Abstract
Preclinical and clinical studies have shown bidirectional interactions within the brain-gut-microbiome axis. Gut microbes communicate to the central nervous system through at least 3 parallel and interacting channels involving nervous, endocrine, and immune signaling mechanisms. The brain can affect the community structure and function of the gut microbiota through the autonomic nervous system, by modulating regional gut motility, intestinal transit and secretion, and gut permeability, and potentially through the luminal secretion of hormones that directly modulate microbial gene expression. A systems biological model is proposed that posits circular communication loops amid the brain, gut, and gut microbiome, and in which perturbation at any level can propagate dysregulation throughout the circuit. A series of largely preclinical observations implicates alterations in brain-gut-microbiome communication in the pathogenesis and pathophysiology of irritable bowel syndrome, obesity, and several psychiatric and neurologic disorders. Continued research holds the promise of identifying novel therapeutic targets and developing treatment strategies to address some of the most debilitating, costly, and poorly understood diseases.
Keywords: Serotonin, Stress, Irritable Bowel Syndrome, Intestinal Permeability
Abbreviations used in this paper: ANS, autonomic nervous system; ASD, autism spectrum disorder; BBB, blood-brain barrier; BGM, brain-gut-microbiome; CNS, central nervous system; ECC, enterochromaffin cell; EEC, enteroendocrine cell; FFAR, free fatty acid receptor; FGF, fibroblast growth factor; 5-HT, serotonin; FXR, farnesoid X receptor; GF, germ-free; GI, gastrointestinal; GLP-1, glucagon-like peptide-1; GPR, G-protein–coupled receptor; IBS, irritable bowel syndrome; LPS, lipopolysaccharide; SCFA, short-chain fatty acid; SPF, specific-pathogen-free; TGR5, G protein-coupled bile acid receptor; Trp, tryptophan; 2BA, secondary bile acid
Summary.
The past decade has seen a paradigm shift in our understanding of the brain-gut axis. The exponential growth of evidence detailing the bidirectional interactions between the gut microbiome and the brain supports a comprehensive model that integrates the central nervous, gastrointestinal, and immune systems with this newly discovered organ. Data from preclinical and clinical studies have shown remarkable potential for novel treatment targets not only in functional gastrointestinal disorders but in a wide range of psychiatric and neurologic disorders, including Parkinson's disease, autism spectrum disorders, anxiety, and depression, among many others.
Results from preclinical studies published during the past decade strongly support the concept of bidirectional brain-gut-microbiome (BGM) interactions. Alterations in these interactions have been implicated not only in the pathogenesis and pathophysiology of classic brain-gut disorders such as irritable bowel syndrome (IBS) and other functional gastrointestinal disorders,1, 2 but a growing list of psychiatric and neurologic pathologies including affective disorders,3, 4 autism spectrum disorders (ASD),3, 5 Parkinson's disease,6 multiple sclerosis,7 and chronic pain.8 Although most of the literature associates gut microbiota composition with human health, development, and disease, evidence for causality remains sparse. The BGM axis’ interface with fundamental and disease-susceptible processes make it a novel therapeutic target, but this network remains insufficiently understood for intervention. In this review, we address current evidence supporting bottom-up and top-down signaling within the BGM axis and the emerging evidence supporting its contribution to human disease.
BGM State of the Science
Preclinical Evidence
Several experimental approaches in animal models have been used to study the influence of gut microbiota on the BGM axis, including manipulation with antibiotics,9 fecal microbial transplantation,9, 10 colonization with synthetic11 or human12, 13 microbiota, cultured gut organ systems,14, 15 probiotic administration,16 and germ-free (GF) animal models.17 Despite limitations to these approaches, significant progress has been made since Sudo et al17 first showed that the absence of normal gut microbiota early in life has significant effects on stress responsiveness in the adult and that these changes can be partially reversed by early colonization of the gut with conventional microbiota, even a single species. Subsequent investigations have further characterized the associated neurochemical changes, including altered cortical and hippocampal brain-derived neurotrophic factor levels,17, 18 reduced hippocampal serotonin (5-HT) receptor 1A expression,18 increased striatal monoamine turnover,19 and reduced synaptic plasticity gene expression,19 showing the microbiome’s diverse and potent influence over central nervous system (CNS) phenotypes. Accordingly, in addition to stress responsiveness,16, 20 the gut microbiota are implicated in relation to anxiety-like16, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 and depression-like behavior,16, 24, 25, 27, 29, 30, 31, 32 nociceptive response,8, 33, 34, 35, 36, 37 feeding behavior, taste preference, metabolic consequences,38, 39, 40 and their respective underlying physiologies. These preclinical studies have been reviewed extensively in the literature.3, 5, 41, 42, 43 Despite acknowledged limitations to the GF model,28, 41, 44 phenotype reversal by recolonization with specific-pathogen-free (SPF), human-derived, and synthetic microbiota validates some of the conclusions. Still, the well-characterized role of microbiota in neurogenesis and neurodevelopment45 moderates the translational relevance of these findings for adult conditions.
An alternative to the GF model approach is the use of broad-spectrum antibiotics to induce transient changes on the composition and diversity of fecal microbiota,9 although the effects on mucosa-associated microbial communities are incompletely understood. Antimicrobials also may interact directly with host physiology in mechanisms independent of the microbiome, such as their well-documented neurotoxic effects (reviewed by Grill and Maganti46). Nonetheless, broad-spectrum antibiotic treatment remains a powerful tool to identify gut microbial influence on the CNS. In mice with SPF microbiota, oral antibiotic administration increased exploratory behavior and hippocampal expression of brain-derived neurotrophic factor, which was associated with changes in the microbial profile.9 The failure to replicate these antibiotic-induced effects in GF mice suggests the CNS changes are not the result of off-target antibiotic interactions, however, developmental alterations in the GF model make this finding inconclusive. Long-term antibiotic treatment in adult mice reduced hippocampal neurogenesis and lead to deficits in novel object recognition tasks through a mechanism dependent on circulating monocytes.47 Adoptive transfer of Ly-6chi monocytes or voluntary exercise and probiotic treatment rescued these phenotypes.47
In contrast to the complete or partial depletion of gut microbiota as an experimental approach to identify and characterize microbial influence on the host CNS, the introduction of known microorganisms (usually as probiotics) to conventional models allows for normal development and risks fewer off-target effects. However, it is critical to acknowledge the possibility that transient exposure induces host responses inaccessible to resident communities. Orally administered probiotics have been shown to reduce basal or induced anxiety-like behavior,16, 20, 22, 24, 30, 48 attenuate induced obsessive-compulsive–like behavior,49 improve inflammation-associated sickness behavior,50 and even normalize developmental trajectories of emotion-related behavior after early life stress.51 Although infrequently used as an intervention directed specifically at the gut microbiota, diet can have profound, rapid, and reproducible effects on the structure of the gut microbiota in human beings and mice.52, 53, 54 Alterations in the gut microbial community through dietary change also have been shown to influence memory and learning,55, 56 while probiotic administration rescued diet-induced memory deficits in rats.57 In summary, preclinical studies have identified unequivocally the potent influence of gut microbiota on the CNS, but issues of reproducibility and off-target intervention effects demand continued improvement of experimental approaches.
Clinical Evidence
Experimental approaches to study the role of gut microbes to brain signaling have been restricted mostly to small clinical studies showing the association of gut microbial community structure with brain parameters and subjective outcomes of interventions with probiotics and prebiotics. Although no high-quality, controlled studies in human beings have reported the effects of interventions such as antibiotics or fecal microbial transplants on the brain or behavior, studies of probiotic interventions are increasing rapidly in number and gradually in scale and quality. A double-blind, placebo-controlled, pilot study of the probiotic Bifidobacterium longum NCC3001 in 44 adults with IBS and diarrhea was shown to reduce responses in the amygdala and frontolimbic regions to negative emotional stimuli as measured by functional magnetic resonance imaging.58 Although depression scores were lower with the intervention, anxiety and IBS symptoms were not affected. In healthy female control subjects, consumption of a fermented milk product with probiotics over 4 weeks was associated with significant changes in the functional connectivity between brain regions during an emotion recognition task, notably without concomitant detectable changes in gut microbial composition.59 Probiotic consumption also has been reported to reduce self-reported feelings of sadness and aggressive thoughts.60 A probiotic cocktail used to achieve reduction of anxiety- and depression-related behaviors in mice48 also was administered to healthy human beings to a similar effect.61
The translation of promising findings obtained in rodent studies has been limited. In a clinical trial with Lactobacillus rhamnosus (JB-1), the effects of which were seminally shown on mice by Bravo et al,16 performed no better than placebo on stress-related measures, hypothalamic pituitary adrenal axis response, inflammation, or cognitive performance in an 8-week trial with healthy males.62 Moreover, the pilot trial of Bifidobacterium longum NCC3001 described earlier did not recapitulate the effects observed in mice by the same research group22 and has been criticized for its fragility.63 This translational disconnect, or inconsistency, highlights the likelihood of host-specific microbiota interactions and underscores the importance of cautious extrapolation of preclinical findings. Furthermore, as shown by several studies, probiotic supplementation in human beings does not appear to change the gut’s microbiota composition but induces its effect on behavior via transient modification of the collective microbiome transcriptional state, as shown in GF mice and confirmed in monozygotic twins.64 This finding demands measurement of probiotic intervention on gut microbial profiles with technologies integrating metatranscriptomics and metabolomics and fundamental reconsideration of the functional equivalence of transient vs resident microorganisms. Better characterization of microbial community dynamics and metabolism coupled with improved models of their community ecology will help refine the mechanisms responsible for these effects and identify putative targets for therapeutic intervention.
Signaling Mechanisms From the Gut Microbiota to the Brain
Current evidence indicates that bottom-up modulation of the CNS by the microbiome occurs primarily through neuroimmune and neuroendocrine mechanisms, often involving the vagus nerve.16, 65, 66, 67 This communication is mediated by several microbially derived molecules that include short-chain fatty acids (SCFAs), secondary bile acids (2BAs), and tryptophan metabolites.65, 68, 69 These molecules propagate signals primarily through interaction with enteroendocrine cells (EECs), enterochromaffin cells (ECCs), and the mucosal immune system, but some cross the intestinal barrier, enter systemic circulation, and may cross the blood-brain barrier.68, 70, 71 It remains poorly understood if these molecules reach brain sites directly or only induce central responses via long-distance neural signaling by vagal and/or spinal afferents.16, 72 In addition to generating these metabolites that activate endogenous CNS signaling mechanisms, the microbiota can independently produce or contribute to the production of a number of neuroactive molecules including but not limited to γ-aminobutyric acid,73, 74 5-HT,75, 76 norepinephrine,76, 77 and dopamine,75, 76, 77 although it is unknown if they reach relevant receptors or achieve sufficient levels to elicit a host response.
Neuroendocrine and Enteroendocrine Signaling Pathways
An important pathway by which gut microbes and their metabolites communicate with the CNS involves the cells making up the endocrine system of the gut.78 There are at least 12 different types of these cells with several subtypes (in particular A, K, and L cells) present as subgroups along the intestine that contain different combinations of molecules. EECs are interspersed between gut epithelial cells throughout the length of the gut and contain more than 20 different types of signaling molecules, which often are colocalized and co-released. Released in response to chemical and or mechanical stimuli, these molecules can enter the systemic circulation and reach centers in the CNS involved in ingestive behavior (including the nucleus tractus solitarius and the hypothalamus) or act locally and activate closely adjacent afferent vagal terminals in the gut or liver to generate brain signals. A series of receptors involved in the regulation of satiety and hunger have been identified on these cells, which are activated by microbial metabolites including bile acids and SCFAs.
