Abstract
Background
A system of care designed to measure and improve process measures such as symptom recognition, emergency response, and hospital care has the potential to reduce mortality and improve quality of life for patients with ST-elevation myocardial infarction (STEMI).
Objective
To document the methodology and rationale for the implementation and impact measurement of the Heart Rescue India project on STEMI morbidity and mortality in Bangalore, India.
Study Design
A hub and spoke STEMI system of care comprised of two interventional, hub hospitals and five spoke hospitals will build and deploy a dedicated emergency response and transport system covering a 10 Km. radius area of Bangalore, India. High risk patients will receive a dedicated emergency response number to call for symptoms of heart attack. A dedicated operations center will use geo-tracking strategies to optimize response times including first responder motor scooter transport, equipped with ECG machines to transmit ECG's for immediate interpretation and optimal triage. At the same time, a dedicated ambulance will be deployed for transport of appropriate STEMI patients to a hub hospital while non-STEMI patients will be transported to spoke hospitals. To enhance patient recognition and initiation of therapy, school children will be trained in basic CPR and signs and symptom of chest pain. Hub hospitals will refine their emergency department and cardiac catheterization laboratory protocols using continuous quality improvement techniques to minimize treatment delays. Prior to hospital discharge, secondary prevention measures will be initiated to enhance long-term patient outcomes.
Keywords: STEMI, Quality improvement, Angioplasty, Thrombolysis
1. Introduction
Cardiovascular disease (CVD) is now the leading cause of morbidity and mortality worldwide [1]. In India, CVD is the leading cause of death, approaching 4–5 million deaths annually; a rate that has doubled over the past two decades. By 2020, 2.6 million Indians are predicted to die due to coronary artery disease (CAD), which constitutes 54% of all CVD deaths [2]. In addition, by 2020, nearly 60% of patients with cardiovascular disease worldwide will be of Indian descent as Indians have a higher genetic predisposition for and earlier risk of CVDs than other global ethnicities [3,4].
The increase in acute ST-elevation myocardial infarction (STEMI and mortality in India is an expanding public health problem. The Heart Rescue India Project addresses this by using a system of care improvement approach shown to improve outcomes in other CVD conditions [[5], [6], [7]]. This approach includes enhancing patient recognition and timely response to symptoms, improving acute treatment, and initiating secondary prevention therapies prior to hospital discharge. In this context, prehospital delay remains a major hurdle in the institution of early reperfusion therapy, which is crucial in salvaging 'at-risk' myocardium and reducing adverse cardiovascular events following STEMI and has not been well addressed in prior studies [8]. Low public awareness, inadequate emergency transportation infrastructure, and the lack of a coordinated Emergency Medical Services (EMS) system are major contributors to problem [9]. Despite efforts aimed at reducing the prehospital time and treatment delay, a considerable proportion of patients with STEMI present late and receive delayed or no reperfusion therapy. Prehospital delay in India is also associated with difficulty in arranging financial means to cover medical costs, place of symptom onset, symptom interpretation, and mode of transportation [10].
Primary percutaneous coronary intervention (PCI) is the current standard of care for acute ST elevation myocardial infarction. Although most of the data on primary PCI in acute STEMI is from western countries, a recent study describes the outcomes of primary PCI for acute STEMI at a tertiary care center in Northern India [11]. Primary PCI was associated with high success rate, low mortality in non-shock patients, and low complication rates.
The goal of HRI is to adapt tested strategies of working systems of care from the United States to build a replicable sustainable model of STEMI care in a defined 10 km radius geographical area in Bangalore, India. This project aims to demonstrate improved outcome in patients diagnosed with STEMI through a multi hospital integrated Hub & Spoke model of STEMI care. This will be accomplished by creating a novel, dedicated prehospital emergency response program which includes prehospital diagnosis and transport to appropriate hospitals capable of providing timely revascularization, and post-acute treatment preventive care to improve patient outcomes and reduce the likelihood of STEMI recurrence (Table 1).
Table 1.
Critical elements for prehospital response to STEMI and related cardiac arrest.
| 1. Hub and Spoke model of care with a pharmacoinvasive strategy using a tiered response system with first responder motor scooters complemented ambulance response for stabilization and transport. |
| 2. Registration process to identify at-risk patients with the use of hospital help desks and a school program to reach potential patients via their children. |
| 3. Initialization of secondary prevention prior to discharge with primary care provider CME programs to enhance continued prevention therapies and behavior change with opportunities for continued engagement of these high risk and post MI patients through texting, calls, and community events. |
| 4. Electronic data collection and process communication via a unique online system for coordination of emergency response, and data collection and continuous feedback to monitor and improve STEMI care. |
| 5. Coordinated emergency response, equipment and personnel from both private and government systems used in a coordinated system. |
Table 2.
