Abstract
Background
Practitioners who enhance how they express empathy and create positive expectations of benefit could improve patient outcomes. However, the evidence in this area has not been recently synthesised.
Objective
To estimate the effects of empathy and expectations interventions for any clinical condition.
Design
Systematic review and meta-analysis of randomised trials.
Data sources
Six databases from inception to August 2017.
Study selection
Randomised trials of empathy or expectations interventions in any clinical setting with patients aged 12 years or older.
Review methods
Two reviewers independently screened citations, extracted data, assessed risk of bias and graded quality of evidence using GRADE. Random effects model was used for meta-analysis.
Results
We identified 28 eligible (n = 6017). In seven trials, empathic consultations improved pain, anxiety and satisfaction by a small amount (standardised mean difference −0.18 [95% confidence interval −0.32 to −0.03]). Twenty-two trials tested the effects of positive expectations. Eighteen of these (n = 2014) reported psychological outcomes (mostly pain) and showed a modest benefit (standardised mean difference −0.43 [95% confidence interval −0.65 to −0.21]); 11 (n = 1790) reported physical outcomes (including bronchial function/ length of hospital stay) and showed a small benefit (standardised mean difference −0.18 [95% confidence interval −0.32 to −0.05]). Within 11 trials (n = 2706) assessing harms, there was no evidence of adverse effects (odds ratio 1.04; 95% confidence interval 0.67 to 1.63). The risk of bias was low. The main limitations were difficulties in blinding and high heterogeneity for some comparisons.
Conclusions
Greater practitioner empathy or communication of positive messages can have small patient benefits for a range of clinical conditions, especially pain.
Protocol registration
Cochrane Database of Systematic Reviews (protocol) DOI: 10.1002/14651858.CD011934.pub2.
Keywords: Communication, family medicine, evidence-based practice
Introduction
Communication between patients and practitioners lies at the heart of healthcare. It can enhance diagnostic accuracy,1 promote patient-centred treatment decisions2 and improve a number of clinical outcomes ranging from treatment adherence3 to safety.4 Good communication can also lower the risk of malpractice claims.5
Much of the recent research in this area has focused on whether empathic and positive communication are beneficial,6,7 and whether empathic communication can be taught (it seems that it can).8 A 2001 systematic review found that empathy and positive communication might also improve patient outcomes.9 However, the evidence has moved on significantly, with numerous randomised trials having been published since,10–29 not all of them with positive findings.28,30 A more recent attempt at synthesising the evidence focused exclusively on pain.31 However, communication interventions are likely to have more general effects across a range of conditions, so it is desirable to evaluate their effect upon multiple outcomes in the context of the same review.32
In this systematic review and meta-analysis, we aimed to combine data from all available randomised trials of empathy interventions (where practitioners deliver enhanced empathy) or expectations interventions (where practitioners deliver positive messages to promote positive patient expectations about outcomes) on patient health for any condition.
Methods
Data sources and searches
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines33 and searched the following databases from inception to 10 August 2017: MEDLINE, CENTRAL, EMBASE, PsychINFO, CINAHL, ProQuest. The full search strategy is further detailed within eMethods and eTable 1 in the Supplement.
Study selection
Randomised trials (including cluster randomised trials) in any disease area were eligible for inclusion. We included trials in which patients aged 12 years or older were involved in a face-to-face interaction with a healthcare practitioner (such as a physician, nurse or allied health professional).
Eligible studies fell into two categories. First, those that randomised participants to enhanced practitioner empathy (‘empathy interventions’) or usual care (see eMethods in the Supplement). Empathy intervention trials were those in which empathy was explicitly manipulated. Within the healthcare setting, empathy is taken to involve shared understanding, and making a therapeutically helpful suggestion based on that shared understanding.34 Second, those that randomised participants to enhanced positive messages aimed at promoting positive patient expectations about recovery (‘expectation interventions’) or usual care. We combined these two types of trials because patients consider appropriately positive messages to be part of empathy34 and because previous reviews in this area have done so.9,31 To minimise risk of bias, we excluded quasi-randomised trials or observational studies, and studies at high risk of bias for random sequence generation.35
We excluded studies in which the intervention was negative. These were trials in which a practitioner would deliver a negative message or reduce their empathy. This is because these studies are not clinically relevant and experimental: one would not encourage a clinician to intentionally give unempathic or negative consultations.
Data extraction and risk of bias assessment
Two researchers (from JH, AM, ED, XYH) independently screened titles and abstracts. Full-text articles were then reviewed in duplicate and disagreements resolved by discussion with a third reviewer. We extracted data about: details of study design, types of participants, description of intervention, description of comparison group, completeness of outcome data, outcome measures, setting, country and funding source. If not reported, study authors were contacted. We assessed the risk of bias based on the Cochrane criteria (see Supplement).
We classified studies as being at a high risk of bias overall if they were scored as at high or unclear risk of bias for either sequence generation or allocation concealment domains, based on growing empirical evidence that these factors are particularly important potential sources of bias (see eMethods in the Supplement for details).35 To evaluate the overall quality of evidence, we used the GRADE system for all three primary outcomes,36 using GRADEpro software to prepare the Summary of Findings tables.37
Outcomes
Primary outcomes were physical or psychological, or harms. When studies reported more than one physical or psychological outcome or harm, we chose the one that the study authors reported as primary, or the outcome for which a sample size calculation was made. If the primary outcome was unclear and there was no sample size calculation, we selected the outcome judged by two independent clinicians (GL and AM) to be most clinically relevant. For example, we deemed longer-term follow-up (weeks or months) to be more clinically relevant for chronic pain. Because empathy and expectations interventions could have global effects, we also collected data on patient satisfaction, quality of life and cost-effectiveness as secondary outcomes.