Although bile acids are endogenous molecules synthesized from cholesterol in the liver, the size and composition of the host’s pool of these molecules is heavily influenced by dietary intake, especially of fat,79 and the downstream metabolism by the gut microbiota (reviewed by de Aguiar et al80 and Wahlstrom et al81). Ileal expression of farnesoid X receptor (FXR), a nuclear receptor, is activated by bile acids leading to production of fibroblast growth factor 19 (FGF19), or its similarly functioning ortholog FGF15 in mice, which can enter the systemic circulation and cross the blood-brain barrier.82 Activation of the arcuate nucleus of the hypothalamus by the FXR/FGF19 action on agouti-related peptide/neuropeptide Y83 has been implicated in improved central regulation of energy and glucose metabolism84, 85, 86 and suppression of hypothalamic pituitary adrenal axis activity.87 Some intestinal L cells express surface receptor G protein-coupled bile acid receptor (TGR5), which is activated mostly by secondary bile acids, which are strongly influenced by microbial activity.88, 89 TGR5 signaling controls glucose homeostasis by mechanisms including increased glucagon-like peptide-1 (GLP-1) release by these L cells.90 Interestingly, these L cells also express FXR, which can regulate GLP-1 synthesis.91
SCFAs have been implicated as major signaling molecules mediating host-microbe communication via EECs and ECCs. These molecules are generated by microbial fermentation of host dietary-resistant starch and nonstarch polysaccharides and serve an important part in the host’s energy harvest while also stimulating colonic blood flow, fluid and electrolyte uptake, and mucosal proliferation.92 Dietary fiber intake is a major regulator of SCFA concentrations. In instances in which the host diet is low in fermentable fibers, microbes feed on mucus glycans and use alternative, less energetically favorable sources, resulting in reduced fermentative activity and SCFA production.93 Both preclinical and clinical data have shown that microbial activity, in particular the production of SCFAs, stimulate L cells located at the distal ileum to secrete peptide YY and GLP-1, which induce satiety and behavioral changes.65, 70, 94 Acetate, butyrate, and propionate modulate the expression and secretion of GLP-1 via free fatty acid receptor 2 (FFAR2)/G-protein–coupled receptor 43 (GPR43) and FFAR3/GPR41 on L cells,65 and GPR41s have been identified on different EECs in the gut.95 This widespread distribution of these receptors on and in EECs and ECCs involved in the regulation of food intake and digestion is consistent with the important role of the gut microbes in these processes and the expectations of holobiont co-evolution.
Enterochromaffin Cell Signaling
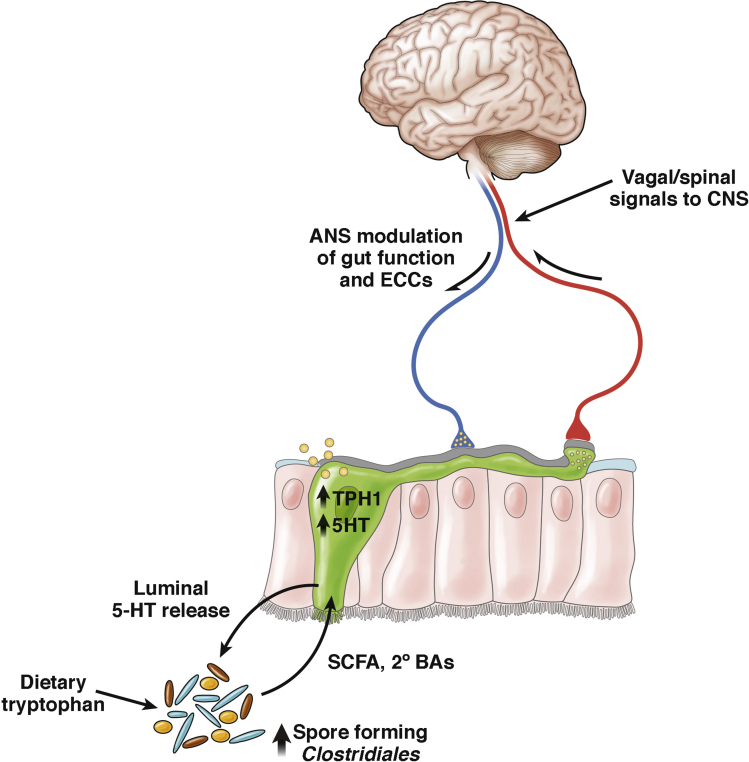
One of the best characterized examples of these microbial host interactions is the bidirectional interaction between microbes, ECCs, and the central nervous system (Figure 1). 5-HT is produced by the ECCs of the gastrointestinal (GI) tract, with 95% of the body’s 5-HT stored in ECCs and enteric neurons, and only 5% stored in the CNS.96 Considering 5-HT’s central role in regulating GI motility and secretion, there is likely immense selective pressure on the gut microorganisms to act on the serotonergic system to modulate their environment effectively (eg, by influencing regional transit times and fluid secretions). An analysis of the plasma metabolite profile of germ-free mice shows a more than 2-fold decrease in 5-HT levels relative to conventionally colonized mice.69 SCFAs and 2BAs derived from spore-forming bacteria of the gut regulate a significant percentage of ECC 5-HT synthesis and release.68 The essential amino acid tryptophan (Trp) is a key molecule in the BGM axis because it is the precursor to the neurotransmitter 5-HT and a number of other metabolites that contribute to the neuroendocrine signaling within the BGM.97 Because the host is unable to produce tryptophan, dietary intake of proteins that contain it serve as the primary regulator of its availability. Gut microbiota contribute to the peripheral availability of Trp, which is imperative to the CNS synthesis of 5-HT. GF mice show increased levels of plasma Trp and hippocampal 5-HT, and, interestingly, colonization with bacteria normalizes plasma Trp but not hippocampal 5-HT.21 Although the exact mechanisms of peripheral Trp regulation are unknown, the same study suggests that the microbiota modulate the degradation of Trp down the kynurenine pathway. In a separate study, this pathway interaction was observed and linked to behavioral phenotypes. Administration of Lactobacillus reuteri normalized stress-induced behavioral changes and was associated with decreased circulating kynurenine levels resulting from microbially derived H2O2 inhibition of ido1 messenger RNA expression.98
Figure 1.
Bidirectional brain-gut-microbiome interactions related to serotonin signaling. Enterochromaffin cells (shown in green) contain more than 90% of the body’s serotonin (5-HT). 5-HT synthesis in ECCs is modulated by SCFAs and 2BAs produced by spore-forming Clostridiales, which increase their stimulatory actions on ECCs with increased dietary tryptophan availability.68 ECCs communicate with afferent nerve fibers through synapse-like connections between neuropod-like extensions and afferent nerve terminals.192 The autonomic nervous system can activate ECCs to release 5-HT into the gut lumen, where it can interact with gut microbes.155 TPH1, tryptophan hydroxylase type 1.
Neuroimmune Signaling
The wide-ranging interaction of commensal bacteria with the gut-associated immune system and consequently the CNS is beyond the scope of this review and has been reviewed extensively elsewhere.99 Mouse models of multiple sclerosis and stroke have identified substantial roles for gut microbial regulation of autoimmunity, inflammation, and immune cell trafficking.66, 100, 101, 102, 103 It is important to highlight that the gut microbiota influence the development and function of the CNS resident immune cells, especially microglia.104 Relative to SPF mice, GF mice have compromised microglia maturation and morphology, leading to weakened early responses to pathogen exposure.104 This phenotype can be normalized by postnatal SCFA supplementation or colonization with a complex microbial community. Remarkably, antibiotic treatment to eradicate bacteria in SPF adult mice leads microglia to regain immature status, which then can be normalized by recolonization with complex microbiota, suggesting that active microbial signaling is required throughout adulthood to preserve microglial maturation.104
Direct Neural Signaling
Most evidence to date relies on vagal receptors that sense regulatory gut peptides, inflammatory molecules, dietary components, and bacterial metabolites to relay signals to the CNS,105 but there is also some evidence for direct activation of neurons by gut microbiota. Toll-like receptors 3 and 7, which recognize viral RNA, and Toll-like receptors 2 and 4, which recognize peptidoglycan and lipopolysaccharide, are expressed in the murine and human enteric nervous systems.106, 107 L rhamnosus (JB-1), B fragilis, and isolated polysaccharide A of B fragilis all have been shown to activate intestinal afferent neurons ex vivo.108 However, it remains unclear to what degree luminal microbial antigens make direct physical contact with neurons in vivo.109
Microbial metabolites also are likely candidates mediating direct activation of neurons. The receptors FXR and TGR5 are expressed in brain neurons, but bile acid concentrations are low or undetectable in these tissues of healthy subjects.110, 111 Several studies have localized GPR41/FFAR3 receptors to the superior cervical ganglion,112 prevertebral ganglia,113 submucosal and myenteric ganglia neurons,114 sympathetic ganglia of the thoracic and lumbar sympathetic trunks, and vagal ganglion,95 suggesting neuronal activation by microbially derived SCFAs. Upon GPR41 activation, primary-cultured superior cervical neurons release norepinephrine, establishing this as a direct functional interface for microbial derivatives and the sympathetic nervous system.112
Barriers to Bottom-Up Signaling
There are 2 natural barriers to signaling within the BGM axis: the intestinal barrier and the blood brain barrier. Because gut microbes, stress, and inflammation are able to modulate the permeability of both structures, the amount of information reaching the brain from the gut is highly variable, depending on the state of the host.
Intestinal Barrier
The intestinal barrier is characterized by 2 layers: a basal monolayer of epithelial cells interconnected by tight junctions, and a mucus layer whose thickness and composition changes over time and that contains secretory IgA and antimicrobial peptides.115 Upon detection of specific microbial products, pattern recognition receptors located throughout GI mucosa can mediate the induction of enhanced antimicrobial defense, intestinal inflammation, and even immunologic tolerance.116, 117 Under healthy homeostatic conditions, many microorganisms and macromolecules gain entry through microfold cells (M cells), found in gut- and mucosa-associated lymphoid tissue, which enables constant sampling by immune cells.118 Paneth cells autonomously sense bacteria though MyD88-dependent Toll-like receptor activation, which triggers antimicrobial factors and ultimately limits bacterial penetration of host tissue.119 Microbes and microbe-derived ligands help maintain the cell-cell junctions critical to integrity.120, 121 Probiotic treatment can help normalize stress-induced barrier defects (discussed later) via unknown mechanisms.122
The intestinal mucus layer is the second component of intestinal barrier function. Colonic mucus is organized into 2 layers: a thicker loose outer layer, and an inner layer attached firmly to the epithelium.123 Commensal microbes inhabit the outer layer, a critical habitat for biofilm formation,124 and a reliable energy source rich in glycoproteins that the microbiota degrade when deprived of dietary fiber, subsequently increasing pathogen susceptibility.11 The inner layer usually is bacteria-free and serves to protect epithelial cells from microbial contact through physical separation, innate immune mechanisms including antimicrobial peptides, and adaptive immune mechanisms including secretory IgA.125
Blood-Brain Barrier
The blood-brain barrier (BBB) regulates molecular traffic between the circulatory system and the cerebrospinal fluid of the CNS. Gut microbiota can up-regulate the expression of tight junction proteins, including occludin and claudin-5, therefore decreasing BBB permeability.126 From intrauterine life through adulthood, GF mice have a more permeable barrier compared with controls, but introduction of normal gut microbiota to GF adults partially restores function. Permeability is decreased by monocolonization with SCFA-producing bacteria and oral gavage with sodium butyrate. SCFAs may serve as the primary signaling metabolite in BBB development and maintenance likely via entering cells and working as histone deacetylase inhibitors to epigenetically modulate the phenotype or via binding to GPR41 and/or GPR43.127, 128
Systemic immune activation may cause disruptive BBB changes and often is modeled using LPS. But in a systematic review, studies evaluating in vivo LPS effects on BBB function only showed disruption 60% of the time, a figure potentially subject to publication bias.129 Interestingly, the host species is the only significant predictor explaining variance: mice are 4 times more likely than rats to show BBB change. Dose-dependent effects were not observed across all studies, although the levels used were mostly equivalent to septic doses. The variability of the BBB response in this model of systemic immune activation limits the generalizability of most preclinical findings to human microbiome interactions, especially in nonpathologic conditions.
Signaling From the Brain to the Gut Microbiota
There is more than 40 years worth of literature showing the effect of stress on the community structure of the gut microbiome.130, 131 Exposure to social stressors for as little as 2 hours can change community profiles and reduce the relative proportions of the primary phyla,132 and maternal prenatal stress is associated with an altered infant microbiome potentiating increased inflammation.133
Indirect Modulation via Autonomic Nervous System–Mediated Change in Microbial Environment
Both branches of the autonomic nervous system (ANS) regulate gut functions including regional motility, secretion of gastric acid, mucus, bicarbonate, gut peptides, antimicrobial peptides, epithelial fluid maintenance, intestinal permeability, and mucosal immune response (reviewed by Mayer1). These ANS-induced changes in gut physiology affect the microbial habitat, thereby modulating microbiota composition and activity.
