Abstract
This study investigated the relationship between self-reported time in bed and sleep quality in association with self-reported internalizing and externalizing symptoms in a sample of 285 elementary school students (52% female) recruited from a rural Midwestern elementary school. Path models were used to estimate proposed associations, controlling for grade level and gender. Curvilinear associations were found between time in bed and anxiety, depressive symptoms, and irritability. Marginal curvilinear trends were found between time in bed and emotion dysregulation, reactive aggression, and proactive aggression. Sleep quality was negatively associated with anxiety, depressive symptoms, irritability, reactive aggression, and delinquency engagement. Gender and grade differences were found across models. Findings suggest that examining self-reported time in bed (both linear and quadratic) and sleep quality is important for understanding internalizing and externalizing symptoms associated with sleep in school-age youth. Incorporating self-reported sleep assessments into clinical practice and school-based evaluations may have implications for a child’s adjustment.
Keywords: Sleep Quality, Time in Bed, Internalizing Problems, Externalizing Problems, Children
Sleep plays a crucial role in children’s development and functioning [1]. The school-age years are an important time for forming healthy habits around sleep [1]. Sleep problems in school-age children can arise in the form of sleep duration (i.e., too little or too much time asleep or time in bed [2, 3]) and subjective sleep quality (e.g., problems with falling or staying asleep, restless sleep [1]). Research consistently finds that children with sleep problems are at risk for a host of internalizing and externalizing symptoms [4]. Studies examining the associations between sleep problems and functioning among school-age youth frequently rely on parent report or use of objective sleep measures (e.g., actigraphy). However, assessing sleep problems based on a child’s subjective experience is important to capture behavioral sleep disturbances not found on objective measures of sleep [5]. Parents also may not be fully aware of their child’s sleep difficulties, as studies have found low correspondence between parent- and child-reported sleep problems [6, 7] and between parent-reported sleep compared to actigraphy [8]. Furthermore, few studies examine and compare different aspects of sleep problems within the same study [3]. To better understand children’s functioning associated with the subjective sleep experience, research is warranted that examines children’s perceived sleep problems in relation to various internalizing and externalizing symptoms [9]. The purpose of the current study was to examine and compare aspects of self-reported sleep problems (i.e., time in bed and sleep quality) associated with self-reported internalizing (e.g., anxiety, depression symptoms) and externalizing (i.e., delinquency, proactive aggression, reactive aggression) symptoms among a sample of elementary school-age youth.
Receiving enough sleep is an important aspect to examine when considering sleep problems in school-age youth. Several organizations provide recommended guidelines for appropriate sleep duration for children, although the amount of sleep recommended within these guidelines has been trending downward over the last century [10]. Indeed, the National Sleep Foundation recently updated their sleep duration recommendations by expanding the school-age recommended sleep duration from 10–11 hours per night to 9–11 hours per night [11]. This change may not be inconsequential, as research indicates that even a one-hour difference in sleep duration can have an impact on children’s functioning [12]. Further, sleep duration recommendations are usually given as a range, indicating that there are individual differences in the optimal amount of sleep [11] and that problems may be associated with a child receiving either too much or too little sleep. Although only a few studies have investigated this hypothesized curvilinear association, using actigraphy and self-report measures of sleep duration, results have supported the notion that physical and behavioral health problems can arise at either end of the sleep duration continuum [13–17]. Given the divergent and changing sleep recommendations across time and organizations, a better understanding of internalizing and externalizing symptoms associated with high and low levels of sleep duration, including time in bed, among children is warranted in order to inform sleep recommendations for school-age youth.
In addition, sleep recommendations do not often account for sleep quality [11], although children may experience poor sleep quality regardless of sleep duration or time in bed [3, 18]. Extant research indicates that sleep duration and sleep quality are both associated with children’s psychological functioning [4, 19]. Few studies, however, have examined associations between self-reported sleep quality and time in bed and internalizing and externalizing problems among school-age youth.
When considering internalizing and externalizing symptoms associated with poor sleep duration and/or quality, a growing body of literature links sleep problems to parent- and child-reported internalizing symptoms in school-aged children [4, 9, 19, 20]. For example, more difficulty sleeping was associated with greater parent-reported anxiety/depression symptoms (but not teacher-reported anxiety/depression) in a large sample of school-aged children [21]. Sleep problem severity is also associated with increased internalizing symptoms in clinical samples of children with sleep disorders [22]. While these studies demonstrate an association between sleep functioning and internalizing problems, there is mixed evidence as to whether sleep duration or quality is more strongly associated with anxiety symptoms [23] or depressive symptoms [24, 25] in school-aged children. In addition to internalizing domains of anxiety and depression, both poor sleep duration and quality are also associated with more emotion regulation difficulties [26, 27].
