Abstract
Background:
Idiopathic adhesive capsulitis is a common condition resulting in painful multidirectional restriction of motion without other identifiable shoulder abnormality. First-line therapies for this condition are nonoperative, but limited data are available regarding which treatments are most effective. Factors associated with contralateral disease are not well established.
Hypothesis:
Younger patients will have a better response to treatments, and older patients and patients with diabetes will be more likely to develop contralateral disease.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Patients diagnosed with idiopathic adhesive capsulitis were treated with a single intra-articular glenohumeral injection of local anesthetic and corticosteroid as well as 4 weeks of supervised physical therapy (PT). Patients were re-evaluated monthly and received additional conservative treatment based on failure to restore normal motion. Patient-reported outcome scores and range of motion were used to assess treatment efficacy.
Results:
Minimum 2-year follow-up data (mean, 3.4 years) were available for 60 of 75 eligible patients (80%). Patients who did not attend supervised PT as prescribed were more likely to undergo repeat injection due to a lack of adequate range of motion at follow-up (P = .003). Conservative therapy failed in 2 patients (3.3%), and they underwent arthroscopic release and manipulation under anesthesia. Twenty-two patients (36.7%) were subsequently diagnosed with contralateral idiopathic adhesive capsulitis, with a higher incidence in patients with diabetes (P = .009) and patients younger than 50 years (P = .005). American Shoulder and Elbow Surgeons score improved from 41.2 (95% CI, 33.0-49.4) at baseline to 92.0 (95% CI, 88.4-95.6) at final follow-up (P < .0001). Patients with diabetes had a decrease in Shoulder Activity Scale score at final follow-up (P = .049).
Conclusion:
Conservative treatment for idiopathic adhesive capsulitis resulted in good clinical outcomes with a low incidence of surgical intervention. Physical therapy reduced the use of a second injection as part of treatment in this treatment algorithm. Young patients and patients with diabetes may be more likely to develop contralateral disease.
Keywords: idiopathic adhesive capsulitis, frozen shoulder, conservative treatment, physical therapy, corticosteroid injection
Idiopathic adhesive capsulitis, also called “frozen shoulder,” is a common condition of unknown origin in which contracture of the rotator interval and capsular thickening result in shoulder pain, decreased capsular volume, and global loss of motion without other identifiable shoulder abnormality.36 The natural history of this condition has been classically described as occurring in 3 distinct clinical phases17,27: (1) painful “freezing” stage, lasting approximately 3 to 9 months, during which range of motion progressively becomes more restricted; (2) second “frozen” stage, characterized by stiffness lasting approximately 4 to 12 months; and (3) “thawing” phase, in which range of motion begins to improve, lasting between 1 and 4 years. However, because these stages exist as a continuum of disease, it is often difficult to distinguish between these phases in the clinical setting. The overall disease incidence is 3% to 5%, with a peak incidence between the ages of 35 and 65 years and a slight female predominance.14,23 Patients with diabetes are at an increased risk of developing idiopathic adhesive capsulitis and have a higher rate of nonoperative treatment failure compared with nondiabetic patients.2, 31
Although idiopathic adhesive capsulitis was traditionally thought to be a self-limited disease with a duration of approximately 2.5 years when untreated,35 recent studies have suggested that pain and motion limitation can persist for longer than 7 years. Furthermore, it is thought that up to 40% of patients may have some degree of permanent loss of motion.7,45 The greatest improvement occurs following early treatment of this condition, which can hasten resolution of symptoms sooner than if the condition is not treated.16,28,44–46 This condition is most frequently treated conservatively with a combination of anti-inflammatory medications, home exercises, physical therapy,10, 15, 36 and glenohumeral intra-articular corticosteroids.31,34,38 Operative treatment consisting of manipulation under anesthesia with or without arthroscopic capsular release may be considered if patients do not improve with nonoperative measures.42
Although idiopathic adhesive capsulitis is one of the most common conditions treated by orthopaedic surgeons, consensus is lacking regarding the optimal nonoperative treatment protocol.27 Although it is universally agreed that the first-line therapies are nonoperative, surgeons and the existing literature disagree on which conservative treatments are most effective.46 Additionally, the risk factors associated with the development of contralateral disease are not well-studied. Therefore, the purpose of this study was to report outcomes following a conservative treatment protocol for idiopathic adhesive capsulitis and to report factors associated with outcomes and the incidence of contralateral disease. We hypothesized that older patients, who experience a decrease in shoulder activity with increasing age,18 and patients with diabetes will be more likely to develop contralateral disease.
