Abstract
Background
This study examines whether young never smokers in Scotland, UK, who have tried an e-cigarette are more likely than those who have not, to try a cigarette during the following year.
Methods
Prospective cohort survey conducted in four high schools in Scotland, UK during February/March 2015 (n=3807) with follow-up 1 year later. All pupils (age 11–18) were surveyed. Response rates were high in both years (87% in 2015) and 2680/3807 (70.4%) of the original cohort completed the follow-up survey. Analysis was restricted to baseline ‘never smokers’ (n=3001/3807), 2125 of whom were available to follow-up (70.8%).
Results
At baseline, 183 of 2125 (8.6%) never smokers had tried an e-cigarette and 1942 had not. Of the young people who had not tried an e-cigarette at baseline, 249 (12.8%) went on to try smoking a cigarette by follow-up. This compares with 74 (40.4%) of those who had tried an e-cigarette at baseline. This effect remained significant in a logistic regression model adjusted for smoking susceptibility, having friends who smoke, family members’ smoking status, age, sex, family affluence score, ethnic group and school (adjusted OR 2.42 (95% CI 1.63 to 3.60)). There was a significant interaction between e-cigarette use and smoking susceptibility and between e-cigarette use and smoking within the friendship group.
Conclusions
Young never smokers are more likely to experiment with cigarettes if they have tried an e-cigarette. Causality cannot be inferred, but continued close monitoring of e-cigarette use in young people is warranted.
Keywords: Electronic Nicotine Delivery Devices, Denormalization, Priority/special Populations
Introduction
In the UK and many other countries, e-cigarette use among young people is largely confined to those who have already tried tobacco and is mostly experimental in nature.1 2 That is, most young people who have never tried tobacco smoking, hereon referred to as never-smokers, do not engage in regular e-cigarette use that is sustained over time. Nevertheless, there remains concern that trying an e-cigarette could ease the pathway to experimentation with tobacco smoking for young never-smokers.
Eight longitudinal studies, all conducted in the USA with follow-up after 63 4 and/or 12 months,5–10 have explored the relationship between e-cigarette use and smoking initiation in young never-smokers. They found that young people who had ever used an e-cigarette at baseline were more likely to have tried a cigarette by follow-up.
Most of the evidence from prospective cohort studies of young never smokers, e-cigarette use and smoking initiation has come from the USA. It is important this evidence can be compared with studies from different countries because varied national contexts, such as different tobacco control regulations, historical and cultural factors around tobacco use, availability and supply of products, ethnic composition of the population and investment in advertising of products, make it difficult to generalise findings across national boundaries. For example, in Poland 27.4% of adolescents report using an e-cigarette in the past month.11 Poland is a major European tobacco and e-cigarette producer. Recently smoking rates have increased among Polish female adolescents although they are stable in men12–14 and by late adolescence most Polish e-cigarette users are dual users (tobacco and e-cigarette use). A recent study found 21.8% of students (16–18 years) were dual users and this was not associated with reduced cigarette consumption compared with tobacco-only users.15 The case of Poland highlights the potential role of national factors such as tobacco production and industry involvement in affecting levels of use in young people.
In Scotland, the prevalence of cigarette smoking among young people has steadily fallen over the last two decades. In 2015, only 2% of 13 year olds and 7% of 15 year olds were regular smokers.16 However, current smoking among young people aged 16–24 years in Scotland is significantly higher at 21%.17 This disparity suggests that smoking initiation may now be delayed until early adulthood. Therefore early risk factors for later smoking initiation require further investigation.
Previous cross-sectional research has shown a positive association between e-cigarette use and weakened intentions not to smoke in children aged 10–11 years in Wales.1 Recently the ever use of e-cigarettes among young non-smokers has increased in Scotland with 10% of non-smoking 15 year olds having tried them in 2013 and 24% in 2015.16 Levels of regular e-cigarette use among young people in Wales have also increased with 2.7% of young people aged 11–18 years reporting using them at least once a week in 2015.18 These increases were preceded by a marked growth in the retail availability of e-cigarettes with the proportion of retailers with displays of e-cigarettes doubling between 2013 and 2014.19 When this study was conducted, within store advertising and promotion of e-cigarettes was not regulated and there was no age restriction on the legal purchase of e-cigarettes in the UK. This study is one of the first to examine e-cigarette use and cigarette experimentation in a UK longitudinal sample.