Sleep problems have also been examined in relation to parent- and teacher-reported externalizing behavior problems (e.g., aggression, delinquency, substance use) in children, with few known studies examining this based on child self-report [9]. Although parents and teachers are reliable reporters of externalizing problems and offer strengths in assessing problem behaviors [28], children may offer a unique perspective on their problem behavior [29]. Studies have found poor sleep to be associated with children’s aggressive behavior [9, 25, 30]. For instance, Becker [9] found worse sleep functioning, assessed through child self-report, to be associated with greater teacher-reported reactive, but not proactive, aggression. Other studies have shown children with shorter sleep duration and/or poorer sleep quality exhibit increased behavioral problems such as oppositionality or rule-breaking behavior compared to youth with more and/or better sleep [31–34], although exceptions have also been reported [9, 35]. In support of this association, Smedje, Broman, and Hetta [36] found more parent-reported sleep-wake difficulties were related to engagement in conduct problems in a sample of 6–8-year-old Swedish children. In another study, lower objectively-measured sleep duration was associated with more parent-reported conduct problems in a sample of 6 to 11-year-old children [37]. Despite the growing number of studies examining the relations among sleep problems and internalizing/externalizing symptoms in school-age youth, few studies have examined these associations while using children’s self-reported sleep assessments and/or self-reported behavior problems.
In summary, given that limited research has examined multiple aspects of self-reported sleep problems in association with diverse internalizing and externalizing symptoms among school-age youth, and that few studies have examined the curvilinear (quadratic) associations of sleep duration, the current study examined the linear and quadratic relations between self-reported sleep duration (defined as time in bed in the current study [38]) and sleep quality in association with both internalizing/emotional problems (i.e., anxiety, depression, irritability, emotion regulation) and externalizing/behavioral problems (i.e., delinquency, proactive and reactive aggression) in a sample of elementary school-age youth. Two main study hypotheses were examined. First, with previous studies finding differences in internalizing and externalizing symptoms based on incremental differences in sleep duration [12], we expected internalizing and externalizing problems to be more pronounced among children who report low (too little) or high (too much) levels of time in bed. Second, we expected poor sleep quality to be positively associated with internalizing and externalizing symptoms. Group differences in grade and gender were also examined, given differences found across internalizing and externalizing symptoms based on these individual factors [39, 40].
Methods
Participants
This study included 285 3rd-5th-grade students attending an elementary school in a rural, Midwestern community. Children attending this school were eligible to participate if they were proficient in English, spent the majority of their education time in a mainstream classroom, and, based on information provided by school administrators, did not have a developmental disability that would hinder comprehension and ability to answer research questions. Written parental consent was required for children to participate in the study. Participants were recruited by including study information and a consent form in the back-to-school materials sent to parents. If no response was received, a separate parent consent letter was mailed to the students’ homes. Of the 391 students eligible for the study, 301 (76.98%) obtained written parental consent to participate in the study. Of the 301 obtaining written parental consent, 295 (98.01%) completed the questionnaires. Ten participants (3.39%) were excluded from the current analysis due to lack of data on time in bed. The final sample included 285 participants (52% female). School records indicate that the majority of students at the school identify as White. The sample’s grade distribution was as follows: 36% in 3rd grade (n = 102), 32% in 4th grade (n = 91), and 32% in 5th grade (n = 92).
Procedures
Study procedures were approved by the researchers’ institutional review board and the school district’s administrators and board prior to data collection. Participants provided verbal assent prior to completing the survey. Surveys were administered by trained research assistants and completed by participants in their classrooms during the school day. Participation took approximately 25–30 minutes. Within each classroom, one member of the research team read items aloud while participants filled in their answers to the questionnaires. Two to three additional research team members were also present to assist in answering questions and to monitor students’ participation. In order to maintain confidentiality, no school personnel were present in the room during survey administration. Students were given a small prize (special pencils) as a reward for their participation.
Measures
Demographics.