Methods
In this institutional review board–approved study, prospectively collected data were analyzed to assess outcomes in a cohort of patients being treated with a conservative treatment regimen for idiopathic adhesive capsulitis. At the clinic of a single academic sports medicine and shoulder fellowship–trained orthopaedic surgeon (R.H.B.), all new patients treated with a chief complaint of shoulder pain underwent a complete history, physical examination, and review of a standard 4-view shoulder radiographic series obtained at the initial clinic visit. A diagnosis of idiopathic adhesive capsulitis was made by physical examination demonstrating a deficit of at least 60° in total active range of motion in the affected shoulder or a deficit of at least 30° in active range of motion in 1 or more of the movements including forward flexion, abduction, external rotation, or internal rotation at 90° of shoulder abduction compared with the contralateral unaffected shoulder.4 Total active range of motion was defined as the sum of active forward flexion, abduction, external rotation, and internal rotation at 90° of shoulder abduction.4 For patients presenting with bilateral idiopathic adhesive capsulitis, range of motion was compared with age- and sex-matched normal motion in asymptomatic patients.6
Patients were included in the study if they were diagnosed with idiopathic adhesive capsulitis without a history of prior injury or surgery on the affected shoulder. Patients were excluded if they were diagnosed with any other identifiable shoulder abnormality based on history, physical examination, or imaging at the time of the initial clinic visit, at any subsequent clinic visit, or on follow-up questionnaire. Patients were also excluded if they presented in the “thawing” phase of idiopathic adhesive capsulitis,17,27 if they were non-English-speaking, or if they had prior stroke with residual upper extremity deficit, neuromuscular disorder affecting ipsilateral upper extremity, or any ipsilateral shoulder disorder other than idiopathic adhesive capsulitis. If patients had bilateral symptoms, then the more severely affected shoulder was included in the primary analysis and the less severely affected shoulder was excluded.
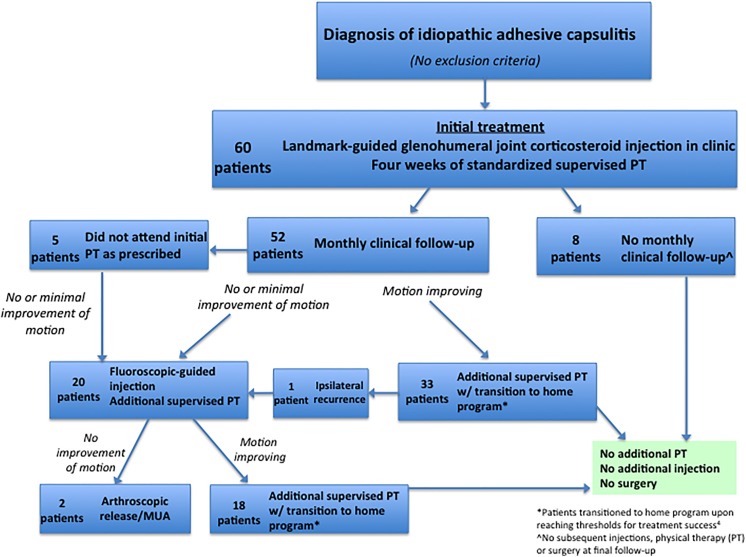
Treatment consisted of a single landmark-guided (without imaging) intra-articular injection into the glenohumeral joint of 4 mL of 1% lidocaine, 4 mL of 0.5% bupivacaine, and 80 mg of methylprednisolone acetate by the senior author (R.H.B.) in the clinic at the time of diagnosis. Patients were given a 4-week prescription for a standardized supervised physical therapy (PT) protocol for aggressive range of motion emphasizing external and internal rotation, posterior capsule stretching, rotator cuff and deltoid isometrics, and a stabilization program for rotator cuff, deltoid cuff, and scapula. No patients had received any prior injections or had undergone PT prior to the initial clinic visit when the diagnosis of idiopathic adhesive capsulitis was made. Patients were re-evaluated at monthly follow-up visits and, depending on their response to treatment, were prescribed additional supervised PT, received a second, fluoroscopically guided glenohumeral joint injection, or were converted to a home exercise program (Figure 1). Patients who had a persistent deficit of 60° or more were indicated for a second corticosteroid injection. Patients with a deficit less than 60° but more than 30° typically were offered additional supervised PT, while those with a deficit less than 30° were encouraged to transition to a home exercise program.
Figure 1.
Treatment algorithm. MUA, manipulation under anesthesia; PT, physical therapy.
All patients who received a second, fluoroscopically guided injection were prescribed additional supervised PT after the second injection. A landmark-guided injection was used initially because there is insufficient evidence to justify the increased cost and inconvenience associated with image-guided injections given the lack of clearly defined benefit in terms of increased accuracy.1,20,21,25,40,43,46 If patients do not improve after a landmark-guided injection and supervised PT, then a second, fluoroscopically guided glenohumeral joint injection followed by additional supervised PT is administered. At this point in the algorithm, a fluoroscopically guided injection is used because it is unlikely to be less accurate than a landmark-guided injection1,20,21,40,43,46 and because we believe it is important to exhaust nonoperative therapies before considering surgical intervention. If no improvement is seen after 4 to 6 months of nonoperative treatment, including 2 glenohumeral joint injections and at least 2 full courses of PT, then surgical intervention is offered.