GI Motility
Regional intestinal transit times affect water content, nutrient availability, and bacterial clearance rates. Relatively rapid flow in the small intestine inhibits permanent colonization of the upper gut, in particular in the proximal small intestine.124 The frequency of migrating motor complexes, which play a crucial role in intestinal transit during the fasting state, is influenced by food intake patterns, sleep quality, and stress. Impaired migrating motor complex regularity can reduce the flow rate, leading to small intestine bacterial overgrowth.134 Intestinal transit time assessed by the Bristol Stool Scale135, 136 strongly correlates with microbial richness and composition.137 In fact, a microbiome population level analysis identified such transit ratings as the top nonredundant covariate.138 A study using radiopaque markers for transit corroborated its association to microbial composition and additionally showed association with diversity and metabolism.139 In vitro simulation with Environmental Controls Systems for Intestinal Microbiota showed that increased transit time causally reduced bacterial biomass and diversity in distal gut regions.140
Intestinal Barrier
Stress can cause epithelial barrier defects (leaky gut) by at least 2 mechanisms: direct modulation of epithelial permeability and alterations in the properties of the intestinal mucosal layer, ultimately leading to increased translocation of gut microbes or microbe-associated molecules.141 Rodent models have shown that jejunal and colonic permeability increases in response to both acute and chronic stress.142, 143 This increased leakiness facilitates the translocation of bacteria, such as Escherichia coli, and their products, such as lipopolysaccharide (LPS), leading to a proinflammatory environment in the gut, although there are conflicting reports describing stress-induced changes in expression of messenger RNA encoding tight junction proteins in the colon and jejunum.144, 145 Increased intestinal permeability and susceptibility to experimental inflammation observed in mouse models of depressive behavior induced by maternal separation is reversed by antidepressant therapy, highlighting brain-driven systemic and epithelial immune activity regulating the gut.146
The ANS modulates the secretion of mucus by intestinal goblet cells, affecting the thickness and quality of the intestinal mucus layer. In addition to hypersensitivity, psychological stress leads to a less-protective mucus layer via catecholamine signaling, which alters the composition and size of secreted mucus.122, 147, 148 Changes in microbiota composition observed in a mouse model of brain injury are thought to result from altered mucoprotein production and goblet cell population size mediated by increased sympathetic nervous system signaling.149, 150
Direct Modulation of Gut Microbiota by Luminal Release of Neurotransmitters
In addition to CNS-induced changes in the intestinal microbial environment (eg, by influencing regional transit and secretions), the host neuroendocrine system can communicate with the microbiota more directly via intraluminal release of host signaling molecules, including but not limited to catecholamines, 5-HT, dynorphin, and cytokines, from neurons, immune cells, and ECCs.151, 152 The CNS likely modulates this process.153, 154, 155 Epinephrine and norepinephrine are shown to increase the virulence properties of several enteric pathogens as well as nonpathogenic microbes via stimulation of native quorum-sensing mechanisms.156, 157, 158, 159, 160 Other gut microbes contain sequences that share 24% to 42% identity to human genome sequences for the binding sites of melatonin,161 whose gut luminal concentrations have been reported at more than 10-fold serum concentrations in rats and pigs.162, 163 In vitro assays of one such microbe, Enterobacter aerogenes, show that melatonin not only induces swarming and motility behavior, but helps synchronize the circadian period and phase across culture plates.161 The gut microbiota show circadian rhythmicity in both abundance and expression in a manner dependent on the host and its behavior, especially feeding timing, and simulated jet-lag shifts composition, enhancing dysbiosis.164
The BGM Axis in GI and Metabolic Disorders
Functional Intestinal Disorders
A number of studies (n = 22 in a total of 827 subjects) have reported significant microbial shifts in fecal microbial community composition between healthy controls and IBS patients, based on disease subtypes (diarrhea-predominant IBS, constipation-predominant IBS, and IBS mixed type), age (pediatric vs adult), and compartment (mucosa vs stool).165 Recent studies have suggested that there are at least 2 subgroups of patients who meet Rome criteria for IBS, based on gut microbial community structure, 1 subgroup not differing from healthy control subjects, despite similar GI symptoms.166, 167 In one of these studies, the dysbiotic IBS subgroup also differed in regional brain volumes from the eubiotic group,166 suggesting a relationship between microbial community structure and brain structure. Another recent study did not find a group difference in microbial composition between HCs and IBS, even though IBS symptom severity was correlated with dysbiosis.168 Despite a lack of consensus on the wide range of gut microbial differences between IBS subjects and healthy controls and the specific microbial changes that may be correlated to disease outcome, recent molecular-based methods of mucosal brushings or luminal aspirates have suggested decreased diversity in small-bowel microbiota with increased abundance of gram-negative organisms in IBS.169, 170 Based on analysis of fecal samples, regardless of the analytical methodology used, a number of studies reported a decreased relative abundance of the genera Bifidobacterium and Lactobacillus, and an increased Firmicutes:Bacteroidetes ratios at the phylum level. Because stress has been associated with a reduction in Lactobacilli in preclinical and clinical studies,132, 171, 172 one may speculate that the reported IBS-related changes in community structure and resulting metabolism are in part owing to altered ANS modulation of the gut as described earlier.
Obesity/Food Addiction
A dysregulation of hedonic feeding behavior (food addiction) plays an important role in the current obesity epidemic.173 The gut microbiota and its metabolites play an crucial role in the modulation of satiety signals (see earlier) and eating behaviors.65, 174, 175 In preclinical studies, fecal transplantation from hyperphagic obese mice to germ-free mice was able to induce hyperphagic behavior and weight gain in the recipients.39, 176 In addition, the gut microbiome has been associated with changes in brain microstructure in obesity, and distinct microbial brain signatures were able to differentiate obese from lean subjects.177 The gut microbiome produces several neuroactive compounds; these bioactive products include several indole-containing metabolites and 5-HT. The administration of probiotics modifies brain function and even brain metabolites including γ-aminobutyric acid and glutamate.59, 178 A handful of studies point to a dramatic change in gut microbial composition after bariatric surgery.179, 180, 181, 182, 183 Remarkably, fecal transplantation from subjects after bariatric surgery was able to transmit the weight loss effects of bariatric surgery to a germ-free nonoperated recipient, inducing weight loss and reduced food intake.184, 185
The BGM Axis in Psychiatric and Neurologic Disorders With GI Comorbidities
Patients with several psychiatric (depression, anxiety) and neurologic disorders (Parkinson's disease, autism spectrum disorders) have significant gastrointestinal comorbidities, and several recent studies point to an important role of the gut microbiota not only in the pathophysiology of the GI symptoms, but a potential role in the primary disorder as well.
Depression and Anxiety
Anxiety and depression often are comorbid conditions in patients with IBS. Preclinical studies have shown the microbiota’s capacity to modulate emotional behaviors, and influence parameters significant to depression pathogenesis and severity.17, 18, 19, 21, 186 Although studies characterizing the gut microbiome of major depressive disorder vs health have yielded marginally distinct assemblage correlations, 3 different types of studies suggest causality: depressed human-to-rodent fecal microbial transplants have induced depressive behaviors in the animal models27, 32; prebiotic and probiotic administration to healthy controls has improved anxiety and mood; and, finally, incidences of E coli subtype outbreaks in Canada and Germany led to increases in depression and anxiety-related symptoms among the affected population (reviewed by Kelly et al186).
Parkinson’s Disease
Although the clinical hallmarks of Parkinson's disease remain motor deficits, gastrointestinal symptoms (in addition to other nonmotor symptoms) are present that contribute more detrimentally to patient quality of life. These nonmotor symptoms include problems related to dysfunctional autonomic and enteric nervous systems, such as slow-transit constipation, and sensory alterations. The risk of Parkinson's disease development increases with infrequency of bowel movement and constipation severity, and there is a significant comorbidity of Parkinson's disease and IBS-like symptoms.187 Moreover, constipation is among the earliest features, appearing as early as 15.3 years before motor dysfunction (reviewed by Fasano et al188). To date, clinical studies of Parkinson’s and the gut microbiota remain limited to characterizing the assemblage differences against healthy controls, and some of the reported differences may be a consequence of impaired colonic transit. However, recent evidence showing that a Parkinson’s rodent model’s physical impairments are enhanced by microbiota from Parkinson’s patients but not healthy controls suggests causality.6 Early gastrointestinal symptoms, thus, may be prodromal, making the gut microbiota a promising source of information for diagnosis, prognosis, and, potentially, pathogenesis.
Autism Spectrum Disorder
In addition to the core symptoms of ASD (difficulty with social and communicative behavior, repetitive behaviors), gastrointestinal symptoms are common and contribute significantly to the morbidity of affected patients.5, 189 GI symptom severity is correlated strongly to ASD symptom severity, as well as anxiety and sensory over-responsivity conditions modulated by gut microbiota in preclinical models (reviewed by Vuong and Hsiao5). Gut dysbiosis is an increasingly documented symptom of ASD but, similar to other clinical conditions, causality remains limited to intriguing, albeit untested, hypotheses and results from uncontrolled clinical studies.190
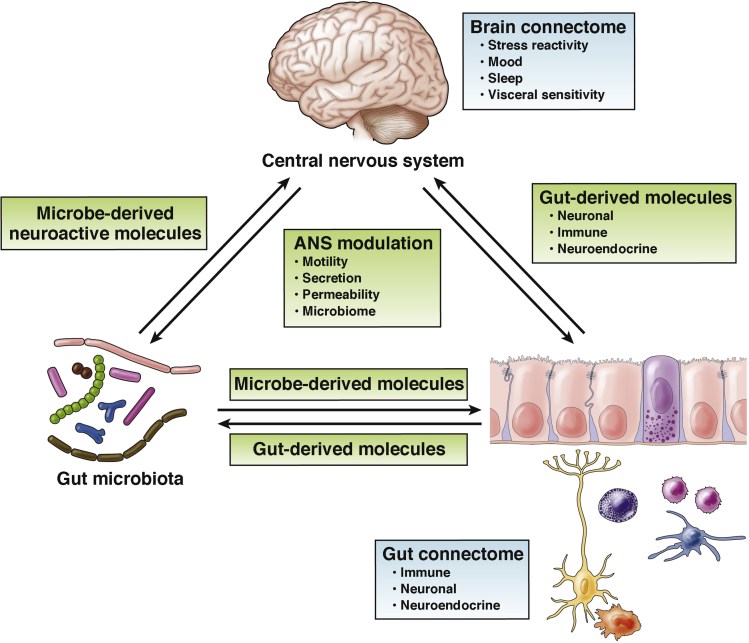
In summary, there is considerable and growing evidence implicating the gut microbiome not only in the normal development and function of the nervous system but also in a range of acute and chronic diseases affecting the gut, as well as the nervous system throughout life. It remains to be determined if the gut microbiota play a causal role, but its facilitation of pathogenesis and potentiation of severity in disease models suggests that it is not merely a secondary effect of the underlying etiology. In view of the extensive preclinical evidence for both top-down and bottom-up signaling within the BGM axis and the emerging findings from clinical studies, we propose a systems biological model of bidirectional BGM interactions191 (Figure 2).
Figure 2.
Systems biological model of brain-gut-microbiome interactions. The gut microbiota communicate with the gut connectome, the network of interacting cell types in the gut that include neuronal, glial, endocrine, and immune cells,192 via microbial metabolites, while changes in gut function can modulate gut microbial behavior. The brain connectome, the multiple interconnected structural networks of the central nervous system,193 generates and regulates autonomic nervous system influences that alter gut microbial composition and function indirectly by modulating the microbial environment in the gut. The gut microbiota can communicate to the brain indirectly via gut-derived molecules acting on afferent vagal and/or spinal nerve endings, or directly via microbe-generated signals. Alterations in the gain of these bidirectional interactions in response to perturbations such as psychosocial or gut-directed (eg, diet, medication, infection) stress can alter the stability and behavior of this system, manifesting as brain-gut disorders. Modified from Fung et al.99
Future
Despite considerable progress characterizing the interaction between the gut microbiome and the CNS over the past 10 years, questions remain regarding their relevance to the pathogenesis, pathophysiology, and treatment of human brain gut disorders and we urge caution in prematurely extrapolating findings in rodent models to human beings. For example, based on clinical experience, long-term treatment with broad-spectrum antibiotics for infectious diseases and total colectomy in ulcerative colitis do not appear to have noticeable effects on mood, affect, or cognition in the vast number of patients. Advances in the field are the consequence of ever-more-powerful biological techniques, such as shotgun metagenomics and metatranscriptomics, coupled to novel bioinformatic and computational approaches that enable multi-omic integration of both microbial and host data using machine learning approaches. Efforts are underway not only to characterize further microbial community structure, function, and the contributions of individual taxa, but also the large communities of viruses (virome) and fungi (mycobiome) that, until recently, have been ignored owing to technological limitations. The decreasing costs of novel multi-omic analysis have facilitated data-driven approaches to identify patient subgroups with distinct patterns of dysbiosis and test the hypothesis that such subgroups will respond to personalized therapy using dietary, prebiotic, or probiotic interventions. However, there is an urgent need for large-scale, highly controlled, longitudinal human studies showing the causes and sequelae of dysbiotic gut states and explaining interindividual variability in susceptibility to BGM-related diseases. The past decade has shown a potent hidden organ. This next decade will see widespread inclusion of this newly discovered organ into diagnostic consideration and in targeted manipulation for therapeutic intervention of many diseases.