Methods
The data presented here are drawn from the Determining the Impact of Smoking Point-of-Sale Legislation Among Youth (DISPLAY) study.20 The DISPLAY study is a 5-year multimodal study designed to measure the impact of UK legislation to ban point-of-sale displays of tobacco products on the smoking attitudes and behaviours of young people. One element of the DISPLAY study is an annual school survey conducted in four Scottish secondary schools located in communities that differ in terms of their socioeconomic and urban–rural profiles. The data presented here are from the 2015 and 2016 surveys which included all pupils (aged 11–18) in the four schools. All four schools had pupils across the age range 11–18 years and a breakdown of participant numbers by school and by year group is given in table 1. The survey was administered by class teachers under exam conditions and took on average 40 min to complete. Pupils who were absent on the day of the survey were given opportunity during the following 2 weeks to complete the survey.
Table 1.
Number of ‘never smoking’ respondents by school and year group
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | Year 6 | Total | |
| School 1 Accessible small town/medium–low deprivation |
207 24.1% |
184 21.5% |
193 22.5% |
129 15.0% |
93 10.8% |
52 6.1% |
858 100% |
| School 2Urban/medium–low deprivation | 147 19.9% |
175 23.7% |
136 18.4% |
134 18.2% |
85 11.5% |
61 8.3% |
738 100% |
| School 3 Other urban/high deprivation |
177 26.3% |
160 23.8% |
106 15.8% |
125 18.6% |
62 9.2% |
42 6.3% |
672 100% |
| School 4 Urban/high deprivation |
151 20.6% |
197 26.9% |
122 16.6% |
126 17.2% |
94 12.8% |
43 5.9% |
733 100% |
| Total | 682 | 716 | 557 | 513 | 333 | 197 | 3001 |
| Mean age (SD) | 12.5 (0.34) | 13.5 (0.34) |
14.6 (0.34) |
15.6 (0.35) |
16.6 (0.36) |
17.6 (0.32) |
14.4 (1.58) |
Ethical approval was obtained from the University of St Andrews, University Teaching and Research Ethics Committee (UTREC). Parental opt-out consent was obtained prior to pupils completing the survey. Pupils also provided active consent by completing the survey.
Derivation of variables
Smoking status
Respondents were asked “Have you ever smoked cigarettes or hand-rolled cigarettes (roll-ups), even if it is just one or two puffs?” to which they could respond ‘yes’ or ‘no’. Young people who responded ‘no’ were deemed to be never-smokers at that point.
E-cigarette use
Respondents were asked whether or not they had heard of e-cigarettes. Pupils who answered that they had not heard of e-cigarettes were routed past further questions on e-cigarettes. Pupils that had heard of e-cigarettes were then asked “Which ONE of the following is closest to describing your experience of e-cigarettes/vapourisers/shisha pens?” with response options of ‘I have never used them’, ‘I have tried them once or twice’, ‘I use them sometimes (more than once a month)’ or ‘I use them often (more than once a week)’. Young people who responded that they had never heard of e-cigarettes were coded as having ‘never used them’.
For the logistic regression analysis, due to low frequencies in the categories reflecting regular use, participants were divided into those who had never tried e-cigarettes versus those who had tried e-cigarettes.
Susceptibility to smoking
Susceptibility to smoking was assessed through two questions “If one of your friends offered you a cigarette or hand-rolled cigarettes (roll-ups), would you smoke it?” and “Do you think you will smoke a cigarette or hand-rolled cigarettes (roll-ups) at any time during the next year?”. The response option for these questions was ‘definitely yes’, ‘probably yes’, ‘probably not’ and ‘definitely not’. If respondents answered anything other than ‘definitely not’ to either of these questions then they were coded as being susceptible to smoking. These measures of smoking susceptibility have been used in related studies6 and are based on validated measures.21
Number of friends and family who smoke
Respondents were asked “How many of your friends smoke cigarettes or hand-rolled cigarettes (roll-ups)?” and could respond ‘most of them’, ‘about half of them’, ‘some of them’, ‘none of them’ or ‘don’t know’. ‘Don’t know’ responses were coded as missing and then a binary variable was generated distinguishing those who responded ‘none of them’ versus any other response.
Respondents were asked “which if any of the following people smoke cigarettes or hand rolled cigarettes (roll-ups)?”. Options included their mother or female carer, father or male carer, brother (eldest if more than one) and sister (eldest if more than one). A binary variable was created splitting participants who had responded that any of these family members smoked versus those that reported no smokers in their immediate family.
Demographic variables
Respondents were asked their gender, ethnic group and date of birth. Individual family material well-being was assessed through the Family Affluence Scale (FAS).22 The FAS consists of four questions (own bedroom, number of family cars, number of computers and number of family holidays abroad per year). The FAS raw scores were transformed though categorical principal component analysis into single-dimensional scores that were then divided into tertiles of high, medium and low FAS.