Pain outcomes were challenging to classify because they can be categorised as both physical and psychological.38 Hence, we conducted subgroup analyses with pain studies. Because the measures of pain in this review were mostly subjective patient reports, we classified pain as psychological in our main analysis.
Data synthesis and analysis
Due to the nature of these types of behavioural interventions,39 we anticipated a degree of heterogeneity of populations, interventions and effect sizes. We pooled results that were sufficiently similar in terms of intervention content using a random effects analysis (see eMethods in the Supplement).35 Except for harms (where all outcomes were dichotomous), we converted odds ratios to standardised mean differences.40 To estimate harms, we analysed data based on the number of events and the number of people assessed in the intervention and comparison groups, then calculated odds ratios and 95% confidence intervals. We conducted analysis on an intention-to-treat basis wherever possible. Otherwise, we analysed data as reported. To assess the degree of variation between studies, we did heterogeneity tests with Higgins’ I2 statistic.35 Where heterogeneity was present in pooled effect estimates, we explored possible reasons for variability by conducting subgroup and sensitivity analyses.
When three or more trials investigated the effects of modifying practitioner empathy and/or inducing positive patient expectations upon a particular condition or clinically relevant outcome, we analysed these trials in separate subgroups. This was in order to identify any condition-specific effects of empathy and expectations.
We conducted two sensitivity analyses. In the first, we excluded studies with high risk of bias; in the second, we excluded studies where assumptions about data had to be made because of missing data, for example, the imputation of missing standard deviation values for continuous data.
Results
We identified 26,902 non-duplicate citations from our searches (eFigure 1 in the Supplement). Of these, 29 studies were eligible for inclusion in this review (Table 1, eTable 2 in the Supplement).10–30,41–46
Table 1.
Characteristics of included studies.
| Study | Year | Country | No. patients | Interventions | Condition being treated | Timing of outcome assessment | Main reported psychological and physical outcomes and adverse events (and assessment tools) |
|---|---|---|---|---|---|---|---|
| Empathy | |||||||
| Chassany11 | 2006 | France | 818 | Intervention delivered by empathy-trained doctor vs. consultation delivered by untrained doctor | Osteoarthritis of knee or hip) | Over two weeks | Physical: n/a Psychological: pain (area under curve, based on 100mm VAS*) Adverse events: any reported |
| Fujimori13 | 2014 | Japan | 601 | Intervention delivered by empathy-trained practitioner (based on SHARE model) vs. treatment delivered by untrained practitioner | Cancer | Immediately after intervention | Physical: n/a Psychological: Distress (Hospital Anxiety and Depression Score) Adverse events: n/a |
| Kaptchuk 14 | 2008 | USA | 175 | Augmented consultation vs. time-limited patient-practitioner relationship (initial consultation duration <5 minutes) | Irritable bowel syndrome (IBS) | 3 weeks after intervention | Physical: n/a Psychological: IBS symptoms (IBS Global Improvement Scale) Adverse events: any reported |
| Little17 | 2015 | UK | 224 | Intervention delivered by empathy-trained practitioner (based on KEPe-Warm model) vs. treatment delivered by untrained practitioner | Any condition in any patient attending their primary care doctor | Immediately after intervention | Physical: n/a Psychological: Satisfaction (7-point Medical Interview Satisfaction Scale) Adverse events: n/a |
| Soltner23 | 2011 | France | 68 | Consultation by practitioner trained to provide additional empathy (with 5 min extra time) vs. consultation delivered by practitioner instructed to give a neutral consultation. | Gynaecological problem requiring day-care procedure | Immediately after intervention | Physical: n/a Psychological: Anxiety (100mm numerical VAS) Adverse events: Changes in acute psychological burden (scores 0-10) |
| Vangronsfeld26 | 2012 | Sweden | 28 | Practitioner actively/empathically listening and validating during a 15 min consultation vs. usual care | Chronic back pain | Immediately after intervention | Physical: n/a Psychological: Pain (0-10 point scale) Adverse events: n/a |
| White30 | 2012 | UK | 221 | Empathetic consultation vs. Non-empathetic consultation | Chronic osteoarthritis) | 7 days after intervention | Physical: n/a Psychological: Pain (100mm VAS) Adverse events: Any reported |
| Expectations | |||||||
| Benedetti10 | 2003a | Italy | 42 | Open delivery of analgesia (lidocaine) with positive message vs hidden delivery of analgesia without message | Post-op pain | 30 and 60 min after intervention | Physical: n/a Psychological: Pain intensity (10-point VAS) Adverse events: n/a |
| Benedetti10 | 2003b | Italy | 30 | Open delivery of sedative (diazepam) with positive message vs hidden of sedative delivery without message | Post-op pain | 2 hours after intervention | Physical: n/a Psychological: Anxiety (State-Trait Anxiety Inventory) Adverse events: n/a |
| Benedetti10 | 2003c | Italy | 10 | Open delivery of electrical subthalamic nucleus stimulation with positive message vs hidden delivery without message | Parkinson’s disease | Immediately after intervention | Physical: Hand movement velocity (m/s) Psychological: n/a Adverse events: n/a |
| de Craen41 | 2001 | Netherlands | 111 | Positive vs. neutral message | Chronic pain | Immediately after intervention | Physical: n/a Psychological: Pain (10cm VAS) Adverse events: any reported |