Footnotes
Author contributions Clair R. Martin played a key role in the concept development, literature review, and writing of the manuscript; Emeran A. Mayer worked on the concept development and drafted the manuscript; and Vadim Osadchiy and Amir Kalani performed the literature review.
Conflicts of interest This author discloses the following: Emeran A. Mayer serves on the scientific advisory boards of Danone, Viome, Axial Biotherapeutic, Whole Biome Prolacta, Amare, Bloom Science and Pharmavite. The remaining authors disclose no conflicts.
Funding Supported by grants DK048351 (EAM) and DK064539 (EAM) and DK041301 (ER) from the National Institute of Diabetes and Digestive and Kidney Diseases.
References
- 1.Mayer E.A. Gut feelings: the emerging biology of gut-brain communication. Nat Rev Neurosci. 2011;12:453–466. doi: 10.1038/nrn3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhee S.H., Pothoulakis C., Mayer E.A. Principles and clinical implications of the brain-gut-enteric microbiota axis. Nat Rev Gastroenterol Hepatol. 2009;6:306–314. doi: 10.1038/nrgastro.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cryan J.F., Dinan T.G. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 2012;13:701–712. doi: 10.1038/nrn3346. [DOI] [PubMed] [Google Scholar]
- 4.Park A.J., Collins J., Blennerhassett P.A., Ghia J.E., Verdu E.F., Bercik P., Collins S.M. Altered colonic function and microbiota profile in a mouse model of chronic depression. Neurogastroenterol Motil. 2013;25 doi: 10.1111/nmo.12153. 733-e575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vuong H.E., Hsiao E.Y. Emerging roles for the gut microbiome in autism spectrum disorder. Biol Psychiatry. 2017;81:411–423. doi: 10.1016/j.biopsych.2016.08.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sampson T.R., Debelius J.W., Thron T., Janssen S., Shastri G.G., Ilhan Z.E., Challis C., Schretter C.E., Rocha S., Gradinaru V., Chesselet M.F., Keshavarzian A., Shannon K.M., Krajmalnik-Brown R., Wittung-Stafshede P., Knight R., Mazmanian S.K. Gut microbiota regulate motor deficits and neuroinflammation in a model of Parkinson's disease. Cell. 2016;167:1469–1480 e12. doi: 10.1016/j.cell.2016.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berer K., Mues M., Koutrolos M., Rasbi Z.A., Boziki M., Johner C., Wekerle H., Krishnamoorthy G. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature. 2011;479:538–541. doi: 10.1038/nature10554. [DOI] [PubMed] [Google Scholar]
- 8.Amaral F.A., Sachs D., Costa V.V., Fagundes C.T., Cisalpino D., Cunha T.M., Ferreira S.H., Cunha F.Q., Silva T.A., Nicoli J.R., Vieira L.Q., Souza D.G., Teixeira M.M. Commensal microbiota is fundamental for the development of inflammatory pain. Proc Natl Acad Sci U S A. 2008;105:2193–2197. doi: 10.1073/pnas.0711891105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bercik P., Denou E., Collins J., Jackson W., Lu J., Jury J., Deng Y., Blennerhassett P., Macri J., McCoy K.D., Verdu E.F., Collins S.M. The intestinal microbiota affect central levels of brain-derived neurotropic factor and behavior in mice. Gastroenterology. 2011;141:599–609. doi: 10.1053/j.gastro.2011.04.052. e1-3. [DOI] [PubMed] [Google Scholar]
- 10.Collins S.M., Kassam Z., Bercik P. The adoptive transfer of behavioral phenotype via the intestinal microbiota: experimental evidence and clinical implications. Curr Opin Microbiol. 2013;16:240–245. doi: 10.1016/j.mib.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Desai M.S., Seekatz A.M., Koropatkin N.M., Kamada N., Hickey C.A., Wolter M., Pudlo N.A., Kitamoto S., Terrapon N., Muller A., Young V.B., Henrissat B., Wilmes P., Stappenbeck T.S., Nunez G., Martens E.C. A dietary fiber-deprived gut microbiota degrades the colonic mucus barrier and enhances pathogen susceptibility. Cell. 2016;167:1339–1353 e21. doi: 10.1016/j.cell.2016.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bowey E., Adlercreutz H., Rowland I. Metabolism of isoflavones and lignans by the gut microflora: a study in germ-free and human flora associated rats. Food Chem Toxicol. 2003;41:631–636. doi: 10.1016/s0278-6915(02)00324-1. [DOI] [PubMed] [Google Scholar]
- 13.Mallett A.K., Bearne C.A., Rowland I.R., Farthing M.J., Cole C.B., Fuller R. The use of rats associated with a human faecal flora as a model for studying the effects of diet on the human gut microflora. J Appl Bacteriol. 1987;63:39–45. doi: 10.1111/j.1365-2672.1987.tb02415.x. [DOI] [PubMed] [Google Scholar]
- 14.Bellono N.W., Bayrer J.R., Leitch D.B., Castro J., Zhang C., O'Donnell T.A., Brierley S.M., Ingraham H.A., Julius D. Enterochromaffin cells are gut chemosensors that couple to sensory neural pathways. Cell. 2017;170:185–198 e16. doi: 10.1016/j.cell.2017.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yissachar N., Zhou Y., Ung L., Lai N.Y., Mohan J.F., Ehrlicher A., Weitz D.A., Kasper D.L., Chiu I.M., Mathis D., Benoist C. An intestinal organ culture system uncovers a role for the nervous system in microbe-immune crosstalk. Cell. 2017;168:1135–1148 e12. doi: 10.1016/j.cell.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bravo J.A., Forsythe P., Chew M.V., Escaravage E., Savignac H.M., Dinan T.G., Bienenstock J., Cryan J.F. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc Natl Acad Sci U S A. 2011;108:16050–16055. doi: 10.1073/pnas.1102999108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sudo N., Chida Y., Aiba Y., Sonoda J., Oyama N., Yu X.N., Kubo C., Koga Y. Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol. 2004;558:263–275. doi: 10.1113/jphysiol.2004.063388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Neufeld K.M., Kang N., Bienenstock J., Foster J.A. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol Motil. 2011;23:255–264. doi: 10.1111/j.1365-2982.2010.01620.x. e119. [DOI] [PubMed] [Google Scholar]
- 19.Diaz Heijtz R., Wang S., Anuar F., Qian Y., Bjorkholm B., Samuelsson A., Hibberd M.L., Forssberg H., Pettersson S. Normal gut microbiota modulates brain development and behavior. Proc Natl Acad Sci U S A. 2011;108:3047–3052. doi: 10.1073/pnas.1010529108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Desbonnet L., Garrett L., Clarke G., Kiely B., Cryan J.F., Dinan T.G. Effects of the probiotic Bifidobacterium infantis in the maternal separation model of depression. Neuroscience. 2010;170:1179–1188. doi: 10.1016/j.neuroscience.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Clarke G., Grenham S., Scully P., Fitzgerald P., Moloney R.D., Shanahan F., Dinan T.G., Cryan J.F. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry. 2013;18:666–673. doi: 10.1038/mp.2012.77. [DOI] [PubMed] [Google Scholar]
- 22.Bercik P., Park A.J., Sinclair D., Khoshdel A., Lu J., Huang X., Deng Y., Blennerhassett P.A., Fahnestock M., Moine D., Berger B., Huizinga J.D., Kunze W., McLean P.G., Bergonzelli G.E., Collins S.M., Verdu E.F. The anxiolytic effect of Bifidobacterium longum NCC3001 involves vagal pathways for gut-brain communication. Neurogastroenterol Motil. 2011;23:1132–1139. doi: 10.1111/j.1365-2982.2011.01796.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crumeyrolle-Arias M., Jaglin M., Bruneau A., Vancassel S., Cardona A., Dauge V., Naudon L., Rabot S. Absence of the gut microbiota enhances anxiety-like behavior and neuroendocrine response to acute stress in rats. Psychoneuroendocrinology. 2014;42:207–217. doi: 10.1016/j.psyneuen.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 24.Savignac H.M., Kiely B., Dinan T.G., Cryan J.F. Bifidobacteria exert strain-specific effects on stress-related behavior and physiology in BALB/c mice. Neurogastroenterol Motil. 2014;26:1615–1627. doi: 10.1111/nmo.12427. [DOI] [PubMed] [Google Scholar]
- 25.De Palma G., Blennerhassett P., Lu J., Deng Y., Park A.J., Green W., Denou E., Silva M.A., Santacruz A., Sanz Y., Surette M.G., Verdu E.F., Collins S.M., Bercik P. Microbiota and host determinants of behavioural phenotype in maternally separated mice. Nat Commun. 2015;6:7735. doi: 10.1038/ncomms8735. [DOI] [PubMed] [Google Scholar]
- 26.Hsiao E.Y., McBride S.W., Hsien S., Sharon G., Hyde E.R., McCue T., Codelli J.A., Chow J., Reisman S.E., Petrosino J.F., Patterson P.H., Mazmanian S.K. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013;155:1451–1463. doi: 10.1016/j.cell.2013.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelly J.R., Borre Y., C OB, Patterson E., El Aidy S., Deane J., Kennedy P.J., Beers S., Scott K., Moloney G., Hoban A.E., Scott L., Fitzgerald P., Ross P., Stanton C., Clarke G., Cryan J.F., Dinan T.G. Transferring the blues: depression-associated gut microbiota induces neurobehavioural changes in the rat. J Psychiatr Res. 2016;82:109–118. doi: 10.1016/j.jpsychires.2016.07.019. [DOI] [PubMed] [Google Scholar]
- 28.Desbonnet L., Clarke G., Traplin A., O'Sullivan O., Crispie F., Moloney R.D., Cotter P.D., Dinan T.G., Cryan J.F. Gut microbiota depletion from early adolescence in mice: implications for brain and behaviour. Brain Behav Immun. 2015;48:165–173. doi: 10.1016/j.bbi.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Schroeder F.A., Lin C.L., Crusio W.E., Akbarian S. Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse. Biol Psychiatry. 2007;62:55–64. doi: 10.1016/j.biopsych.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 30.Desbonnet L., Garrett L., Clarke G., Bienenstock J., Dinan T.G. The probiotic Bifidobacteria infantis: an assessment of potential antidepressant properties in the rat. J Psychiatr Res. 2008;43:164–174. doi: 10.1016/j.jpsychires.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 31.Arseneault-Breard J., Rondeau I., Gilbert K., Girard S.A., Tompkins T.A., Godbout R., Rousseau G. Combination of Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 reduces post-myocardial infarction depression symptoms and restores intestinal permeability in a rat model. Br J Nutr. 2012;107:1793–1799. doi: 10.1017/S0007114511005137. [DOI] [PubMed] [Google Scholar]
- 32.Zheng P., Zeng B., Zhou C., Liu M., Fang Z., Xu X., Zeng L., Chen J., Fan S., Du X., Zhang X., Yang D., Yang Y., Meng H., Li W., Melgiri N.D., Licinio J., Wei H., Xie P. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host's metabolism. Mol Psychiatry. 2016;21:786–796. doi: 10.1038/mp.2016.44. [DOI] [PubMed] [Google Scholar]
- 33.Ait-Belgnaoui A., Han W., Lamine F., Eutamene H., Fioramonti J., Bueno L., Theodorou V. Lactobacillus farciminis treatment suppresses stress induced visceral hypersensitivity: a possible action through interaction with epithelial cell cytoskeleton contraction. Gut. 2006;55:1090–1094. doi: 10.1136/gut.2005.084194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eutamene H., Lamine F., Chabo C., Theodorou V., Rochat F., Bergonzelli G.E., Corthesy-Theulaz I., Fioramonti J., Bueno L. Synergy between Lactobacillus paracasei and its bacterial products to counteract stress-induced gut permeability and sensitivity increase in rats. J Nutr. 2007;137:1901–1907. doi: 10.1093/jn/137.8.1901. [DOI] [PubMed] [Google Scholar]
- 35.Rousseaux C., Thuru X., Gelot A., Barnich N., Neut C., Dubuquoy L., Dubuquoy C., Merour E., Geboes K., Chamaillard M., Ouwehand A., Leyer G., Carcano D., Colombel J.F., Ardid D., Desreumaux P. Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med. 2007;13:35–37. doi: 10.1038/nm1521. [DOI] [PubMed] [Google Scholar]
