Introduction
Trichophyton erinacei is a member of the Trichophyton mentagrophytes complex, a zoonotic dermatophyte that is very rarely isolated as a human pathogen. It often causes a localized itchy rash at the size of contact, such as the extremities, and is typically reported in the context of hedgehog exposure.1, 2, 3, 4, 5, 6, 7, 8
Epidemiologically, T erinacei was first recognized in New Zealand then in Europe, Africa, and Australia. Case reports existed in East Asia since the early 2000s in Japan,7 Korea,1 and Taiwan.5 We report the first case, to our knowledge, of T erinacei arising in Southeast Asia in the context of hedgehog exposure.
Case report
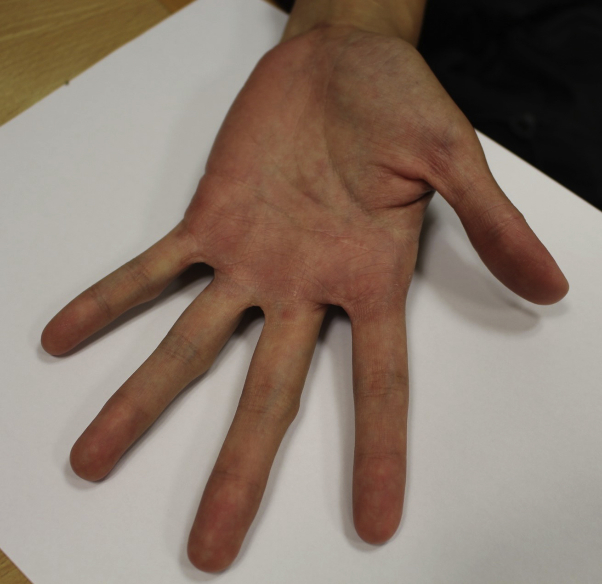
A 37-year-old woman with a history of human leukocyte antigen (HLA)-B27–positive spondyloarthropathy treated with methotrexate (7.5 mg once a week) and prednisolone (10 mg once a day) presented to the emergency department (ED) and subsequently dermatology clinic for a pustular rash over the left hand. It started 2 weeks prior as a single pustule on the thumb before spreading to involve the whole palm. It was itchy and painful. She had intermittent fevers for the previous 2 weeks.
She reported an exposure to cactus sap and getting pricked in the plant nursery she was working in before the onset of the rash. During her first presentation in the ED, there were small erythematous pustules over the first dorsal web space and scattered over the palm (Fig 1).
Fig 1.

Small erythematous papules and pustules over the left palm.
On dermatology review 2 days later, the number of pustules was increased, coalescing into small pustular lakes over the palm and dorsal web space (Fig 2). The nails were uninvolved, and there were no other rashes on other parts of her body.
Fig 2.
Small lakes of pustules over the left palm.
The initial impression was a contact dermatitis to cactus sap with secondary pyoderma. The differential diagnosis was pustular psoriasis in view of her history of HLA-B27 spondyloarthropathy. A swab was taken from the pustule for bacterial, mycobacterial, and fungal cultures. She was treated with oral Augmentin, topical betamethasone dipropionate, gentamicin and miconazole, and potassium permanganate compress and advised to avoid gardening until the lesions healed.
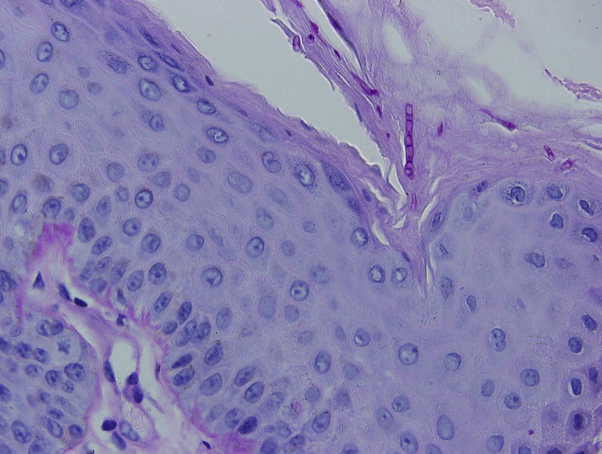
On review 6 days later, new pustules continued to develop; hence, a skin biopsy was performed with deeper tissue specimens sent for culture. The histology findings showed spongiotic dermatitis with subcorneal pustules and a neutrophilic infiltrate. Septated fungal hyphae were seen in the stratum corneum (Fig 3).
Fig 3.
Section of skin biopsy shows septated fungal hyphae within the stratum corneum. (Periodic acid–Schiff; original magnification: ×600.)