| Dutt-Gupta12 | 2007 | n/a | 101 | Positive vs. neutral message | Acute pain | Immediately after intervention | Physical: n/a Psychological: Pain (10-point Verbal numerical rating scale). Adverse events: % of patients vocalising pain |
| Goodenough 42 | 1997 | Australia | 36 | Positive vs. neutral message | Acute pain | Immediately after intervention | Physical: n/a Psychological: Pain (Faces Pain Scale, scoring 0-6) Adverse events: n/a |
| Kemeny 15 | 2007 | USA | 45 | Positive vs. neutral message | Asthma | Unclear (most likely 1 week following treatment) | Physical: Calculated concentration of methacholine required to induce 20% decrease in FEV1 Psychological: n/a Adverse events: n/a |
| Knipschild 16 | 2005 | The Netherlands and Belgium | 128 | Positive message and communication of certainty vs. neutral message | Acute pain | 14 days following treatment | Physical: n/a Psychological: Feeling recovered from illness (yes/no) Adverse events: n/a |
| Lauder43 | 1995 | UK | 226 | Positive vs. neutral message | Post-op nausea | 24 hours after surgery | Physical: Antiemetic use Psychological: Nausea (10- point scale) Adverse events: Patient experience of vomiting or retching (yes/no) |
| Olsson44 | 1989 | Sweden | 100 | Positive vs. neutral message | Acute streptococcal tonsillitis | Two days after intervention | Physical: n/a Psychological: Feel better after operation (yes/no) Adverse events: n/a |
| Petersen19 | 2012 | Denmark | 19 | Positive vs. neutral message | Post-op neuropathic pain | Immediately after the intervention | Physical: n/a Psychological: Pain (10-point VAS) Adverse events: n/a |
| Petersen18 | 2014 | Denmark | 18 | Positive vs. neutral message | Post-op neuropathic pain | Immediately after treatment | Physical: n/a Psychological: Pain (10-point VAS) Adverse events: n/a |
| Phillips20 | 2006 | USA | 80 | Positive suggestion vs. neutral suggestion delivered by healthcare practitioner | Impaired physical function requiring rehabilitation | Immediately after intervention | Physical: Functional performance (7-point scale) Psychological: Self-efficacy (9-item Likert measure) Adverse events: n/a |
| Resnick45 | 1996 | USA | 77 | Positive vs. neutral message | Impaired physical function among the elderly requiring rehabilitation | 2 days after discharge | Physical: Functional performance (7-point scale) Psychological: Pain (11-point scale) Adverse events: n/a |
| Rief21 | 2017 | Germany | 78 | Positive vs. neutral message | Disability after heart surgery | 6 months after surgery | Physical: Physical quality of life (12-item Short Form Health Survey, 0-100) Psychological: Pain (Disability Index, range=0-70) Adverse events: any reported |
| Ronel22 | 2011 | Germany | 28 | Positive vs. neutral message | Acute chest pain with negative biomarkers | Immediately after intervention | Physical: % Diameter stenosis Psychological: Chest pain (10-point scale) Adverse events: n/a |
| Suarez-Almazor24 | 2010 | USA | 455 | Positive vs. neutral message | Osteoarthritis of the knee | 3 months after treatment | Physical: Mobility (timed get up and go test) Psychological: Pain (WOMAC subscale, range: 0-500) Adverse events: exacerbation of knee pain, bruising at injection site, cramps, headache, infection at needle site |
| Szilagyi25 | 2007 | Hungary | 60 | Positive vs. neutral message | Osteoarthritis Ventilated for ≥48 hrs in a hospital ICU | 2 weeks after treatment | Physical: Mean ventilation hours Psychological: n/a Adverse events: Deaths |
| Thomas46 | 1987 | UK | 200 | Positive vs. neutral message | Undiagnosed symptoms experienced by primary care patients | Two weeks after consultation | Physical: n/a Psychological: Dichotomous (feel much better or not) Adverse events: n/a |
| Varelmann27 | 2010 | USA | 140 | Positive suggestion vs. negative suggestion | Acute needle pain | Immediately after intervention | Physical: n/a Psychological: Pain (10-point VAS) Adverse events: n/a |
| Wang28 | 2008 | China | 241 | Positive suggestion vs. neutral suggestion | Acute pain after abdominal hysterectomy | 6 hours after surgery | Physical: Morphine consumption (mg) Psychological: Pain (10-point VAS) Adverse events: Various including nausea, dizziness, vomiting) |
| Wise29 | 2009 | USA | 478 | Positive vs. neutral message | Asthma | From baseline over 4 weeks | Psychological: Asthma quality of life Physical: Peak expiratory flow (PEF) Adverse events: Headaches |
VAS: visual analog scale.
Empathy interventions
Seven trials (n = 2169) tested the effects of empathy interventions.11,13,14,17,23,26,30 Two of these were carried out in each of: the United Kingdom and France; and one in each of: Japan, United States and Sweden. Most studies were conducted in primary care, and the timing of the outcome assessment ranged from immediately after the intervention to three weeks. The studies included between 2826 and 818 patients,29 with an average of 317 (Table 1).
The interventions within these trials involved practitioners displaying a range of verbal and non-verbal behaviours (eTable 3 in the Supplement). These behaviours were all similar because they instantiated the same conceptualisation of empathy (see Methods). The control groups in these trials received standard care, which did not involve additional time with the patient. The conditions and experiences included in these studies were chronic pain,11,26,30 anxiety,23 distress among cancer patients,13 symptoms of irritable bowel syndrome14 and satisfaction after primary care consultations.17 Outcomes were assessed using questionnaires, validated symptom scores and visual analogue scores.