Bilateral passive and active shoulder range of motion in forward flexion, abduction, external rotation, and internal rotation was assessed by a certified physical therapist at the initial clinic visit at the time of diagnosis and at each subsequent clinic visit, as well as at each PT session. Shoulder range of motion at the time of each follow-up clinic and PT session was compared with range of motion at the time of diagnosis. Successful treatment thresholds were defined as active and passive elevation of 160°, active and passive external rotation of 45°, and active internal rotation to T10.4 The amount of time until this range of motion was restored was calculated. Disease recurrence was defined as loss of range of motion in the ipsilateral shoulder following documented improvement as detailed above.4 Time to disease recurrence was based on the amount of time elapsed between the initial clinic visit and the follow-up visit when recurrence was diagnosed and treated. Time to diagnosis of contralateral idiopathic adhesive capsulitis was based on the amount of time elapsed between the initial clinic visit and the follow-up visit when contralateral disease was diagnosed and treated.
At minimum 2-year follow-up, all patients completed the American Shoulder and Elbow Surgeons (ASES) Shoulder Score29 and the Shoulder Activity Scale (SAS).8 The SAS is validated to reliably assess the activity of patients with shoulder disorders, allows for functional assessment of response to treatment, and has been suggested as a relevant variable for patients with idiopathic adhesive capsulitis.8,22 The ASES Standardized Shoulder Assessment Form is a valid, reliable measure of outcomes for patients with shoulder dysfunction.29 All patients also completed a supplemental questionnaire regarding recurrent symptoms, subsequent surgery on the affected shoulder, repeat injections, and the development of contralateral adhesive capsulitis. Eligible patients were mailed packets containing the ASES, SAS, and supplemental questionnaires, and if these were not completed and returned, then 2 separate attempts were made to contact each patient. If the patient declined or was unavailable for participation, he or she was considered lost to follow-up. The final analysis excluded patient-reported outcome scores for patients in whom conservative treatment failed and who underwent arthroscopic release and manipulation under anesthesia, as this study aimed to assess outcomes after a conservative treatment protocol rather than outcomes after surgical management.
Mean ASES and SAS scores at follow-up were compared with baseline by use of paired t tests. Baseline, follow-up, and changes in ASES and SAS scores were compared by age (<50 vs ≥50 years), sex, body mass index (BMI) (<30 vs ≥30), and diagnosis of diabetes mellitus, a risk factor for idiopathic adhesive capsulitis,46,48 by use of Mann-Whitney U tests. Fisher exact tests were used to compare incidence of contralateral symptoms by age, sex, BMI, and diagnosis of diabetes mellitus. Statistical significance was determined at the level of P < .05. All analysis was conducted with SPSS (IBM).
Results
Patient Demographics
A total of 75 patients were diagnosed with idiopathic adhesive capsulitis and met eligibility criteria. Nine patients (12%) refused participation, and 6 (8%) were lost to follow-up. Minimum 2-year follow-up data (mean, 3.4 years; range, 2.0-5.75 years) were collected on 60 patients (80.0%). The mean age was 52.6 years (range, 35-73 years) and mean BMI was 28.3 (range, 19.2-61.8) (Table 1).
TABLE 1.
Patient Demographic Characteristics
| No. (%) | |
|---|---|
| Sex | |
| Male | 25 (41.7) |
| Female | 35 (58.3) |
| Age | |
| <50 y | 39 (65.0) |
| ≥50 y | 21 (35.0) |
| Body mass index | |
| <30 | 39 (65.0) |
| ≥30 | 21 (35.0) |
| Diabetes status | |
| Diabetes mellitus | 9 (15.0) |
| No diabetes | 51 (85.0) |
Nine of the 60 patients (15.0%) had a diagnosis of diabetes mellitus at initial presentation, 8 of these (88.9%) with type 1 diabetes. The mean age of patients with diabetes was 49.6 years (range, 35-73 years) compared with 53.1 years (range, 40-72 years) for nondiabetic patients (P = .15). Overall, the mean duration of shoulder pain prior to presentation was 5.3 months (95% CI, 4.3-6.3 months). Three patients (5.0%), all female, were diagnosed with bilateral idiopathic adhesive capsulitis at the initial clinic visit. There was a trend toward patients with diabetes being more likely to have bilateral symptoms at initial presentation compared with patients without diabetes (22.2% vs 1.9%; P = .056).
Glenohumeral Joint Injections
All 60 patients (100%) underwent a landmark-guided glenohumeral joint injection at the initial clinic visit when the diagnosis was established. Twenty patients (33.3%) received a second glenohumeral joint injection under fluoroscopic guidance. Every patient who did not attend supervised PT as prescribed at the time of initial diagnosis returned to the office with persistent deficits in shoulder range of motion and received a fluoroscopically guided glenohumeral joint injection. Patients who did not attend supervised PT as initially prescribed were more likely to undergo repeat glenohumeral joint injection than those who completed the prescribed PT (100% vs 27.3%; P = .003). Fluoroscopically guided injections were performed at a mean of 57.4 days (95% CI, 46.9-67.8 days) after the first landmark-guided glenohumeral joint injection. No patients received a third glenohumeral joint injection. No significant difference was noted in the incidence or timing of a second glenohumeral joint injection based on age (<50 vs ≥50 years), sex, BMI (<30 vs ≥30), or diagnosis of diabetes mellitus (Table 2). There was a nonsignificant trend toward patients with diabetes being more likely to receive a second injection (55.6% vs 29.4%; P = .15).
