (median age, 64 years; range, 36-88 years) previously treated by embolisation with platinum coils, were evaluated. The mean size of the aneurysm was 10.5 cm3 (range, 0.3-132 cm3). Among them, 19 lesions were treated by aneurysmal packing with or without distal-to-proximal embolisation. For the remaining two lesions, distal-to-proximal embolization alone was performed. The mean observation period after embolotherapy was 35 weeks (range, 4-216). All patients underwent TR-MRA following an intravenous bolus injection of gadolinium chelate. Recanalisation was diagnosed when any portion of the aneurysmal sac was enhanced in the arterial phase.
Results
On TR-MRA, two lesions were diagnosed as recanalised. They were confirmed by transcatheter arteriography and re-treated by embolotherapy. For the remaining 19 lesions, there were no findings of recanalisation on TR-MRA.
Conclusions
TR-MRA appears to be a feasible method for follow-up examination of VAAs treated by embolotherapy.
Keywords: time-resolved MRA, embolization, aneurysm
Introduction
Owing to the increased use of cross-sectional imaging and an aging population, visceral artery aneurysms (VAAs) are now more frequently diagnosed than before. The reported incidence is approximately 0.01% to 2% in autopsy and angiographic studies [1]. They are clinically important because of the high incidence of rupture and life-threatening haemorrhage associated with mortality rates of 20-75%, depending on the location of the aneurysm [2]. Considering the natural history of VAAs and the risk of rupture, the general consensus in the literature is to treat such lesions even when patients are asymptomatic [3]. Although endovascular procedures are used increasingly often for the treatment of aneurysms, recanalisation due to coil compaction and/or aneurysm regrowth (9-26%) remains a limitation of this method and requires long-term imaging follow-up [4-6].
Digital subtraction angiography (DSA) is an invasive procedure that involves risks of complications such as formation of a pseudoaneurysm at the puncture site and arterial dissection and/or occlusion due to endothelial injury caused by mal-manipulation of catheters or guidewires. Computed tomography angiography (CTA) is very effective in detecting aneurysms; however, metal artefacts limit its use after coil embolisation. Recently, time-resolved magnetic resonance angiography (TR-MRA) has been reported as a valuable option for noninvasive follow-up because it offers a noninvasive, high-temporal-resolution alternative to DSA for screening after coil embolisation [7]. In this study, we followed-up VAAs treated with coil embolisation by using TR-MRA, and assessed its patency and intra-aneurysmal blood flow.
Material and methods
Patients
The protocol for this study was approved by our institutional review board. Twenty-one VAAs (11 splenic, six renal, three internal iliac, and one superior pancreaticoduodenal artery aneurysms) in 18 patients (median age 64 years, range 36-88 years), treated by embolotherapy with 0.014 to 0.018-inch platinum coils with or without nylon or polyester fibres from January 2008 to March 2016, were evaluated. All the patients had undergone contrast-enhanced CTA before treatment, and the lesions were measured on 1-mm-thickness images at the arterial phase. The volumes of the aneurysms were measured and calculated as described in the following section. Among the 21 lesions, 19 were treated by aneurysmal packing with or without distal-to-proximal embolisation, and the remaining two lesions were treated by distal-to-proximal embolisation alone. For lesions treated with aneurysmal packing alone (n = 15), packing density was calculated as described in the following section. All patients underwent TR-MRA as described in the separate section.
Calculation of visceral artery aneurysm volume and coil-packing density
Theoretical coil-packing density (CPD) was calculated using the formula: CPD = 100 × (total coil volume/targeted VAA volume). Total coil volumes were calculated assuming a cylindrical coil shape, using the formula: coil volume = = π x (coil radius)2 × (coil length) for each coil. The VAA volume was measured on pre-treatment CTA and calculated using the formula: VAA volume = (4/3) × π x (length/2) × (width/2) × (height/2).
