Abstract
Depression is a disabling affective disorder for which the majority of patients are not effectively treated. This problem is exacerbated in children and adolescents for whom only two antidepressants are approved, both of which are selective serotonin reuptake inhibitor (SSRIs). Unfortunately SSRIs are often less effective in juveniles than in adults; however, the mechanism(s) underlying age-dependent responses to SSRIs is unknown. To this end, we compared the antidepressant-like response to the SSRI escitalopram using the tail suspension test and saturation binding of [3H]citalopram to the serotonin transporter (SERT), the primary target of SSRIs, in juvenile [postnatal day (P)21], adolescent (P28), and adult (P90) wild-type (SERT+/+) mice. In addition, to model individuals carrying low-expressing SERT variants, we studied mice with reduced SERT expression (SERT+/−) or lacking SERT (SERT−/−). Maximal antidepressant-like effects were less in P21 mice relative to P90 mice. This was especially apparent in SERT+/− mice. However, the potency for escitalopram to produce antidepressant-like effects in SERT+/+ and SERT+/− mice was greater in P21 and P28 mice than in adults. SERT expression increased with age in terminal regions and decreased with age in cell body regions. Binding affinity values did not change as a function of age or genotype. As expected, in SERT−/− mice escitalopram produced no behavioral effects, and there was no specific [3H]citalopram binding. These data reveal age- and genotype-dependent shifts in the dose-response for escitalopram to produce antidepressant-like effects, which vary with SERT expression, and may contribute to the limited therapeutic response to SSRIs in juveniles and adolescents.

Introduction
Depression is a disabling affective disorder for which the majority of patients are not effectively treated. This problem is exacerbated in juveniles and adolescents by limited therapeutic options (Bylund and Reed, 2007). Only two selective serotonin (5-HT) reuptake inhibitor (SSRI) antidepressants, escitalopram and fluoxetine, have U.S. Food and Drug Administration approval as treatments for pediatric depression. SSRIs act on the serotonergic system by blocking the 5-HT transporter (SERT) (SLC6A4), the high affinity clearance mechanism for extracellular 5-HT. The resultant increase in extracellular 5-HT is thought to trigger therapeutic downstream effects. However, escitalopram and fluoxetine are often less effective in treating symptoms of depression in juveniles and adolescents than in adults (Tsapakis et al., 2008; Hetrick et al., 2007, 2010). Furthermore, in adolescents certain SERT gene variants are associated with increased risk of developing SSRI-resistant depression after stressful life events, triggering a lifelong struggle with the disorder (Serretti et al., 2007; Petersen et al., 2012). Given the high incidence of depression in adolescents, which comprises 4%–8% of the U.S. population, and the fact that suicide is the third most likely cause of death in this age group, there is a distinct need to uncover mechanism(s) limiting the therapeutic benefits of SSRIs in young patients (Kessler et al., 2001; Bujoreanu et al., 2011). A better understanding of the age dependency of SSRI efficacy is therefore an important first step toward improving therapeutics for pediatric depression.
Rodents are indispensable tools for studying the behavioral and neurochemical effects of antidepressants. However, most studies to date have focused on antidepressant-like behavior in adult rodents and have largely ignored the use of juveniles and adolescents. One study reported that SSRIs reduced immobility time in the forced swim test (FST), an index of antidepressant-like action, in juvenile [postnatal day (P)21] and adolescent (P28–P35) rats (Reed et al., 2008). Recently, we discovered differences in behavioral responses to SSRIs in juvenile mice. We used escitalopram at a dose of 10 mg/kg, which is known to produce maximal antidepressant-like effects in adult mice in the tail suspension test (TST), an assay commonly used to assess antidepressant-like activity in mice (Cryan et al., 2005; O’Leary et al., 2007). At this dose the antidepressant-like effect of escitalopram was less in juvenile mice than in adult mice (Mitchell et al., 2013), a finding consistent with clinical reports. The present study expands upon this initial finding by examining the dose dependency of escitalopram’s antidepressant-like effects in juvenile (P21), adolescent (P28), and adult (P90) mice. In addition, because individuals carrying low-expressing variants of SERT are often reported to benefit less from treatment with SSRIs than individuals who do not harbor such gene variants, we studied mice with reduced SERT expression (SERT+/−) or lacking SERT (SERT−/−) and compared them to wild-type mice (SERT+/+).
In murine models, serotonergic neuronal innervation, dendritic connections, and extracellular 5-HT concentration have been shown to be similar to adults by P21 (Loizou and Salt, 1970; Wallace and Lauder, 1983; Miranda-Contreras et al., 1998). These studies suggest that some aspects of the central serotonergic system are functionally developed in juveniles; however, a developmental lag in SERT expression or function could limit the therapeutic benefit of SSRIs. In rats, SERT expression reaches adult levels between birth and P21 with expression patterns varying in different brain regions (Moll et al., 2000; Galineau et al., 2004; Bylund and Reed, 2007; Slotkin et al., 2008). However, these studies did not evaluate possible developmental changes in SERT affinity (Kd). Recently, we discovered that SERT binding properties in juvenile (P21) and adolescent (P28) mice may differ from adults. While maximal binding (Bmax) of the SERT-selective ligand, [3H]citalopram, in hippocampal membranes revealed no differences among ages, variance in the Kd value for P21 mice was significantly greater than in older mice (Mitchell et al., 2013), suggesting that the functionality of SERT may be at a developmentally dynamic transitional stage. To better characterize age- and brain region–dependent changes in SERT function, the present study used quantitative autoradiography, an anatomically more sensitive assay, to examine [3H]citalopram binding properties and their relation to behavior in the TST.
Materials and Methods
Animals
Male and female SERT wild-type (SERT+/+), heterozygote (SERT+/−), or homozygote knockout (SERT−/−) mice (backcrossed to C57BL/6J for >10 generations) were used for all experiments. Colony founders were provided by Dr. Dennis Murphy (National Institute of Mental Health, Bethesda, MD), and were bred and identified as previously described (Bengel et al., 1998). P21 (juvenile), P28 (adolescent), and P90–P100 (adult) mice (Spear, 2000) were used. Mice of each genotype were generated by crossing male and female SERT+/− mice. Animals were housed in a temperature-controlled (24°C) vivarium maintained on a 12/12-hour light/dark cycle (lights on at 7:00 AM) in plastic cages (29 × 18 × 13 cm) containing rodent bedding (Sani-chips; Harlan Teklad, Madison, WI) with free access to food (irradiated rodent sterilizable diet; Harlan Teklad) and water. After weaning on P28, mice were housed in groups of five with same-sex peers. TST experiments were conducted prior to weaning in mice aged P21 and P28. All procedures were conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals (Institute of Laboratory Animal Resources, Commission on Life Sciences, National Research Council, https://grants.nih.gov/grants/olaw/Guide-for-the-Care-and-use-of-laboratory-animals.pdf), and with the approval of the Institutional Animal Care and Use Committee at the University of Texas Health Science Center.
Tail Suspension Test
The TST was conducted as originally described by Steru et al. (1985) (for a review, see Castagné et al., 2011). Naive mice were moved from the colony room to the testing room and allowed a 1- to 2-hour acclimation period. All experiments were conducted between 12:00 and 5:00 PM. All mice received saline vehicle i.p. 1 hour before testing, followed 30 minutes later by s.c. injection of either escitalopram (0.1, 0.32, 1.0, 3.2, or 10.0 mg/kg) or saline vehicle (control condition). This drug administration protocol was selected to be consistent with previously published procedures (Baganz et al., 2008; Horton et al., 2013; Mitchell et al., 2015). In addition, administration of antidepressant 30 minutes before testing is standard (Steru et al., 1985; Holmes et al., 2002; Ripoll et al., 2003). Immediately before testing, the distal portion of the tail was fastened to a flat aluminum bar (2 × 0.3 × 10 cm) using adhesive tape placed at a 90° angle to the longitudinal axis of the mouse tail, with 3 to 4 cm between the base of the mouse tail and the aluminum bar. A hole opposite the taped end of the bar was used to secure the bar to a hook on the ceiling of a visually isolated white box (40 × 40 × 40 cm). Each mouse was suspended by its tail for 6 minutes, allowing the ventral surface and the front and hind limbs to be recorded using a digital video camera facing the testing box. Total immobility time was measured (in seconds) during the 6-minute time period. Immobility was defined as the absence of initiated movements, and included passive swaying of the body. A mouse was excluded from the study if it climbed and held its tail or the aluminum bar for a period of 3 seconds or longer. Immobility was scored twice from the videos by observers who were blind to the treatments. Each mouse was tested only once, and all mice were randomly assigned to treatments.