TABLE 2.
Characteristics of Patients Undergoing Second Glenohumeral Joint Injectiona
| % | P Value | |
|---|---|---|
| Male | 36.0 | .78 |
| Female | 31.4 | |
| Age <50 y | 33.3 | ≥.999 |
| Age ≥50 y | 33.3 | |
| Body mass index <30 | 28.2 | .27 |
| Body mass index ≥30 | 42.9 | |
| Diabetes mellitus | 55.6 | .15 |
| No diabetes | 29.4 | |
| Attended physical therapy | 27.3 | .003 |
| Did not attend physical therapy | 100 |
aPercentages are based on the entire sample of 60 patients. Of this sample, 20 (33.3%) patients underwent a second glenohumeral joint injection. Bolded value indicates statistical significance (P < .05).
Treatment Failure and Recurrence
Conservative therapies, including supervised PT and 2 intra-articular corticosteroid injections (the first landmark guided and the second fluoroscopically guided) failed in 2 patients (3.3%); these patients underwent arthroscopic capsular release and manipulation under anesthesia at 6.5 and 12.6 months after diagnosis, respectively, without symptom recurrence at final follow-up. These patients were both nondiabetic females 50 years or older with BMI less than 30. One of them developed contralateral symptoms that responded to conservative treatment. No additional patients underwent surgical intervention.
Only 1 patient had ipsilateral recurrence after meeting the threshold for successful treatment.4 This patient met the threshold for successful treatment at 38 days after the initial injection; then she had a second injection after recurrence and met the threshold for successful treatment again, at 33 days after the second injection. She had no subsequent injections or surgery.
Range of Motion
Forty-nine patients (81.7%) met range of motion thresholds for successful treatment,4 regaining motion at a mean of 76.6 days (95% CI, 59.9-93.4 days) after initial diagnosis and glenohumeral joint injection. Nine patients (15.0%) did not have follow-up range of motion data, but none of these patients underwent subsequent injections, PT, or surgery or saw another physician for shoulder pain following initial diagnosis and treatment.
Patient-Reported Outcomes
Patients with available baseline ASES and SAS scores were similar to those providing final follow-up with respect to sex, age, BMI, and diabetes status. A difference was found in baseline ASES scores in male compared with female patients (95% CI, 44.5-58.7 vs 24.5-45.5; P = .017) (Table 3). No significant differences were found in baseline ASES scores based on age (<50 vs ≥50 years), BMI (<30 vs ≥30), or diagnosis of diabetes mellitus.
TABLE 3.
American Shoulder and Elbow Surgeons (ASES) Scores
| ASES Score, mean ± 95% CI | P Value | |
|---|---|---|
| At baseline | ||
| Overall cohort | 41.2 ± 8.2 | |
| Male | 51.6 ± 7.1 | .017 |
| Female | 31.5 ± 7.0 | |
| Age <50 y | 37.6 ± 8.6 | .40 |
| Age ≥50 y | 43.2 ± 8.1 | |
| Body mass index <30 | 43.2 ± 9.1 | .57 |
| Body mass index ≥30 | 38.6 ± 7.2 | |
| Diabetes mellitus | 33.3 ± 8.4 | .44 |
| No diabetes | 42.7 ± 8.2 | |
| At follow-up | ||
| Overall cohort | 92.0 ± 3.6 | |
| Male | 95.4 ± 1.7 | .25 |
| Female | 89.5 ± 4.5 | |
| Age <50 y | 87.2 ± 4.1 | .006 |
| Age ≥50 y | 94.8 ± 3.2 | |
| Body mass index <30 | 93.9 ± 2.9 | .19 |
| Body mass index ≥30 | 88.7 ± 4.6 | |
| Diabetes mellitus | 85.1 ± 3.8 | .06 |
| No diabetes | 93.3 ± 3.5 | |
The ASES score at final follow-up was higher compared with baseline (95% CI, 88.4-95.6 vs 33.0-49.4; P < .0001). We noted a higher final ASES score in patients 50 years or older compared with those younger than 50 years (95% CI, 91.6-98.0 vs 83.1-91.3; P = .006). A trend was noted toward lower final ASES scores among patients with diabetes (95% CI, 81.3-88.9 vs 89.8-96.8; P = .06). The mean ASES score at final follow-up for patients who did not have follow-up range of motion data to assess for treatment success4 was similar to the mean score for patients who did meet range of motion thresholds for treatment success (95% CI, 90.0-95.2 vs 88.0-95.7; P ≥ .999).
The mean baseline SAS score was 10.7 (95% CI, 9.6-11.8). No significant differences were found in baseline SAS score based on age, sex, BMI, or diagnosis of diabetes mellitus. At final follow-up, the SAS score was higher among male compared with female patients (95% CI, 10.8-12.6 vs 6.4-8.4; P < .0001) (Table 4). The mean SAS score at final follow-up for patients who did not have follow-up range of motion data to assess for treatment success4 was similar to the mean score for patients who did meet did meet range of motion thresholds for treatment success (95% CI, 8.2-10.7 vs 7.8-10.1; P = .92). No significant difference was found between pre- and posttreatment SAS score overall or according to sex, age, BMI, or diagnosis of diabetes mellitus.