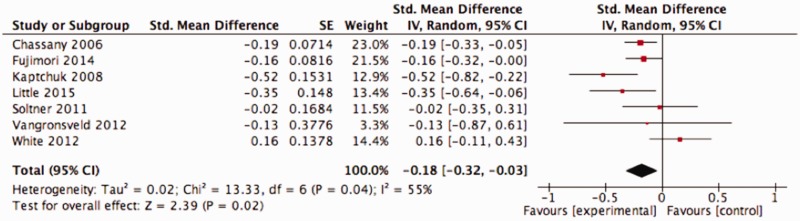
All but one study reported the same (positive) effect direction.30 Enhanced practitioner empathy had a small patient benefit, with a standardised mean difference −0.18 (95% confidence interval −0.32 to −0.03; I2 = 55%) (Figure 1). A funnel plot did not reveal evidence of publication bias (see eFigure 2 in the Supplement); however, the funnel plots with so few studies are difficult to interpret so publication bias remains possible. The overall risk of bias for these outcomes was low, and the quality of the evidence was low (eTable 4 in the Supplement).
Figure 1.
Effects of empathy interventions.
In the three empathy studies (n = 1214) reporting harms,11,30 we found no significant between intervention groups (odds ratio 1.00 [95% confidence interval 0.40 to 2.48; I2 = 61%]) (eFigure 3 in the Supplement). The quality of the evidence was very low (eTable 4 in the Supplement).
One empathy intervention study14 reported participant-assessed quality of life, using the 34-question irritable bowel syndrome Quality of Life47 score. Empathic care seemed to improve quality of life (standardised mean difference 0.43 [95% confidence interval 0.13 to 0.73]). Four studies (including 955 patients) reporting satisfaction as an outcome13,17,23,26 suggested that this was improved by a small and not statistically significant amount (standardised mean difference 0.26 [95% confidence interval −0.02 to 0.54; I2 = 67%]) (eFigure 4 in the Supplement).
There was no direct evidence on the cost-effectiveness of interventions designed to train clinicians in empathic behaviours. However, two empathy intervention studies reported how much time was allowed for physicians to respond to questions in an emphatic manner.14,23 Practitioners took 50% more time (5 min for a 10-min consultation) to enhance empathy in one trial, and an additional 35–40 min in another.14
For our subgroup analysis investigating trials investigating the same condition, three empathy trials11,26,30 reported effects of empathic care on pain (all chronic). These reported a non-statistically significant benefit (standardised mean difference −0.05 [95% confidence interval −0.32 to 0.22; I2 = 61%]) (eFigure 5 in the Supplement). For our sensitivity analysis of less biased trials, three studies were judged to have an unclear risk of bias for random allocation or allocation concealment.11,13,23 When these were removed from the analysis, the effect size increased from −0.18 (95% confidence interval −0.32 to −0.03) to −0.22 (95% confidence interval −0.57 to 0.13) but was no longer statistically significant. There were too few studies to conduct our pre-planned sensitivity analysis for studies in which we imputed data, or harms (see eMethods and eResults in the Supplement).
In an exploratory analysis, we found no difference in outcomes between studies with longer or shorter follow-up (see eResults, eFigure 6 in the Supplement), and the effect seems to last up to six weeks.
Expectation interventions
Twenty-two studies investigated expectation interventions (n = 2732) (Table 1).10,12,15,16,18–22,24,25,27–29,41–46 All but one had adequate data for pooling12 and one publication reported three studies.10 We refer to the separate studies within the same publication in the figures as Benedetti 2003a, Benedetti 2003b, and Benedettie 2003c, and report details of each study individually in eTable 2 within the Supplement. Six studies were carried out in the United States, three in Italy, two in each of Australia, Denmark, Germany, The Netherlands and/or Belgium, and the United Kingdom; and one in each of Hungary, Sweden and China. Most of the studies were conducted in primary care, and the timing of the outcome assessment ranged from immediately after the intervention to six months later. The studies included between 1110 and 455 patients,24 with an average of 119 (eTable 2 in the Supplement). Most of the studies were conducted in primary care, and the intervention involved similar verbal messages intended to induce a positive expectation about the outcome in the patient (eTable 3 in the Supplement). All but two of the studies had the same (positive) effect direction.16,28
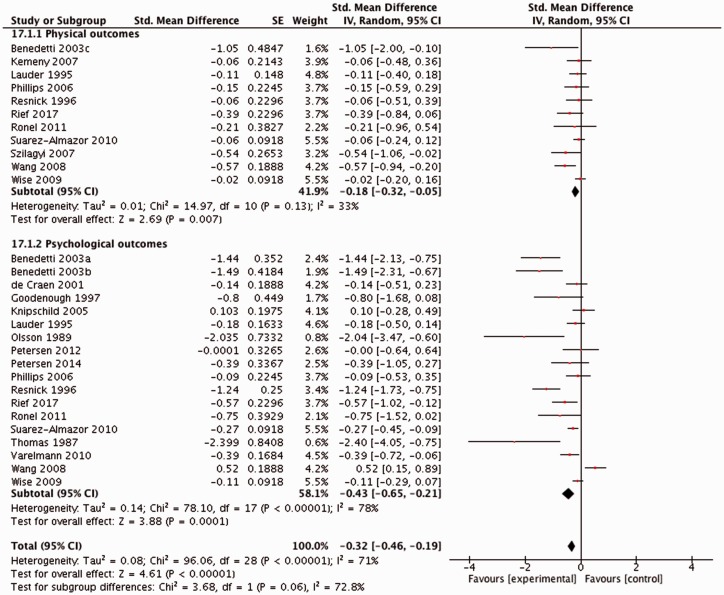
Eleven of the expectation studies (n = 1790) reported the effects of expectations on physical outcomes and showed a significant benefit of expectation interventions (standardised mean difference −0.18 [95% confidence interval −0.32 to −0.05; I2 = 33%]) (Figure 2). Outcomes included physical function, artery diameter stenosis and length of stay in hospital (Table 1, eTable 2 in the Supplement). The quality of the evidence was moderate (eTable 4 in the Supplement). Eighteen studies within 17 publications (n = 2014) reported the effects of expectations on psychological outcomes. The effect was statistically significant (standardised mean difference -0.43 [95% confidence interval -0.65 to -0.21; I2 = 78%]) (Figure 2). Funnel plots revealed some evidence of publication bias for studies with psychological outcomes, and the quality of the evidence was low (eTable 4 in the Supplement). The effects of expectation interventions with psychological outcomes were tested in pain, anxiety and patient satisfaction.