Participants completed a questionnaire that evaluated several demographic variables, including gender. Information about participating students’ grade levels was provided by school administrators separately.
Time in Bed.
To assess time in bed, participants responded to the following two questions: “What time do you usually go to bed on the days you have to go to school?” and “What time do you wake up in the morning on the days that you have to go to school?” As in previous research examining self-reported time in bed in elementary-aged children [17], time in bed was calculated as the difference between these two times. Originally measured in minutes, values were converted to hours for all analyses in order to facilitate clear interpretation of the results.
Sleep Quality.
Sleep quality was measured using the 4-item child self-report scale developed by Meijer and colleagues [2]. All items were rated on a 3-point Likert scale with response options tailored to the each question. Specifically, items assessed the presence of common childhood sleep problems, including sleep latency (“When you’re in bed and the lights are turned off: 1 = it takes you a long time to fall asleep, 2 = you stay awake for a while, 3 = you fall asleep at once”), frequency of night wakings (“Do you ever sometimes wake up during the night? 1 = nearly every night, 2 = sometimes, 3 = never”), and difficulty returning to sleep (“If you wake up during the night: 1 = it takes you a while to fall asleep again, 2 = you fall asleep again, 3 = mostly you don’t notice”), as well as the child’s subjective sleep quality (“Do you sleep well at night? 1 = no, 2 = sometimes, 3 = yes, always”) [2, p. 153]. This scale has demonstrated evidence of reliability and validity in previous research among school-age children and early adolescents [e.g., 2], and evidence supports the validity of child self-reported sleep quality in its convergence with more objective sleep measures such as actigraphy [17]. In the present sample, the internal consistency of sleep quality was in the questionable to adequate range (α = .59), which is likely due to the small number of items and limited scale variability in the measure [41] as well as the distinctiveness across sleep quality domains [22]. Indeed, sleep quality is a heterogeneous construct that has been operationalized in many different ways [5,17]. Thus, low internal consistency is common among brief screeners for sleep problems/quality [e.g., 21], which nonetheless demonstrate evidence of reliability, validity, and utility [5]. This brief, broad measure was selected in light of participation time constraints and given the useful separation between general sleep quality and time in bed [2,3,17].
Emotion Dysregulation.
Students completed the Children’s Emotion Management Scales (CEMS) to assess emotion dysregulation [42, 43]. Both the 12-item Sadness (CSMS) and 11-item Anger (CAMS) versions of the scale were administered. The CEMS results in a total Dysregulation scale utilizing 3 items from the CSMS (e.g., “I cry and carry on when I’m sad”) and 3 items from the CAMS (e.g., “I do things like slam doors when I am mad”). The Dysregulation scale evaluates the extent to which participants lack the ability to manage certain emotional responses (e.g., slamming doors, whining). Previous research has found evidence of moderate internal consistency (α = .60-.68) and good test-retest reliability (r = .62-.63) on the dysregulation scales of the CSMS and CAMS [42], as well good convergent and discriminant validity with the dysregulation scale of the CEMS [42] and good construct validity with the dysregulation scale of the CAMS [43]. Items were measured on a 3-point Likert scale of 1 (hardly ever), 2 (sometimes), or 3 (often). Total scores were calculated using the mean across the 6 responses. Internal consistency was adequate (α = .65).
Anxiety Symptoms.
To assess anxiety symptoms, participants completed the 8-item self-report Pediatric Anxiety Scale of the Patient-Reported Outcomes Measurement Information System (PROMIS)[44]. Items (e.g., “I felt worried”) were rated on a 5-point scale, from 1 (never) to 5 (always). Mean scores were calculated for the current study. Internal consistency for the scale in this sample was good (α = .89).
Depressive Symptoms.
To evaluate depressive symptoms, the Short Mood and Feelings Questionnaire (SMFQ) was administered to participants [45, 46]. This 13-item self-report measure asks participants to rate statements on a 3-point Likert scale, from 0 (Not True) to 2 (True), based on how they felt in the previous two weeks (e.g., “I didn’t enjoy anything at all”). Previous research with clinical and community samples have demonstrated good internal consistency and content, criterion, and construct validity [45, 47]. Internal consistency in the current study was good (α = .87).
Irritability.