TABLE 4.
Shoulder Activity Scale (SAS) Scores
| SAS Score, mean ± 95% CI | P Value | |
|---|---|---|
| At baseline | ||
| Overall cohort | 10.7 ± 1.1 | |
| Male | 11.9 ± 1.0 | .19 |
| Female | 9.5 ± 1.1 | |
| Age <50 y | 9.6 ± 1.1 | .37 |
| Age ≥50 y | 11.3 ± 1.1 | |
| Body mass index <30 | 11.8 ± 1.3 | .18 |
| Body mass index ≥30 | 9.3 ± 0.7 | |
| Diabetes mellitus | 11.5 ± 1.0 | .84 |
| No diabetes | 10.5 ± 1.1 | |
| At follow-up | ||
| Overall cohort | 9.2 ± 1.1 | |
| Male | 11.7 ± 0.9 | <.0001 |
| Female | 7.4 ± 1.0 | |
| Age <50 y | 9.3 ± 1.1 | .87 |
| Age ≥50 y | 9.2 ± 1.1 | |
| Body mass index <30 | 9.8 ± 1.1 | .11 |
| Body mass index ≥30 | 8.3 ± 1.2 | |
| Diabetes mellitus | 8.6 ± 1.4 | .44 |
| No diabetes | 9.3 ± 1.1 | |
Contralateral Adhesive Capsulitis
Twenty-two patients (36.7%) were subsequently diagnosed with idiopathic adhesive capsulitis in the contralateral shoulder, with a higher incidence in patients with diabetes (77.8% vs 29.4%; P = .009) and in patients younger than 50 years (61.9% vs 23.1%; P = .005). Patients with contralateral disease presented at a mean time of 2.0 years (range, 0-5.0 years; 95% CI, 1.2-2.8 years) following their initial diagnosis.
Discussion
This study of a conservative treatment protocol for idiopathic adhesive capsulitis demonstrated clinically significant improvements, a low rate of treatment failure warranting surgical intervention, a low rate of ipsilateral recurrence, and a moderate rate of contralateral disease. Contralateral disease was more likely in patients with diabetes and those younger than 50 years. Patients had clinically significant improvements in ASES scores, with higher ASES scores in patients 50 years and older. Patients who did not attend supervised PT after initial diagnosis were more likely to receive a second glenohumeral joint corticosteroid injection.
This treatment protocol resulted in a low rate of treatment failure requiring operative intervention (3.3%) when compared with previously reported rates in the literature, which range from 7% to 28%.15,26,36 Before considering surgical intervention, we advocate an exhaustive trial of conservative treatment as outlined by our treatment algorithm. Substantially higher rates of conservative treatment failure warranting operative intervention than those reported in the present study may indicate overtreatment of this condition. As such, surgeons considering operative intervention must be sure to have exhausted nonoperative treatment options. Higher rates of contralateral disease in patients younger than 50 years and in patients with diabetes have not been previously described, although diabetes has been associated with a higher overall risk of developing this disorder.46,48 Why patients who develop this disorder before the age of 50 have a higher risk for contralateral disease deserves further study. A higher incidence of subsequent corticosteroid injections among patients who did not attend supervised PT suggests that therapy is an important aspect of the treatment protocol.
In a previous study, we demonstrated that patients with idiopathic adhesive capsulitis have similar shoulder activity levels compared with age- and sex-matched controls without shoulder problems.22 In the present study, conservative treatment was not associated with a decrease in activity level among most patients, suggesting that most were able to return to the activity level that they had prior to developing adhesive capsulitis. We anticipated that idiopathic adhesive capsulitis would be more likely to develop in less active patients. Our hypothesis that older patients would be more likely to develop contralateral idiopathic adhesive capsulitis was largely based on a previous study demonstrating a decrease in shoulder activity level with increasing age18; however, that study evaluated healthy controls rather than patients with idiopathic adhesive capsulitis. According to our previous study, which used the same cohort of patients as the present study, older male patients with this condition had higher shoulder activity levels compared with younger patients and female patients.22 In the present study, we found that older patients were less likely to develop contralateral idiopathic adhesive capsulitis. As such, it is possible that patients with higher shoulder activity levels are also less likely to develop this condition in the contralateral shoulder. However, further study is needed to better assess the association between shoulder activity level and the development of this disorder.
Several studies have reported outcomes following various nonoperative therapies for adhesive capsulitis. Although intra-articular corticosteroid injections are frequently used, results following these injections have been mixed.46 Two randomized controlled trials (RCTs) demonstrated no significant benefit in favor of corticosteroid injections alone compared with PT alone.3,13 However, the majority of studies have suggested a short- to mid-term benefit in terms of pain reduction and improved range of motion in patients after corticosteroid injection compared with various control groups, including those undergoing just PT or home exercises.‡ Two RCTs demonstrated that adding an intra-articular corticosteroid injection to PT leads to better outcomes than PT alone.12,38 Most studies have described a clinically significant positive effect in pain relief, motion, and patient-reported outcomes between 2 and 24 weeks following injection compared with other nonoperative therapies.46 The injection may relieve pain in the short to mid term while also facilitating less painful PT sessions to help expediently restore a functional range of motion.