Drugs
Escitalopram [s-citalopram or (S)-1[3-(Dimethylamino)propyl]-1-(4-fluorophenyl)-1,3-dihydroisobenzofuran-5-carbonitrile] oxalate (Sigma-Aldrich, St. Louis, MO) was dissolved in physiologic saline and injected s.c. at doses expressed as base weight per kilogram body weight. The injection volume was 10 ml/kg. Drug doses were chosen that ranged from subthreshold (0.32 mg/kg) to maximally effective (10 mg/kg) in adult SERT+/+ mice.
Autoradiography
SERT saturation binding was assessed in mouse brain by quantitative autoradiography using the SERT-selective ligand [3H]citalopram and methods adapted from D’Amato et al., (1987). Naive mice were killed by decapitation and brains rapidly removed and frozen on powdered dry ice before being stored at −80°C until sectioned for quantitative autoradiography. Brains were brought to −20°C in a cryostat (Leica CM 1850, Meyer Instruments, Houston, TX) and coronal sections (20 µm) were collected at the level of plate 12 (prefrontal cortex), plate 47 [hippocampal subregions, cornu ammonis (CA) 1–3 and dentate gyrus; parietal cortex; amygdala; and ventromedial hypothalamus], and plate 64 (raphe nuclei) according to the Paxinos and Franklin (1997) mouse brain atlas. Sections were thaw mounted onto gelatin-coated microscope slides, vacuum desiccated for 18–24 hours at 4°C and stored at −80°C until use. In preparation for binding, sections were thawed and then preincubated for 1 hour in a 50 mM Tris-HCl, 120 mM NaCl, and 5 mM KCl pH 7.4 at room temperature (∼24°C). Incubation was carried out in slide mailers (VWR International, Radnor, PA) filled with 10 ml of the same buffer containing [3H]citalopram at concentrations of 0.32, 0.56, 1.0, 3.2, or 5.6 nM for 1 hour at room temperature. Nonspecific binding was defined by 20 µM sertraline (Pfizer, Groton, CT) and was ∼11%–23% total binding in low-binding regions (i.e., parietal cortex) and ∼5%–9% total binding in high-binding regions (i.e., dorsal raphe). The incubation was terminated by two 10-minute washes in 50 mM Tris-HCl, 120 mM NaCl, 5 mM KCl pH 7.4 at 4°C, followed by a 5-second dip in deionized water at 4°C. Slides were dried on a slide warmer for 20 minutes. [3H]citalopram-labeled sections were exposed to Carestream Biomax MR film for 6 weeks, along with tritium standards (American Radiolabeled Chemicals, St Louis, MO). Films were developed in a film processor (AFP imaging, Elmsford, NY). Autoradiogram images were captured on a digital image system: 12-digital bit camera (CFW-1612M, Scion Corp., Frederick, MD), Nikon Lens, Northern Lights Illuminator, and Kaiser RS1 copy stand (all from InterFocus Imaging Ltd., Linton, United Kingdom), and were calibrated and measured with the National Institutes of Health Image J public access shareware https://imagej.nih.gov/ij/download.html on a MacBook (OS 10).
Data Analysis
Statistical analyses were performed using Prism 6.0 (GraphPad, San Diego, CA).
TST.
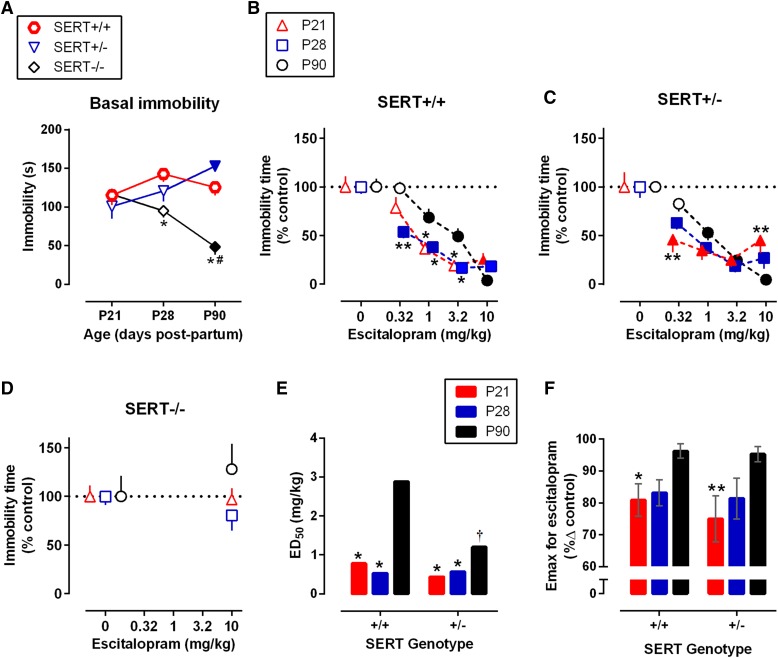
Under vehicle conditions, Mitchell et al. (2013, 2015) previously found that time spent immobile varies by age and SERT genotype. Because similar findings were obtained here (Fig. 1A), dose-response data were expressed as percentage from vehicle control (Fig. 1, B–D) and analyzed by two-factor analysis of variance (ANOVA), i.e., age and drug dose, followed by Tukey’s and Dunnett’s multiple comparisons tests. Within each genotype and age group there were no significant differences in drug-induced immobility between males and females (main effect of sex: P ≥ 0.11; interaction between sex and dose, P ≥ 0.10; data not shown); thus, data for both sexes were pooled. Maximal effect (Emax) and half-maximally effective dose (ED50) values, derived from data shown in Fig. 1, B and C are shown in Fig. 1, E and F. All data are expressed as mean ± S.E.M., except the ED50 values, which are expressed as the mean. P < 0.05 was considered statistically significant.
Fig. 1.
Escitalopram reduces immobility time in the TST in juvenile, adolescent, and adult mice as a function of SERT genotype. (A) Basal immobility time (saline-injected controls) in seconds across age and SERT genotype. Solid symbols represent a significant difference from P21 with Dunnett’s post hoc multiple comparisons test after two-factor ANOVA (age, SERT genotype) *P < 0.05 represents the difference from age-matched SERT+/+ and #P < 0.05 represents the difference from age-matched SERT+/− with Tukey’s post hoc multiple comparisons test. (B–D) Escitalopram dose-effect curves across age in SERT+/+, SERT+/−, and SERT−/− mice. Immobility expressed as a percentage of saline-injected controls. Solid symbols represent a significant difference from vehicle treatment with Dunnett’s post hoc multiple comparisons test after two-factor ANOVA (age, drug dose) performed separately for each genotype. *P < 0.05, **P < 0.01 represent a significant difference from SERT gene–matched P90; Tukey’s post hoc multiple comparisons test. (E) Half-maximally effective dose (ED50); *P < 0.05, **P < 0.01 represent a significant difference from SERT gene–matched P90; † P < 0.05 P90 SERT+/+ versus P90 SERT+/−. (F) Maximal effect (Emax, expressed as a percent from control) of dose-effect curves (B and C); *P < 0.05, **P < 0.01 represent a significant difference from SERT gene–matched P90 with Tukey’s post hoc multiple comparisons test after two-factor ANOVA (age, SERT genotype). There were no statistically significant main effects of sex or sex × dose interactions in any age group or SERT genotype; therefore, data for both genders were pooled. Data are mean ± S.E.M., except for ED50 values, which are expressed as mean. SERT+/+, n = 17–31 (males n = 4–16 and females n = 9–21 pooled); SERT+/−, n = 14–20 (males n = 8–10 and females n = 6–11 pooled); and SERT−/−, n = 18–26 (males n = 9–14 and females 8–12 pooled) per data point.