Time-resolved magnetic resonance angiography
All TR-MRA were performed on a 1.5-T MR system (Achieva: Philips Healthcare, Best, the Netherlands) or a 3.0-T system (Skyra: Siemens, Erlangen, Germany; or Ingenia: Philips Healthcare). TR-MRA was acquired with a 3D-T1-weighted gradient recalled echo sequence with the following parameters: for Achieva, TR/TE = 4.7/1.4 ms, flip angle (FA) = 40, field of view (FOV) = 400 mm with 80% rectangular FOV, matrix = 336 × 227, slice thickness (ST) = 4 mm interpolated to 2.0 mm, slice number (SN) = 25, and slab thickness = 50 mm; for Skyra, TR/TE = 2.1/0.9 ms, FA = 10, FOV = 430 mm, matrix = 320 × 320, ST = 2 mm, SN = 40, and slab thickness = 80.0 mm; and for Ingenia, TR/TE = 2.7/0.9 ms, FA = 8, FOV = 450 mm with 70% rectangular FOV, matrix = 352 × 264, ST = 3 mm interpolated to 1.5 mm, SN = 40, and slab thickness = 60 mm. To reduce the number of in-plane phase-encoding steps, parallel imaging and keyhole imaging techniques were applied with a parallel imaging factor of 2.5 and keyhole factor of 20% for Achieva, and 3 and 10% with a sampling density of 20% for Skyra, respectively, and factors of 4 and 25% for Ingenia, achieving temporal resolutions of 1.7, 1.05, and 1.7 s, respectively. Each acquisition slab was set to include the afferent/efferent artery and aneurysmal sac with portions of the aorta. Twenty-five consecutive 3D volume images were acquired immediately after an injection of contrast media (0.1 mmol/kg of Gd-chelate, Magnevist: Bayer HealthCare, Whippany, NJ, USA) at a flow rate of 3 ml/s, followed by a saline flush of 30 ml during breath-holding. All source images from each frame were reconstructed with a maximum intensity projection (MIP) algorithm.
Computed tomography scanning
Dynamic contrast CT angiography was performed at 120 kVp with a 64-detector row scanner (Somatom Definition: Siemens, Forchheim, Germany) with a collimation of 64 × 0.6 mm and a pitch of 1. All scans were reconstructed in transverse, coronal, and sagittal orientations at a slice thickness of 1 mm and increments of 1 mm, using the corresponding soft-tissue kernel B30f.
Diagnostic procedure on time-resolved magnetic resonance angiography and computed tomography angiography
On TR-MRA, all the MIP and source images were assessed by two experienced radiologists with experience of 13 and 11 years, respectively, and they made diagnoses by consensus. Recanalisation was diagnosed when any portion of the aneurysmal sac was enhanced in the arterial phase. For 11 lesions in nine patients for which CTA was performed within two weeks before or after TR-MRA, contrast enhancement in the aneurysm was also assessed in the arterial phase by two radiologists different from the former ones (with 13- and 8-year experience, respectively). It was classified into the following three groups by consensus: 1) enhanced, 2) unenhanced, and 3) unevaluable.
Results
The mean size of the aneurysm was 10.5 cm3 (range, 0.3-132). For lesions treated with aneurysmal packing alone (n = 15), the mean coil-packing density was 22.4% (range, 9.5-40.0). The mean observation period after embolotherapy was 35 weeks (range, 4-216). For three cases with a total of four lesions, follow-up DSA was performed. On TR-MRA, two lesions out of 21 lesions (9.5%) were diagnosed as recanalised. Thereafter, they were confirmed by transcatheter arteriography and re-treated by re-embolisation by placing additional coils (Figure 1). For 19 lesions (90.5%), there were no findings of recanalisation on TR-MRA, and observation was continued for them (Figure 2). Among the recanalised lesions, one lesion had been treated by aneurysmal packing alone, and the other had been treated by proximal-to-distal embolisation alone. For the former one, the coil-packing density was 9.5%, lower than the mean of those of other lesions treated with coil packing alone (24%, n = 14; statistical analysis was not applicable). Among 11 lesions where CTA was also performed after treatment within two weeks before or after TR-MRA, the contrast enhancement in nine lesions (82%) was unevaluable by the two radiologists because of prominent metallic artefact, including the one recanalised lesion. Of the two lesions where the enhancement was detected on CTA, one lesion had been treated by distal-to-proximal embolisation alone, and the other had been treated by aneurysmal packing in addition to distal-to-proximal embolisation. In the latter case, recanalisation was not detected on TR-MRA or DSA (Figure 3). Table 1 shows the summary of the 21 lesions.