Hub & spoke hospitals, with distance to hub hospital.
| Hub | Spoke |
| M S Ramaiah Memorial Hospital | 1. People Tree Hospital 5.8 km |
| 2. Aveksha Hospital-8.3 km | |
| 3. Santhosh Hospital-7.7 km | |
| Hub | Spoke |
| Suguna Hospital | 1. Ananya Hospital-2.2 km |
| 2. Sreenivasa Hospital-3.8 km |
2. Methods
2.1. Professional engagement
A professional advisory group has been constituted to share expertise and experience in formulating process recommendations for the conduct of Heart Rescue India (HRI) program, provide ongoing feedback on the conduct of HRI and serve as a vehicle to inform policy makers and the cardiology community in India about the progress and findings from the program. The advisory group is composed of prominent cardiologists, cardiac surgeons, and emergency room physicians from across India involved in both private and government healthcare facilities. In addition, there are representatives from health and family welfare, the government of Karnataka Community Services Groups, Road Transport Department, secondary high school principals, Civil Defense, Home Guards, Red Cross Society, and other non-governmental organizations.
2.2. Patient engagement
Help desks in each of the hub and spoke hospitals will be used to screen, identify, and engage patients at risk for CVD in the HRI catchment area communities, educate them on the signs and symptoms of acute CVD. Help desk staff will teach patients how to access the HRI system of care and motivate them to call the toll-free emergency phone number when they or someone they witness is experiencing symptoms of STEMI. The focus will be on high-risk patients because the information will be more personally relevant and engaging for them since they are more likely to develop heart attack symptoms.
Knowing that simply raising awareness does not necessarily lead to behavior change [[12], [13], [14]], the HRI Program will incorporate formative research (e.g., focus groups) with patients into the development of our education strategies. Patients in the catchment area face several barriers beyond lack of awareness that may prevent behavior change (i.e., calling the toll-free number), such as lack of confidence in emergency medical service response time or the quality of care, and fears about financial burdens that emergency medical services and medical treatment might mean for the family. Formative research will help us develop a better understanding of what educational message(s) and modalities who will motivate them, what influences them, and how they like to receive information, and learn more about the context surrounding patient response to symptom onset so that we can develop more effective messages which can lead to reduction in delays in seeking treatment.
2.3. Engaging school children
One important lesson learned during the implementation of HRI was the impact that children can have in helping their parents recognize the need for cardiac care. As a result, Heart Rescue India (HRI) includes school children in its plans for community engagement by forming a task force of local physicians, teachers and principals. Goals for the program include education to identify CVD risk factors, recognize signs and symptoms of acute CVD and understand when and how to call for help. Students will also be trained in cardiopulmonary resuscitation (CPR) and the use of an automatic external defibrillator (AED). After completing the program, they will be asked to educate their parents by bringing the emergency phone number home, and encourage their parents to enroll in the HRI system and call the HRI emergency phone number if they develop heart attack symptoms.
2.4. Prehospital response
As noted above, delay in treatment of STEMI is a major contributor to morbidity and mortality [15]. Though several factors contribute to prehospital delay, two critical factors are patient's delay in seeking help and transportation delay. In the HRI catchment area, we will increase awareness of heart attack symptoms by organizing community educational outreach events In addition, we will reach higher risk patients through the use of “help desks”, manned by volunteers, at the two hub and seven spoke hospitals involved in this project. These high-risk patients, identified through simple World Health Organization (WHO) cardiovascular risk score screenings, will be targeted for continued text messaging and other communication vehicles to reinforce our messaging over time, since heart attack symptoms may develop over the months and years following their initial educational opportunities.
To reduce prehospital delays in the heavy traffic of Bangalore, Motor scooters will be used to transport a first responder nurse or paramedic who will assess and stabilize the patient, perform and transmit an ECG to the MS Ramaiah command center. If there is evidence of STEMI, the cardiac catheterization laboratory personnel will be activated at the nearest available hub hospital. At the same time an ambulance will be dispatched to transport the patient to the hospital for urgent PCI.