Our findings suggest that PT is an important component of a conservative treatment protocol, as PT decreased the likelihood of receiving a second injection from 100% to 27.3%. We emphasize the importance of supervised PT to patients, as the exercises in the protocol can be difficult for them to perform on their own as part of a home program. In particular, we have found that passive range of motion exercises and posterior capsular stretching are best initially performed under the guidance of a licensed physical therapist. Furthermore, in our experience, supervised PT improves patient compliance compared with a home program without any supervised PT. After patients have achieved successful treatment thresholds,4 they are transitioned to a home therapy program as part of our treatment protocol. However, aside from a significant difference in the number of second glenohumeral joint injections, no significant differences were found in patient-reported outcomes comparing those who did and did not initially attend supervised PT as prescribed.
Several studies have examined the accuracy of landmark-guided injections and image-guided injections within the glenohumeral joint, reporting a relatively wide range of accuracy for both types. Landmark-guided injections have a reported accuracy of 45% to 98%,20,21,40,43 while image-guided injections have a reported accuracy of 63% to 100%.1,46 Interestingly, multiple studies have reported an accuracy of greater than 90% for landmark-guided injections alone.20,21,40 Only 1 study investigated the efficacy of ultrasound- versus landmark-guided injections for adhesive capsulitis, demonstrating improved pain relief and range of motion only within the first 2 weeks following ultrasound-guided injection, after which no significant differences were noted in any outcome measures.25 Furthermore, studies have demonstrated no difference in pain or range of motion when comparing intra-articular and subacromial injections, suggesting that landmark-guided injections that miss the glenohumeral joint may still be effective.32,37,41 Currently, insufficient evidence is available to justify the increased cost associated with image-guided injections for the initial treatment of idiopathic adhesive capsulitis, considering the lack of apparent benefit in terms of increased accuracy.46
This study has several limitations. First, this was a single-center, single-surgeon study at an academic medical center, and thus the results may not be generalizable to all patient populations. Idiopathic adhesive capsulitis was diagnosed clinically based on history, physical examination, and normal shoulder radiographs. Although distinct stages of idiopathic adhesive capsulitis have been described, the definition of this condition, including the number of stages, descriptions of each stage, and the duration of each stage, varies among reports.17,27,30,49 As the clinical presentation of these stages can overlap, we did not believe that we could accurately distinguish between the “freezing” and “frozen” stages of idiopathic adhesive capsulitis and therefore did not specifically assess how each stage of disease related to treatment outcomes. Further study is required to determine how the various stages of disease respond to this treatment protocol.
Also, because no single, widely accepted definition of idiopathic adhesive capsulitis is available, we used the best available definition as previously described in a level 1 study.4 Although a standardized PT protocol was prescribed, supervised PT was not performed at a single institution by a single therapist but rather was provided by a certified physical therapist at a location of the patient’s choosing, which reflects clinical reality and makes the findings more generalizable. This study did not include a control group, and all patients were treated with the same protocol. A subset of patients did not return for final range of motion assessment, and therefore we could not assess motion thresholds for treatment success4 in these patients. However, no differences were noted in patient-reported outcome scores, and none of these patients underwent subsequent PT or surgery, received subsequent injections, reported symptom recurrence, or saw another provider for shoulder pain. Finally, the study may have been underpowered to demonstrate significant associations of ASES and SAS scores with certain demographic and patient-specific risk factors, and no previous study has established minimal clinically important differences for ASES and SAS scores in this disease process.
Conclusion
At a minimum 2-year follow-up, patients with idiopathic adhesive capsulitis treated conservatively with 1 or more intra-articular glenohumeral joint corticosteroid injections and supervised PT demonstrated clinically significant improvements in shoulder range of motion, pain, and function; a low rate of conservative treatment failure warranting surgical intervention; a low incidence of ipsilateral recurrence; and a moderate rate of contralateral disease. Patients who did not initially attend supervised PT were more likely to receive a second intra-articular injection, suggesting that PT has an important role in the treatment of adhesive capsulitis. Finally, patients with diabetes and younger patients may be more likely to develop contralateral idiopathic adhesive capsulitis.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: R.H.B. is a paid speaker/presenter for Arthrex and Smith & Nephew and is a consultant for Sanofi, Zimmer, and ISTO Technologies.
Ethical approval for this study was obtained from the Washington University in St Louis Institutional Review Board (ID: 201601087).