Figure 1.
A 40-year-old woman with a splenic aneurysm. A) Computed tomography angiography (CTA) demonstrated a 24 × 18-mm aneurysm in the main trunk of the splenic artery (arrowhead). B-C) Digital subtraction angiography (DSA) just before and after coil embolisation showed complete occlusion of the aneurysm. D) Time-resolved magnetic resonance angiography showed inhomogeneous enhancement within the aneurysm in the arterial phase (arrow; axial MIP image). E) On CTA evaluation of enhancement in the aneurysm was difficult due to prominent metal artefacts. F) Recanalisation was confirmed by DSA (arrow)
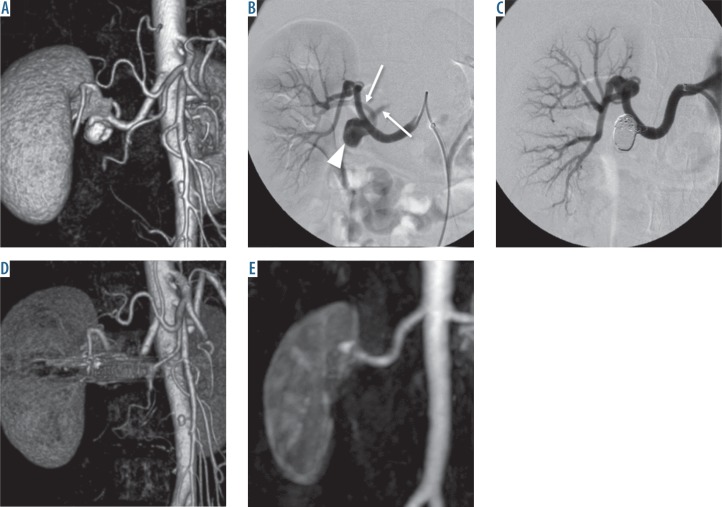
Figure 2.
A 56-year-old woman with a right renalaneurysm. A) Computed tomography angiography (CTA) demonstrated an 11-mm aneurysm at the hilum of the right renal artery. B) Digitalsubtraction angiography showed a narrow-neckaneurysm (arrowhead) at the main trunk ofthe right renal artery and two efferent branches (arrows). C) It was treated by aneurysmal coilpacking. D) On CTA 39 months after the treatmentenhancement of the aneurysm was difficult toevaluate due to prominent metal artefacts. E) Ontime-resolved magnetic resonance angiographythe aneurysm was not enhanced and thus wasdiagnosed as occluded
Figure 3.
An 80-year-old woman with a right internal artery aneurysm. A) Computed tomography angiography (CTA) demonstrated a 35 × 35-mm aneurysm with a thick mural thrombus in the main trunk of the internal iliac artery just proximal to the superior gluteal artery (arrowhead). B-C) Digital subtraction angiography (DSA) just before and after coil embolisation showed complete occlusion of the aneurysm. D) On time-resolved magnetic resonance angiography there was no apparent enhancement in the aneurysm. A tiny, high-intensity area (asterisk) indicated a venous flow artefact because it was continuously observed before an injection of gadolinium chelate. E) CTA showed a tiny contrast-enhanced area in the caudal part of the aneurysm (arrow). F) On DSA recanalisation was not detected
Table 1.