Since out of hospital cardiac arrest (OHCA) may occur in patients with STEMI, an organized and coordinated resuscitation program will be part of our STEMI emergency response. The Resuscitation Academies (RA) concept revolves around the motto ‘measure and improve’ and utilizes hands-on experiential learning for health care providers across the continuum of care. This includes emergency call takers, prehospital providers as well as receiving health care teams at the hospital to train and function as a system. The HRI program will follow the American Heart Association (AHA) recommendations for chain of survival, beginning with the initiation of the call from family members. Early recognition of a cardiac event and immediate initiation of emergency care, including the dispatch of prehospital providers and clear directions to the family regarding compression only CPR, has been demonstrated to double or triple neurologically intact survival [16].
The RA, during its annual continuing medical education programs and training events will follow the American Heart Association (AHA) recommendations and will also include didactic education on the pathophysiology of STEMI, how it differs from sudden cardiac arrest (SCA), and explain Standard of Care treatments for both. The RA will also demonstrate the care priorities and elements associated with High-Performance CPR. Quality CPR training is a means to improve survival from cardiac arrest and for this project, raise awareness about STEMI recognition and emergency care. CPR that is performed in accordance with standard guidelines, minimizing breaks in compressions, allowing full chest recoil, with adequate compression depth, and with adequate compression rate can increase survival from cardiac arrest [17].
2.5. Hospitals
HRI is a complex project reaching across the continuum of acute care for STEMI. The project has engaged two hub hospitals that are percutaneous coronary intervention (PCI) capable and strategically located within a 10 Km radius of each other in the northwest region of Bangalore with a catchment area population of about 400,000. Within this area are five participating spoke hospitals which will provide emergency and general care, including thrombolysis, but do not have invasive cardiology facilities. This group of seven hospitals have agreed to work together as a coordinated network to provide appropriate emergency services for chest pain patients with ECG evidence of STEMI. They will be linked together by a prehospital control system utilizing a central control center coordinating first responder motor scooters with ECG capability to facilitate triage to the appropriate network hospital. Patients with evidence of STEMI as identified by first responders will be transported directly to a hub hospital, if available. There are also five spoke hospitals within the catchment area to provide care for identified patients without evidence of STEMI and for STEMI patients provide thrombolytic therapy as part of a pharmacoinvasive strategy when catheterization facilities are not available. In addition HRI will interface with the only public hospital which provides PCI which is the south of Bangalore. Because of more prolonged transport times, we will use a pharmacoinvasive strategy when STEMI patients request transfer. The relationship of the hub and spoke hospitals is indicated in Table 2. A recent trial of a hub-and spoke model for STEMI patients in Tamil Nadu, India has demonstrated an increase of the use of PCI for STEMI in a more rural setting [18]. We seek to apply this approach to urban Bangalore.
2.6. Reperfusion strategies
The most critical component of STEMI care is to quickly recognize the presence of STEMI and activate the emergency response system. HRI will develop and use a dedicated emergency response system with a dedicated toll free emergency number to call for patients experiencing symptoms of a possible myocardial infarction (MI). Patients at high risk of MI, identified by the help desks at each of the hub and spoke hospitals, will receive educational messages as reminders of the symptoms of MI and the importance of calling the emergency number.
Toll free calls will be received by the 24 h helpline/dispatch center located at MS Ramaiah Memorial Hospital (RMH) through a dedicated toll free number staffed by trained professionals who will identify the geographical location of the call and activate the nearest the HRI spoke hospital to attend to the patient. The nearest spoke hospital will send a nurse/EMT on a motor scooter equipped with an emergency kit. On arrival to the location, the first responder will record symptoms, vitals, perform ECG and dispatch the same to the central server of the Ramaiah control center. At the same time, an Advanced Cardiac Life Support (ACLS) ambulance will also be dispatched to the scene, but will usually arrive after the scooter and initial assessment has been completed. The heart code personnel (Emergency/Cardiology) at RMH will interpret the ECG when received in the control center; if the patient is found to have a STEMI and is a candidate for PCI, he/she will be transferred the nearest available hub hospital and the catheterization laboratory will be activated to receive the patient. If the patient requests transfer to Sri Jayadeva Institute government hospital, which may result from patient financial concerns, a pharmacoinvasive strategy will be employed with the PCI done at Jayadeva Hospital. If the ECG is found to be inconclusive, the patient will be asked to be taken to the nearest spoke hospital (if stable) or to the hub hospital (if unstable) for further evaluation and management.