The Emax value was defined as the greatest observed percentage change in immobility from the saline control condition. To calculate the ED50 values, time spent immobile was expressed as the percentage of the vehicle control, and the linear portion of the dose-response curves was analyzed by log-linear regression of data from individual subjects with the following equation: effect = slope × log(dose) + intercept, using methods detailed elsewhere (Koek et al., 2009). Maximal effects were analyzed using two-factor ANOVA (age and genotype) followed by Tukey’s multiple comparisons test.
Quantitative Autoradiography.
Nonspecific binding was subjected to unweighted linear regression and subtracted from total [3H]citalopram binding to give specific binding. Specific [3H]citalopram binding data were submitted to unweighted nonlinear regression and the saturation binding isotherm fitted according to a one-site model: Y = Bmax * X/(Kd + X). Mean Bmax and Kd values were analyzed using two-factor (age and genotype) ANOVA (Fig. 4), with Tukey’s post hoc test for multiple comparisons. Within genotype-, age-, and brain region–matched groups there were no statistically significant differences in Bmax and Kd values for [3H]citalopram binding between males and females; thus, data from both sexes were pooled (P ≥ 0.051) (data not shown). All data are expressed as mean ± S.E.M. P < 0.05 was considered statistically significant.
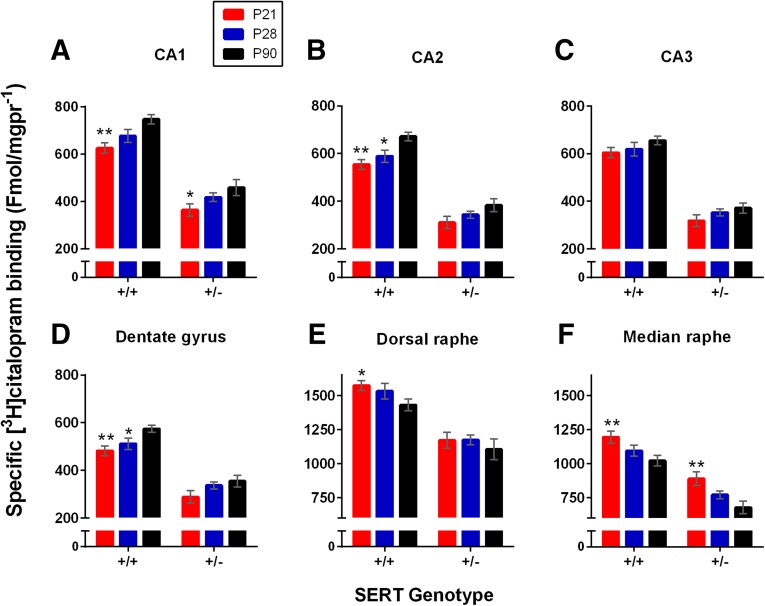
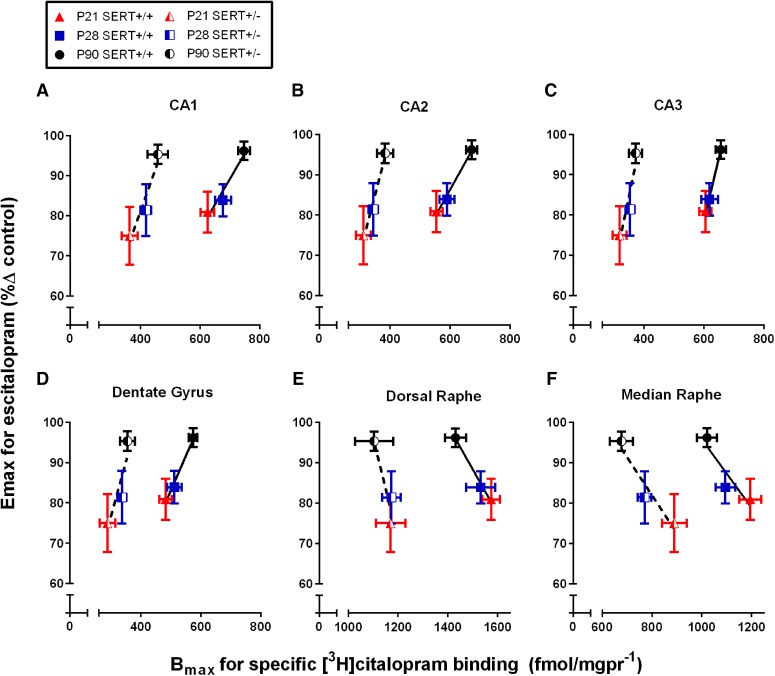
Fig. 4.
Bmax values for [3H]citalopram binding to SERT in SERT+/+ and SERT+/− mice aged P21, P28, and P90. The Bmax values were determined from one-site curve fits to data plotted in Fig. 2, B–D and Fig. 3, B and C from P21 (red), P28 (blue), and P90 (black) SERT+/+ and SERT+/− mice. Data are mean ± S.E.M. pooled from male and female mice. *P < 0.05, **P < 0.01 represent a significant difference from SERT gene–matched P90, Tukey’s post hoc multiple comparisons test after repeated-measure two-factor ANOVA (age, brain region). SERT+/+, n = 8–11 (males n = 5 and females n = 3–6 pooled); and SERT+/−, n = 5–10 (males n = 3–5 and females 2–5 pooled).
Correlations.
As shown in Fig. 4, A–F, Pearson’s correlation was used to examine the relationship between the Emax value for escitalopram to reduce immobility time in the TST values taken from Fig. 1F, and maximal specific [3H]citalopram binding values taken from Fig. 4, A–F. All data are expressed as mean ± S.E.M.
Results
Maximal Effect and Potency of Escitalopram to Reduce Immobility Time in the TST Is Age- and SERT-Genotype Dependent
Under control (saline-injected) conditions (Fig. 1A), basal immobility varied in an age- and genotype-dependent manner [age versus SERT-genotype interaction: F(4,169) = 7.35, P < 0.0001]. Baseline immobility increased in age SERT+/− mice, but not in SERT+/+ or SERT−/− mice (Fig. 1A). At P21, differences among the genotypes were not statistically significant. At P28 and P90, SERT−/− mice showed less immobility than SERT+/+ mice. At P90, SERT−/− mice showed less immobility than at P21; in contrast, SERT+/− mice showed more immobility at P90 than at P21.
In SERT+/+ mice, escitalopram reduced immobility time in the TST in all age groups [F(4,299) = 56.3, P < 0.0001] (Fig. 1B). Overall, P21 and P28 mice spent less time immobile than P90 mice following escitalopram [F(2,299) = 7.86, P = 0.0005]. In addition, escitalopram dose interacted with age [F(8,299) = 3.39, P = 0.001]: at low doses, P21 and P28 mice showed less immobility than mice aged P90. P21 SERT+/+ mice spent less time immobile than P90 mice following 1.0 and 3.2 mg/kg doses of escitalopram (P = 0.013 and 0.012, respectively), and P28 SERT+/+ mice spent significantly less time immobile than P90 mice following 0.32, 1.0, and 3.2 mg/kg doses of escitalopram (P < 0.0001 and P = 0.013 and 0.005, respectively). There was no significant difference in time spent immobile among ages following 10 mg/kg escitalopram, although there was a trend for P21 mice to spend more time immobile than P90 mice (P = 0.11). The lowest effective dose for P28 was 0.32 mg/kg escitalopram (P = 0.0004), while 1.0 mg/kg was the lowest for P21 (P < 0.0001) and P90 mice (P = 0.008).
As for SERT+/+ mice, escitalopram reduced immobility in all age groups of SERT+/− mice [F(4,250) = 37.4, P < 0.0001] and its effects interacted with age [F(8,250) = 2.60, P = 0.0095] (Fig. 1C). P21 SERT+/− mice spent significantly less time immobile than P90 SERT+/− mice following 0.32 mg/kg escitalopram (P = 0.01), but significantly more time immobile following 10 mg/kg escitalopram (P = 0.006). The lowest effective dose for P21 and P28 SERT+/− mice was 0.32 mg/kg (P < 0.001 and P = 0.014, respectively), while the lowest effective dose for P90 SERT+/− mice was 1.0 mg/kg (P < 0.001).