Figure 2.
Effects of expectations interventions.
The effects were positive for all physical outcomes and in all but two of the psychological outcomes.16,48 The effect was positive but not statistically significant in the study without data eligible for pooling (see eResults in the Supplement).12
Eight expectation intervention trials (n = 1492) reported harms, and there was no significant difference in the frequency of harm between intervention groups: odds ratio 1.05 ([95% confidence interval 0.60 to 1.85] I2 = 75%, p = 0.52) (eFigure 3 in the Supplement). A funnel plot did not reveal evidence of publication bias (see eFigure 2 in the Supplement) and the quality of the evidence was very low (eTable 4 in the Supplement).
For the secondary outcomes, three expectation intervention studies21,24,29 reported participant assessed quality of life (assessed in different ways, see eMethods in the Supplement). Expectation interventions seemed to slightly improve quality of life (standardised mean difference 0.25 [95% confidence interval 0.06 to 0.56; I2 = 74%]) (eFigure 8 and eTable 4 in the Supplement).
Four studies (n = 924) reported the effects of patient satisfaction using patient-reported scales.24,28 Patients in the expectation intervention group reported significantly higher satisfaction scores (standardised mean difference 0.60 [95% confidence interval 0.04 to 1.15; I2 = 87%]) (eFigure 4 in the Supplement). None of the expectation intervention trials reported whether the consultation time was increased.
For our subgroup analysis, 10 expectation studies reported the effects on pain and the effects were moderate (−0.28 [95% confidence interval −0.52 to −0.05; I2 = 2%]) (eFigure 5 in the Supplement). Within these, five reported effects on acute pain and five reported effects on chronic pain. The effect was greater in acute pain (0.54 [95% confidence interval −1.06 to −0.02]) compared with chronic pain (−0.08 [95% confidence interval −0.23 to −0.06]) (eFigure 9 in the Supplement). The methods for assessing acute and chronic pain were similar (mostly visual analog scales).
For our sensitivity analysis, when five expectation intervention trials with physical outcomes judged to be at a high risk of bias10,15,25,43,45 were excluded from the analysis, the effect size was reduced from −0.18 (95% confidence interval −0.32 to −0.05) to −0.17 (95% confidence interval −0.35 to −0.00). When the 11 expectation intervention trials with psychological outcomes judged to be at a high risk of bias according to the same criteria were removed from the analysis, the effect size was reduced from −0.43 (95% confidence interval −0.65 to −0.21) to −0.27 (95% confidence interval −0.56 to 0.02). When the expectation intervention studies reporting harms with a high risk of bias were removed, the harms remained similar with the odds ratio changing from 1.19 (95% confidence interval 0.71 to 1.99) to 1.21 (95% confidence interval 0.64 to 2.31). There were too few studies to conduct our pre-planned sensitivity analysis for studies in which we imputed data (see eMethods and eResults in the Supplement).
Table 2.
Effects of interventions.
| Standardised mean difference (95% confidence interval) | Heterogeneity (I2) | References | |
|---|---|---|---|
| Empathy | −0.18 (−0.32 to −0.03) | 55% | 11,13,14,17,23,26,30 |
| Expectations | −0.33 (−0.47 to −0.22) | 72% | 10,12,15,16,18–22,24,25,27–29,41–46 |
| Physical | −0.18 (−0.31 to −0.05) | 33% | 10,15, 20–22,24,25,28,29,43,45 |
| Psychological | -0.43 (-0.65 to -0.21) | 78% | 10,16,18–22,24,27–29,41–46 |
| Quality of life | 0.29 (0.04 to 0.54) | 75% | 14,21,24,29 |
| Empathy | 0.43 (0.13 to 0.73) | n/a (one study) | 14 |
| Expectations | 0.25 (−0.06 to 0.56) | 80% | 21,24,29 |
| Patient satisfaction | 0.41 (0.16 to 0.67) | 80% | 13,16,17,23,24,26,28,44 |
| Empathy | 0.26 (−0.02 to 0.54) | 67% | 13,17,23,26 |
| Expectations | 0.60 (0.04 to 1.15) | 87% | 16,24,28,44 |
| Pain | −0.22 (−0.40, −0.05) | 64% | |
| Empathy | −0.05 (−0.32, 0.22) | 61% | 11,26,30 |
| Expectations | -0.28 (-0.52 to -0.05) | 62% | 10,16,18,19,22,24,28,41,42 |
The effect seemed to last six months, with no difference between studies with longer and shorter follow-up (see eResults, eFigure 6 in the Supplement).