Summary of the lesion profiles and diagnosis on time-resolved magnetic resonance angiography (TR-MRA) and computed tomography angiography (CTA)
| Patient no. | Sex | Lesionno. | Age (years) | Loca-tion | Volume (cm3 | Observation period (week) | Embolisation technique | Coli packing density (%) | TR-MRAdiagnosis | CTAdiagnosis | Angiography |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 1 | 36 | SpA | 3.8 | 213 | P | 9.5 | Recanalization | Unevaluable | Recanalisation |
| 2 | F | 2 | 56 | RA | 1.1 | 216 | P | 15.8 | Occlusion | ||
| 3 | F | 3 | 80 | IIA | 26.4 | 55 | P + I | N/A | Occlusion | Enhanced | Occlusion |
| 4 | IIA | 25.6 | 55 | I | N/A | Recanalisation | Enhanced | Recanalisation | |||
| 4 | M | 5 | 88 | IIA | 131.8 | 11 | I | N/A | Occlusion | ||
| 5 | F | 6 | 50 | SpA | 1.2 | 7 | P | 21.5 | Occlusion | Unevaluable | Occlusion |
| 7 | SpA | 1.2 | 15 | P + I | N/A | Occlusion | Unevaluable | ||||
| 6 | F | 8 | 78 | SpA | 0.3 | 13 | P + I | N/A | Occlusion | ||
| 7 | F | 9 | 64 | SpA | 0.8 | 8 | P | 18.6 | Occlusion | Unevaluable | |
| 8 | F | 10 | 72 | SpA | 2.2 | 10 | P | 18.9 | Occlusion | ||
| 9 | M | 11 | 60 | SpA | 2.1 | 10 | P + I | N/A | Occlusion | ||
| 10 | M | 12 | 46 | SpA | 1.5 | 12 | P | 40.0 | Occlusion | Unevaluable | |
| 11 | F | 13 | 74 | RA | 2.9 | 12 | P | 13.9 | Occlusion | ||
| 14 | RA | 3.9 | 12 | P | 17.6 | Occlusion | |||||
| 12 | F | 15 | 80 | RA | 3.7 | 26 | P | 22.0 | Occlusion | ||
| 13 | M | 16 | 55 | RA | 1.0 | 6 | P | 21.0 | Occlusion | Unevaluable | |
| 14 | M | 17 | 70 | SpA | 8.5 | 13 | P | 19.6 | Occlusion | ||
| 15 | F | 18 | 50 | SpA | 1.3 | 9 | P | 24.5 | Occlusion | ||
| 16 | F | 19 | 56 | RA | 0.3 | 4 | P | 39.7 | Occlusion | Unevaluable | |
| 17 | M | 20 | 41 | SpA | 1.1 | 13 | P | 21.9 | Occlusion | Unevaluable | |
| 18 | M | 21 | 83 | ASPD | 0.2 | 13 | P | 27.9 | Occlusion | Unevaluable |
SpA – splenic artery, RA – renal artery, IIA – internal iliac artery, ASPD – anterior superior pancreaticoduodenal artery, P – packing, I – isolation (distal-to-proximal embolisation), N/A – not applicable
Discussion
In this study, we evaluated post-treated VAAs with TR-MRA and successfully detected recanalisation in two lesions. The recanalisation rate was 9.5% and was similar to those already reported [4,6]. Generally, there are two major treatment strategies for VAAs by endovascular therapy: aneurysmal packing and isolation of the aneurysm by distal-to-proximal embolisation, using fibred and/or non-fibred metallic coils; sometimes they are performed together [8]. Because the majority of VAAs incidentally detected are true aneurysms, aneurysmal packing is considered favourable for their treatment compared to isolation alone from the aspect of preservation of the parent vessel as well as preventing potential retrograde inflow from branches connecting to the aneurysm after treatment [8]. Yasumoto et al. [6] reported, in a study with 46 lesions of VAAs followed by CTA, that the coil-packing density was one of the most important keys for long-term clinical success, and a major cause of recanalisation was coil compaction, more likely to occur especially when the coil-packing density was relatively low. In our study, we also found coil compaction on the plain X-ray image of a lesion with recanalisation when the packing density was 9.5%. Therefore, it is crucial to place as many coils as possible into the lesion to prevent coil compaction. However, a dilemma presents itself when many coils are placed in a small space; they produce more prominent metallic artefacts and worsen the visibility of contrast enhancement at the treated site on CTA. Furthermore, because coil compaction is an indirect and merely a supportive finding for recanalisation, a reliable tool to detect recanalisation precisely is necessary.