Because previous studies have shown that SSRIs do not produce antidepressant-like effects in SERT−/− mice (Holmes et al., 2002), we evaluated only the 10 mg/kg dose of escitalopram, which is maximally effective in P90 SERT+/+ and SERT+/− mice. As expected, there was no effect of drug [F(1,115) = 0.86, P = 0.42], age [F(2,115) = 0.86, P = 0.42], or interaction [F(2,115) = 0.86, P = 0.42] (Fig. 1D). There were no significant differences in immobility among ages and between vehicle and 10 mg/kg escitalopram.
The ED50 and Emax values for escitalopram to reduce immobility time in SERT+/+ and SERT+/− mice are summarized in Fig. 1, E and F (SERT−/− mice were not included in the analysis because escitalopram did not alter immobility time in these mice). The ED50 value of escitalopram to inhibit immobility varied as a function of age [SERT+/+: F(2,191) = 19.45, P < 0.001; SERT+/−: F(2,156) = 4.18, P = 0.017]; escitalopram more potently inhibited immobility in P21 and P28 mice than in P90 mice for both genotypes [SERT+/+: F(1,133) = 15.7, P < 0.001, and F(1,137) = 34.7, P < 0.001; SERT+/−: F(1,104) = 6.24, P = 0.014, and F(1,110) = 5.7, P = 0.019] (Fig. 1E). Within-age comparisons showed no potency difference of escitalopram to reduce immobility in SERT+/+ and SERT+/− mice aged P21 and P28. However, at P90 the ED50 value was significantly lower in SERT+/− mice than in SERT+/+ mice [F(1,138) = 8.35, P = 0.005].
In SERT+/+ and SERT+/− mice, the Emax values for escitalopram were smaller in young mice than in adult (P90) mice [F(2,103) = 7.59, P < 0.001] (Fig. 1F). Genotype had no effect on the Emax values [F(1,103) = 0.55, P = 0.46], nor was there an age-by-genotype interaction [F(2,103) = 7.59, P = 0.86]. The Emax values in SERT+/+ and SERT+/− mice aged P21 were smaller than those for genotype-matched P90 mice (P = 0.047 and 0.008, respectively). No significant difference was found between P28 and P90 Emax values in SERT+/+ and SERT+/− mice (P = 0.12 and 0.10, respectively).
In summary, for SERT+/+ and SERT+/− mice the ED50 value for escitalopram to decrease immobility time was lower in P21 and P28 mice than in P90 mice, suggesting that escitalopram is more potent in juvenile and adolescent mice than in adult mice. In contrast, the Emax values were smaller in young mice than in P90 mice, suggesting that escitalopram is less efficacious in juvenile and adolescent mice than in adult mice.
SERT Expression Increases with Age in Select 5-HT Terminal Regions and Decreases with Age in Cell Body Regions
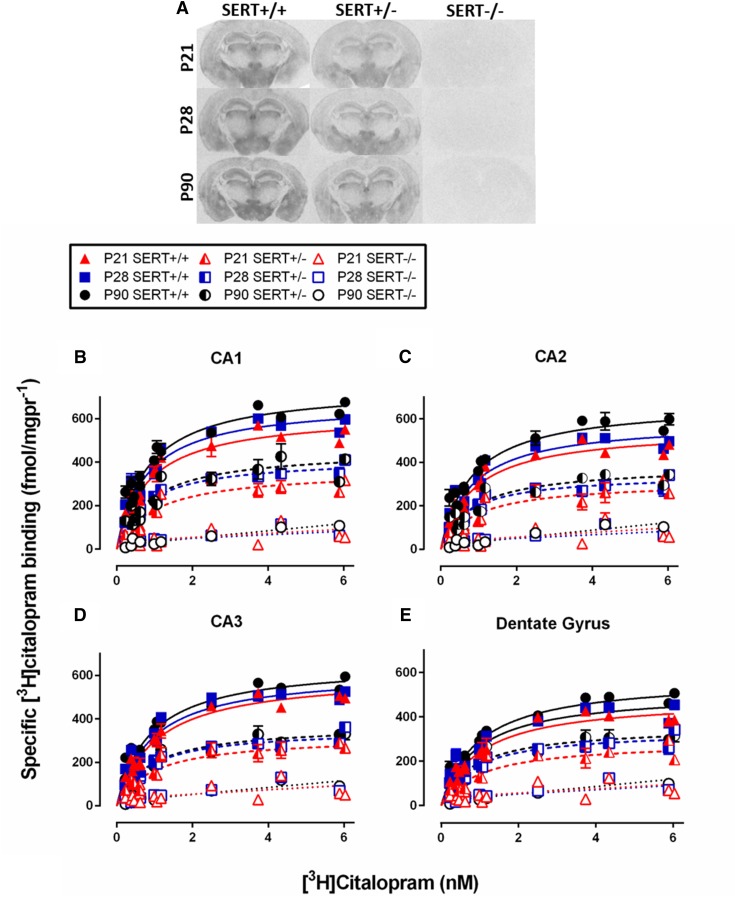
Maximal specific [3H]citalopram binding (Bmax) values and Kd values derived from curve fitting were analyzed separately for each brain region with two-factor ANOVA (age and genotype) (Figs. 2–4; Table 1). As expected, [3H]citalopram binding in SERT+/− mice was less than that in SERT+/+ mice and there was no [3H]citalopram binding detected in SERT−/− mice (Figs. 2 and 3).
Fig. 2.
Specific binding of [3H]citalopram to SERT in hippocampal subregions as a function of age and SERT genotype. Brain sections from P21, P28, and P90 mice were incubated with increasing concentrations of [3H]citalopram. Nonspecific binding was defined by sertraline (20µM). (A) Representative coronal sections showing [3H]citalopram binding at the level of plate 47 (Paxinos and Franklin, 1997) in P21, P28, and P90, SERT+/+, SERT+/−, and SERT−/− mice. Saturation binding isotherms in CA1 (B), CA2 (C), and CA3 (D) regions of hippocampus, and dentate gyrus (E) of P21, P28, and P90, SERT+/+, SERT+/−, and SERT−/− mice. The Bmax values for each curve are summarized in Fig. 4. There were no significant differences in Kd values among ages or between SERT+/+ and SERT+/− mice. There was no significant difference between males and females for any age or SERT genotype; therefore, data for both genders were pooled. SERT+/+, n = 8–11 (males n = 5 and females n = 3–6 pooled); SERT+/−, n = 5–10 (males n = 3–5 and females 2–5 pooled); and SERT−/−, n = 2–4 (males n = 1 to 2 and females n = 1 to 2 pooled) mice per group. Note that because binding in SERT−/− mice was not different from background the sample size was not further increased.
TABLE 1.
Summary of Bmax values for specific [3H]citalopram binding in SERT+/+ and SERT+/− mice
Data are mean ± S.E.M. fmol/mg protein. There was no significant difference between males and females for any age or SERT genotype; therefore, data for both genders were pooled. Tukey’s multiple comparisons test after two-factor ANOVA, n = 8–11.
| Genotype | P21 | P28 | P90 |
|---|---|---|---|
| Prefrontal cortex | |||
| SERT+/+ | 568 ± 25 | 588 ± 25 | 583 ± 18 |
| SERT+/− | 322 ± 32 | 331 ± 15 | 363 ± 28 |
| Parietal cortex | |||
| SERT+/+ | 342 ± 24* | 382 ± 21 | 431 ± 24 |
| SERT+/− | 186 ± 37 | 214 ± 24 | 225 ± 22 |
| Amygdala | |||
| SERT+/+ | 970 ± 31 | 1032 ± 29 | 1058 ± 29 |
| SERT+/− | 669 ± 58 | 678 ± 21a | 801 ± 48 |
| Ventromedial hypothalamus | |||
| SERT+/+ | 999 ± 38 | 933 ± 37 | 938 ± 30 |
| SERT+/− | 696 ± 57 | 677 ± 29 | 597 ± 37 |
Difference from SERT genotype–matched P90 group, *P < 0.05.