2.7. Secondary prevention
The project will initiate secondary prevention interventions including medical therapy and lifestyle change recommendations prior to hospital discharge as listed as measures 15–20 in Table 3 Quality Measures. This is designed to increase the post hospital adherence to these recommendations as demonstrated in multiple observational studies [16].
Table 3.
Quality measures heart rescue India.
| Prehospital |
| 1. Number of calls to central call center/month (rolling total to track usage) |
| 2. Time from MI symptom (chest pain, dyspnea, nausea, diaphoresis, dizziness, syncope) onset to call placed to the center |
| a. Numerator: number of calls with time < = 60 min |
| b. Denominator: number of calls reporting symptoms listed above |
| c. Mean time and range for all calls per month |
| 3. Time from initial call placed to center to nurse motorcycle arrival |
| a. Numerator: number of arrivals<< = 15 min from call center call |
| b. Denominator: number of calls |
| c. Mean time and range for all calls per month |
| 4. Time from initial call placed to call center and first ECG |
| a. Numerator: Number of patients who call within 30 min |
| b. Denominator: Number of patients who have a first ECG done by first responder |
| 5. Time from first responder ECG diagnosis of STEMI to hospital arrival |
| a. Numerator: STEMI prehospital setting diagnosis to Hub hospital ambulance arrival within 30 min |
| b. Denominator: number of patient with STEMI diagnosis in prehospital setting transported to Hub hospital by ambulance |
| Hospital |
| 6. Percent STEMI patients arriving at the hospital by ambulance |
| a. Numerator: Number of patients with STEMI who arrive by ambulance |
| b. Denominator: All STEMI patients who arrive at the hospital |
| 7. STEMI patients with cardiac arrest in prehospital setting and survival to hospital |
| a. Numerator: Number of cardiac arrest patients with STEMI diagnosed in prehospital setting surviving to hospital arrival |
| b. Denominator: All cardiac arrest patients with STEMI diagnosed in prehospital setting |
| 8. Time from first medical contact to reperfusion |
| a. Numerator: Number of STEMI patients who receive PCI or thrombolysis within 3 h from initial call placed to call center |
| b. Denominator: Number of patient with STEMI receiving PCI/thrombolysis |
| 9. Door to needle time |
| a. Numerator: Number of patients with STEMI who arrive by ambulance and door to needle time <30 min |
| b. Denominator: All patient arriving by ambulance, with STEMI receiving thrombolytic agents in the ED |
| 10. Door to needle time walk-in |
| a. Numerator: Number of patients with STEMI who do not arrive by ambulance with door to needle time <60 min |
| b. Denominator: All patients not arriving by ambulance with STEMI receiving thrombolytic agents in the ED |
| 11. Door to balloon time |
| a. Numerator: Number of STEMI patients who with door to balloon time < = ;60 min |
| b. Denominator: All STEMI patients receiving PCI on hospital arrival |
| 12. Door to balloon time walk-in |
| a. Numerator: Number of STEMI patients who do not arrive by ambulance with door to balloon time < = ;90 min |
| b. Denominator: All STEMI patients not arriving by ambulance, receiving PCI on hospital arrival |
| 13. Percent STEMI patients receiving reperfusion |
| a. Numerator: Number of STEMI patients who receive reperfusion |
| b. Denominator: All STEMI patients not transferred out of networka |
| 14. Survival to hospital discharge (in-hospital mortality) |
| a. Numerator: All STEMI patients surviving until hospital discharge not transfer out of network |
| b. Denominator: All STEMI patients not transferred out of networka |
| 15. Adverse events (heart failure, stroke, bleeding requiring transfusion) |
| a. Numerator: All STEMI patients discharge without adverse events |
| b. Denominator: All STEMI patients admitted to the hospital |
| 16. Beta blocker |
| a. Numerator: All STEMI patients discharged with a beta blocker |
| b. Denominator: All STEMI patients discharged without contraindications to beta blockers |
| 17. Angiotensin converting enzyme/angiotensin receptor blockers (ACE/ARB) |
| a. Numerator: All STEMI patients discharged with ACE/ARB |
| b. Denominator: All STEMI patients discharged without contraindications to ACE/ARB |
| 18. Aspirin (ASA) |
| a. Numerator: All STEMI patients discharged with ASA |
| b. Denominator: All STEMI patients discharged without contraindications to ASA |
| 19. Statins |
| a. Numerator: All STEMI patients discharged with a statin |
| b. Denominator: All STEMI patients discharged without contraindications to statins |
| 20. Smoking cessation counseling |
| a. Numerator: All STEMI patients who report tobacco use discharged with smoking cessation counseling |
| b. Denominator: All STEMI patients discharged who report tobacco use |
| 21. Follow-up appointment |
| a. Numerator: All STEMI patient discharged who have a follow-up appointment (Family practitioner, cardiologist, or general practitioner) |
| b. Denominator: All STEMI patients discharged to home |
Network is defined as any Hub, Spoke hospital within the Heart Rescue India list of participating hospitals.