The usefulness of TR-MRA has already been reported for post-treated intracranial aneurysms and pulmonary arteriovenous malformations [9,10]. TR-MRA is one of the dynamic contrast-enhanced MR angiography methods and provides high-quality images while maintaining both adequate spatial and temporal resolutions by using the keyhole technique [11]. Kawai et al. [12,13] reported that the advantages of TR-MRA compared to contrast-enhanced and/or unenhanced CT were: 1) less susceptibility to metallic artefacts from platinum coils, 2) detectability of dynamic blood flow at a high temporal resolution, and 3) no radiation exposure. In the two cases in which recanalisation was confirmed on DSA in our study, intra-aneurysmal blood flow was clearly shown on TR-MRA with a minimal signal void, whereas it was difficult to assess contrast enhancement on CT, especially for one lesion for which aneurysmal packing was performed because of severe metallic artefacts. Overall, for all five lesions confirmed by DSA, detectability of recanalisation was 100% by TR-MRA. However, we experienced one lesion in which the remaining blood flow was suspected only on CTA but not on TR-MRA or DSA (Figure 3). It was hypothesised that because the timings of the CTA and DSA were different or the perfused area was so small, it could not be detected by TR-MRA or DSA. Nonetheless, it was considered that clinical significance might not be so important. On the other hand, for 9 out of 10 lesions treated with aneurysmal packing, contrast enhancement could not be evaluated on CTA because of metallic artefacts, including the lesion with the lowest packing density (9.5%). Regarding these aspects, TR-MRA might be a suitable modality to assess recanalisation of VAAs after coil embolisation, especially for lesions treated by aneurysmal packing, although there are a small number of contraindications: patients with internal devices (e.g. pacemakers), renal failure, and claustrophobia. Because the population of patients with VAAs are relatively old and chronic kidney disease is relatively common, sometimes it might be worrisome to administer gadolinium chelate [14,15]. Although a former study [13] reported that a motion artefact was one of the factors affecting image quality, it was acceptable in all the cases in our study. Perhaps it was because the reported cases had relatively small pulmonary arteriovenous malformations located in the area close to the apex of the left ventricle of the heart, where the motion of the lesion tends to be vigorous even in a good breath-holding state. In contrast, most of the VAAs in our study could be relatively stable in position as long as the patients could hold their breath properly.
Dynamic contrast-enhanced MRI might be an alternative choice for detecting intra-aneurysmal blood flow [16]. Although it is a conventional method that could be performed by general MR equipment without the specialised applications for keyhole imaging, the temporal resolution is not high enough (~15 sec or more, depending on the number of slices) to differentiate between direct and retrograde inflow from collateral pathways into the aneurysm. It might be a drawback for pretreatment assessment before re-embolisation therapy. In addition, even the lesions with complete occlusion sometimes appear hyperintense on pre-contrast MRI due to thrombi in the aneurysms, which makes it difficult to evaluate the contrast enhancement [17]. Four-dimensional computed tomography might be another option. Similar to TR-MRA, this method could assess haemodynamic states around the lesions with a high temporal resolution [18]. However, with the nature of X-ray CT, it might also be difficult to evaluate contrast enhancement of VAAs after treatment by placement of platinum coils.
There are some limitations to this study. First, this is a retrospective study with a small sample size. Second, diagnoses were not confirmed by transcatheter angiography in all cases. Nevertheless, it might have a strong potential for detection of blood flow in coil-embolised VAAs.
In conclusion, although this study was a small series and further investigation is needed, TR-MRA appears to be useful and highly recommended for assessment of recanalisation of VAAs after coil embolisation.
Acknowledgements
This work is partly supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (24791323).
Conflict of interest
The authors report no conflict of interest.