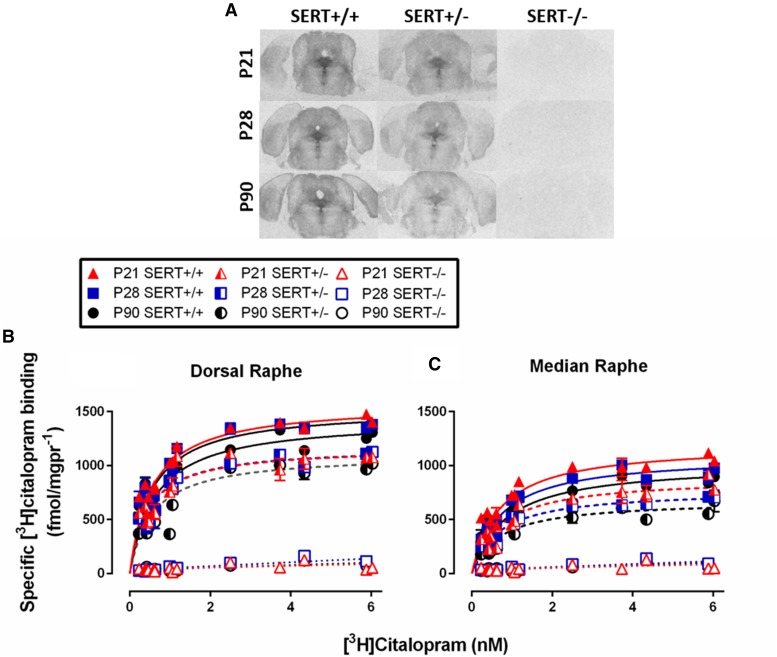
Fig. 3.
Specific binding of [3H]citalopram to SERT in dorsal and median raphe nuclei as a function of age and SERT genotype. Brain sections from P21, P28, and P90 mice were incubated with increasing concentrations of [3H]citalopram. Nonspecific binding was defined by sertraline (20µM). (A) Representative coronal sections showing [3H]citalopram binding at the level of plate 64 (Paxinos and Franklin, 1997) in P21, P28, and P90, SERT+/+, SERT+/−, and SERT−/− mice. Saturation binding isotherms in dorsal raphe (B) and median raphe (C) of P21, P28, and P90, SERT+/+, SERT+/−, and SERT−/− mice. The Bmax values for each curve are summarized in Fig. 4. There were no significant differences in Kd values among ages or between SERT+/+ and SERT+/− mice. There was no significant difference between males and females for any age or SERT genotype; therefore, data for both genders were pooled. SERT+/+, n = 8–11 (males n = 5 and females n = 3–6 pooled); SERT+/−, n = 5–10 (males n = 3–5 and females 2–5 pooled); and SERT−/−, n = 2–4 (males n = 1 to 2 and females n = 1 to 2 pooled) mice per group. Note that because binding in SERT−/− mice was not different from background the sample size was not further increased.
Terminal Regions.
The Bmax value for [3H]citalopram binding increased with age in CA1, CA2, and dentate gyrus [F(2,44) = 9.84, P < 0.001; F(2, 44) = 9.42, P < 0.001; F(2,44) = 7.17, P = 0.002]; however, age did not significantly influence the Bmax value for [3H]citalopram binding in CA3 [F(2,44) = 2.80, P = 0.071] (Fig. 4, A–D). As expected, the Bmax values for [3H]citalopram binding in SERT+/− mice were lower than those in SERT+/+ mice [for CA1, CA2, CA3, and dentate gyrus, respectively: F(1,44) = 182, P < 0.001; F(1,44) = 206, P < 0.001; F(1,44) = 240, P < 0.001; and F(1,44) = 132, P < 0.001]. No interactions were found between age and SERT genotype in the CA1, CA2, and CA3 regions of hippocampus or dentate gyrus [F(2,44) = 0.24, P = 0.79; F(2,44) = 0.66, P = 0.52; F(2,44) = 0.13, P = 0.88; F(2,44) = 0.56, P = 0.58]. Among-age comparisons showed the Bmax values to be smaller in P21 SERT+/+ and P28 SERT mice than in P90 SERT+/+ mice in CA2 and dentate gyrus (P < 0.01 and 0.05 for P21 and P28 mice, respectively). In CA1, the Bmax values for [3H]citalopram binding were smaller in P21 SERT+/+ and P21 SERT+/− mice than in the SERT genotype–matched P90 group (P < 0.01 and 0.05 for SERT+/+ and SERT+/− mice, respectively).
The effects of age on the Bmax value for [3H]citalopram binding in either the prefrontal cortex, parietal cortex, or ventromedial hypothalamus were not statistically significant [F(2,44) = 0.68, P = 0.51; F(2,44) = 2.858, P = 0.07; and F(2,44) = 2.16, P = 0.13, respectively] (Table 1), except that the Bmax value in the parietal cortex of SERT+/+ mice was lower in P21 than in P90 mice. The Bmax values for [3H]citalopram binding in SERT+/+ mice were higher than those for SERT+/− mice in the prefrontal cortex, parietal cortex, and ventromedial hypothalamus [F(1,44) = 154, P < 0.01; F(1,44) = 64.9, P < 0.01; and F(1,44) = 90.27, P < 0.01, respectively], and no interaction was found between age and SERT genotype [F(2,44) = 0.32, P = 0.73; F(2,44) = 0.47, P = 0.63; and F(2,44) = 0.61, P = 0.55, respectively].
The Bmax value for [3H]citalopram binding increased with age in the amygdala [F(2,44) = 5.17, P < 0.01] (Table 1). As expected, lower [3H]citalopram binding was found in amygdala of SERT+/− mice compared with SERT+/+ mice [F(1,44) = 112.7, P < 0.01]. There was no interaction between age and SERT genotype [F(2,44) = 0.97, P = 0.39]. Among-age comparisons showed the Bmax value for [3H]citalopram binding in amygdala to be lower in P28 SERT+/− mice than in P90 SERT+/− mice (P = 0.046) (Table 1). There was no effect of age or genotype on the Kd values for [3H]citalopram binding in any terminal region (data not shown, P ≥ 0.06). Values ranged from 0.6 to 1.4 nM [3H]citalopram.
Cell Body Regions.
The Bmax value for [3H]citalopram binding significantly decreased with age in the median raphe nucleus [F(2,44) = 10.3, P < 0.01] (Fig. 4F). In the dorsal raphe, a statistically nonsignificant trend showed lower Bmax values in younger mice than in older mice [F(2,44) = 2.46, P = 0.098] (Fig. 4E). In both cell body regions, higher Bmax values were observed in SERT+/+ mice than in SERT+/− mice [F(1,44) = 86.7, P < 0.01, and F(1,44) = 78.7, P < 0.01, for the median and dorsal raphe, respectively]. For both median or dorsal raphe, no interactions between SERT genotype and age were observed [F(2,44) = 0.1, P = 0.91; F(2,44) = 0.3, P = 0.74]. Among-age comparisons in the median and dorsal raphe of SERT+/+ mice showed greater Bmax values in P21 than in P90 mice (P < 0.01, P = 0.04). Similarly, greater Bmax values were found in the median raphe of P21 SERT+/− mice than in P90 SERT+/− mice (P < 0.01). There were no statistically significant effects of age or SERT genotype on Kd values for [3H]citalopram binding (data not shown, P ≥ 0.051). Values ranged from 0.54 to 0.85 nM [3H]citalopram.
Relationship between Antidepressant-like Effects of Escitalopram in the TST and [3H]Citalopram Binding in Hippocampus and Raphe Nuclei
Terminal Regions.
Figure 5, A–D shows a positive relation between the Emax values (i.e., antidepressant-like response) for escitalopram and the Bmax values for [3H]citalopram binding in hippocampal subregions as a function of age and SERT genotype. In both SERT+/+ and SERT+/− mice this positive relation can be adequately described by a straight line in each of the hippocampal regions (r ≥ 0.80–0.99, Pearson’s correlation) (Fig. 5, A–D).