2.8. Process improvement strategies
A critical element of Heart Rescue India will be the ability to document and improve care that is based on evidence-based clinical guidelines. Tools and processes to support data collection and the use of these data, as well as the necessary system and cultural changes needed to utilize the data, are critically dependent on a framework of continuous improvement and sharing of best practices. Standardized protocols are a key first step. Much of STEMI care is time dependent and thus relies on efficient care delivery strategies. As noted above, a new system of prehospital care using a pre-notification strategy will facilitate triage and, for STEMI, activation of the catheterization laboratory team prior to the patient's arrival.
Didactic presentations, regular team sharing meetings for all of the involved hospital staff and prehospital responders will be strategies employed to accelerate the rate of improvement [17,18]. Health care staff will be trained to conduct improvement cycles to change existing systems and will be provided with a mechanism to learn from each other to determine what works best. Since hospital environments have their own, unique characteristics, staff will be taught key methods to adapt and customize these ideas. Treatment teams will collectively develop, in conjunction with project leadership, effective evidence-based protocols which will be shared and standardized across the HRI network for prehospital and hospital STEMI care. Prehospital, emergency room and catheterization laboratory teams will find the most effective way to move patients through the system for the right treatment at the right time by adapting key strategies from other programs around the world and from each other. Finally, post intervention care will include the initiation of secondary prevention treatments prior to hospital discharge for all STEMI patients [19]. Bringing together resources and expertise to actively support quality improvement programs from the seven diverse hospitals and the prehospital coordinated response system will play a key role in reaching our shared goal of providing the right care for every STEMI patient every time.
2.9. Data collection and measures
Data collection will be largely automated by electronic interfacing with existing hospital systems. Included in the design are customized mobile applications (apps) to enable collection of care processes in real time and to support execution of the processes of care throughout the flow of STEMI patients through the acute response system.
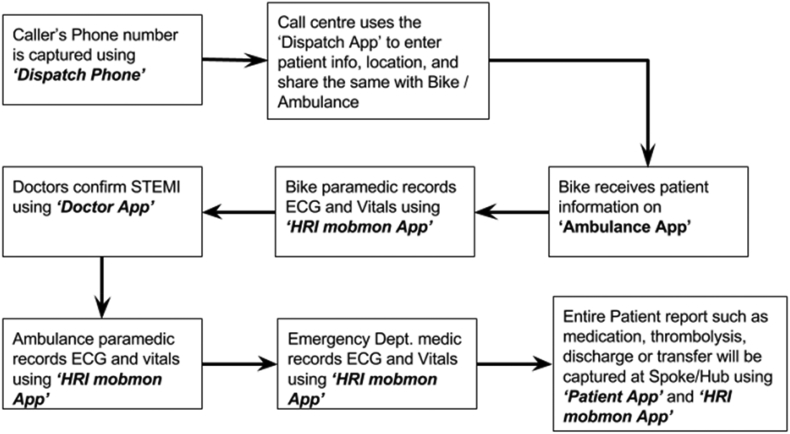
The sequence of events for the response to STEMI patients is illustrated in Fig. 1. The workflow is supported by mobile applications and PC software to be installed and used during the HRI program:
-
●
Dispatch Phone - a single phone capable of displaying the incoming caller's phone number.
-
●
Dispatch App - a single Windows PC app that will gather patient information and help relay the information and location to the ambulance app (bike and ambulance).
-
●
Ambulance App - This app will share information from the Dispatch to track the patient.
-
●
HRI Ambulance and Hospital App - This will gather ECG and other vitals, to the remote doctors for STEMI diagnosis.
-
●
Doctor App - This app - to be used by Doctors - will share information from the Dispatch to track the patient arrival in the Emergency Department/Coronary Care Unit (ED/CCU), and to capture timestamped events.
-
●
Patient App - a single Windows PC software tool that will help gather all patient data elements within the scope of HRI project. This PC software would be used in ED, CCU, Catheterization lab, etc.
Fig. 1.
Workflow of the HRI project.