References
- 1.Huang Y-K, Hsieh H-C, Tsai F-C, et al. Visceral artery aneurysm: risk factor analysis and therapeutic opinion. Eur J Vasc Endovasc Surg. 2007;33:293–301. doi: 10.1016/j.ejvs.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 2.Shanley CJ, Shah NL, Messina LM. Common splanchnic artery aneurysms: splenic, hepatic, and celiac. Ann Vasc Surg. 1996;10:315–322. doi: 10.1007/BF02001900. [DOI] [PubMed] [Google Scholar]
- 3.Liu Q, Lu JP, Wang F, et al. Visceral artery aneurysms: evaluation using 3D contrast-enhanced MR angiography. AJR Am J Roentgenol. 2008;191:826–833. doi: 10.2214/AJR.07.3255. [DOI] [PubMed] [Google Scholar]
- 4.Sessa C, Tinelli G, Porcu P, et al. Treatment of visceral artery aneurysms: description of a retrospective series of 42 aneurysms in 34 patients. Ann Vasc Surg. 2004;18:695–703. doi: 10.1007/s10016-004-0112-8. [DOI] [PubMed] [Google Scholar]
- 5.Cochennec F, Riga CV, Allaire E, et al. Contemporary management of splanchnic and renal artery aneurysms: results of endovascular compared with open surgery from two European vascular centers. Eur J Vasc Endovasc Surg. 2011;42:340–346. doi: 10.1016/j.ejvs.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 6.Yasumoto T, Osuga K, Yamamoto H, et al. Long-term outcomes of coil packing for visceral aneurysms: correlation between packing density and incidence of coil compaction or recanalization. J Vasc Interv Radiol. 2013;24:1798–1807. doi: 10.1016/j.jvir.2013.04.030. [DOI] [PubMed] [Google Scholar]
- 7.Kurosaka K, Kawai T, Shimohira M, et al. Time-resolved Magnetic Resonance Angiography for assessment of recanalization after coil embolization of visceral artery aneurysms. Pol J Radiol. 2013;78:64–68. doi: 10.12659/PJR.883769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chadha M, Ahuja C. Visceral artery aneurysms: diagnosis and percutaneous management. Semin Intervent Radiol. 2009;26:196–206. doi: 10.1055/s-0029-1225670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi JW, Roh HG, Moon WJ, et al. Time-resolved 3D contrast-enhanced MRA on 3.0T: a non-invasive follow-up technique after stent-assisted coil embolization of the intracranial aneurysm. Korean J Radiol. 2011;12:662–670. doi: 10.3348/kjr.2011.12.6.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimohira M, Kawai T, Hashizume T, et al. Reperfusion Rates of Pulmonary Arteriovenous Malformations after Coil Embolization: Evaluation with Time-Resolved MR Angiography or Pulmonary Angiography. J Vasc Interv Radiol. 2015;26:856–864. doi: 10.1016/j.jvir.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 11.Jaspers K, Nijenhuis RJ, Backes WH. Differentiation of spinal cord arteries and veins by time-resolved MR angiography. J Magn Reson Imaging. 2007;26:31–40. doi: 10.1002/jmri.20940. [DOI] [PubMed] [Google Scholar]
- 12.Kawai T, Shimohira M, Kan H, et al. Feasibility of time-resolved MR angiography for detecting recanalization of pulmonary arteriovenous malformations treated with embolization with platinum coils. J Vasc Interv Radiol. 2014;25:1339–1347. doi: 10.1016/j.jvir.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 13.Kawai T, Shimohira M, Ohta K, et al. The Role of Time-Resolved MRA for Post-treatment Assessment of Pulmonary Arteriovenous Malformations: A Pictorial Essay. Cardiovasc Intervent Radiol. 2016;39:965–972. doi: 10.1007/s00270-016-1325-2. [DOI] [PubMed] [Google Scholar]
- 14.White SL, Polkinghorne KR, Atkins RC, et al. Comparison of the prevalence and mortality risk of CKD in Australia using the CKD Epidemiology Collaboration (CKD-EPI) and Modification of Diet in Renal Disease (MDRD) Study GFR estimating equations: the AusDiab (Australian Diabetes, Obesity and Lifestyle) Study. Am J Kidney Dis. 2010;55:660–670. doi: 10.1053/j.ajkd.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 15.Sadowski EA, Bennett LK, Chan MR, et al. Nephrogenic systemic fibrosis: risk factors and incidence estimation. Radiology. 2007;243:148–157. doi: 10.1148/radiol.2431062144. [DOI] [PubMed] [Google Scholar]
- 16.Koganemaru M, Abe T, Nonoshita M, et al. Follow-up of true visceral artery aneurysm after coil embolization by three-dimensional contrast-enhanced MR angiography. Diagn Interv Radiol. 2014;20:129–135. doi: 10.5152/dir.2013.13236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martin AJ, Hetts SW, Dillon WP, et al. MR imaging of partially thrombosed cerebral aneurysms: characteristics and evolution. AJNR Am J Neuroradiol. 2011;32:346–351. doi: 10.3174/ajnr.A2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian B, Xu B, Lu J, et al. Four-dimensional computed tomography angiographic evaluation of cranial dural arteriovenous fistula before and after embolization. Eur J Radiol. 2015;84:1144–1149. doi: 10.1016/j.ejrad.2015.03.009. [DOI] [PubMed] [Google Scholar]