Fig. 5.
Relationship between the Emax values for escitalopram to reduce immobility time in the TST and the Bmax values for specific [3H]citalopram binding in hippocampal and raphe subregions as a function of age and SERT genotype. P21, P28, and P90 mice. The CA1 (A), CA2 (B), and CA3 (C) regions of hippocampus, dentate gyrus (D), dorsal raphe (E), and median raphe (F) are shown. Data are taken from Fig. 1 (SERT+/+, n = 18–20; SERT+/−, n = 16–19) and Fig. 4 (SERT+/+, n = 8–11; SERT+/−, n = 5–10). Data are mean ± S.E.M.; male and female data were pooled.
Cell Body Regions.
Figure 5, E and F shows a negative relation between the Emax values (i.e., maximal antidepressant-like response) and the Bmax values for [3H]citalopram binding in dorsal and median raphe nuclei as a function of age and SERT genotype. In both SERT+/+ and SERT+/− mice this negative relation can be adequately described by a straight line in both the median and dorsal raphe (r ≥ 0.83–0.99, Pearson’s correlation) (Fig. 5, E and F).
Discussion
To our knowledge, we are the first to investigate the dose dependency of escitalopram’s antidepressant-like effect and its relation to SERT expression and affinity in juvenile and adolescent SERT+/+, SERT+/−, and SERT−/− mice. The Emax value for escitalopram to reduce immobility time in the TST was lower in juvenile (P21) and adolescent (P28) mice than in adults (P90) (Fig. 1F), while the potency of escitalopram was greater in younger mice than in adults (Fig. 1 E). These age-related variations in the Emax values and potency were apparent in SERT+/+ and SERT+/− mice. SERT expression, quantified by [3H]citalopram binding using autoradiography, increased with age in CA1 and CA2 regions of hippocampus, dentate gyrus, and amygdala (Fig. 4, A–D; Table 1), and decreased with age in dorsal and median raphe nuclei (Fig. 4, E and F). Age-related increases in the Emax value for escitalopram to reduce immobility time in the TST were positively related to age-related increases in the Bmax value for [3H]citalopram binding (SERT expression) in hippocampus (Fig. 5, A–D), and negatively related to SERT expression in raphe nuclei (Fig. 5, E and F). Our data further support the feasibility of using juvenile and adolescent mice to study antidepressant activity (Mitchell et al., 2013), and suggest a link between antidepressant-like activity of escitalopram and relative expression of its target, SERT.
Adolescent (P28–P35) mice respond to SSRIs in the TST and FST (Bourin et al., 1998; Mason et al., 2009) and juveniles (P21) respond to SSRIs in the TST; however, the magnitude of the effect in P21 mice was less than in adult (P90) mice (Mitchell et al., 2013). Our data in SERT+/+ mice are consistent with these findings (Fig. 1B), as well as with experiments with rats that have shown escitalopram to reduce immobility in the FST in juveniles (P21) and adolescents (P28) (Reed et al., 2008). Results from these studies parallel clinical literature suggesting SSRIs yield limited therapeutic effects in many children (Tsapakis et al., 2008; Hetrick et al., 2007, 2010).
Another population that is reported to show a limited therapeutic response to SSRIs is comprised of individuals carrying low-expressing SERT gene variants (Serretti et al., 2007). SERT+/− mice provide a model to study these gene variants (Fox et al., 2007; Homberg and Lesch, 2011). Escitalopram reduced immobility in P21, P28, and P90 SERT+/+ and SERT+/− mice (Fig. 1C), a finding consistent with previous work in adults showing that imipramine (a SERT and norepinephrine transporter blocker) and fluoxetine (an SSRI) reduced immobility time in the TST equally in SERT+/+ and SERT+/− mice (Holmes et al., 2002). SERT−/− mice did not respond to escitalopram at 10 mg/kg, a dose that is maximally effective in wild-type mice (Fig. 1D), underscoring the selective nature of escitalopram’s actions at SERT.
The ED50 value for escitalopram to reduce immobility was lower in P21 and P28 SERT+/+ and SERT+/− mice than in genotype-matched P90 mice (Fig. 1E). This observation is consistent with the finding that adolescent mice (P35) were more sensitive to the anti-immobility effects of low SSRI doses than adults in the FST (David et al., 2001). Pharmacokinetic factors could explain differences in antidepressant drug potency (Bylund and Reed, 2007); however, the elimination rate of escitalopram has yet to be determined in young mice. In contrast to the effects of age on the potency of escitalopram, the Emax values were lower in P21 SERT+/+ and SERT+/− mice than in SERT genotype–matched P90 mice (Fig. 1F), which is consistent with and expands upon previous studies in young SERT+/+ mice (Mitchell et al., 2013).
During postnatal development, 5-HT serves as a mitogen to regulate neuronal growth, dendritic pruning, and additional aspects of neurodevelopment (Migliarini et al., 2013). Expression of SERT, as a function of age, may vary by brain region to regulate extracellular 5-HT and direct, for example, neuronal growth, which is known to vary by brain region (Daval et al., 1987; Krogsrud et al., 2014; Sussman et al., 2016). However, there is a paucity of studies investigating antidepressant mechanisms in juvenile and adolescent mice. In an effort to account for age-related changes in antidepressant response, we quantified SERT expression using autoradiography (Figs. 2 and 3). SERT density increased with age in many serotonergic terminal regions, including the CA1 and CA2 regions of hippocampus, dentate gyrus, and amygdala, but did not vary with age in the CA3 region of hippocampus, cortex, or hypothalamus (Fig. 4; Table 1). These data partially diverge from a previous study, where [3H]citalopram saturation binding was used in hippocampal membrane preparations and SERT expression in P21 mice was found to be the same as that in adults (Mitchell et al., 2013). This is likely because analysis of whole hippocampal homogenates does not afford the anatomic resolution of quantitative autoradiography where hippocampal subregions can be readily discerned. The affinity values for [3H]citalopram binding in the current study (Kd: 0.54–1.4 nM) were similar to those in the previous study (Kd: 1.3–2.3 nM) (Mitchell et al., 2013).
Experiments describing SERT ontogeny in terminal regions of rat brain report peak SERT expression to occur during adolescence (∼ P35), with expression decreasing to plateau in adulthood (P70–P100) (Galineau et al., 2004; Slotkin et al., 2008; Daws and Gould, 2011). In contrast, we found either no difference in SERT expression between adolescent (P28) and adult (P90) mice (CA1, CA3, amygdala, hypothalamus, and prefrontal cortex), or lower SERT expression in adolescent mice compared with adults (CA2, dentate gyrus, and parietal cortex) (Fig. 4; Table 1). The brain regions studied possibly explain this disparity; for example, no study in rats has compared hippocampal expression of SERT across these age groups. In rats, SERT density in serotonergic cell bodies decreased from the early postnatal period to adulthood (Moll et al., 2000; Galineau et al., 2004). Our findings in dorsal and median raphe of SERT+/+ mice (Fig. 3; Fig. 4, E and F) are consistent with those in rats. One study compared mouse SERT mRNA levels in dorsal raphe and found they peaked at P14 and remained fairly constant from P17–P28 (Sidor et al., 2010). Our data show a trend toward decreased [3H]citalopram binding in raphe nuclei from P21 to P28; however, it is difficult to compare these data since mRNA levels do not always correlate with protein levels.
In adult mice, SERT expression has been quantified using autoradiography in brain (Bengel et al.., 1998; Sora et al., 2001; Montañez et al., 2003; Li et al., 2004; Perez et al., 2006). In general, these studies show that the Bmax values in SERT+/− mice are ∼50% of those in SERT+/+ mice, and SERT−/− mice show no binding beyond background levels. Our results are consistent with these reports. SERT expression in P21 and P28 SERT+/− mice revealed age-dependent changes that were similar to those in SERT+/+ mice; however, the magnitude of the changes was often smaller in SERT+/− mice (Fig. 4). The differences in the Bmax values between P21 and P90 were only observed in CA1, amygdala, and median raphe of SERT+/− mice, whereas in SERT+/+ mice, age-dependent differences were found in CA1, CA2, dentate gyrus, and dorsal and median raphe (Fig. 4). Because these regions are believed to be important for antidepressant action, these results may help to explain age-related changes in antidepressant response.