- 36.Ma X., Mao Y.K., Wang B., Huizinga J.D., Bienenstock J., Kunze W. Lactobacillus reuteri ingestion prevents hyperexcitability of colonic DRG neurons induced by noxious stimuli. Am J Physiol Gastrointest Liver Physiol. 2009;296:G868–G875. doi: 10.1152/ajpgi.90511.2008. [DOI] [PubMed] [Google Scholar]
- 37.Kunze W.A., Mao Y.K., Wang B., Huizinga J.D., Ma X., Forsythe P., Bienenstock J. Lactobacillus reuteri enhances excitability of colonic AH neurons by inhibiting calcium-dependent potassium channel opening. J Cell Mol Med. 2009;13:2261–2270. doi: 10.1111/j.1582-4934.2009.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duca F.A., Swartz T.D., Sakar Y., Covasa M. Increased oral detection, but decreased intestinal signaling for fats in mice lacking gut microbiota. PLoS One. 2012;7:e39748. doi: 10.1371/journal.pone.0039748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vijay-Kumar M., Aitken J.D., Carvalho F.A., Cullender T.C., Mwangi S., Srinivasan S., Sitaraman S.V., Knight R., Ley R.E., Gewirtz A.T. Metabolic syndrome and altered gut microbiota in mice lacking Toll-like receptor 5. Science. 2010;328:228–231. doi: 10.1126/science.1179721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanida M., Yamano T., Maeda K., Okumura N., Fukushima Y., Nagai K. Effects of intraduodenal injection of Lactobacillus johnsonii La1 on renal sympathetic nerve activity and blood pressure in urethane-anesthetized rats. Neurosci Lett. 2005;389:109–114. doi: 10.1016/j.neulet.2005.07.036. [DOI] [PubMed] [Google Scholar]
- 41.Mayer E.A., Tillisch K., Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125:926–938. doi: 10.1172/JCI76304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mayer E.A., Knight R., Mazmanian S.K., Cryan J.F., Tillisch K. Gut microbes and the brain: paradigm shift in neuroscience. J Neurosci. 2014;34:15490–15496. doi: 10.1523/JNEUROSCI.3299-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bercik P., Collins S.M., Verdu E.F. Microbes and the gut-brain axis. Neurogastroenterol Motil. 2012;24:405–413. doi: 10.1111/j.1365-2982.2012.01906.x. [DOI] [PubMed] [Google Scholar]
- 44.Martin C.R., Mayer E.A. Gut-brain axis and behavior. Nestle Nutr Inst Workshop Ser. 2017;88:45–53. doi: 10.1159/000461732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sharon G., Sampson T.R., Geschwind D.H., Mazmanian S.K. The central nervous system and the gut microbiome. Cell. 2016;167:915–932. doi: 10.1016/j.cell.2016.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Grill M.F., Maganti R.K. Neurotoxic effects associated with antibiotic use: management considerations. Br J Clin Pharmacol. 2011;72:381–393. doi: 10.1111/j.1365-2125.2011.03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohle L., Mattei D., Heimesaat M.M., Bereswill S., Fischer A., Alutis M., French T., Hambardzumyan D., Matzinger P., Dunay I.R., Wolf S.A. Ly6C(hi) monocytes provide a link between antibiotic-induced changes in gut microbiota and adult hippocampal neurogenesis. Cell Rep. 2016;15:1945–1956. doi: 10.1016/j.celrep.2016.04.074. [DOI] [PubMed] [Google Scholar]
- 48.Messaoudi M., Lalonde R., Violle N., Javelot H., Desor D., Nejdi A., Bisson J.F., Rougeot C., Pichelin M., Cazaubiel M., Cazaubiel J.M. Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. Br J Nutr. 2011;105:755–764. doi: 10.1017/S0007114510004319. [DOI] [PubMed] [Google Scholar]
- 49.Kantak P.A., Bobrow D.N., Nyby J.G. Obsessive-compulsive-like behaviors in house mice are attenuated by a probiotic (Lactobacillus rhamnosus GG) Behav Pharmacol. 2014;25:71–79. doi: 10.1097/FBP.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 50.D'Mello C., Ronaghan N., Zaheer R., Dicay M., Le T., MacNaughton W.K., Surrette M.G., Swain M.G. Probiotics improve inflammation-associated sickness behavior by altering communication between the peripheral immune system and the brain. J Neurosci. 2015;35:10821–10830. doi: 10.1523/JNEUROSCI.0575-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cowan C.S., Callaghan B.L., Richardson R. The effects of a probiotic formulation (Lactobacillus rhamnosus and L. helveticus) on developmental trajectories of emotional learning in stressed infant rats. Transl Psychiatry. 2016;6:e823. doi: 10.1038/tp.2016.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.David L.A., Maurice C.F., Carmody R.N., Gootenberg D.B., Button J.E., Wolfe B.E., Ling A.V., Devlin A.S., Varma Y., Fischbach M.A., Biddinger S.B., Dutton R.J., Turnbaugh P.J. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carmody R.N., Gerber G.K., Luevano J.M., Jr., Gatti D.M., Somes L., Svenson K.L., Turnbaugh P.J. Diet dominates host genotype in shaping the murine gut microbiota. Cell Host Microbe. 2015;17:72–84. doi: 10.1016/j.chom.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turnbaugh P.J., Ridaura V.K., Faith J.J., Rey F.E., Knight R., Gordon J.I. The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med. 2009;1:6ra14. doi: 10.1126/scitranslmed.3000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li W., Dowd S.E., Scurlock B., Acosta-Martinez V., Lyte M. Memory and learning behavior in mice is temporally associated with diet-induced alterations in gut bacteria. Physiol Behav. 2009;96:557–567. doi: 10.1016/j.physbeh.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 56.Jorgensen B.P., Hansen J.T., Krych L., Larsen C., Klein A.B., Nielsen D.S., Josefsen K., Hansen A.K., Sorensen D.B. A possible link between food and mood: dietary impact on gut microbiota and behavior in BALB/c mice. PLoS One. 2014;9:e103398. doi: 10.1371/journal.pone.0103398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beilharz J.E., Kaakoush N.O., Maniam J., Morris M.J. Cafeteria diet and probiotic therapy: cross talk among memory, neuroplasticity, serotonin receptors and gut microbiota in the rat. Mol Psychiatry. 2018;23:351–361. doi: 10.1038/mp.2017.38. [DOI] [PubMed] [Google Scholar]
- 58.Pinto-Sanchez M.I., Hall G.B., Ghajar K., Nardelli A., Bolino C., Lau J.T., Martin F.P., Cominetti O., Welsh C., Rieder A., Traynor J., Gregory C., De Palma G., Pigrau M., Ford A.C., Macri J., Berger B., Bergonzelli G., Surette M.G., Collins S.M., Moayyedi P., Bercik P. Probiotic Bifidobacterium longum NCC3001 reduces depression scores and alters brain activity: a pilot study in patients with irritable bowel syndrome. Gastroenterology. 2017;153:448–459 e8. doi: 10.1053/j.gastro.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 59.Tillisch K., Labus J., Kilpatrick L., Jiang Z., Stains J., Ebrat B., Guyonnet D., Legrain-Raspaud S., Trotin B., Naliboff B., Mayer E.A. Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology. 2013;144:1394–1401. doi: 10.1053/j.gastro.2013.02.043. 401 e1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Steenbergen L., Sellaro R., van Hemert S., Bosch J.A., Colzato L.S. A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood. Brain Behav Immun. 2015;48:258–264. doi: 10.1016/j.bbi.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 61.Messaoudi M., Violle N., Bisson J.F., Desor D., Javelot H., Rougeot C. Beneficial psychological effects of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in healthy human volunteers. Gut Microbes. 2011;2:256–261. doi: 10.4161/gmic.2.4.16108. [DOI] [PubMed] [Google Scholar]
- 62.Kelly J.R., Allen A.P., Temko A., Hutch W., Kennedy P.J., Farid N., Murphy E., Boylan G., Bienenstock J., Cryan J.F., Clarke G., Dinan T.G. Lost in translation? The potential psychobiotic Lactobacillus rhamnosus (JB-1) fails to modulate stress or cognitive performance in healthy male subjects. Brain Behav Immun. 2017;61:50–59. doi: 10.1016/j.bbi.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 63.Meyer C., Vassar M. The fragility of probiotic Bifidobacterium longum NCC3001 use for depression in patients with irritable bowel syndrome. Gastroenterology. 2018;154:764. doi: 10.1053/j.gastro.2017.09.055. [DOI] [PubMed] [Google Scholar]
- 64.McNulty N.P., Yatsunenko T., Hsiao A., Faith J.J., Muegge B.D., Goodman A.L., Henrissat B., Oozeer R., Cools-Portier S., Gobert G., Chervaux C., Knights D., Lozupone C.A., Knight R., Duncan A.E., Bain J.R., Muehlbauer M.J., Newgard C.B., Heath A.C., Gordon J.I. The impact of a consortium of fermented milk strains on the gut microbiome of gnotobiotic mice and monozygotic twins. Sci Transl Med. 2011;3:106ra106. doi: 10.1126/scitranslmed.3002701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tolhurst G., Heffron H., Lam Y.S., Parker H.E., Habib A.M., Diakogiannaki E., Cameron J., Grosse J., Reimann F., Gribble F.M. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes. 2012;61:364–371. doi: 10.2337/db11-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang Y., Telesford K.M., Ochoa-Reparaz J., Haque-Begum S., Christy M., Kasper E.J., Wang L., Wu Y., Robson S.C., Kasper D.L., Kasper L.H. An intestinal commensal symbiosis factor controls neuroinflammation via TLR2-mediated CD39 signalling. Nat Commun. 2014;5:4432. doi: 10.1038/ncomms5432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singh V., Roth S., Llovera G., Sadler R., Garzetti D., Stecher B., Dichgans M., Liesz A. Microbiota dysbiosis controls the neuroinflammatory response after stroke. J Neurosci. 2016;36:7428–7440. doi: 10.1523/JNEUROSCI.1114-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yano J.M., Yu K., Donaldson G.P., Shastri G.G., Ann P., Ma L., Nagler C.R., Ismagilov R.F., Mazmanian S.K., Hsiao E.Y. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015;161:264–276. doi: 10.1016/j.cell.2015.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wikoff W.R., Anfora A.T., Liu J., Schultz P.G., Lesley S.A., Peters E.C., Siuzdak G. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci U S A. 2009;106:3698–3703. doi: 10.1073/pnas.0812874106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Samuel B.S., Shaito A., Motoike T., Rey F.E., Backhed F., Manchester J.K., Hammer R.E., Williams S.C., Crowley J., Yanagisawa M., Gordon J.I. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc Natl Acad Sci U S A. 2008;105:16767–16772. doi: 10.1073/pnas.0808567105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Haghikia A., Jorg S., Duscha A., Berg J., Manzel A., Waschbisch A., Hammer A., Lee D.H., May C., Wilck N., Balogh A., Ostermann A.I., Schebb N.H., Akkad D.A., Grohme D.A., Kleinewietfeld M., Kempa S., Thone J., Demir S., Muller D.N., Gold R., Linker R.A. Dietary fatty acids directly impact central nervous system autoimmunity via the small intestine. Immunity. 2015;43:817–829. doi: 10.1016/j.immuni.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 72.Goehler L.E., Gaykema R.P., Opitz N., Reddaway R., Badr N., Lyte M. Activation in vagal afferents and central autonomic pathways: early responses to intestinal infection with Campylobacter jejuni. Brain Behav Immun. 2005;19:334–344. doi: 10.1016/j.bbi.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 73.Barrett E., Ross R.P., O'Toole P.W., Fitzgerald G.F., Stanton C. gamma-Aminobutyric acid production by culturable bacteria from the human intestine. J Appl Microbiol. 2012;113:411–417. doi: 10.1111/j.1365-2672.2012.05344.x. [DOI] [PubMed] [Google Scholar]
- 74.Minuk G.Y. Gamma-aminobutyric-acid (Gaba) production by 8 common bacterial pathogens. Scand J Infect Dis. 1986;18:465–467. doi: 10.3109/00365548609032366. [DOI] [PubMed] [Google Scholar]