To assess irritability, a symptom present in various mood disorders, participants completed the Affective Reactivity Index (ARI) [48]. The ARI included 6 items evaluating 3 facets of irritability: (a) anger threshold (e.g., “I am easily annoyed by others.”); (b) regularity of angry feelings and behaviors (e.g., “I get angry frequently”); and (c) the length of time these angry feelings and behaviors last (e.g., “I stay angry for a long time”). Items are rated on a 3-point Likert scale, from 0 (not true) to 2 (certainly true) based on how participants felt in the previous six months, and means were calculated for the current study. Previous research has shown good internal consistency (α = 0.88) and factorial structure in clinical and community samples using this measure [48]. Internal consistency for the questionnaire in the current sample was good (α = .81).
Engagement in Delinquency.
Students’ engagement in delinquency was measured utilizing a 14-item self-report questionnaire regarding deviant and antisocial behavior that had been committed in the previous year [49]. This measure was originally designed to assess parent- and child-reported peer delinquency, but has since been adapted for use as a self-report measure [50, 51]. Questions asked about behaviors such as absenteeism from school, contact with law enforcement, and property damage, with a Yes/No response option to each item. Total scores were generated by calculating a summed score, and higher total scores denote greater engagement in delinquency. Participants reported engaging in 0–6 delinquent acts, with 17% of participants reporting that they engaged in one or more delinquent act. Internal consistency was low (α =.52), which may be due to the dichotomous nature of the response options [52].
Reactive/Proactive Aggression.
Children were evaluated on reactive and proactive aggression using the 6-item self-report reactive-proactive aggression scale [53]. This scale includes three items that evaluate proactive aggression [e.g., “I use physical force (or threaten to use physical force) in order to dominate other kids”] and three items that assess reactive aggression (e.g., “When I have been teased or threatened, I get angry easily and strike back”). Answers were based on a 5-point Likert scale, from 1 (never) to 5 (almost always). Although initially developed for use by teachers, this measure has shown to be valid and reliable when used with school-age children [54, 55]. Mean subscales for reactive aggression and proactive aggression were calculated and analyzed. In the present study, αs = .71 and .56 for reactive and proactive aggression, respectively.
Analytic Plan
Univariate and bivariate characteristics of the data were examined prior to analyses. Missing data (<4%) were handled with pairwise deletion in correlation analyses and with full information maximum likelihood estimation in path analyses [56, 57]. Robust estimation was utilized in order to address the non-normality of the data [58]. The study questions were examined in a stepwise manner using two path models estimated in Mplus Version 7 [58]. We specified an internalizing model (endogenous variables: anxiety, depression, emotion dysregulation, and irritability) as well as an externalizing model (endogenous variables: delinquency, proactive aggression, and reactive aggression). All models were estimated with sleep quality, time in bed, and a quadratic term for time in bed included as the main exogenous variables, while also controlling for grade and gender. For time in bed, both the linear and the quadratic terms were included because the association between sleep and behavior is not always found to be entirely linear [13, 15]. To model these kinds of associations, both the linear and quadratic terms are needed [52]. We followed a model-trimming approach wherein the quadratic term was included in the initial models, based on the hypothesized curvilinear associations. If the quadratic term was not found to be significant, the model was then re-estimated with the linear term only. To aid in the interpretation of results, all exogenous and control variables were mean-centered prior to analyses, while endogenous variables were left on their original scale.
Grade and gender differences were examined by re-estimating the above path models using a multiple group approach. First, we estimated the internalizing and externalizing path models with substantive paths constrained to be equal across gender (M = F) and grade level (3rd = 4th = 5th). Then we removed these equality constraints and allowed parameters to be estimated independently for each group (M, F; 3rd, 4th, 5th) while still keeping the covariates constrained (e.g., controlling for the effect of grade in the gender models, and vice versa). We then applied Satorra and Bentler’s (2001) scaled chi-square difference test, which accounts for the chi-square correction imposed by robust estimation [58]. A nonsignificant test statistic would indicate that the simpler (single-group) model is preferred for reasons of fit and parsimony, such that results can be applied similarly for boys and girls; conversely, a significant test statistic would indicate that the more complex model (i.e., with path estimates allowed to vary across groups) exhibits better fit than the simpler model. Given this latter scenario, our next step was to examine the modification indices (MIs) from the single-group model to identify which particular paths were driving the dissimilarities between groups. Using the hypothesized path models as a guide, we identified MIs > 5 for any regression or covariance paths that corresponded to a substantive model path, and re-estimated the model with these paths freed.