Increasing extracellular 5-HT in hippocampus produces a number of actions that are thought to be necessary for the therapeutic effects of SSRIs (Campbell and MacQueen, 2004; Dale et al.., 2016). Consistent with this, infusion of imipramine into the CA1 region of hippocampus in rats produces antidepressant-like effects in the FST (Przegaliński et al., 1997). Our data illustrate a positive relation between the Emax value for escitalopram to produce antidepressant-like effects and the Bmax value for [3H]citalopram binding in hippocampus (Fig. 5, A–D). Expression does not always indicate function; however, it is tempting to speculate that a developmental lag in hippocampal SERT expression could limit the antidepressant-like response to SSRIs.
In contrast, there was a negative relation between the Emax value for antidepressant-like response and the Bmax value for [3H]citalopram binding in raphe nuclei (Fig. 5, E and F). Greater SERT expression in the raphe of juvenile and adolescent mice than in adult mice could produce age-dependent differences in brain region–specific extracellular 5-HT concentrations after SSRI administration; however, it is unclear exactly how region-specific differences in 5-HT may limit the therapeutic effects of SSRIs. Of course, age-dependent shifts in expression and/or function of 5-HT receptors may also contribute to the limited antidepressant-like response of escitalopram in young mice and should not be overlooked (Carr and Lucki, 2011). Future studies are necessary to better understand the mechanism(s) contributing to the limited antidepressant-like response of escitalopram in young mice. Moreover, because SSRIs differ in their affinity for SERT as well as other targets (including receptors and transporters), studies examining a broader range of SSRIs may provide valuable insight into identifying antidepressants that may be more effective for the treatment of depression in juveniles.
To our knowledge, this is the first study to evaluate the ontogeny of SERT expression and antidepressant-like response in P21, P28, and P90 SERT+/+ and SERT+/− mice. Its findings help build the foundation needed to discern mechanisms underlying the limited therapeutic benefit of SSRIs in juveniles and adolescents.
Acknowledgments
The authors gratefully acknowledge the technical assistance of Melissa Vitela and Myrna Herrera-Rosales.
Abbreviations
- ANOVA
analysis of variance
- Bmax
maximal binding
- CA
cornu ammonis
- Emax
maximal effect
- FST
forced swim test
- 5-HT
serotonin
- Kd
affinity
- P
postnatal day
- SERT
serotonin transporter
- SSRI
selective serotonin reuptake inhibitor
- TST
tail suspension test
Authorship Contributions
Participated in research design: Mitchell, Gould, Koek, Daws.
Conducted experiments: Mitchell, Gould.
Performed data analysis: Mitchell.
Wrote or contributed to the writing of the manuscript: Mitchell, Gould, Koek, Daws.
Footnotes
This work was supported by the National Institutes of Health National Institute of Mental Health [Grants MH106978, MH093320, and MH086708] and the Congressionally Directed Medical Research Programs [Award AR110109].
The research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Baganz NL, Horton RE, Calderon AS, Owens WA, Munn JL, Watts LT, Koldzic-Zivanovic N, Jeske NA, Koek W, Toney GM, et al. (2008) Organic cation transporter 3: Keeping the brake on extracellular serotonin in serotonin-transporter-deficient mice. Proc Natl Acad Sci USA 105:18976–18981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengel D, Murphy DL, Andrews AM, Wichems CH, Feltner D, Heils A, Mössner R, Westphal H, Lesch KP. (1998) Altered brain serotonin homeostasis and locomotor insensitivity to 3, 4-methylenedioxymethamphetamine (“Ecstasy”) in serotonin transporter-deficient mice. Mol Pharmacol 53:649–655. [DOI] [PubMed] [Google Scholar]
- Bourin M, Colombel MC, Redrobe JP, Nizard J, Hascoët M, Baker GB. (1998) Evaluation of efficacies of different classes of antidepressants in the forced swimming test in mice at different ages. Prog Neuropsychopharmacol Biol Psychiatry 22:343–351. [DOI] [PubMed] [Google Scholar]
- Bujoreanu S, Benhayon D, Szigethy E. (2011) Treatment of depression in children and adolescents. Pediatr Ann 40:548–555. [DOI] [PubMed] [Google Scholar]
- Bylund DB, Reed AL. (2007) Childhood and adolescent depression: why do children and adults respond differently to antidepressant drugs? Neurochem Int 51:246–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell S, MacQueen G. (2004) The role of the hippocampus in the pathophysiology of major depression. J Psychiatry Neurosci 29:417–426. [PMC free article] [PubMed] [Google Scholar]
- Carr GV, Lucki I. (2011) The role of serotonin receptor subtypes in treating depression: a review of animal studies. Psychopharmacology (Berl) 213:265–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castagné V, Moser P, Roux S, Porsolt RD. (2011) Rodent models of depression: forced swim and tail suspension behavioral despair tests in rats and mice, in Curr Protoc Neurosci 55:8.10A.1–8.10A.14, John Wiley and Sons, Hoboken. [DOI] [PubMed] [Google Scholar]
- Cryan JF, Mombereau C, Vassout A. (2005) The tail suspension test as a model for assessing antidepressant activity: review of pharmacological and genetic studies in mice. Neurosci Biobehav Rev 29:571–625. [DOI] [PubMed] [Google Scholar]
- Dale E, Pehrson AL, Jeyarajah T, Li Y, Leiser SC, Smagin G, Olsen CK, Sanchez C. (2016) Effects of serotonin in the hippocampus: how SSRIs and multimodal antidepressants might regulate pyramidal cell function. CNS Spectr 21:143–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amato RJ, Largent BL, Snowman AM, Snyder SH. (1987) Selective labeling of serotonin uptake sites in rat brain by [3H]citalopram contrasted to labeling of multiple sites by [3H]imipramine. J Pharmacol Exp Ther 242:364–371. [PubMed] [Google Scholar]
- Daval G, Vergé D, Becerril A, Gozlan H, Spampinato U, Hamon M. (1987) Transient expression of 5-HT1A receptor binding sites in some areas of the rat CNS during postnatal development. Int J Dev Neurosci 5:171–180. [DOI] [PubMed] [Google Scholar]
- David DJ, Bourin M, Hascoët M, Colombel MC, Baker GB, Jolliet P. (2001) Comparison of antidepressant activity in 4- and 40-week-old male mice in the forced swimming test: involvement of 5-HT1A and 5-HT1B receptors in old mice. Psychopharmacology (Berl) 153:443–449. [DOI] [PubMed] [Google Scholar]
- Daws LC, Gould GG. (2011) Ontogeny and regulation of the serotonin transporter: providing insights into human disorders. Pharmacol Ther 131:61–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MA, Andrews AM, Wendland JR, Lesch KP, Holmes A, Murphy DL. (2007) A pharmacological analysis of mice with a targeted disruption of the serotonin transporter. Psychopharmacology (Berl) 195:147–166. [DOI] [PubMed] [Google Scholar]
- Galineau L, Kodas E, Guilloteau D, Vilar MP, Chalon S. (2004) Ontogeny of the dopamine and serotonin transporters in the rat brain: an autoradiographic study. Neurosci Lett 363:266–271. [DOI] [PubMed] [Google Scholar]
- Hetrick SE, McKenzie JE, Merry SN. (2010) The use of SSRIs in children and adolescents. Curr Opin Psychiatry 23:53–57. [DOI] [PubMed] [Google Scholar]
- Hetrick SE, Merry SN, McKenzie J, Sindahl P, Proctor M. (2007) Selective serotonin reuptake inhibitors (SSRIs) depressive disorders in children and adolescents. Cochrane Database Syst Rev, Issue 3: CD004851 1–91. [DOI] [PubMed] [Google Scholar]