- 75.Ozogul F. Effects of specific lactic acid bacteria species on biogenic amine production by foodborne pathogen. Int J Food Sci Tech. 2011;46:478–484. [Google Scholar]
- 76.Shishov V.A., Kirovskaya T.A., Kudrin V.S., Oleskin A.V. Amine neuromediators, their precursors, and oxidation products in the culture of Escherichia coli K-12. Appl Biochem Micro. 2009;45:494–497. [PubMed] [Google Scholar]
- 77.Asano Y., Hiramoto T., Nishino R., Aiba Y., Kimura T., Yoshihara K., Koga Y., Sudo N. Critical role of gut microbiota in the production of biologically active, free catecholamines in the gut lumen of mice. Am J Physiol Gastrointest Liver Physiol. 2012;303:G1288–G1295. doi: 10.1152/ajpgi.00341.2012. [DOI] [PubMed] [Google Scholar]
- 78.Furness J.B., Rivera L.R., Cho H.J., Bravo D.M., Callaghan B. The gut as a sensory organ. Nat Rev Gastroenterol Hepatol. 2013;10:729–740. doi: 10.1038/nrgastro.2013.180. [DOI] [PubMed] [Google Scholar]
- 79.Morton G.J., Kaiyala K.J., Foster-Schubert K.E., Cummings D.E., Schwartz M.W. Carbohydrate feeding dissociates the postprandial FGF19 response from circulating bile acid levels in humans. J Clin Endocrinol Metab. 2014;99:E241–E245. doi: 10.1210/jc.2013-3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.de Aguiar Vallim T.Q., Tarling E.J., Edwards P.A. Pleiotropic roles of bile acids in metabolism. Cell Metab. 2013;17:657–669. doi: 10.1016/j.cmet.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wahlstrom A., Sayin S.I., Marschall H.U., Backhed F. Intestinal crosstalk between bile acids and microbiota and its impact on host metabolism. Cell Metab. 2016;24:41–50. doi: 10.1016/j.cmet.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 82.Hsuchou H., Pan W., Kastin A.J. Fibroblast growth factor 19 entry into brain. Fluids Barriers CNS. 2013;10:32. doi: 10.1186/2045-8118-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Marcelin G., Jo Y.H., Li X., Schwartz G.J., Zhang Y., Dun N.J., Lyu R.M., Blouet C., Chang J.K., Chua S., Jr. Central action of FGF19 reduces hypothalamic AGRP/NPY neuron activity and improves glucose metabolism. Mol Metab. 2014;3:19–28. doi: 10.1016/j.molmet.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tomlinson E., Fu L., John L., Hultgren B., Huang X., Renz M., Stephan J.P., Tsai S.P., Powell-Braxton L., French D., Stewart T.A. Transgenic mice expressing human fibroblast growth factor-19 display increased metabolic rate and decreased adiposity. Endocrinology. 2002;143:1741–1747. doi: 10.1210/endo.143.5.8850. [DOI] [PubMed] [Google Scholar]
- 85.Fu L., John L.M., Adams S.H., Yu X.X., Tomlinson E., Renz M., Williams P.M., Soriano R., Corpuz R., Moffat B., Vandlen R., Simmons L., Foster J., Stephan J.P., Tsai S.P., Stewart T.A. Fibroblast growth factor 19 increases metabolic rate and reverses dietary and leptin-deficient diabetes. Endocrinology. 2004;145:2594–2603. doi: 10.1210/en.2003-1671. [DOI] [PubMed] [Google Scholar]
- 86.Ryan K.K., Kohli R., Gutierrez-Aguilar R., Gaitonde S.G., Woods S.C., Seeley R.J. Fibroblast growth factor-19 action in the brain reduces food intake and body weight and improves glucose tolerance in male rats. Endocrinology. 2013;154:9–15. doi: 10.1210/en.2012-1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Perry R.J., Lee S., Ma L., Zhang D., Schlessinger J., Shulman G.I. FGF1 and FGF19 reverse diabetes by suppression of the hypothalamic-pituitary-adrenal axis. Nat Commun. 2015;6:6980. doi: 10.1038/ncomms7980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Maruyama T., Miyamoto Y., Nakamura T., Tamai Y., Okada H., Sugiyama E., Nakamura T., Itadani H., Tanaka K. Identification of membrane-type receptor for bile acids (M-BAR) Biochem Biophys Res Commun. 2002;298:714–719. doi: 10.1016/s0006-291x(02)02550-0. [DOI] [PubMed] [Google Scholar]
- 89.Ridlon J.M., Kang D.J., Hylemon P.B. Bile salt biotransformations by human intestinal bacteria. J Lipid Res. 2006;47:241–259. doi: 10.1194/jlr.R500013-JLR200. [DOI] [PubMed] [Google Scholar]
- 90.Thomas C., Gioiello A., Noriega L., Strehle A., Oury J., Rizzo G., Macchiarulo A., Yamamoto H., Mataki C., Pruzanski M., Pellicciari R., Auwerx J., Schoonjans K. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10:167–177. doi: 10.1016/j.cmet.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Trabelsi M.S., Daoudi M., Prawitt J., Ducastel S., Touche V., Sayin S.I., Perino A., Brighton C.A., Sebti Y., Kluza J., Briand O., Dehondt H., Vallez E., Dorchies E., Baud G., Spinelli V., Hennuyer N., Caron S., Bantubungi K., Caiazzo R., Reimann F., Marchetti P., Lefebvre P., Backhed F., Gribble F.M., Schoonjans K., Pattou F., Tailleux A., Staels B., Lestavel S. Farnesoid X receptor inhibits glucagon-like peptide-1 production by enteroendocrine L cells. Nat Commun. 2015;6:7629. doi: 10.1038/ncomms8629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Topping D.L., Clifton P.M. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev. 2001;81:1031–1064. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 93.Russell W.R., Gratz S.W., Duncan S.H., Holtrop G., Ince J., Scobbie L., Duncan G., Johnstone A.M., Lobley G.E., Wallace R.J., Duthie G.G., Flint H.J. High-protein, reduced-carbohydrate weight-loss diets promote metabolite profiles likely to be detrimental to colonic health. Am J Clin Nutr. 2011;93:1062–1072. doi: 10.3945/ajcn.110.002188. [DOI] [PubMed] [Google Scholar]
- 94.Cani P.D., Lecourt E., Dewulf E.M., Sohet F.M., Pachikian B.D., Naslain D., De Backer F., Neyrinck A.M., Delzenne N.M. Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr. 2009;90:1236–1243. doi: 10.3945/ajcn.2009.28095. [DOI] [PubMed] [Google Scholar]
- 95.Nohr M.K., Egerod K.L., Christiansen S.H., Gille A., Offermanns S., Schwartz T.W., Moller M. Expression of the short chain fatty acid receptor GPR41/FFAR3 in autonomic and somatic sensory ganglia. Neuroscience. 2015;290:126–137. doi: 10.1016/j.neuroscience.2015.01.040. [DOI] [PubMed] [Google Scholar]
- 96.Kim D.Y., Camilleri M. Serotonin: a mediator of the brain-gut connection. Am J Gastroenterol. 2000;95:2698–2709. doi: 10.1111/j.1572-0241.2000.03177.x. [DOI] [PubMed] [Google Scholar]
- 97.Ruddick J.P., Evans A.K., Nutt D.J., Lightman S.L., Rook G.A., Lowry C.A. Tryptophan metabolism in the central nervous system: medical implications. Exp Rev Mol Med. 2006;8:1–27. doi: 10.1017/S1462399406000068. [DOI] [PubMed] [Google Scholar]
- 98.Marin I.A., Goertz J.E., Ren T., Rich S.S., Onengut-Gumuscu S., Farber E., Wu M., Overall C.C., Kipnis J., Gaultier A. Microbiota alteration is associated with the development of stress-induced despair behavior. Sci Rep. 2017;7:43859. doi: 10.1038/srep43859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fung T.C., Olson C.A., Hsiao E.Y. Interactions between the microbiota, immune and nervous systems in health and disease. Nat Neurosci. 2017;20:145–155. doi: 10.1038/nn.4476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ochoa-Reparaz J., Mielcarz D.W., Ditrio L.E., Burroughs A.R., Begum-Haque S., Dasgupta S., Kasper D.L., Kasper L.H. Central nervous system demyelinating disease protection by the human commensal Bacteroides fragilis depends on polysaccharide A expression. J Immunol. 2010;185:4101–4108. doi: 10.4049/jimmunol.1001443. [DOI] [PubMed] [Google Scholar]
- 101.Ochoa-Reparaz J., Mielcarz D.W., Ditrio L.E., Burroughs A.R., Foureau D.M., Haque-Begum S., Kasper L.H. Role of gut commensal microflora in the development of experimental autoimmune encephalomyelitis. J Immunol. 2009;183:6041–6050. doi: 10.4049/jimmunol.0900747. [DOI] [PubMed] [Google Scholar]
- 102.Benakis C., Brea D., Caballero S., Faraco G., Moore J., Murphy M., Sita G., Racchumi G., Ling L., Pamer E.G., Iadecola C., Anrather J. Commensal microbiota affects ischemic stroke outcome by regulating intestinal gammadelta T cells. Nat Med. 2016;22:516–523. doi: 10.1038/nm.4068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Winek K., Engel O., Koduah P., Heimesaat M.M., Fischer A., Bereswill S., Dames C., Kershaw O., Gruber A.D., Curato C., Oyama N., Meisel C., Meisel A., Dirnagl U. Depletion of cultivatable gut microbiota by broad-spectrum antibiotic pretreatment worsens outcome after murine stroke. Stroke. 2016;47:1354–1363. doi: 10.1161/STROKEAHA.115.011800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Erny D., Hrabe de Angelis A.L., Jaitin D., Wieghofer P., Staszewski O., David E., Keren-Shaul H., Mahlakoiv T., Jakobshagen K., Buch T., Schwierzeck V., Utermohlen O., Chun E., Garrett W.S., McCoy K.D., Diefenbach A., Staeheli P., Stecher B., Amit I., Prinz M. Host microbiota constantly control maturation and function of microglia in the CNS. Nat Neurosci. 2015;18:965–977. doi: 10.1038/nn.4030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.de Lartigue G., de La Serre C.B., Raybould H.E. Vagal afferent neurons in high fat diet-induced obesity; intestinal microflora, gut inflammation and cholecystokinin. Physiol Behav. 2011;105:100–105. doi: 10.1016/j.physbeh.2011.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Barajon I., Serrao G., Arnaboldi F., Opizzi E., Ripamonti G., Balsari A., Rumio C. Toll-like receptors 3, 4, and 7 are expressed in the enteric nervous system and dorsal root ganglia. J Histochem Cytochem. 2009;57:1013–1023. doi: 10.1369/jhc.2009.953539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brun P., Giron M.C., Qesari M., Porzionato A., Caputi V., Zoppellaro C., Banzato S., Grillo A.R., Spagnol L., De Caro R., Pizzuti D., Barbieri V., Rosato A., Sturniolo G.C., Martines D., Zaninotto G., Palu G., Castagliuolo I. Toll-like receptor 2 regulates intestinal inflammation by controlling integrity of the enteric nervous system. Gastroenterology. 2013;145:1323–1333. doi: 10.1053/j.gastro.2013.08.047. [DOI] [PubMed] [Google Scholar]
- 108.Mao Y.K., Kasper D.L., Wang B., Forsythe P., Bienenstock J., Kunze W.A. Bacteroides fragilis polysaccharide A is necessary and sufficient for acute activation of intestinal sensory neurons. Nat Commun. 2013;4:1465. doi: 10.1038/ncomms2478. [DOI] [PubMed] [Google Scholar]
- 109.Keita A.V., Soderholm J.D. The intestinal barrier and its regulation by neuroimmune factors. Neurogastroenterol Motil. 2010;22:718–733. doi: 10.1111/j.1365-2982.2010.01498.x. [DOI] [PubMed] [Google Scholar]
- 110.Huang C., Wang J., Hu W., Wang C., Lu X., Tong L., Wu F., Zhang W. Identification of functional farnesoid X receptors in brain neurons. FEBS Lett. 2016;590:3233–3242. doi: 10.1002/1873-3468.12373. [DOI] [PubMed] [Google Scholar]
- 111.Keitel V., Gorg B., Bidmon H.J., Zemtsova I., Spomer L., Zilles K., Haussinger D. The bile acid receptor TGR5 (Gpbar-1) acts as a neurosteroid receptor in brain. Glia. 2010;58:1794–1805. doi: 10.1002/glia.21049. [DOI] [PubMed] [Google Scholar]
- 112.Kimura I., Inoue D., Maeda T., Hara T., Ichimura A., Miyauchi S., Kobayashi M., Hirasawa A., Tsujimoto G. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41) Proc Natl Acad Sci U S A. 2011;108:8030–8035. doi: 10.1073/pnas.1016088108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Won Y.J., Lu V.B., Puhl H.L., 3rd, Ikeda S.R. beta-Hydroxybutyrate modulates N-type calcium channels in rat sympathetic neurons by acting as an agonist for the G-protein-coupled receptor FFA3. J Neurosci. 2013;33:19314–19325. doi: 10.1523/JNEUROSCI.3102-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nohr M.K., Pedersen M.H., Gille A., Egerod K.L., Engelstoft M.S., Husted A.S., Sichlau R.M., Grunddal K.V., Poulsen S.S., Han S., Jones R.M., Offermanns S., Schwartz T.W. GPR41/FFAR3 and GPR43/FFAR2 as cosensors for short-chain fatty acids in enteroendocrine cells vs FFAR3 in enteric neurons and FFAR2 in enteric leukocytes. Endocrinology. 2013;154:3552–3564. doi: 10.1210/en.2013-1142. [DOI] [PubMed] [Google Scholar]