Discussion
Summary of evidence
We found that conveying empathy and inducing positive expectations in healthcare consultations consistently reduce pain and anxiety by a small amount. Positive messages delivered by practitioners also seem to improve some physical outcomes such as bronchial activity in asthmatic patients and physical function in postoperative patients. Some studies also suggest that delivering positive messages can improve patient satisfaction and health-related quality of life. In the most common condition (pain), the effect of both empathy and expectations interventions was equivalent to a 1- to 2-point reduction in pain on a 10-point visual analog scale. These interventions are unlikely to harm patients. In most analyses, the risk of bias was low to moderate, and the quality of the evidence was low.
Strengths and limitations
This is an up-to-date, comprehensive study of an area that patients have stated is important (see eMethods in the Supplement). Other strengths include the use of a published protocol, the use of GRADE to evaluate the overall quality of evidence and a search strategy that identified trials in this conceptually complex area.
A limitation is that there is likely to be overlap between the studies in our review and other studies of interventions that modify the way practitioners communicate. Empathy is related to compassion, self-efficacy, self-hypnosis and motivational interviewing, and any intervention involving patient–practitioner communication may involve some degree of empathy. Also, any intervention aimed at changing the way healthcare practitioners communicate might be expected to convey something about outcomes, which, in the context of treatments, would often be positive. We mitigated this limitation by using an explicit and replicable search strategy identified trials in which empathy and expectations were explicitly manipulated. This marks an important step forward in this conceptually difficult field and can be used as a benchmark for future studies in this area. Another limitation was the variability of interventions, practitioners, patients and conditions, which led to high statistical heterogeneity in most outcomes and was the main factor leading to a low grading of evidence quality.35 In spite of the high statistical heterogeneity, the effect direction was, with two exceptions, consistent. This justified pooling results and informed our interpretation of the findings. Furthermore, the classification of some outcomes (in addition to pain) as psychological or physical was challenging. To address this limitation we reported conditions and outcomes, and conducted an exploratory analysis comparing subjective with objective outcomes (see Table 1, eFigure 10 in the Supplement).
Also, most trials in our review did not contain sufficient data about how practitioners were trained, what specific behaviours they were trained to change and which behaviours were most effective for improving patient outcomes.49 Future research addressing this gap is required to optimise implementation of this evidence. Given that the National Institute for Health and Care Excellence (NICE) defines empathy as a component of high-quality care,50 further research in this area should arguably be a priority.
The trials in this review also did not report potential harms to practitioners, for example due to additional emotional demands. This should be considered in future empathy research. Finally, the cost-effectiveness of empathy and expectations interventions remains to be evaluated.
Comparison with other studies
This is the most up-to-date review of this topic and, unlike in previous studies in this area, we were able to pool results because of consistent effect direction.35 Our results complement a related review showing benefits of patient-centred care;2 empathy may be a precondition for patient-centred decision making.51 The benefits of empathy and expectations interventions for pain appear to be similar to those of many common pharmacological treatments.52,53
Conclusions and implications
Practitioners who take time to enhance how they express empathy and deliver positive messages are likely to bring small improvements to a range of psychological and physical patient conditions, improve overall patient satisfaction with care, without inducing any harm. The effects appear to be similar to those of many common pharmacological treatments for the conditions treated. A clear grasp of the best and most cost-effective approaches to practitioner training in empathic and positive communication is now required to optimise how we implement this evidence.
Supplemental Material
Supplemental material for Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis by Jeremy Howick, Andrew Moscrop, Alexander Mebius, Thomas R Fanshawe, George Lewith, Felicity L Bishop, Patriek Mistiaen, Nia W Roberts, Eglė Dieninytė, Xiao-Yang Hu, Paul Aveyard and Igho J Onakpoya in Journal of the Royal Society of Medicine
Declarations
Competing Interests
None declared.
Funding
JH and AM were supported by the British Medical Association Dawkins and Strutt Award. PA was supported by the CLAHRC (The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health).
Ethics approval
This is a secondary analysis and no ethical approval is required.
Guarantor
JH.
Contributorship
JH wrote the first draft of the manuscript, screened half of the titles, abstracts and full text, extracted data from half of the studies, and is guarantor. AnM contributed to title, abstract, and full text screening, data extraction, as well as giving editorial input to the manuscript. TF provided editorial input, and provided statistical advice. ED contributed to title, abstract and full text screening, data extraction. MX contributed to title, abstract and full text screening, data extraction. FB assisted with the data extraction, and with general editorial input to the manuscript. NR assisted with the literature searches. GL passed away in April 2017. He assisted with the conceptualisation of the project, assisted with title, abstract, and full text screening, data extraction and with suggestions for framing the background and conclusion. He did not participate in the final writing up of the results, as this was done after his passing. PM assisted with title, abstract, and full text screening, data extraction. PA contributed to the conceptualisation of the. AM contributed to the Characteristics of Included Studies, assisted with the analysis. IJO contributed to the screening, extraction of updated searches, the GRADE assessments. All authors made editorial suggestions on the entire manuscript and approved before it was submitted.
Acknowledgements
We thank Paul Little for his input to the conceptualisation of the project, Zelda di Blasi for the inspiration, and Stephen Senn also provided some additional statistical advice.
Provenance
Not commissioned; peer-reviewed by Julie Morris and revised following peer review at another journal.