Because all of the initial path models were specified to be fully saturated (df = 0), model fit statistics are not interpretable and therefore not reported for these models. However, this was not the case in the models testing for gender differences; thus, we report the Chi Square test statistic, Root Mean Square Error of Approximation (RMSEA), Confirmatory Fit Index (CFI), and Standardized Root Mean Squared Residual (SRMSR) for all models testing gender and grade differences. A model is considered to have acceptable fit when CFI ≥ .90, with values closer to 1.0 indicating better fit; and values ≤ .08 for both RMSEA and SRMR, with values closer to 0.0 indicating better fit [57, 60]. Given their interdependency, the linear and quadratic terms for time in bed were always specified in the same manner within any particular model (i.e., both were constrained or both were fixed).
Results
Participants reported spending an average of 9.77 hours (SD = 1.00) in bed. Notably, 83.5% (n = 238) of the sample reported spending between 9 and 11 hours in bed at night, which is in accordance with recent sleep duration recommendations [11], while 10.9% (n = 31) of participants reported being in bed for less than 9 hours and 5.6% (n = 16) reported being in bed for longer than 11 hours. Bivariate linear correlations (Table 1) showed that higher sleep quality was associated with lower levels of anxiety (r = −.35, p < .01), depression (r = −.39, p < .01), emotion dysregulation (r = −.12, p < .10), irritability (r = −.24, p < .01), delinquency engagement (r = −.18, p < .01), and reactive aggression (r = −.16, p < .01). Less time in bed was associated with increased engagement in delinquency (r = −.20, p < .01). No gender differences were found in relation to sleep quality or time in bed (ps > .05). Girls reported more anxiety symptoms (r = .12, p < .05) and less irritability (r = −.14, p < .05), delinquency engagement (r = −.19, p < .05), and reactive aggression (r = −.17, p < .01) compared to boys. Children in lower grades reported being in bed for less time (r = −.20, p < .01). No grade differences were seen across the internalizing or externalizing variables (ps > .05).
Table 1. Correlations, means, and standard deviations.
| Sleep Variables | Internalizing Variables | Externalizing Variables | Demographic Variables | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
| 1. Sleep Quality | 1 | ||||||||||
| 2. Time in Bed | −.02 | 1 | |||||||||
| 3. Anxiety | −.35** | .11+ | 1 | ||||||||
| 4. Depression | −.39** | .03 | .61** | 1 | |||||||
| 5. Em Dysreg | −.12+ | −.03 | .24** | .31** | 1 | ||||||
| 6. Irritability | −.24** | .08 | .40** | .48** | .37** | 1 | |||||
| 7. Delinquency | −.18** | −.20** | .10+ | .29** | .25** | .36** | 1 | ||||
| 8. Reactive Agg | −.16** | .03 | .27** | .43** | .36** | .55** | .36** | 1 | |||
| 9. Proactive Agg | −.09 | −.02 | .11+ | .35** | .19** | .38** | .35** | .48** | 1 | ||
| 10. Female | −.03 | .04 | .12* | −.06 | −.08 | −.14* | −.19** | −.17** | −.12* | 1 | |
| 11. Grade | −.01 | −.20** | .07 | .06 | .00 | .07 | .05 | −.07 | −.07 | .01 | 1 |
|
| |||||||||||
| M (%) | 2.02 | 9.77 | 1.95 | .32 | 1.54 | .44 | .25 | 1.73 | 1.10 | (52.0) | 3.96 |
| SD | .43 | 1.00 | .85 | .36 | .43 | .46 | .67 | .81 | .33 | -- | .83 |
Note. Em Dysreg = emotion dysregulation, Agg = aggression.
p < .1,
p < .05,
p < .01
Path Models
Results of the internalizing and externalizing path models are presented in Tables 2 and 3, respectively. In the internalizing model, a similar pattern was observed across endogenous variables with regard to their associations with sleep quality, time in bed-linear, and time in bed-quadratic; although, in some cases, these trends did not reach statistical significance. Sleep quality was negatively associated with irritability, depressive symptoms, and anxiety, and showed a marginal relationship with emotion dysregulation (p < .10). Time in bed exhibited significant curvilinear associations (see Figure 1) with irritability, depressive symptoms, and anxiety, and a similar marginal pattern for emotion dysregulation (p < .10). Gender associations were found for irritability and anxiety, such that boys reported higher levels of irritability whereas girls reported higher levels of anxiety. In contrast, gender was not associated with emotion dysregulation or depressive symptoms. Grade level was significantly associated with irritability and marginally associated with depressive symptoms and anxiety, with children in more advanced grades reporting higher levels of these variables. Grade level was not associated with emotion dysregulation. Overall, these models accounted for a significant portion of the variance (approximately 15–22%) in irritability, depressive symptoms, and anxiety; but not for emotion dysregulation (approximately 3%).