- 115.Kelly J.R., Kennedy P.J., Cryan J.F., Dinan T.G., Clarke G., Hyland N.P. Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders. Front Cell Neurosci. 2015;9:392. doi: 10.3389/fncel.2015.00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ivanov I.I., Atarashi K., Manel N., Brodie E.L., Shima T., Karaoz U., Wei D., Goldfarb K.C., Santee C.A., Lynch S.V., Tanoue T., Imaoka A., Itoh K., Takeda K., Umesaki Y., Honda K., Littman D.R. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–498. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Round J.L., Lee S.M., Li J., Tran G., Jabri B., Chatila T.A., Mazmanian S.K. The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science. 2011;332:974–977. doi: 10.1126/science.1206095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kucharzik T., Lugering N., Rautenberg K., Lugering A., Schmidt M.A., Stoll R., Domschke W. Role of M cells in intestinal barrier function. Ann N Y Acad Sci. 2000;915:171–183. doi: 10.1111/j.1749-6632.2000.tb05240.x. [DOI] [PubMed] [Google Scholar]
- 119.Vaishnava S., Behrendt C.L., Ismail A.S., Eckmann L., Hooper L.V. Paneth cells directly sense gut commensals and maintain homeostasis at the intestinal host-microbial interface. Proc Natl Acad Sci U S A. 2008;105:20858–20863. doi: 10.1073/pnas.0808723105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hooper L.V., Wong M.H., Thelin A., Hansson L., Falk P.G., Gordon J.I. Molecular analysis of commensal host-microbial relationships in the intestine. Science. 2001;291:881–884. doi: 10.1126/science.291.5505.881. [DOI] [PubMed] [Google Scholar]
- 121.Rakoff-Nahoum S., Paglino J., Eslami-Varzaneh F., Edberg S., Medzhitov R. Recognition of commensal microflora by toll-like receptors is required for intestinal homeostasis. Cell. 2004;118:229–241. doi: 10.1016/j.cell.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 122.Da Silva S., Robbe-Masselot C., Ait-Belgnaoui A., Mancuso A., Mercade-Loubiere M., Salvador-Cartier C., Gillet M., Ferrier L., Loubiere P., Dague E., Theodorou V., Mercier-Bonin M. Stress disrupts intestinal mucus barrier in rats via mucin O-glycosylation shift: prevention by a probiotic treatment. Am J Physiol Gastrointest Liver Physiol. 2014;307:G420–G429. doi: 10.1152/ajpgi.00290.2013. [DOI] [PubMed] [Google Scholar]
- 123.Atuma C., Strugala V., Allen A., Holm L. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 2001;280:G922–G929. doi: 10.1152/ajpgi.2001.280.5.G922. [DOI] [PubMed] [Google Scholar]
- 124.Macfarlane S., Dillon J.F. Microbial biofilms in the human gastrointestinal tract. J Appl Microbiol. 2007;102:1187–1196. doi: 10.1111/j.1365-2672.2007.03287.x. [DOI] [PubMed] [Google Scholar]
- 125.Johansson M.E., Larsson J.M., Hansson G.C. The two mucus layers of colon are organized by the MUC2 mucin, whereas the outer layer is a legislator of host-microbial interactions. Proc Natl Acad Sci U S A. 2011;108(Suppl 1):4659–4665. doi: 10.1073/pnas.1006451107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Braniste V., Al-Asmakh M., Kowal C., Anuar F., Abbaspour A., Toth M., Korecka A., Bakocevic N., Ng L.G., Kundu P., Gulyas B., Halldin C., Hultenby K., Nilsson H., Hebert H., Volpe B.T., Diamond B., Pettersson S. The gut microbiota influences blood-brain barrier permeability in mice. Sci Transl Med. 2014;6:263ra158. doi: 10.1126/scitranslmed.3009759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Brown A.J., Goldsworthy S.M., Barnes A.A., Eilert M.M., Tcheang L., Daniels D., Muir A.I., Wigglesworth M.J., Kinghorn I., Fraser N.J., Pike N.B., Strum J.C., Steplewski K.M., Murdock P.R., Holder J.C., Marshall F.H., Szekeres P.G., Wilson S., Ignar D.M., Foord S.M., Wise A., Dowell S.J. The orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids. J Biol Chem. 2003;278:11312–11319. doi: 10.1074/jbc.M211609200. [DOI] [PubMed] [Google Scholar]
- 128.Michel L., Prat A. One more role for the gut: microbiota and blood brain barrier. Ann Transl Med. 2016;4:15. doi: 10.3978/j.issn.2305-5839.2015.10.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Varatharaj A., Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12. doi: 10.1016/j.bbi.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 130.Aguilera M., Vergara P., Martinez V. Stress and antibiotics alter luminal and wall-adhered microbiota and enhance the local expression of visceral sensory-related systems in mice. Neurogastroenterol Motil. 2013;25:e515–e529. doi: 10.1111/nmo.12154. [DOI] [PubMed] [Google Scholar]
- 131.Tannock G.W., Savage D.C. Influences of dietary and environmental stress on microbial populations in the murine gastrointestinal tract. Infect Immun. 1974;9:591–598. doi: 10.1128/iai.9.3.591-598.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Galley J.D., Nelson M.C., Yu Z.T., Dowd S.E., Walter J., Kumar P.S., Lyte M., Bailey M.T. Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota. BMC Microbiol. 2014;14:189. doi: 10.1186/1471-2180-14-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zijlmans M.A., Korpela K., Riksen-Walraven J.M., de Vos W.M., de Weerth C. Maternal prenatal stress is associated with the infant intestinal microbiota. Psychoneuroendocrinology. 2015;53:233–245. doi: 10.1016/j.psyneuen.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 134.Van Felius I.D., Akkermans L.M., Bosscha K., Verheem A., Harmsen W., Visser M.R., Gooszen H.G. Interdigestive small bowel motility and duodenal bacterial overgrowth in experimental acute pancreatitis. Neurogastroenterol Motil. 2003;15:267–276. doi: 10.1046/j.1365-2982.2003.00410.x. [DOI] [PubMed] [Google Scholar]
- 135.Lewis S.J., Heaton K.W. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32:920–924. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 136.Saad R.J., Rao S.S., Koch K.L., Kuo B., Parkman H.P., McCallum R.W., Sitrin M.D., Wilding G.E., Semler J.R., Chey W.D. Do stool form and frequency correlate with whole-gut and colonic transit? Results from a multicenter study in constipated individuals and healthy controls. Am J Gastroenterol. 2010;105:403–411. doi: 10.1038/ajg.2009.612. [DOI] [PubMed] [Google Scholar]
- 137.Vandeputte D., Falony G., Vieira-Silva S., Tito R.Y., Joossens M., Raes J. Stool consistency is strongly associated with gut microbiota richness and composition, enterotypes and bacterial growth rates. Gut. 2016;65:57–62. doi: 10.1136/gutjnl-2015-309618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Falony G., Joossens M., Vieira-Silva S., Wang J., Darzi Y., Faust K., Kurilshikov A., Bonder M.J., Valles-Colomer M., Vandeputte D., Tito R.Y., Chaffron S., Rymenans L., Verspecht C., De Sutter L., Lima-Mendez G., D'Hoe K., Jonckheere K., Homola D., Garcia R., Tigchelaar E.F., Eeckhaudt L., Fu J., Henckaerts L., Zhernakova A., Wijmenga C., Raes J. Population-level analysis of gut microbiome variation. Science. 2016;352:560–564. doi: 10.1126/science.aad3503. [DOI] [PubMed] [Google Scholar]
- 139.Roager H.M., Hansen L.B., Bahl M.I., Frandsen H.L., Carvalho V., Gobel R.J., Dalgaard M.D., Plichta D.R., Sparholt M.H., Vestergaard H., Hansen T., Sicheritz-Ponten T., Nielsen H.B., Pedersen O., Lauritzen L., Kristensen M., Gupta R., Licht T.R. Colonic transit time is related to bacterial metabolism and mucosal turnover in the gut. Nat Microbiol. 2016;1:16093. doi: 10.1038/nmicrobiol.2016.93. [DOI] [PubMed] [Google Scholar]
- 140.Tottey W., Feria-Gervasio D., Gaci N., Laillet B., Pujos E., Martin J.F., Sebedio J.L., Sion B., Jarrige J.F., Alric M., Brugere J.F. Colonic transit time is a driven force of the gut microbiota composition and metabolism: in vitro evidence. J Neurogastroenterol Motil. 2017;23:124–134. doi: 10.5056/jnm16042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Santos J., Yang P.C., Soderholm J.D., Benjamin M., Perdue M.H. Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut. 2001;48:630–636. doi: 10.1136/gut.48.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Saunders P.R., Santos J., Hanssen N.P., Yates D., Groot J.A., Perdue M.H. Physical and psychological stress in rats enhances colonic epithelial permeability via peripheral CRH. Dig Dis Sci. 2002;47:208–215. doi: 10.1023/a:1013204612762. [DOI] [PubMed] [Google Scholar]
- 143.Meddings J.B., Swain M.G. Environmental stress-induced gastrointestinal permeability is mediated by endogenous glucocorticoids in the rat. Gastroenterology. 2000;119:1019–1028. doi: 10.1053/gast.2000.18152. [DOI] [PubMed] [Google Scholar]
- 144.Demaude J., Salvador-Cartier C., Fioramonti J., Ferrier L., Bueno L. Phenotypic changes in colonocytes following acute stress or activation of mast cells in mice: implications for delayed epithelial barrier dysfunction. Gut. 2006;55:655–661. doi: 10.1136/gut.2005.078675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Lauffer A., Vanuytsel T., Vanormelingen C., Vanheel H., Salim Rasoel S., Toth J., Tack J., Fornari F., Farre R. Subacute stress and chronic stress interact to decrease intestinal barrier function in rats. Stress. 2016;19:225–234. doi: 10.3109/10253890.2016.1154527. [DOI] [PubMed] [Google Scholar]
- 146.Varghese A.K., Verdu E.F., Bercik P., Khan W.I., Blennerhassett P.A., Szechtman H., Collins S.M. Antidepressants attenuate increased susceptibility to colitis in a murine model of depression. Gastroenterology. 2006;130:1743–1753. doi: 10.1053/j.gastro.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 147.Rubio C.A., Huang C.B. Quantification of the sulphomucin-producing cell population of the colonic mucosa during protracted stress in rats. In Vivo. 1992;6:81–84. [PubMed] [Google Scholar]
- 148.Soderholm J.D., Yang P.C., Ceponis P., Vohra A., Riddell R., Sherman P.M., Perdue M.H. Chronic stress induces mast cell-dependent bacterial adherence and initiates mucosal inflammation in rat intestine. Gastroenterology. 2002;123:1099–1108. doi: 10.1053/gast.2002.36019. [DOI] [PubMed] [Google Scholar]
- 149.Houlden A., Goldrick M., Brough D., Vizi E.S., Lenart N., Martinecz B., Roberts I.S., Denes A. Brain injury induces specific changes in the caecal microbiota of mice via altered autonomic activity and mucoprotein production. Brain Behav Immun. 2016;57:10–20. doi: 10.1016/j.bbi.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Kim Y.S., Ho S.B. Intestinal goblet cells and mucins in health and disease: recent insights and progress. Curr Gastroenterol Rep. 2010;12:319–330. doi: 10.1007/s11894-010-0131-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lyte M. The role of microbial endocrinology in infectious disease. J Endocrinol. 1993;137:343–345. doi: 10.1677/joe.0.1370343. [DOI] [PubMed] [Google Scholar]
- 152.Mayer E.A., Savidge T., Shulman R.J. Brain-gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500–1512. doi: 10.1053/j.gastro.2014.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Santos J., Saperas E., Nogueiras C., Mourelle M., Antolin M., Cadahia A., Malagelada J.R. Release of mast cell mediators into the jejunum by cold pain stress in humans. Gastroenterology. 1998;114:640–648. doi: 10.1016/s0016-5085(98)70577-3. [DOI] [PubMed] [Google Scholar]