References
- 1. Aly AR, Rajasekaran S, Ashworth N. Ultrasound-guided shoulder girdle injections are more accurate and more effective than landmark-guided injections: a systematic review and meta-analysis. Br J Sports Med. 2015;49(16):1042–1049. [DOI] [PubMed] [Google Scholar]
- 2. Arkkila PE, Kantola IM, Viikari JS, Ronnemaa T. Shoulder capsulitis in type I and II diabetic patients: association with diabetic complications and related diseases. Ann Rheum Dis. 1996;55(12):907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Arslan S, Celiker R. Comparison of the efficacy of local corticosteroid injection and physical therapy for the treatment of adhesive capsulitis. Rheumatol Int. 2001;21(1):20–23. [DOI] [PubMed] [Google Scholar]
- 4. Badalamente MA, Wang ED. CORR® ORS Richard A. Brand Award: clinical trials of a new treatment method for adhesive capsulitis. Clin Orthop Relat Res. 2016;474(11):2327–2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bal A, Eksioglu E, Gulec B, Aydog E, Gurcay E, Cakci A. Effectiveness of corticosteroid injection in adhesive capsulitis. Clin Rehabil. 2008;22(6):503–512. [DOI] [PubMed] [Google Scholar]
- 6. Barnes CJ, Van Steyn SJ, Fischer RA. The effects of age, sex, and shoulder dominance on range of motion of the shoulder. J Shoulder Elbow Surg. 2001;10(3):242–246. [DOI] [PubMed] [Google Scholar]
- 7. Binder AI, Bulgen DY, Hazleman BL, Roberts S. Frozen shoulder: a long-term prospective study. Ann Rheum Dis. 1984;43(3):361–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brophy RH, Beauvais RL, Jones EC, Cordasco FA, Marx RG. Measurement of shoulder activity level. Clin Orthop Relat Res. 2005;439:101–108. [DOI] [PubMed] [Google Scholar]
- 9. Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S. Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis. 1984;43(3):353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bunker TD, Anthony PP. The pathology of frozen shoulder: a Dupuytren-like disease. J Bone Joint Surg Br. 1995;77(5):677–683. [PubMed] [Google Scholar]
- 11. Calis M, Demir H, Ulker S, Kirnap M, Duygulu F, Calis HT. Is intraarticular sodium hyaluronate injection an alternative treatment in patients with adhesive capsulitis? Rheumatol Int. 2006;26(6):536–540. [DOI] [PubMed] [Google Scholar]
- 12. Carette S, Moffet H, Tardif J, et al. Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum. 2003;48(3):829–838. [DOI] [PubMed] [Google Scholar]
- 13. Dacre JE, Beeney N, Scott DL. Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis. 1989;48(4):322–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ewald A. Adhesive capsulitis: a review. Am Fam Physician. 2011;83(4):417–422. [PubMed] [Google Scholar]
- 15. Griggs SM, Ahn A, Green A. Idiopathic adhesive capsulitis: a prospective functional outcome study of nonoperative treatment. J Bone Joint Surg Am. 2000;82-A(10):1398–1407. [PubMed] [Google Scholar]
- 16. Hand GC, Athanasou NA, Matthews T, Carr AJ. The pathology of frozen shoulder. J Bone Joint Surg Br. 2007;89(7):928–932. [DOI] [PubMed] [Google Scholar]
- 17. Hazleman BL. Frozen shoulder In: Rockwood CA, Jr, Matsen FA, III, eds. The Shoulder. Vol 2 Philadelphia, PA: WB Saunders; 1990:623–677. [Google Scholar]
- 18. Hepper CT, Smith MV, Steger-May K, Brophy RH. Normative data of shoulder activity level by age and sex. Am J Sports Med. 2013;41(5):1146–1151. [DOI] [PubMed] [Google Scholar]
- 19. Hong JY, Yoon SH, Moon DJ, Kwack KS, Joen B, Lee HY. Comparison of high- and low-dose corticosteroid in subacromial injection for periarticular shoulder disorder: a randomized, triple-blind, placebo-controlled trial. Arch Phys Med Rehabil. 2011;92(12):1951–1960. [DOI] [PubMed] [Google Scholar]
- 20. Jo CH, Shin YH, Shin JS. Accuracy of intra-articular injection of the glenohumeral joint: a modified anterior approach. Arthroscopy. 2011;27(10):1329–1334. [DOI] [PubMed] [Google Scholar]
- 21. Johnson TS, Mesfin A, Farmer KW, et al. Accuracy of intra-articular glenohumeral injections: the anterosuperior technique with arthroscopic documentation. Arthroscopy. 2011;27(6):745–749. [DOI] [PubMed] [Google Scholar]
- 22. Lamplot JD, Lillegraven O, Brophy RH. Shoulder activity level in patients with idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2017;26(9):1514–1519. [DOI] [PubMed] [Google Scholar]
- 23. Le Lievre HM, Murrell GA. Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. J Bone Joint Surg Am. 2012;94(13):1208–1216. [DOI] [PubMed] [Google Scholar]
- 24. Lebrun CM. Ultrasound-guided corticosteroid injections for adhesive capsulitis more effective than placebo. Evid Based Med. 2016;21(2):71. [DOI] [PubMed] [Google Scholar]