Analysis
Analysis was conducted in Stata V.14 (StataCorp).
Never smokers were divided into those who had tried an e-cigarette at baseline and those who had not and these groups were compared in terms of the proportion of participants that reported having experimented with cigarettes by follow-up. Tobacco experimentation in this study was defined as any cigarette use, even just one or two puffs.
Multivariate logistic regression was used to control for potential confounding factors—sex, age, ethnicity, family affluence, smoking within the family, smoking by friends and susceptibility to smoking. The model was built in three blocks, first with only e-cigarette use and smoking-related variables as independent variables and in the second block demographic variables were added and an indicator for school was included in the model. Including school as a covariate makes explicit the effect of school as school-level smoking norms are an important influence on smoking behaviour.23 In the third block interactions between e-cigarette use, smoking susceptibility and smoking within friendship group were included. The risk ratio (RR) for the unadjusted model was obtained from a binomial log-linear regression and for the adjusted models a Poisson regression model with a robust variance estimator.24
To test the effect of missing data on the parameter estimates, we used multiple imputation by chained equations (Stata V.14: mi impute chained). Further information on the imputation procedure is given in the online supplementary materials.
tobaccocontrol-2017-053691supp001.pdf (162.4KB, pdf)
Results
Sample characteristics
In 2015, there were 3001 never smokers in our sample, of these 9.4% had tried an e-cigarette. Twenty-six per cent were coded as susceptible to smoking, 32.8% had a family member who smoked and 23.8% reported having at least one friend who smoked.
Our final sample included 2125 young people for whom we had data on e-cigarette use and smoking status at baseline and follow-up. Of these, 183 (8.6%) had tried an e-cigarette at baseline and 1942 (91.4%) had not. Table 1 shows the year group distribution of the sample by school.
Relationship between baseline e-cigarette use and smoking status at follow-up in baseline never smokers
Of the young people who had tried an e-cigarette at baseline (n=183), 74 (40.4%) went on to initiate smoking cigarettes by follow-up. This compares with 249 (12.8%) of those who reported never having used an e-cigarette at baseline (n=1942) and went on to initiate smoking cigarettes by follow-up. Table 2 shows the bivariate relationship between e-cigarette use in 2015 and smoking status in 2016.
Table 2.
Baseline e-cigarette use in 2015 and follow-up smoking status in 2016
| Have you ever smoked cigarettes or roll-ups, even if it is just one or two puffs? (2016) | Total | |||
| No | Yes | |||
| E-cigarette use (2015) | I have never used an e-cigarette | 1693 | 249 | 1942 |
| 87.2% | 12.8% | 100% | ||
| I have only used them once or twice | 104 | 65 | 169 | |
| 61.5% | 38.5% | 100% | ||
| I use them sometimes (monthly) | 3 | 5 | 8 | |
| 37.5% | 62.5% | 100% | ||
| I use them often (weekly) | 2 | 4 | 6 | |
| 33.3% | 66.7% | 100% | ||
| Total | 1802 | 323 | 2125 | |
| 84.9% | 15.2% | 100% | ||
Logistic regression on ‘experimented with cigarettes by follow-up’
Baseline e-cigarette use is a significant predictor of experimentation with cigarettes. In an unadjusted model, the OR for ever-smoking at follow-up in ever e-cigarette users versus never e-cigarette users was 4.62 (95% CI 3.34 to 6.38), giving a RR of 3.15 (95% CI 2.55 to 3.89). Table 3 below shows the ORs, p values and 95% CIs for the OR for each of the models. All the models below were adjusted for sex, age centred on the mean (ie, individual age minus the mean age of the sample) FAS, ethnic group and school.
Table 3.