References
- 1.Vermani M, Marcus M, Katzman MA. Rates of detection of mood and anxiety disorders in primary care: a descriptive, cross-sectional study. Primary Care Companion CNS Disord 2011; 13: e1–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2012; 12: CD003267–CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care 2009; 47: 826–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013; 3: e001570–e001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore PJ, Adler NE, Robertson PA. Medical malpractice: the effect of doctor-patient relations on medical patient perceptions and malpractice intentions. West J Med 2000; 173: 244–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract 2013; 63: e76–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians' empathy and clinical outcomes for diabetic patients. Acad Med 2011; 86: 359–364. [DOI] [PubMed] [Google Scholar]
- 8.Kiosses VN, Karathanos VT, Tasioni A. Empathy promoting interventions for health professionals: a systematic review of RCTs. J Compassionate Health Care 2016; 3: 7–7. [Google Scholar]
- 9.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet 2001; 357: 757–762. [DOI] [PubMed] [Google Scholar]
- 10.Benedetti F, Maggi G, Lopiano L, Lanotte M, Rainero I, Vighetti S, et al. Open versus hidden medical treatments: the patient's knowledge about a therapy affects the therapy outcome. Prevent Treat 2003; 6. [Google Scholar]
- 11.Chassany O, Boureau F, Liard F, Bertin P, Serrie A, Ferran P, et al. Effects of training on general practitioners' management of pain in osteoarthritis: a randomized multicenter study. J Rheumatol 2006; 33: 1827–1834. [PubMed] [Google Scholar]
- 12.Dutt-Gupta J, Bown T, Cyna AM. Effect of communication on pain during intravenous cannulation: a randomized controlled trial. Br J Anaesth 2007; 99: 871–875. [DOI] [PubMed] [Google Scholar]
- 13.Fujimori M, Shirai Y, Asai M, Kubota K, Katsumata N, Uchitomi Y. Effect of communication skills training program for oncologists based on patient preferences for communication when receiving bad news: a randomized controlled trial. J Clin Oncol 2014; 32: 2166–2172. [DOI] [PubMed] [Google Scholar]
- 14.Kaptchuk TJ, Kelley JM, Conboy LA, Davis RB, Kerr CE, Jacobson EE, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 2008; 336: 999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kemeny ME, Rosenwasser LJ, Panettieri RA, Rose RM, Berg-Smith SM, Kline JN. Placebo response in asthma: a robust and objective phenomenon. J Allergy Clin Immunol 2007; 119: 1375–1381. [DOI] [PubMed] [Google Scholar]
- 16.Knipschild P, Arntz A. Pain patients in a randomized trial did not show a significant effect of a positive consultation. J Clin Epidemiol 2005; 58: 708–713. [DOI] [PubMed] [Google Scholar]
- 17.Little P, White P, Kelly J, Everitt H, Mercer S. Randomised controlled trial of a brief intervention targeting predominantly non-verbal communication in general practice consultations. Brit J Gen Pract 2015; 65: e351–e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Petersen GL, Finnerup NB, Grosen K, Pilegaard HK, Tracey I, Benedetti F, et al. Expectations and positive emotional feelings accompany reductions in ongoing and evoked neuropathic pain following placebo interventions. Pain 2014; 155: 2687–2698. [DOI] [PubMed] [Google Scholar]
- 19.Petersen GL, Finnerup NB, Norskov KN, Grosen K, Pilegaard HK, Benedetti F, et al. Placebo manipulations reduce hyperalgesia in neuropathic pain. Pain 2012; 153: 1292–1300. [DOI] [PubMed] [Google Scholar]
- 20.Phillips RJ. An Examination o f the Impact of Self-efficacy Interventions versus Outcome Expectancy Interventions on Efficacy Beliefs, Expectancy Beliefs, Participation, and Functional Performance in a Population of Medical Rehabilitation Patients, Santa Barbara, CA: Fielding Graduate University, 2006, pp. 218–218. [Google Scholar]
- 21.Rief W, Shedden-Mora MC, Laferton JA, Auer C, Petrie KJ, Salzmann S, et al. Preoperative optimization of patient expectations improves long-term outcome in heart surgery patients: results of the randomized controlled PSY-HEART trial. BMC Med 2017; 15: 4–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ronel J, Mehilli J, Ladwig KH, Blattler H, Oversohl N, Byrne RA, et al. Effects of verbal suggestion on coronary arteries: Results of a randomized controlled experimental investigation during coronary angiography. Am Heart J 2011; 162: 507–511. [DOI] [PubMed] [Google Scholar]
- 23.Soltner C, Giquello JA, Monrigal-Martin C, Beydon L. Continuous care and empathic anaesthesiologist attitude in the preoperative period: impact on patient anxiety and satisfaction. Br J Anaesth 2011; 106: 680–686. [DOI] [PubMed] [Google Scholar]
- 24.Suarez-Almazor ME, Looney C, Liu Y, Cox V, Pietz K, Marcus DM, et al. A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res 2010; 62: 1229–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szilágyi K, Diószeghy C, Benczúr L, Varga K. Effectiveness of psychological support based on positive suggestion with the ventilated patient. Eur J Ment Health 2007; 2: 149–170. [Google Scholar]
- 26.Vangronsveld KL, Linton SJ. The effect of validating and invalidating communication on satisfaction, pain and affect in nurses suffering from low back pain during a semi-structured interview. Eur J Pain 2012; 16: 239–246. [DOI] [PubMed] [Google Scholar]
- 27.Varelmann D, Pancaro C, Cappiello EC, Camann WR. Nocebo-induced hyperalgesia during local anesthetic injection. Anesth Analg 2010; 110: 868–870. [DOI] [PubMed] [Google Scholar]