Table 2. Results of Internalizing Path Model.
| Endogenous Variables |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exogenous Variables | Emotion Dysregulation | Irritability | Depressive Symptoms | Anxiety | ||||||||
|
| ||||||||||||
| B | (B SE) | β | B | (B SE) | β | B | (B SE) | β | B | (B SE) | β | |
| Intercept | 1.539** | (.025) | 3.567 | .439** | (.025) | .958 | .323** | (.019) | .899 | 1.951** | (.046) | 2.288 |
| Grade | .000 | (.030) | .000 | .068* | (.028) | .122 | .042+ | (.024) | .097 | .112+ | (.058) | .108 |
| Female | −.071 | (.051) | −.164 | −.140** | (.051) | −.305 | −.053 | (.038) | −.147 | .183* | (.093) | .215 |
| Sleep Quality | −.110+ | (.059) | −.107 | −.228** | (.069) | −.208 | −.306** | (.055) | −.356 | −.665** | (.135) | −.326 |
| Time in Bed | −.007 | (.025) | −.016 | .061* | (.027) | .130 | .027 | (.029) | .076 | .116* | (.053) | .137 |
| Time in Bed2 | .015+ | (.009) | .084 | .046** | (.010) | .242 | .036** | (.012) | .241 | .036* | (.018) | .104 |
|
| ||||||||||||
| R2 | .028 | (.018) | .150** | (.049) | .217** | (.054) | .162** | (.039) | ||||
p < .1,
p < .05,
p < .01
Table 3. Results of Externalizing Path Model.
| Endogenous Variables |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Exogenous Variables | Proactive Aggression |
Reactive Aggression |
Delinquency |
||||||
| B | (B SE) | β | B | (B SE) | β | B | (B SE) | β | |
| Intercept | 1.098** | (.019) | 3.377 | 1.729** | (.045) | 2.149 | .249** | (.036) | .373 |
| Grade | −.020 | (.017) | −.051 | −.048 | (.051) | −.049 | .030 | (.037) | .038 |
| Female | −.078* | (.039) | −.241 | −.271** | (.092) | −.337 | −.248** | (.073) | −.371 |
| Sleep Quality | −.057 | (.055) | −.073 | −.260* | (.124) | −.135 | −.253* | (.098) | −.158 |
| Time in Bed | −.001 | (.031) | −.004 | .034 | (.064) | .042 | −.106+ | (.062) | −.159 |
| Time in Bed2 | .024+ | (.014) | .178 | .061+ | (.034) | .184 | .068 | (.046) | .249 |
|
| |||||||||
| R2 | .059 | (.042) | .091+ | (.047) | .168 | (.111) | |||
p < .1,
p < .05,
p < .01
Figure 1.
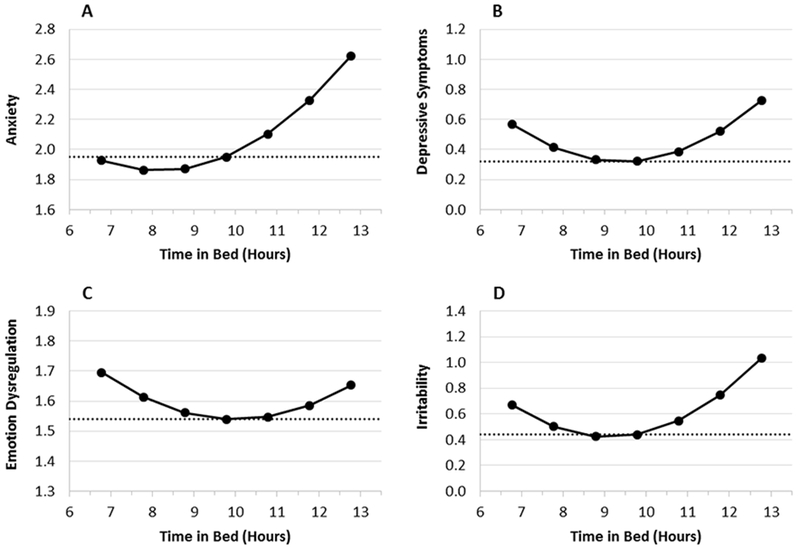
Significantly and marginally significant curvilinear relations between time in bed and internalizing problems controlling for grade, gender, and sleep quality. Solid line and circular markers represent the model-estimated values at the mean level of time in bed, 9.78 hours (center marker) ± 3 hours (outer markers). Dotted line represents the sample mean of the y-axis variable. Panel A (anxiety), quadratic trend p = .039; Panel B (depressive symptoms), quadratic trend p = .004; Panel C (emotion dysregulation), quadratic trend p = .086; Panel D (irritability), quadratic trend p < .001.