Multivariate logistic regressions on ‘ever smoked a cigarette’ in 2016
| Variable | Model 1—adjusted main effects model (n=1806) | Model 2—adjusted model including interactions (n=1806) | Model 3—imputed model with interactions (n=2520) | ||||||
| OR | CI | p | OR | CI | p | OR | CI | p | |
| E-cigarette ever use 2015 | 2.42 | 1.63 to 3.60 | <0.001 | 5.97 | 3.12 to 11.40 | <0.001 | 6.64 | 3.60 to 12.26 | <0.001 |
| Susceptibility to smoking 2015 | 3.65 | 2.70 to 4.94 | <0.001 | 4.13 | 2.98 to 5.72 | <0.001 | 5.19 | 3.74 to 7.21 | <0.001 |
| Any family member smokes 2015 | 1.89 | 1.40 to 2.56 | <0.001 | 1.93 | 1.43 to 2.61 | <0.001 | 1.83 | 1. 37 to 2.44 | <0.001 |
| ‘At least some’ friends smoke 2015 | 1.33 | 0.95 to 1.85 | 0.094 | 1.56 | 1.09 to 2.25 | 0.016 | 1.51 | 1.07 to 2.14 | 0.020 |
| Interaction between e-cigarette and susceptibility | 0.42 | 0.19 to 0.94 | 0.036 | 0.42 | 0.20 to 0.88 | 0.021 | |||
| Interaction between e-cigarette and friends smoking | 0.49 | 0.23 to 1.07 | 0.072 | 0.52 | 0.25 to 1.09 | 0.082 | |||
Model 1 RR for e-cigarette use is 1.72 (95% CI 1.31 to 2.26), model 2 RR for e-cigarette use is 4.09 (95% CI 2.57 to 6.52), RR for e-cigarette*susceptibility interaction is 0.43 (95% CI 0.25 to 0.72), RR for e-cigarette*friend smokes interaction 0.62 (95% CI 0.39 to 0.99), model 3 RR for e-cigarette use is 4.22 (95% CI 2.83 to 6.36), RR for e-cigarette*susceptibility interaction is 0.41 (95% CI 0.26 to 0.64) and RR for e-cigarette*friend smokes interaction 0.65 (95% CI 0.44 to 0.97).
Figure 1 shows that the impact of having tried an e-cigarette at baseline on probability of tobacco experimentation at follow-up is much greater for young people who were non-susceptible to smoking at baseline. The contrast of predicted probabilities is significant (χ2=53.93, p<0.001).
Figure 1.
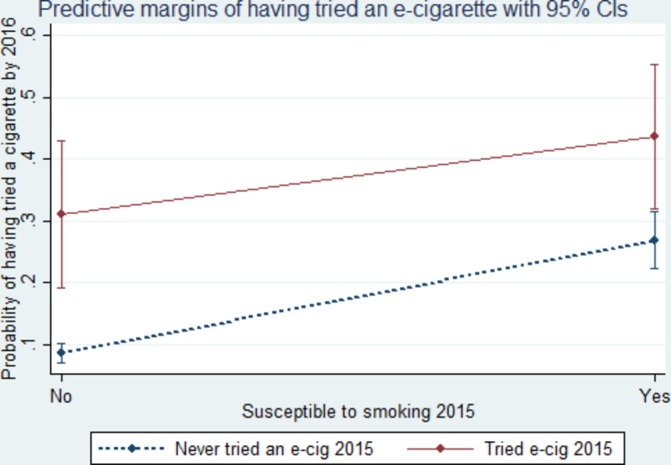
Marginal probabilities of cigarette experimentation by e-cigarette use and smoking susceptibility. e-cig, e-cigarette.
Figure 2 shows that the impact of having tried an e-cigarette at baseline on probability of tobacco experimentation at follow-up is much greater for young people who have no friends who smoke. The contrast of predicted probabilities is significant (χ2=4.91, p=0.042).
Figure 2.
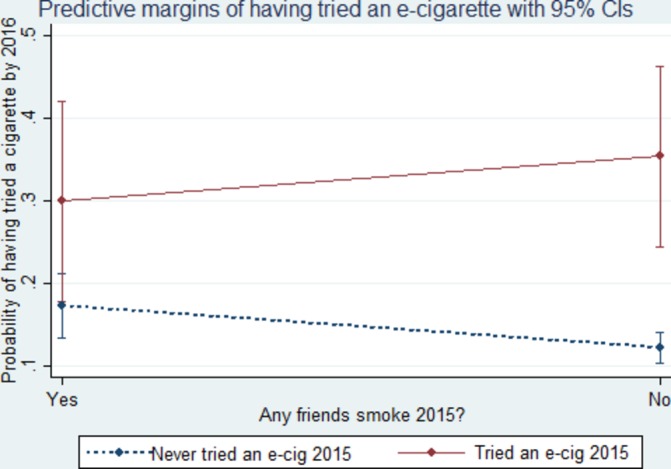
Marginal probabilities of cigarette experimentation by e-cigarette use and smokers within friendship. e-cig, e-cigarette.
Further information on characteristics of missing cases is given in online supplementary materials. To test the effect of missing data on our parameter estimates we used multiple imputation by chained equations. Model 3 shows the estimates from an imputed model (m=100). The model estimates are stable under complete case analysis and imputation.