Fungal culture from the skin swab and skin biopsy grew T erinacei; bacterial and mycobacterial cultures were negative. The mold was initially isolated on Sabouraud dextrose agar with chloramphenicol and Mycosel agar (Becton Dickinson, Franklin Lakes, NJ) at 30°C. Urease was positive at day 4, and the final identification was confirmed based on 100% similarity of internal transcribed spacer region sequence to T erinacei ATCC 28443 on the National Institutes of Health database.9
Subsequently, we discovered that she was in contact with her friend's pet hedgehog on 2 occasions in the month before the rash and was bitten and pricked by its thorns. She was given a 2-week course of oral terbinafine with remarkable resolution of the rash (Fig 4).
Fig 4.
Resolution of pustular lesions 2 weeks after initiation of terbinafine.
Discussion
T erinacei is the most common dermatophyte isolated in hedgehogs, with infection rates of 20% to 47%.6 Other than hedgehog exposure, other reported exposures include an elephant10 and direct human-to-human contact by kissing.3 Immunosuppression use in our patient likely predisposed her to infection after contact with the hedgehog.
Infection typically occurs at the sites of contact—most commonly the hands as in tinea manuum,1, 4, 6, 7 and less frequently as tinea facei2, 8 and tinea kerion barbae.3 They may present as an erosive inflammatory vesiculopustular eruption1, 5 or scaling eczematous plaques mimicking eczema.1, 4 Infection in hedgehogs may be asymptomatic or may present with scaling and loss of quills.1
Diagnosis is confirmed by culturing the fungus on agar plates and DNA sequencing. Topical antifungals are rarely adequate, and systemic treatment options include terbinafine and itraconzole. The animal ideally should be treated as well.
Such zoonotic infections are rare and, as in our patient, the inoculating event may be only determined after isolation of the fungus.3 An index of suspicion is important, especially with the increasing number of exotic domestic pets.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Rhee D.-Y., Kim M.-S., Chang S.-E. A case of tinea manuum caused by Trichophyton mentagrophytes var. erinacei: the first isolation in Korea. Mycoses. 2009;52(3):287–290. doi: 10.1111/j.1439-0507.2008.01556.x. [DOI] [PubMed] [Google Scholar]
- 2.Concha M., Nicklas C., Balcells E. The first case of tinea faciei caused by Trichophyton mentagrophytes var. erinacei isolated in Chile. Int J Dermatol. 2012;51(3):283–285. doi: 10.1111/j.1365-4632.2011.04995.x. [DOI] [PubMed] [Google Scholar]
- 3.Sidwell R.U., Chan I., Francis N., Bunker C.B. Trichophyton erinacei kerion barbae from a hedgehog with direct osculatory transfer to another person. Clin Exp Dermatol. 2014;39(1):38–40. doi: 10.1111/ced.12197. [DOI] [PubMed] [Google Scholar]
- 4.Schauder S., Kirsch-Nietzki M., Wegener S., Switzer E., Qadripur S.A. [From hedgehogs to men. Zoophilic dermatophytosis caused by Trichophyton erinacei in eight patients] Hautarzt. 2007;58(1):62–67. doi: 10.1007/s00105-006-1100-4. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh C.-W., Sun P.-L., Wu Y.-H. Trichophyton erinacei infection from a hedgehog: a case report from Taiwan. Mycopathologia. 2010;170(6):417–421. doi: 10.1007/s11046-010-9333-2. [DOI] [PubMed] [Google Scholar]
- 6.Philpot C.M., Bowen R.G. Hazards from hedgehogs: two case reports with a survey of the epidemiology of hedgehog ringworm. Clin Exp Dermatol. 1992;17(3):156–158. doi: 10.1111/j.1365-2230.1992.tb00193.x. [DOI] [PubMed] [Google Scholar]
- 7.Mochizuki T., Takeda K., Nakagawa M., Kawasaki M., Tanabe H., Ishizaki H. The first isolation in Japan of Trichophyton mentagrophytes var. erinacei causing tinea manuum. Int J Dermatol. 2005;44(9):765–768. doi: 10.1111/j.1365-4632.2004.02180.x. [DOI] [PubMed] [Google Scholar]
- 8.Lee D.-W., Yang J.-H., Choi S.-J. An unusual clinical presentation of tinea faciei caused by Trichophyton mentagrophytes var. erinacei. Pediatr Dermatol. 2011;28(2):210–212. doi: 10.1111/j.1525-1470.2011.01391.x. [DOI] [PubMed] [Google Scholar]
- 9.Innis M., Gelfand D., Sninsky J., White T. PCR Protocols: A Guide to Methods and Applications. Academic Press Inc; New York: 1990. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics; pp. 315–322. [Google Scholar]
- 10.Borges-Costa J., Martins M da L. Trichophyton erinacei skin infection after recreational exposure to an elephant in Southeast Asia. Pathog Glob Health. 2014;108(1):58–59. doi: 10.1179/2047773213Y.0000000117. [DOI] [PMC free article] [PubMed] [Google Scholar]