- 154.Stephens R.L., Tache Y. Intracisternal injection of a TRH analogue stimulates gastric luminal serotonin release in rats. Am J Physiol. 1989;256:G377–G383. doi: 10.1152/ajpgi.1989.256.2.G377. [DOI] [PubMed] [Google Scholar]
- 155.Yang H., Stephens R.L., Tache Y. TRH analogue microinjected into specific medullary nuclei stimulates gastric serotonin secretion in rats. Am J Physiol. 1992;262:G216–G222. doi: 10.1152/ajpgi.1992.262.2.G216. [DOI] [PubMed] [Google Scholar]
- 156.Clarke M.B., Hughes D.T., Zhu C., Boedeker E.C., Sperandio V. The QseC sensor kinase: a bacterial adrenergic receptor. Proc Natl Acad Sci U S A. 2006;103:10420–10425. doi: 10.1073/pnas.0604343103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lyte M. The role of catecholamines in gram-negative sepsis. Med Hypotheses. 1992;37:255–258. doi: 10.1016/0306-9877(92)90197-k. [DOI] [PubMed] [Google Scholar]
- 158.Alverdy J., Holbrook C., Rocha F., Seiden L., Wu R.L., Musch M., Chang E., Ohman D., Suh S. Gut-derived sepsis occurs when the right pathogen with the right virulence genes meets the right host: evidence for in vivo virulence expression in Pseudomonas aeruginosa. Ann Surg. 2000;232:480–489. doi: 10.1097/00000658-200010000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hughes D.T., Sperandio V. Inter-kingdom signalling: communication between bacteria and their hosts. Nat Rev Microbiol. 2008;6:111–120. doi: 10.1038/nrmicro1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Cogan T.A., Thomas A.O., Rees L.E., Taylor A.H., Jepson M.A., Williams P.H., Ketley J., Humphrey T.J. Norepinephrine increases the pathogenic potential of Campylobacter jejuni. Gut. 2007;56:1060–1065. doi: 10.1136/gut.2006.114926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Paulose J.K., Wright J.M., Patel A.G., Cassone V.M. Human gut bacteria are sensitive to melatonin and express endogenous circadian rhythmicity. PLoS One. 2016;11:e0146643. doi: 10.1371/journal.pone.0146643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Bubenik G.A., Brown G.M. Pinealectomy reduces melatonin levels in the serum but not in the gastrointestinal tract of rats. Biol Signals. 1997;6:40–44. doi: 10.1159/000109107. [DOI] [PubMed] [Google Scholar]
- 163.Bubenik G.A., Pang S.F., Hacker R.R., Smith P.S. Melatonin concentrations in serum and tissues of porcine gastrointestinal tract and their relationship to the intake and passage of food. J Pineal Res. 1996;21:251–256. doi: 10.1111/j.1600-079x.1996.tb00294.x. [DOI] [PubMed] [Google Scholar]
- 164.Thaiss C.A., Zeevi D., Levy M., Zilberman-Schapira G., Suez J., Tengeler A.C., Abramson L., Katz M.N., Korem T., Zmora N., Kuperman Y., Biton I., Gilad S., Harmelin A., Shapiro H., Halpern Z., Segal E., Elinav E. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159:514–529. doi: 10.1016/j.cell.2014.09.048. [DOI] [PubMed] [Google Scholar]
- 165.Simren M., Barbara G., Flint H.J., Spiegel B.M., Spiller R.C., Vanner S., Verdu E.F., Whorwell P.J., Zoetendal E.G. Rome Foundation Committee. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013;62:159–176. doi: 10.1136/gutjnl-2012-302167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Labus J.S., Hollister E.B., Jacobs J., Kirbach K., Oezguen N., Gupta A., Acosta J., Luna R.A., Aagaard K., Versalovic J., Savidge T., Hsiao E., Tillisch K., Mayer E.A. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. 2017;5:49. doi: 10.1186/s40168-017-0260-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Jeffery I.B., O'Toole P.W., Ohman L., Claesson M.J., Deane J., Quigley E.M., Simren M. An irritable bowel syndrome subtype defined by species-specific alterations in faecal microbiota. Gut. 2012;61:997–1006. doi: 10.1136/gutjnl-2011-301501. [DOI] [PubMed] [Google Scholar]
- 168.Tap J., Derrien M., Tornblom H., Brazeilles R., Cools-Portier S., Dore J., Storsrud S., Le Neve B., Ohman L., Simren M. Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology. 2017;152:111–123 e8. doi: 10.1053/j.gastro.2016.09.049. [DOI] [PubMed] [Google Scholar]
- 169.Kerckhoffs A.P., Ben-Amor K., Samsom M., van der Rest M.E., de Vogel J., Knol J., Akkermans L.M. Molecular analysis of faecal and duodenal samples reveals significantly higher prevalence and numbers of Pseudomonas aeruginosa in irritable bowel syndrome. J Med Microbiol. 2011;60:236–245. doi: 10.1099/jmm.0.022848-0. [DOI] [PubMed] [Google Scholar]
- 170.Pimentel M.F., Giamarellos-Bourboulis E.J., Pyleris E., Pistiki K., Tang J., Lee C., Harkins T., Kim G., Weitsman S., Barlow G.M., Chang C. The first large scale deep sequencing of the duodenal microbiome in irritable bowel syndrome reveals striking differences compared to healthy controls. Gastroenterology. 2013;144:S59. [Google Scholar]
- 171.Bailey M.T., Dowd S.E., Galley J.D., Hufnagle A.R., Allen R.G., Lyte M. Exposure to a social stressor alters the structure of the intestinal microbiota: implications for stressor-induced immunomodulation. Brain Behav Immun. 2011;25:397–407. doi: 10.1016/j.bbi.2010.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Knowles S.R., Nelson E.A., Palombo E.A. Investigating the role of perceived stress on bacterial flora activity and salivary cortisol secretion: a possible mechanism underlying susceptibility to illness. Biol Psychol. 2008;77:132–137. doi: 10.1016/j.biopsycho.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 173.Pedram P., Wadden D., Amini P., Gulliver W., Randell E., Cahill F., Vasdev S., Goodridge A., Carter J.C., Zhai G., Ji Y., Sun G. Food addiction: its prevalence and significant association with obesity in the general population. PLoS One. 2013;8:e74832. doi: 10.1371/journal.pone.0074832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lin H.V., Frassetto A., Kowalik E.J., Jr., Nawrocki A.R., Lu M.M., Kosinski J.R., Hubert J.A., Szeto D., Yao X., Forrest G., Marsh D.J. Butyrate and propionate protect against diet-induced obesity and regulate gut hormones via free fatty acid receptor 3-independent mechanisms. PLoS One. 2012;7:e35240. doi: 10.1371/journal.pone.0035240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Everard A., Lazarevic V., Derrien M., Girard M., Muccioli G.G., Neyrinck A.M., Possemiers S., Van Holle A., Francois P., de Vos W.M., Delzenne N.M., Schrenzel J., Cani P.D. Responses of gut microbiota and glucose and lipid metabolism to prebiotics in genetic obese and diet-induced leptin-resistant mice. Diabetes. 2011;60:2775–2786. doi: 10.2337/db11-0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 177.Fernandez-Real J.M., Serino M., Blasco G., Puig J., Daunis-i-Estadella J., Ricart W., Burcelin R., Fernandez-Aranda F., Portero-Otin M. Gut microbiota interacts with brain microstructure and function. J Clin Endocrinol Metab. 2015;100:4505–4513. doi: 10.1210/jc.2015-3076. [DOI] [PubMed] [Google Scholar]
- 178.Janik R., Thomason L.A.M., Stanisz A.M., Forsythe P., Bienenstock J., Stanisz G.J. Magnetic resonance spectroscopy reveals oral Lactobacillus promotion of increases in brain GABA, N-acetyl aspartate and glutamate. Neuroimage. 2016;125:988–995. doi: 10.1016/j.neuroimage.2015.11.018. [DOI] [PubMed] [Google Scholar]
- 179.Zhang H., DiBaise J.K., Zuccolo A., Kudrna D., Braidotti M., Yu Y., Parameswaran P., Crowell M.D., Wing R., Rittmann B.E., Krajmalnik-Brown R. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci U S A. 2009;106:2365–2370. doi: 10.1073/pnas.0812600106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Li J.V., Ashrafian H., Bueter M., Kinross J., Sands C., le Roux C.W., Bloom S.R., Darzi A., Athanasiou T., Marchesi J.R., Nicholson J.K., Holmes E. Metabolic surgery profoundly influences gut microbial-host metabolic cross-talk. Gut. 2011;60:1214–1223. doi: 10.1136/gut.2010.234708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Damms-Machado A., Mitra S., Schollenberger A.E., Kramer K.M., Meile T., Konigsrainer A., Huson D.H., Bischoff S.C. Effects of surgical and dietary weight loss therapy for obesity on gut microbiota composition and nutrient absorption. Biomed Res Int. 2015;2015:806248. doi: 10.1155/2015/806248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Furet J.P., Kong L.C., Tap J., Poitou C., Basdevant A., Bouillot J.L., Mariat D., Corthier G., Dore J., Henegar C., Rizkalla S., Clement K. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59:3049–3057. doi: 10.2337/db10-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Graessler J., Qin Y., Zhong H., Zhang J., Licinio J., Wong M.L., Xu A., Chavakis T., Bornstein A.B., Ehrhart-Bornstein M., Lamounier-Zepter V., Lohmann T., Wolf T., Bornstein S.R. Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J. 2013;13:514–522. doi: 10.1038/tpj.2012.43. [DOI] [PubMed] [Google Scholar]
- 184.Liou A.P., Paziuk M., Luevano J.M., Jr., Machineni S., Turnbaugh P.J., Kaplan L.M. Conserved shifts in the gut microbiota due to gastric bypass reduce host weight and adiposity. Sci Transl Med. 2013;5:178ra41. doi: 10.1126/scitranslmed.3005687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Tremaroli V., Karlsson F., Werling M., Stahlman M., Kovatcheva-Datchary P., Olbers T., Fandriks L., le Roux C.W., Nielsen J., Backhed F. Roux-en-Y gastric bypass and vertical banded gastroplasty induce long-term changes on the human gut microbiome contributing to fat mass regulation. Cell Metab. 2015;22:228–238. doi: 10.1016/j.cmet.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kelly J.R., Clarke G., Cryan J.F., Dinan T.G. Brain-gut-microbiota axis: challenges for translation in psychiatry. Ann Epidemiol. 2016;26:366–372. doi: 10.1016/j.annepidem.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 187.Mertsalmi T.H., Aho V.T.E., Pereira P.A.B., Paulin L., Pekkonen E., Auvinen P., Scheperjans F. More than constipation - bowel symptoms in Parkinson's disease and their connection to gut microbiota. Eur J Neurol. 2017;24:1375–1383. doi: 10.1111/ene.13398. [DOI] [PubMed] [Google Scholar]
- 188.Fasano A., Visanji N.P., Liu L.W.C., Lang A.E., Pfeiffer R.F. Gastrointestinal dysfunction in Parkinson's disease. Lancet Neurol. 2015;14:625–639. doi: 10.1016/S1474-4422(15)00007-1. [DOI] [PubMed] [Google Scholar]
- 189.Mayer E.A., Padua D., Tillisch K. Altered brain-gut axis in autism: comorbidity or causative mechanisms? Bioessays. 2014;36:933–939. doi: 10.1002/bies.201400075. [DOI] [PubMed] [Google Scholar]
- 190.Kang D.W., Adams J.B., Gregory A.C., Borody T., Chittick L., Fasano A., Khoruts A., Geis E., Maldonado J., McDonough-Means S., Pollard E.L., Roux S., Sadowsky M.J., Lipson K.S., Sullivan M.B., Caporaso J.G., Krajmalnik-Brown R. Microbiota transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome. 2017;5:10. doi: 10.1186/s40168-016-0225-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Mayer E.A., Labus J.S., Tillisch K., Cole S.W., Baldi P. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol. 2015;12:592–605. doi: 10.1038/nrgastro.2015.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Bohorquez D.V., Liddle R.A. The gut connectome: making sense of what you eat. J Clin Invest. 2015;125:888–890. doi: 10.1172/JCI81121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Sporns O. The human connectome: origins and challenges. Neuroimage. 2013;80:53–61. doi: 10.1016/j.neuroimage.2013.03.023. [DOI] [PubMed] [Google Scholar]