Discussion
This study found that young ‘never-smokers’ who had tried an e-cigarette were more likely to try a cigarette during the following year than young never-smokers who had not tried an e-cigarette. This is consistent with the results of all previous published longitudinal studies of the relationship between e-cigarettes and tobacco experimentation in young people from the USA,3–9 providing further confirmation in a non-US context.
It is possible that the relationship between e-cigarettes and tobacco experimentation may not be causal if young never-smokers who try an e-cigarette would have gone on to initiate smoking anyway due to being already favourably disposed towards tobacco use. In other words, it is possible that e-cigarette use and tobacco experimentation have common liability25 and the former is incidental to tobacco experimentation. To address this possibility, we controlled for factors associated with transition to smoking such as smoking susceptibility26 and smoking among friends and family27 in the analysis. However, even when these items were included in the model e-cigarette use remained a significant predictor of cigarette experimentation. Importantly, there was also an interaction between smoking susceptibility and e-cigarette use and between e-cigarette use and having friends who smoked. These data indicate that e-cigarette use had a greater effect on the odds of cigarette experimentation in young people not traditionally thought to be high risk, that is, those with a firm intention not to smoke and/or those with no smokers in their friendship group.
There is some evidence from other studies that young people who try e-cigarettes before tobacco have different characteristics to those who go straight to smoking. Wills and colleagues28 found that those who used an e-cigarette first were less rebellious and more likely to receive social support from their parents. Miech and colleagues10 found that young never-smokers who had tried e-cigarettes were more likely to move away from the perception that cigarettes were a ‘great risk’ over the following year. Wills and colleagues29 also found that young never smokers who used e-cigarettes were also more likely to increase their positive smoking expectancies (such as beliefs that smoking would make them more confident, help them relax and reduce boredom) and were more likely to become friends with smokers and subsequently try smoking. However, with only 1-year follow-up these studies were not able to determine whether changes in expectancies or affiliations preceded smoking. Further research on this topic is required over longer follow-up periods.
Schneider and Diehl have outlined a ‘catalyst model’ of e-cigarette influence on smoking uptake in adolescence.30 This is intended as an alternative to ’gateway theory'31 32 as an explanation of the relationship between e-cigarette and tobacco use. They break the process down into two stages: factors influencing transition from ‘no use’ to ‘e-cigarette use’ and then the factors influencing the second stage of transition from ‘e-cigarette use’ to ‘tobacco use’. The first-stage mechanisms include easing the process of initial trial, for example, with sweet flavours. The second-stage mechanisms include increased accessibility and learning of smoking rituals. Thus, there are a number of paths within the catalyst model whereby e-cigarette use, even single trial, might facilitate smoking uptake. There are also pathways by which e-cigarettes could mitigate against a transition to regular smoking. For those young people who are curious to try the performative aspects of smoking (the hand to mouth action and inhalation process), the act of trying e-cigarettes may result in lower motivation to try tobacco smoking.
Levy and colleagues have modelled the public health impacts of e-cigarettes and estimate that under a range of conditions, e-cigarettes may have a positive net impact on public health at a population level because of the greater benefits conferred on smokers relative to the potential harm to young people.33 Further studies could usefully examine e-cigarette use, smoking and smoking-related attitudes over longer time periods to determine the conditions under which e-cigarettes enhance adult quit rates without facilitating uptake in young people.
The importance of research findings about the relationship between e-cigarette use and smoking initiation has been debated on the basis that most e-cigarette use among young people is occasional and therefore unlikely to be directly harmful or be sufficient to influence other behaviours. However, some argue that the influence of e-cigarette experimentation may be psychosocial rather than chemical; it has been suggested that e-cigarettes ‘(convey) to young apprehensive would-be smokers that nicotine is a benign drug and potentially weaken the established message that smoking kills’.34 E-cigarette advertising has emphasised the commonalities between the products with the message that e-cigarettes can give the psychological and social benefits of smoking without the health or social costs.35 There are some signs that these messages confuse young people about the harms of smoking. For example, a recent study found that after viewing an e-cigarette advert young people were more likely to rate occasional cigarette smoking as less harmful.36
At the time this research was conducted there were no legal restrictions on sales or advertisement of e-cigarettes. However, in the UK e-cigarettes are now banned from sale to people under 1837 38 and advertising on television, print media and radio is prohibited under the Tobacco Products Directive and associated UK regulations,39 40 although at present point-of-sale marketing is still permitted. It will be important to ascertain if this legislation is sufficient to prevent or reduce the numbers of young people trying e-cigarettes.