Quality measures for HRI have been adapted from STEMI processes of care for prior projects in the United States and India as previously noted. Table 3 lists the measures for prehospital and hospital care of STEMI patients to evaluate the effectiveness of HRI. In addition to the acute care measures, we will also initiate measures of secondary prevention started in the hospital prior to discharge that have been adapted from the American Heart Association's Get with the Guidelines project in the United States, China, and Brazil [20].
2.10. Statistical analysis
Based on the findings of India STEMI studies and our own experience, sample size calculations for the present study will give us the ability to detect decreases in the fraction of STEMI patients who delay over 2 h by at least 7.5% for time from symptom onset to reperfusion and at least a 7% reduction in patients with delayed door to reperfusion with 80% power and a 95% confidence level. Our roll out of data collection, targeted at-risk population education, expansion of pre-hospital care and monthly data reports starting in May 2018, will likely require 16 months to demonstrate effect. This time will allow for data collection from at least 300 patients in the initial 3 months of launch to establish a baseline. All analyses will be performed using SAS (SAS Institute, Research Triangle, NC). Data are presented as proportions. For the other HRI measures, changes in compliance rates for the measured outcomes over the study period were assessed using the Fisher exact test, with the Bonferroni method of Holm for multiple comparisons. All P values are 2-sided, with P ≤ 0.05 considered statistically significant. The baseline period is defined as the time period in which the projects initial 300 records are submitted. Progress over the study period will be further assessed at each calendar quarter subsequent to baseline. When missing data elements are present for a specific measure, that patient was excluded for analysis for the measure. At least 1200 additional STEMI patients seen over the course of the next 12 months will allow for measurement of effect of ongoing quality improvement efforts and further expansion of pre-hospital care.
3. Discussion
3.1. Expected outcomes
HRI will develop and test a model for high quality, timely treatment of STEMI patients in a densely populated urban area of a large city in Southern India. Project success will depend on reaching patients at risk of MI and motivating them and their family to call for help when symptoms occur. The issues of traffic congestion will be addressed by using motor scooters for first responders equipped with ECG transmission capability. It is expected that using ECG transmission to confirm STEMI for catheterization laboratory pre-notification will reduce delays on arrival to the hospital.
A sophisticated data entry and coordination system will substantially automate data collection, including the use of timestamps to accurately determine critical time delays that will be addressed with our structural and quality improvement strategies. In addition, the location of scooters and ambulances will be tracked in the central control center to optimize their availability as needed. Finally, secondary prevention therapies will be initiated in the hospitals, prior to hospital discharge to enhance adherence and reduce recurrent events [21,22].
3.2. Sustainability planning
For any interventional strategy or process improvement to be long lasting, the program will need to be sustained. A sustainability program will need trained personnel who will undergo periodic training and retraining, ongoing process improvement and financial support. Programs are already in place to ensure ongoing personnel training and continuous process improvement. To continue and sustain these activities beyond the 5-year funding from the Medtronic Foundation, HRI will need to identify new sources of funding. There are several sources of funding including support from the Local, State and Central Governments, individual donations and Corporate Social Responsibility (CSR) mandated funds.
We anticipate considerable in-kind support from the local Government by allowing public employees such as police, paramedics, firefighters, home guard, and members of other publicly supported volunteer organizations to undergo training, and provide First Aid and Cardiopulmonary resuscitation (CPR) in the community when the need arises. We anticipate that the State Government will expand their skills development program to include paramedic training required to function effectively as First Responders during medical emergency. The State Government of Karnataka already has such programs, which cover the cost of providing training. The Central Government has several schemes for skills development that will provide financial support to the trainees to cover the cost of transportation to the training site, and boarding and lodging while they undergo training. Heart Rescue India leaders will apply for these funds to ensure continuity of the program. Toward this goal, The State of Karnataka has designated Heart Rescue India as its technical partner.
HRI will create a Development Office that will solicit grants from various National and International funding agencies, charitable foundations, and nonprofit organizations. We also expect this office to launch fund-raising programs to seek donations from individuals and smaller business entities.