Figure 1 presents the curvilinear associations between time in bed and all internalizing problems—anxiety (Panel A), depressive symptoms (Panel B), emotion dysregulation (Panel C), and irritability (Panel D)—after controlling for age, gender, and sleep quality. It is clear from these data that children who fall toward either tail end of the distribution1 of time in bed are likely to report higher levels of depressive symptoms, irritability, and (marginally) emotion dysregulation. Anxiety showed a similar pattern, except that the model predicted elevated anxiety scores for children at high levels of sleep but not at low levels.
Results were slightly less consistent for the externalizing path model. Lower sleep quality was significantly associated with higher levels of delinquency and reactive aggression, but not proactive aggression. Further, marginal (p < .10) quadratic trends were found between time in bed and reactive and proactive aggression. Only a marginal linear trend was found between time in bed and delinquency, and this path was attenuated to nonsignificance (p = .14) when the model was re-estimated without the quadratic term. Unlike the internalizing regression paths, the externalizing path model revealed no associations with grade, and uniform associations with gender. That is, boys reported higher scores than girls on all measures of externalizing problems. Despite these trends and significant paths, the externalizing model accounted for only 9% of the variance in reactive aggression (p < .10). The R-squares for proactive aggression (6%) and delinquency (17%) did not approach significance.
Similar to Figure 1 with internalizing problems, Figure 2 plots the curvilinear associations that were found (at p < .01) between time in bed and externalizing problems, controlling for grade and gender. Results are presented for proactive aggression in Panel A and reactive aggression in Panel B. Strikingly, the shape of the curvilinear trends for these externalizing problems generally resembles those that were found for internalizing problems, as described above. Higher levels of proactive and reactive aggression were found for children reporting very low or very high levels of time in bed.
Figure 2.
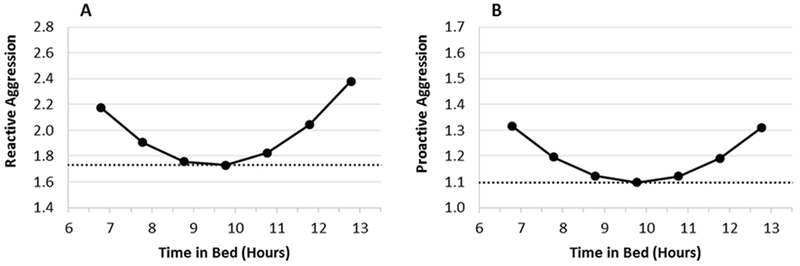
Marginally significant curvilinear relations between time in bed and externalizing problems controlling for grade, gender, and sleep quality. Solid line and circular markers represent the model-estimated values at the mean level of time in bed, 9.78 hours (center marker) ± 3 hours (outer markers). Dotted line represents the sample mean of the y-axis variable. Panel A (reactive aggression), quadratic trend p = .073; Panel B (proactive aggression), quadratic trend p = .088.
Gender and Grade Differences
Results of multiple group models assessing for grade and gender differences are presented in Table 4. Internalizing path models showed no significant differences associated with gender (Models 1a vs. 1b), but there were some overall differences across grade levels (Models 2a vs. 2b). Examination of MIs in the fully constrained model (Model 2a) suggested that the between-grade differences were largely driven by four paths: depressive and anxiety symptoms regressed on time in bed-linear and time in bed-quadratic terms. Accordingly, these four paths were freed to vary across grade levels (Model 2c). Results showed good overall fit for Model 2c, with greater parsimony and no significant differences compared to the fully unconstrained model (Model 2b). Thus, this model was retained as the preferred model. The group-specific path estimates from Model 2c indicated that the curvilinear association between time in bed and anxiety was observed among 5th graders (B = .26, p <.001) and 3rd graders (B = .05, p = .05), but not 4th graders (p = .22). Similarly, the curvilinear association between time in bed and depressive symptoms was significant among both 5th (B = .09, p = .001) and 3rd graders (B = .05, p = .02), but nonsignificant for 4th graders (p = .49).