Strengths and limitations
The strengths of this study are its prospective design, large sample and high response and follow-up rates. Importantly, the multiple imputation models indicate that model estimates are not biased by missing data. However, there are a number of limitations. First, most of the young people whom we categorised as having initiated smoking may have only taken one or two puffs of a cigarette during the follow-up period. Therefore, we do not know whether any of these young people will transition to regular smoking. Transition from never-smoker to smoker is often conceptualised as a multistep pathway.41–43 Recent research suggests that any experimentation with cigarettes is a strong predictor of transition to regular smoking, with experimentation at baseline identifying two-thirds of regular smokers at 2-year follow-up with a false positive rate of only 8%.44
Second, participants were drawn from only four schools in Scotland and therefore may not be representative of the Scottish school population. However, comparison of the demographic characteristics of our sample with a nationally representative one does not indicate any significant deviation.45 Third, the study is based on self-reports and we do not yet know the reliability of young people’s self-reported use of e-cigarettes.
The age range of the sample (11–18 years) is broader than in some other research in this area. Therefore, we split our sample in half by age and repeated the analysis on the split samples. The results we obtained were the same and are presented in the online supplementary materials.
Finally, although we have used validated measures of smoking susceptibility, they were developed more than 20 years ago and there may be other aspects of common liability to tobacco and e-cigarette use that are not assessed by existing measures of susceptibility.
Conclusions
This UK longitudinal study found that young never-smokers who try e-cigarettes are at elevated risk of initiating smoking compared with young never-smokers who do not try e-cigarettes. Further research with longer follow-up is required to discover how many of the full sample of young people, if any, transition to regular smoking and to explore the longitudinal relationship between use of e-cigarettes and changes in attitudes to smoking. Careful and regular monitoring of smoking rates and e-cigarette use among young people is necessary over the coming years. This needs to be set within the context of the rapidly changing landscape of tobacco and nicotine product availability, recent changes in the regulation of advertising and strategies used by industry, particularly the tobacco industry, to promote these products.
What this paper adds.
Eight prospective studies in the USA have reported a temporal relationship between trying an e-cigarette and subsequent experimentation with cigarettes.
Consistent with the US studies, this study indicates a positive relationship between e-cigarette use in never smokers and their subsequent first experimentation with cigarettes by follow-up 1 year later.
This UK study found that e-cigarette use had a greater impact on the odds of cigarette experimentation in young never smokers not traditionally thought to be high risk, that is, those with a firm intention not to smoke and/or no smokers in their friendship group.
Footnotes
Contributors: CB conducted the analysis and wrote the first draft of the paper, DC, GO and FH managed the administration of the school survey, data cleaning and analysis and commented on the development of the paper, DE, MS, AMMK, JP, AA, AM and JF were coinvestigators responsible for devising the overall study design and commented on the development of the paper, SH is principal investigator for the DISPLAY study and was involved in devising the overall study, drafting and revising this paper and is its guarantor.
Funding: This project was funded by the UK National Institute for Health Research (NIHR) PHR project 10/3000/07. The study sponsor had no influence on study design and the collection, analysis, and interpretation of data and the writing of the article and the decision to submit it for publication.
Competing interests: None declared.
Ethics approval: University of St Andrews, School of Medicine Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Anonymised data from this study will be made publically available after the end of the study (December 2017). Stata syntax is available from the corresponding author on request.
References
- 1.Moore G, Hewitt G, Evans J, et al. Electronic-cigarette use among young people in Wales: evidence from two cross-sectional surveys. BMJ Open 2015;5:e007072 10.1136/bmjopen-2014-007072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bauld L, MacKintosh AM, Ford A, et al. E-Cigarette Uptake Amongst UK Youth: experimentation, but little or no regular use in nonsmokers. Nicotine Tob Res 2016;18:102–3. 10.1093/ntr/ntv132 [DOI] [PubMed] [Google Scholar]