- 28.Wang F, Shen X, Xu S, Liu Y, Ma L, Zhao Q, et al. Negative words on surgical wards result in therapeutic failure of patient-controlled analgesia and further release of cortisol after abdominal surgeries. Minerva Anestesiol 2008; 74: 353–365. [PubMed] [Google Scholar]
- 29.Wise RA, Bartlett SJ, Brown ED, Castro M, Cohen R, Holbrook JT, et al. Randomized trial of the effect of drug presentation on asthma outcomes: the American Lung Association Asthma Clinical Research Centers. J Allergy Clin Immunol 2009; 124: 436–44, 44e1–8–436–44, 44e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White P, Bishop FL, Prescott P, Scott C, Little P, Lewith G. Practice, practitioner, or placebo? A multifactorial, mixed-methods randomized controlled trial of acupuncture. Pain 2012; 153: 455–462. [DOI] [PubMed] [Google Scholar]
- 31.Mistiaen P, van Osch M, van Vliet L, Howick J, Bishop FL, Di Blasi Z, et al. The effect of patient-practitioner communication on pain: a systematic review. Eur J Pain 2016; 20: 675–688. [DOI] [PubMed] [Google Scholar]
- 32.Chen YF, Hemming K, Chilton PJ, Gupta KK, Altman DG, Lilford RJ. Scientific hypotheses can be tested by comparing the effects of one treatment over many diseases in a systematic review. J Clin Epidemiol 2014; 67: 1309–1319. [DOI] [PubMed] [Google Scholar]
- 33.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009; 151: W65–W94. [DOI] [PubMed] [Google Scholar]
- 34.Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract 2002; 52(Suppl): S9–S12. [PMC free article] [PubMed] [Google Scholar]
- 35.Higgins JJ, Green S. The Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011), Chichester: The Cochrane Collaboration, 2011. [Google Scholar]
- 36.Schünemann H, Brozek J, Oxman A. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendation, Hamilton: Group TGW, 2008. [Google Scholar]
- 37.GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.). Available from gradepro.org.
- 38.Jain R. Pain and the brain: lower back pain. J Clin Psychiatry 2009; 70: e41–e41. [DOI] [PubMed] [Google Scholar]
- 39.Song F, Sheldon TA, Sutton AJ, Abrams KR, Jones DR. Methods for exploring heterogeneity in meta-analysis. Eval Health Prof 2001; 24: 126–151. [DOI] [PubMed] [Google Scholar]
- 40.Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med 2000; 19: 3127–3131. [DOI] [PubMed] [Google Scholar]
- 41.de Craen AJ, Lampe-Schoenmaeckers AJ, Kraal JW, Tijssen JG, Kleijnen J. Impact of experimentally-induced expectancy on the analgesic efficacy of tramadol in chronic pain patients: a 2 x 2 factorial, randomized, placebo-controlled, double-blind trial. J Pain Symptom Manage 2001; 21: 210–217. [DOI] [PubMed] [Google Scholar]
- 42.Goodenough B, Kampel L, Champion GD, Laubreaux L, Nicholas MK, Ziegler JB, et al. An investigation of the placebo effect and age-related factors in the report of needle pain from venipuncture in children. Pain 1997; 72: 383–391. [DOI] [PubMed] [Google Scholar]
- 43.Lauder GR, McQuillan PJ, Pickering RM. Psychological adjunct to perioperative antiemesis. Br J Anaesth 1995; 74: 266–270. [DOI] [PubMed] [Google Scholar]
- 44.Olsson B, Olsson B, Tibblin G. Effect of patients' expectations on recovery from acute tonsillitis. Fam Pract 1989; 6: 188–192. [DOI] [PubMed] [Google Scholar]
- 45.Resnick BM. Self-efficacy in Geriatric Rehabilitation, Maryland, MD: Faculty of the Graduate School, University of Maryland, 1996, pp. 296–296. [Google Scholar]
- 46.Thomas KB. General practice consultations: is there any point in being positive? Br Med J (Clin Res Ed) 1987; 294: 1200–1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, et al. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol 2000; 95: 999–1007. [DOI] [PubMed] [Google Scholar]
- 48.Wang L, Xun P, Zhao Y, Wang X, Qian L, Chen F. Effects of lead exposure on sperm concentrations and testes weight in male rats: a meta-regression analysis. J Toxicol Environ Health Part A 2008; 71: 454–463. [DOI] [PubMed] [Google Scholar]
- 49.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687–g1687. [DOI] [PubMed] [Google Scholar]
- 50.National Institute for Health and Care Excellence. Service User Experience in Adult Mental Health Services. Quality Statement 2: Empathy, Dignity and Respect, London: National Institute for Health and Care Excellence, 2017. [Google Scholar]
- 51.The Health Foundation. Person-centred Care Made Simple, London: The Health Foundation, 2014. [Google Scholar]
- 52.Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW. Non-steroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev 2016; 2: CD012087–CD012087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moore R, Chi C, Wiffen P, Derry S, Rice A. Oral nonsteroidal anti-inflammatory drugs (NSAIDs) for neuropathic pain in adults. Cochrane Database Syst Rev 2015; 10: CD010902–CD010902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rief W, Nestoriuc Y, von Lilienfeld-Toal A, Dogan I, Schreiber F, Hofmann SG, et al. Differences in adverse effect reporting in placebo groups in SSRI and tricyclic antidepressant trials: a systematic review and meta-analysis. Drug Saf 2009; 32: 1041–1056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis by Jeremy Howick, Andrew Moscrop, Alexander Mebius, Thomas R Fanshawe, George Lewith, Felicity L Bishop, Patriek Mistiaen, Nia W Roberts, Eglė Dieninytė, Xiao-Yang Hu, Paul Aveyard and Igho J Onakpoya in Journal of the Royal Society of Medicine