The Companies Act 2013, first update in nearly 50 years, passed by the Indian Parliament has a “2%” clause. The 2% clause requires companies to set up a CSR board consisting of at least three directors with one of them being independent. The board is required to ensure that the company spends at least 2% of net profits it earned during the preceding 3 years. This rule applies to companies with a net worth of Indian Rupees (Rs). 5 billion or more, annual turnover or net profit of at least Rs. 10 billion or Rs. 50 million respectively. It is estimated that over 8000 companies will need to spend approximately Rs. 150 annually on CSR. Although there will be considerable demand for the CSR funds from over 3 million NGOs already operating in India, Heart Rescue India is confident that it can draw support from various corporations within the State of Karnataka because the act stipulates that companies “shall give preference to the local area and areas around where it operates.” Moreover, the HRI program is independently monitored by a program management team from the Research Triangle Institute (RTI), and the needs and outcome assessments are conducted independently by the Institute for Health Metrics and Evaluation (IHME). These arrangements ensure a high degree of transparency and will also ensure that the impact of the study will be evaluated objectively.
4. Conclusion
HRI is a complex, multi-facet program designed to integrate and optimize existing resources with improved strategies and systems to deliver definitive interventions for patients with STEMI in a defined urban area of Bangalore. The program will draw on practice guidelines, successful improvement strategies and outcome measures of STEMI systems of care in the United States and India to minimize the time from first medical contact to revascularization. This program will focus on ways to reduce the delay time from symptom onset to activating the prehospital emergency response, including training first responders to effectively treat associated cardiac arrest. HRI will support system improvement to reduce time to revascularization and provide improved post PCI care in the hospital, recognizing that initiation of secondary prevention measures will further improve quality of life and reduce recurrence [23,24].
Funding source
Medtronic Philanthropy provided input on site selection and the selection of ST elevation myocardial infarction as the primary focus of this initiative, but did not participate in the design of the study or data collection.
Contributor Information
Aruna Ramesh, Email: arunacr2@gmail.com.
Kenneth A. LaBresh, Email: klabesh@rti.org.
Bentley Bobrow, Email: Bentley.Bobrow@azdhs.gov.
Nayanjeet Chaudhury, Email: nayanjeet.chaudhury@medtronic.com.
Marcia Edison, Email: marciae@uic.edu.
Timothy B. Erickson, Email: timothyberickson@gmail.com.
John D. Manning, Email: john.d.manning@gmail.com.
Bellur S. Prabhakar, Email: bprabhak@uic.edu.
Pavitra Kotini-Shah, Email: pkotini@gmail.com.
Pamela A. Williams, Email: pamwilliams@rti.org.
Terry Vanden Hoek, Email: tvh@uic.edu.
References
- 1.Kalra A., Bhatt D.L., Rajagopalan S. Overview of coronary heart disease risk initiatives in South asia. Curr Atheroscler Rep. 2017;19:25. doi: 10.1007/s11883-017-0662-1. [DOI] [PubMed] [Google Scholar]
- 2.Mathers C.D., Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3 doi: 10.1371/journal.pmed.0030442. e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohn D. Getting to the heart of the matter in India. Lancet. 2008;372:523–524. doi: 10.1016/s0140-6736(08)61217-9. https://www.ncbi.nlm.nih.gov/pubmed/18711800 [DOI] [PubMed] [Google Scholar]
- 4.Rissam H.S., Kishore S., Trehan N. Coronary artery disease in young Indians—the missing link. J. Indian Acad. Clin. Med. 2001;2:128–131. http://medind.nic.in/jac/t01/i3/jact01i3p128.pdf [Google Scholar]
- 5.Diepen S.V., Girotra S., Abella B.S., Becker L.B., Bobrow B.J., Chan P.S., Fahrenbruch C., Granger C.B., Jollis J.G., McNally B., White L., Yannopoulos D., Rea T.D. Multistate 5-year initiative to improve care for out-of-hospital cardiac arrest: primary results from the HeartRescue project. J Am Heart Assoc. 2017;6 doi: 10.1161/JAHA.117.005716. e005716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwamm L.H., Fonarow G.C., Reeves M.J., Pan W., Frankel M.R., Smith E.E., Ellrodt A.G., Cannon C.P., Liang L., Peterson E.D., LaBresh K.A. Get with the Guidelines–Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or TIA. Circulation. 2009;119(1):107–115. doi: 10.1161/CIRCULATIONAHA.108.783688. [DOI] [PubMed] [Google Scholar]