- 25. Lee HJ, Lim KB, Kim DY, Lee KT. Randomized controlled trial for efficacy of intra-articular injection for adhesive capsulitis: ultrasonography-guided versus blind technique. Arch Phys Med Rehabil. 2009;90(12):1997–2002. [DOI] [PubMed] [Google Scholar]
- 26. Levine WN, Kashyap CP, Bak SF, Ahmad CS, Blaine TA, Bigliani LU. Nonoperative management of idiopathic adhesive capsulitis. J Shoulder Elbow Surg. 2007;16(5):569–573. [DOI] [PubMed] [Google Scholar]
- 27. Manske RC, Prohaska D. Diagnosis and management of adhesive capsulitis. Curr Rev Musculoskelet Med. 2008;1(3-4):180–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Marx RG, Malizia RW, Kenter K, Wickiewicz TL, Hannafin JA. Intra-articular corticosteroid injection for the treatment of idiopathic adhesive capsulitis of the shoulder. HSS J. 2007;3(2):202–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. [DOI] [PubMed] [Google Scholar]
- 30. Neviaser AS, Neviaser RJ. Adhesive capsulitis of the shoulder. J Am Acad Orthop Surg. 2011;19(9):536–542. [DOI] [PubMed] [Google Scholar]
- 31. Ogilvie-Harris DJ, Biggs DJ, Fitsialos DP, MacKay M. The resistant frozen shoulder: manipulation versus arthroscopic release. Clin Orthop Relat Res. 1995;319:238–248. [PubMed] [Google Scholar]
- 32. Oh JH, Oh CH, Choi JA, Kim SH, Kim JH, Yoon JP. Comparison of glenohumeral and subacromial steroid injection in primary frozen shoulder: a prospective, randomized short-term comparison study. J Shoulder Elbow Surg. 2011;20(7):1034–1040. [DOI] [PubMed] [Google Scholar]
- 33. Prestgaard T, Wormgoor ME, Haugen S, Harstad H, Mowinckel P, Brox JI. Ultrasound-guided intra-articular and rotator interval corticosteroid injections in adhesive capsulitis of the shoulder: a double-blind, sham-controlled randomized study. Pain. 2015;156(9):1683–1691. [DOI] [PubMed] [Google Scholar]
- 34. Ranalletta M, Rossi LA, Zaidenberg EE, et al. Midterm outcomes after arthroscopic anteroinferior capsular release for the treatment of idiopathic adhesive capsulitis. Arthroscopy. 2017;33(3):503–508. [DOI] [PubMed] [Google Scholar]
- 35. Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4(4):193–196. [DOI] [PubMed] [Google Scholar]
- 36. Rill BK, Fleckenstein CM, Levy MS, Nagesh V, Hasan SS. Predictors of outcome after nonoperative and operative treatment of adhesive capsulitis. Am J Sports Med. 2011;39(3):567–574. [DOI] [PubMed] [Google Scholar]
- 37. Rizk TE, Pinals RS, Talaiver AS. Corticosteroid injections in adhesive capsulitis: investigation of their value and site. Arch Phys Med Rehabil. 1991;72(1):20–22. [PubMed] [Google Scholar]
- 38. Ryans I, Montgomery A, Galway R, Kernohan WG, McKane R. A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology (Oxford). 2005;44(4):529–535. [DOI] [PubMed] [Google Scholar]
- 39. Shin SJ, Lee SY. Efficacies of corticosteroid injection at different sites of the shoulder for the treatment of adhesive capsulitis. J Shoulder Elbow Surg. 2013;22(4):521–527. [DOI] [PubMed] [Google Scholar]
- 40. Sidon E, Velkes S, Shemesh S, Levy J, Glaser E, Kosashvili Y. Accuracy of non assisted glenohumeral joint injection in the office setting. Eur J Radiol. 2013;82(12):e829–e831. [DOI] [PubMed] [Google Scholar]
- 41. Song A, Higgins LD, Newman J, Jain NB. Glenohumeral corticosteroid injections in adhesive capsulitis: a systematic search and review. PM R. 2014;6(12):1143–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tasto JP, Elias DW. Adhesive capsulitis. Sports Med Arthrosc. 2007;15(4):216–221. [DOI] [PubMed] [Google Scholar]
- 43. Tobola A, Cook C, Cassas KJ, et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. J Shoulder Elbow Surg. 2011;20(7):1147–1154. [DOI] [PubMed] [Google Scholar]
- 44. Vastamaki H, Kettunen J, Vastamaki M. The natural history of idiopathic frozen shoulder: a 2- to 27-year followup study. Clin Orthop Relat Res. 2012;470(4):1133–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wong CK, Levine WN, Deo K, et al. Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy. 2017;103(1):40–47. [DOI] [PubMed] [Google Scholar]
- 46. Xiao RC, Walley KC, DeAngelis JP, Ramappa AJ. Corticosteroid injections for adhesive capsulitis: a review. Clin J Sport Med. 2017;27(3):308–320. [DOI] [PubMed] [Google Scholar]
- 47. Yoon SH, Lee HY, Lee HJ, Kwack KS. Optimal dose of intra-articular corticosteroids for adhesive capsulitis: a randomized, triple-blind, placebo-controlled trial. Am J Sports Med. 2013;41(5):1133–1139. [DOI] [PubMed] [Google Scholar]
- 48. Zreik NH, Malik RA, Charalambous CP. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6(1):26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zuckerman JD, Rokito A. Frozen shoulder: a consensus definition. J Shoulder Elbow Surg. 2011;20(2):322–325. [DOI] [PubMed] [Google Scholar]