- 3.Leventhal AM, Strong DR, Kirkpatrick MG, et al. Association of Electronic Cigarette Use with initiation of combustible tobacco product smoking in early adolescence. JAMA 2015;314:700 10.1001/jama.2015.8950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leventhal AM, Stone MD, Andrabi N, et al. Association of e-Cigarette Vaping and Progression to Heavier patterns of Cigarette Smoking. JAMA 2016;316:1918 10.1001/jama.2016.14649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barrington-Trimis JL, Urman R, Berhane K, et al. E-Cigarettes and future cigarette use. Pediatrics 2016;138 10.1542/peds.2016-0379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Primack BA, Soneji S, Stoolmiller M, et al. Progression to Traditional Cigarette Smoking after Electronic Cigarette Use among US Adolescents and Young adults. JAMA Pediatr 2015;169:1018–23. 10.1001/jamapediatrics.2015.1742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wills TA, Knight R, Sargent JD, et al. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control 2017;26:34–9. 10.1136/tobaccocontrol-2015-052705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Unger JB, Soto DW, Leventhal A. E-cigarette use and subsequent cigarette and marijuana use among hispanic young adults. Drug Alcohol Depend 2016;163:261–4. 10.1016/j.drugalcdep.2016.04.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spindle TR, Hiler MM, Cooke ME, et al. Electronic cigarette use and uptake of cigarette smoking: A longitudinal examination of U.S. college students. Addict Behav 2017;67:66–72. 10.1016/j.addbeh.2016.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miech R, Patrick ME, O’Malley PM, et al. E-cigarette use as a predictor of cigarette smoking: results from a 1-year follow-up of a national sample of 12th grade students. Tob Control 2017:tobaccocontrol-2016-053291 10.1136/tobaccocontrol-2016-053291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaleta D, Wojtysiak P, Polańska K. Use of electronic cigarettes among secondary and high school students from a socially disadvantaged rural area in Poland. BMC Public Health 2016;15:703 10.1186/s12889-016-3417-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aar? LE, Mazur J, Zato?ski WA, et al. Trends in smoking among polish and norwegian youth 1986-2014. Journal of Health Inequalities 2016;1:44–51. 10.5114/jhi.2016.61420 [DOI] [Google Scholar]
- 13.Currie C, Zanotti C, Morgan A, et al. Social Determinants of Health and Well-Being Among Young People. Health Behaviour in School-Aged Children (HBSC) Study: International Report From the 2009/2010 Survey. Copenhagen, 2012. http://www.euro.who.int/__data/assets/pdf_file/0003/163857/Social-determinants-of-health-and-well-being-among-young-people.pdf?ua=1 [Google Scholar]
- 14.Inchley J, Currie D, Young T, et al. Growing Up Unequal: Gender and Socioeconomic Differences in Young People’ S Health and Well-Being. Health Behaviour in School-Aged Children (HBSC) Study: International Report From the 2013/2014 Survey. Copenhagen: WHO Regional Office for Europe, 2016. http://www.euro.who.int/__data/assets/pdf_file/0003/303438/HSBC-No.7-Growing-up-unequal-Full-Report.pdf?ua=1 [Google Scholar]
- 15.Goniewicz ML, Leigh NJ, Gawron M, et al. Dual use of electronic and tobacco cigarettes among adolescents: a cross-sectional study in Poland. Int J Public Health 2016;61:189–97. 10.1007/s00038-015-0756-x [DOI] [PubMed] [Google Scholar]
- 16. Scottish Government. Scottish Schools Adolescent Lifestyle and Substance Use Survey (SALSUS). Edinburgh, 2016. http://www.gov.scot/Publications/2016/10/5514 [Google Scholar]
- 17. Scottish Government. Scottish Health Survey 2015. Edinburgh, 2016. https://beta.gov.scot/publications/scottish-health-survey-2015-volume-1-main-report/. [Google Scholar]
- 18.de Lacy E, Fletcher A, Hewitt G, et al. Cross-sectional study examining the prevalence, correlates and sequencing of electronic cigarette and tobacco use among 11-16-year olds in schools in Wales. BMJ Open 2017;7:e012784 10.1136/bmjopen-2016-012784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eadie D, Stead M, MacKintosh AM, et al. E-cigarette marketing in UK stores: an observational audit and retailers' views. BMJ Open 2015;5:e008547 10.1136/bmjopen-2015-008547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haw S, Amos A, Eadie D, et al. Determining the impact of smoking point of sale legislation among youth (Display) study: a protocol for an evaluation of public health policy. BMC Public Health 2014;14:251 10.1186/1471-2458-14-251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pierce JP, Choi WS, Gilpin EA, et al. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol 1996;15:355–61. 10.1037/0278-6133.15.5.355 [DOI] [PubMed] [Google Scholar]
- 22.Currie C, Molcho M, Boyce W, et al. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med 2008;66:1429–36. 10.1016/j.socscimed.2007.11.024 [DOI] [PubMed] [Google Scholar]