- 7.Nichol G., Aufderheide T.P., Eigel B., Neumar R.W., Lurie G., Bufalino V.J., Callaway C.W., Menon V., Bass R.R., Abella B.S., Sayre M., Dougherty C.M., Racht E.M., Kleinman M.E., O'Connor R.E., Reilly J.P., Ossmann E.W., Peterson E. Regional systems of care for out-of-hospital cardiac arrest: a policy statement from the american heart association. Circulation. 2010;121:709–729. doi: 10.1161/CIR.0b013e3181cdb7db. [DOI] [PubMed] [Google Scholar]
- 8.Khan A., Phadke M., Lokhandwala Y.Y. A study of prehospital delay patterns in acute myocardial infarction in an urban tertiary care Institute in Mumbai. J Assoc Physicians India. 2017;65:24–27. https://www.ncbi.nlm.nih.gov/pubmed/28598044 [PubMed] [Google Scholar]
- 9.George L., Ramamoorthy L., Satheesh S. Prehospital delay and time to reperfusion therapy in ST elevation myocardial infarction. J Emerg Trauma Shock. 2017;10:64–69. doi: 10.4103/0974-2700.201580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubey G., Verma S.K., Bahl V.K. Primary percutaneous coronary intervention for acute ST elevation myocardial infarction: outcomes and determinants of outcomes: a tertiary care center study from North India. Indian Heart J. 2017;69:294–298. doi: 10.1016/j.ihj.2016.11.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathew A., Abdullakutty J., Sebastian P. Population access to reperfusion services for ST-segment elevation myocardial infarction in Kerala. India. Indian Heart J. 2017;69:S51–S56. doi: 10.1016/j.ihj.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ajzen I., Fishbein M. Prentice-Hall; 1980. Understanding Attitudes and Predicting Social Behaviour.http://www.citeulike.org/group/38/article/235626 [Google Scholar]
- 13.Christiano A., Neimand A. Stop raising awareness already. Stanford Soc. Innovat. Rev. 2017;15:34–41. [Google Scholar]
- 14.Cacioppo J.T., Petty R.E., Kao C.F. Central and peripheral routes to persuasion: an individual difference perspective. J. Pers. Soc. Psychol. 1986;51:1032. http://psycnet.apa.org/fulltext/1987-07221-001.html [Google Scholar]
- 15.Wu J.-R., Moser D.K., Riegel B. Impact of prehospital delay in treatment seeking on in-hospital complications after acute myocardial infarction. J. Cardiovasc. Nurs. 2011;26:184–193. doi: 10.1097/JCN.0b013e3181efea66. [DOI] [PubMed] [Google Scholar]
- 16.Bobrow B.J., Spaite D.W., Vadeboncoeur T.F. Implementation of a regional telephone cardiopulmonary resuscitation program and outcomes after out-of-hospital cardiac arrest. JAMA Cardiol. 2016;1:294–302. doi: 10.1001/jamacardio.2016.0251. [DOI] [PubMed] [Google Scholar]
- 17.Meaney P.A., Bobrow B.J., Mancini M.E. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 18.Alexander T., Mullasari A.S., Joseph G. A system of care for patients with ST-segment elevation myocardial infarction in India: the Tamil Nadu-ST-segment elevation myocardial infarction program. JAMA Cardiol. 2017;2:498–505. doi: 10.1001/jamacardio.2016.5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keller P.-F., Carballo S., Carballo D. Present and future of secondary prevention after an acute coronary syndrome. EPMA J. 2011;2:371–379. doi: 10.1007/s13167-011-0129-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berwick D.M. The science of improvement. J. Am. Med. Assoc. 2008;299:1182–1184. doi: 10.1001/jama.299.10.1182. [DOI] [PubMed] [Google Scholar]
- 21.LaBresh K.A. Using ‘get with the guidelines’ to prevent recurrent cardiovascular disease. Curr. Treat. Options Cardiovasc. Med. 2005;7:287–292. doi: 10.1007/s11936-005-0039-6. https://www.ncbi.nlm.nih.gov/pubmed/16004859 [DOI] [PubMed] [Google Scholar]
- 22.Jollis J.G., Al-Khalidi H.R., Roettig M.L. Regional systems of care demonstration project: american heart association mission: lifeline STEMI systems accelerator. Circulation. 2016;134:365–374. doi: 10.1161/CIRCULATIONAHA.115.019474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaBresh K.A., Fonarow G.C., Smith S.C., Jr. Improved treatment of hospitalized coronary artery disease patients with the get with the guidelines program. Crit. Pathw. Cardiol. 2007;6:98–105. doi: 10.1097/HPC.0b013e31812da7ed. [DOI] [PubMed] [Google Scholar]
- 24.Bushnell C.D., Olson D.M., Zhao X. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011;77:1182–1190. doi: 10.1212/WNL.0b013e31822f0423. [DOI] [PMC free article] [PubMed] [Google Scholar]