- Holmes A, Yang RJ, Murphy DL, Crawley JN. (2002) Evaluation of antidepressant-related behavioral responses in mice lacking the serotonin transporter. Neuropsychopharmacology 27:914–923. [DOI] [PubMed] [Google Scholar]
- Homberg JR, Lesch KP. (2011) Looking on the bright side of serotonin transporter gene variation. Biol Psychiatry 69:513–519. [DOI] [PubMed] [Google Scholar]
- Horton RE, Apple DM, Owens WA, Baganz NL, Cano S, Mitchell NC, Vitela M, Gould GG, Koek W, Daws LC. (2013) Decynium-22 enhances SSRI-induced antidepressant-like effects in mice: uncovering novel targets to treat depression. J Neurosci 33:10534–10543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Ries Merikangas K. (2001) Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry 49:1002–1014. [DOI] [PubMed] [Google Scholar]
- Koek W, Mercer SL, Coop A, France CP. (2009) Behavioral effects of γ-hydroxybutyrate, its precursor γ-butyrolactone, and GABAB receptor agonists: time course and differential antagonism by the GABAB receptor antagonist 3-aminopropyl(diethoxymethyl)phosphinic acid (CGP35348). J Pharmacol Exp Ther 330:876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krogsrud SK, Tamnes CK, Fjell AM, Amlien I, Grydeland H, Sulutvedt U, Due-Tønnessen P, Bjørnerud A, Sølsnes AE, Håberg AK, et al. (2014) Development of hippocampal subfield volumes from 4 to 22 years. Hum Brain Mapp 35:5646–5657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Ma L, Innis RB, Seneca N, Ichise M, Huang H, Laruelle M, Murphy DL. (2004) Pharmacological and genetic characterization of two selective serotonin transporter ligands: 2-[2-(dimethylaminomethylphenylthio)]-5-fluoromethylphenylamine (AFM) and 3-amino-4-[2-(dimethylaminomethyl-phenylthio)]benzonitrile (DASB). J Pharmacol Exp Ther 308:481–486. [DOI] [PubMed] [Google Scholar]
- Loizou LA, Salt P. (1970) Regional changes in monoamines of the rat brain during postnatal development. Brain Res 20:467–470. [DOI] [PubMed] [Google Scholar]
- Mason SS, Baker KB, Davis KW, Pogorelov VM, Malbari MM, Ritter R, Wray SP, Gerhardt B, Lanthorn TH, Savelieva KV. (2009) Differential sensitivity to SSRI and tricyclic antidepressants in juvenile and adult mice of three strains. Eur J Pharmacol 602:306–315. [DOI] [PubMed] [Google Scholar]
- Migliarini S, Pacini G, Pelosi B, Lunardi G, Pasqualetti M. (2013) Lack of brain serotonin affects postnatal development and serotonergic neuronal circuitry formation. Mol Psychiatry 18:1106–1118. [DOI] [PubMed] [Google Scholar]
- Miranda-Contreras L, Mendoza-Briceño RV, Palacios-Prü EL. (1998) Levels of monoamine and amino acid neurotransmitters in the developing male mouse hypothalamus and in histotypic hypothalamic cultures. Int J Dev Neurosci 16:403–412. [DOI] [PubMed] [Google Scholar]
- Mitchell NC, Gould GG, Smolik CM, Koek W, Daws LC. (2013) Antidepressant-like drug effects in juvenile and adolescent mice in the tail suspension test: Relationship with hippocampal serotonin and norepinephrine transporter expression and function. Front Pharmacol 4:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell NC, Koek W, Daws LC. (2015) Antidepressant-like effects and basal immobility depend on age and serotonin transporter genotype. Genes Brain Behav 14:543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moll GH, Mehnert C, Wicker M, Bock N, Rothenberger A, Rüther E, Huether G. (2000) Age-associated changes in the densities of presynaptic monoamine transporters in different regions of the rat brain from early juvenile life to late adulthood. Brain Res Dev Brain Res 119:251–257. [DOI] [PubMed] [Google Scholar]
- Montañez S, Owens WA, Gould GG, Murphy DL, Daws LC. (2003) Exaggerated effect of fluvoxamine in heterozygote serotonin transporter knockout mice. J Neurochem 86:210–219. [DOI] [PubMed] [Google Scholar]
- O’Leary OF, Bechtholt AJ, Crowley JJ, Hill TE, Page ME, Lucki I. (2007) Depletion of serotonin and catecholamines block the acute behavioral response to different classes of antidepressant drugs in the mouse tail suspension test. Psychopharmacology (Berl) 192:357–371. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Franklin KBJ. (1997) The Mouse Brain in Stereotaxic Coordinates, Academic Press, San Diego, CA. [Google Scholar]
- Perez XA, Bianco LE, Andrews AM. (2006) Filtration disrupts synaptosomes during radiochemical analysis of serotonin uptake: comparison with chronoamperometry in SERT knockout mice. J Neurosci Methods 154:245–255. [DOI] [PubMed] [Google Scholar]
- Petersen IT, Bates JE, Goodnight JA, Dodge KA, Lansford JE, Pettit GS, Latendresse SJ, Dick DM. (2012) Interaction between serotonin transporter polymorphism (5-HTTLPR) and stressful life events in adolescents’ trajectories of anxious/depressed symptoms. Dev Psychol 48:1463–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Przegaliński E, Tatarczyńska E, Dereń-Wesołek A, Chojnacka-Wojcik E. (1997) Antidepressant-like effects of a partial agonist at strychnine-insensitive glycine receptors and a competitive NMDA receptor antagonist. Neuropharmacology 36:31–37. [DOI] [PubMed] [Google Scholar]
- Reed AL, Happe HK, Petty F, Bylund DB. (2008) Juvenile rats in the forced-swim test model the human response to antidepressant treatment for pediatric depression. Psychopharmacology (Berl) 197:433–441. [DOI] [PubMed] [Google Scholar]
- Ripoll N, David DJ, Dailly E, Hascoët M, Bourin M. (2003) Antidepressant-like effects in various mice strains in the tail suspension test. Behav Brain Res 143:193–200. [DOI] [PubMed] [Google Scholar]
- Serretti A, Kato M, De Ronchi D, Kinoshita T. (2007) Meta-analysis of serotonin transporter gene promoter polymorphism (5-HTTLPR) association with selective serotonin reuptake inhibitor efficacy in depressed patients. Mol Psychiatry 12:247–257. [DOI] [PubMed] [Google Scholar]
- Sidor MM, Amath A, MacQueen G, Foster JA. (2010) A developmental characterization of mesolimbocortical serotonergic gene expression changes following early immune challenge. Neuroscience 171:734–746. [DOI] [PubMed] [Google Scholar]
- Slotkin TA, Ryde IT, Levin ED, Seidler FJ. (2008) Developmental neurotoxicity of low dose diazinon exposure of neonatal rats: effects on serotonin systems in adolescence and adulthood. Brain Res Bull 75:640–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sora I, Hall FS, Andrews AM, Itokawa M, Li XF, Wei HB, Wichems C, Lesch KP, Murphy DL, Uhl GR. (2001) Molecular mechanisms of cocaine reward: combined dopamine and serotonin transporter knockouts eliminate cocaine place preference. Proc Natl Acad Sci USA 98:5300–5305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP. (2000) The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev 24:417–463. [DOI] [PubMed] [Google Scholar]
- Steru L, Chermat R, Thierry B, Simon P. (1985) The tail suspension test: a new method for screening antidepressants in mice. Psychopharmacology (Berl) 85:367–370. [DOI] [PubMed] [Google Scholar]
- Sussman D, Leung RC, Chakravarty MM, Lerch JP, Taylor MJ. (2016) Developing human brain: age-related changes in cortical, subcortical, and cerebellar anatomy. Brain Behav 6:e00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsapakis EM, Soldani F, Tondo L, Baldessarini RJ. (2008) Efficacy of antidepressants in juvenile depression: meta-analysis. Br J Psychiatry 193:10–17. [DOI] [PubMed] [Google Scholar]
- Wallace JA, Lauder JM. (1983) Development of the serotonergic system in the rat embryo: an immunocytochemical study. Brain Res Bull 10:459–479. [DOI] [PubMed] [Google Scholar]