- 23.Leatherdale ST, Manske S. The relationship between student smoking in the school environment and smoking onset in elementary school students. Cancer Epidemiol Biomarkers Prev 2005;14:1762–5. 10.1158/1055-9965.EPI-05-0065 [DOI] [PubMed] [Google Scholar]
- 24.Cummings P. Methods for estimating adjusted risk ratios. Stata J 2010;10:288–308. [Google Scholar]
- 25.Vanyukov MM, Tarter RE, Kirillova GP, et al. Common liability to addiction and "gateway hypothesis": theoretical, empirical and evolutionary perspective. Drug Alcohol Depend 2012;123:S3–S17. 10.1016/j.drugalcdep.2011.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nodora J, Hartman SJ, Strong DR, et al. Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav 2014;39:1695–700. 10.1016/j.addbeh.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Loughlin J, Paradis G, Renaud L, et al. One-year predictors of smoking initiation and of continued smoking among elementary schoolchildren in multiethnic, low-income, inner-city neighbourhoods. Tob Control 1998;7:268–75. 10.1136/tc.7.3.268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wills TA, Sargent JD, Gibbons FX, et al. E-cigarette use is differentially related to smoking onset among lower risk adolescents. Tob Control 2016. 10.1136/tobaccocontrol-2016-053116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wills TA, Gibbons FX, Sargent JD, et al. How is the effect of adolescent e-cigarette use on smoking onset mediated: a longitudinal analysis. Psychol Addict Behav 2016;30:876–86. 10.1037/adb0000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneider S, Diehl K. Vaping as a Catalyst for Smoking? an Initial Model on the initiation of Electronic Cigarette Use and the transition to tobacco smoking among adolescents. Nicotine Tob Res 2016;18:647–53. 10.1093/ntr/ntv193 [DOI] [PubMed] [Google Scholar]
- 31.Mayet A, Legleye S, Beck F, et al. The Gateway hypothesis, common liability to addictions or the route of Administration Model A Modelling process linking the three theories. Eur Addict Res 2016;22:107–17. 10.1159/000439564 [DOI] [PubMed] [Google Scholar]
- 32.Kandel D. Stages in adolescent involvement in drug use. Science 1975;190:912–4. 10.1126/science.1188374 [DOI] [PubMed] [Google Scholar]
- 33.Levy DT, Borland R, Villanti AC, et al. The application of a Decision-Theoretic Model to Estimate the Public Health Impact of Vaporized Nicotine Product initiation in the United States. Nicotine Tob Res 2017;19:ntw158 10.1093/ntr/ntw158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chapman S. Should electronic cigarettes be as freely available as tobacco cigarettes? no. BMJ 2013;346:f3840. [DOI] [PubMed] [Google Scholar]
- 35.de Andrade M, Hastings G, Angus K. Promotion of electronic cigarettes: tobacco marketing reinvented? BMJ 2013;347:f7473. [DOI] [PubMed] [Google Scholar]
- 36.Petrescu DC, Vasiljevic M, Pepper JK, et al. What is the impact of e-cigarette adverts on children’s perceptions of tobacco smoking? An experimental study. Tob Control 2017;26 10.1136/tobaccocontrol-2016-052940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Department for Education & Department of Health. Children and Families Act 2014. UK: Queen’s Printer of Acts of Parliament, 2014. [Google Scholar]
- 38. Scottish Government. Health (Tobacco, Nicotine etc. and Care) (Scotland) Bill: The Scottish Parliament, 2015. [Google Scholar]
- 39. EU Commission. Directive 2014/40/EU of the European Parliament and of the Council of 3 April 2014 on the Approximation of the Laws, Regulations and Administrative Provisions of the Member States Concerning the Manufacture, Presentation and Sale of Tobacco and Related Products: European Union, 2014. [Google Scholar]
- 40. UK Government. The Tobacco and Related Products Regulations. UK, 2016. [Google Scholar]
- 41.Leventhal H, Cleary PD. The smoking problem: a review of the research and theory in behavioral risk modification. Psychol Bull 1980;88:370–405. 10.1037/0033-2909.88.2.370 [DOI] [PubMed] [Google Scholar]
- 42.Stern RA, Prochaska JO, Velicer WF, et al. Stages of adolescent cigarette smoking acquisition: measurement and sample profiles. Addict Behav 1987;12:319-29. [DOI] [PubMed] [Google Scholar]
- 43.Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug Alcohol Depend 2000;59 Suppl 1:61–81. 10.1016/S0376-8716(99)00165-9 [DOI] [PubMed] [Google Scholar]
- 44.Sargent JD, Gabrielli J, Budney A, et al. Adolescent smoking experimentation as a predictor of daily cigarette smoking. Drug Alcohol Depend 2017;175:55–9. 10.1016/j.drugalcdep.2017.01.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dodds B, Wood L, Bainbridge R. Scottish Schools Adolescent Lifestyle and Substance Use Survey (SALSUS). National Report. Edinburgh, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
tobaccocontrol-2017-053691supp001.pdf (162.4KB, pdf)