Table 4. Assessing Gender and Grade Differences.
| Model & Description | χ2 (df) | SB χ2 Correction | Δ χ2 (df) | RMSEA (90% CI) | CFI | SRMR | MIs > 5 | |
|---|---|---|---|---|---|---|---|---|
| INTERNALIZING MODELS | ||||||||
| Gender differences | ||||||||
| 1a | Constrained | 23.192 (16) | 1.0231 | – | .056 (.000-.103) | .975 | .045 | Yes |
| 1b | Unconstrained | 5.305 (4) | .8633 | 17.887 (12) | .048 (.000-.143) | .995 | .020 | No |
| Grade differences | ||||||||
| 2a | Constrained | 49.874 (32) | 1.0950 | – | .077 (.029-.116) | .949 | .059 | Yes |
| 2b | Unconstrained | 8.479 (8) | .9375 | 41.395* (24) | .025 (.000-.125) | .999 | .022 | No |
| 2c | Select paths freed a | 25.398 (24) | 1.0335 | 16.919 (16) | .025 (.000-.088) | .996 | .044 | No |
|
| ||||||||
| EXTERNALIZING MODELS | ||||||||
| Gender differences | ||||||||
| 3a | Constrained | 72.577 (12) | .5823 | – | .188 (.148-.231) | .591 | .080 | Yes |
| 3b | Unconstrained | 3.456 (3) | .6228 | 69.121** (9) | .033 (.000-.149) | .997 | .011 | No |
| 3c | Select paths freed b | 23.700 (10) | .8346 | 20.244** (7) | .098 (.047-.150) | .908 | .059 | No |
| Grade differences | ||||||||
| 4a | Constrained | 38.920 (24) | 1.0875 | – | .081 (.027-.126) | .888 | .063 | Yes |
| 4b | Unconstrained | 7.976 (6) | .8739 | 30.944* (18) | .059 (.000-.154) | .985 | .025 | No |
| 4c | Select paths freed c | 13.575 (18) | 1.1901 | 5.599 (12) | .000 (.000-.065) | 1.000 | .037 | No |
p < .1,
p< .05,
p < .01
Four path coefficients were allowed to vary across groups: depressive symptoms and anxiety regressed on sleep duration linear and quadratic terms.
Two path coefficients were allowed to vary across groups: delinquency regressed on time in bed linear and quadratic terms.
Three path coefficients were allowed to vary across groups: delinquency regressed on sleep quality and time in bed linear and quadratic terms. SB χ2 factor = Satorra-Bentler scaling correction factor for robust chi square statistic.
With respect to the externalizing models, overall differences were found for both gender (Models 3a vs. 3b) and grade (Models 4a vs. 4b). In each case, the between-group differences were associated with the delinquency variable. In the fully constrained gender model (Model 3a), MIs were elevated for two substantive paths: delinquency regressed on time in bed-linear and time in bed-quadratic terms. When these paths were allowed to vary across groups (Model 3c), the resulting model showed adequate overall fit to the data. The chi-square comparison test (Models 3b vs. 3c) indicated that Model 3b showed better overall fit; however, Model 3c did not yield any elevated MIs to suggest any substantive paths that might be different between males and females. Therefore, Model 3c was considered acceptable and preferred for its parsimony. In this modified model, the curvilinear association between time in bed and delinquency was found to be significant for males (B = .13, p = .004) but not for females (p = .73).
Finally, the MIs for Model 4a suggested that the between-grade differences in the externalizing path models appeared to be driven largely by three paths: delinquency regressed on sleep quality, time in bed-linear, and time in bed-quadratic. When these three paths were allowed to vary between groups (Model 4c), the results showed good overall fit, with greater parsimony and no significant differences compared to the unconstrained model (Model 4b). Examination of group-specific path coefficients revealed some interesting variations across grade levels. Among 5th graders, time in bed showed a curvilinear association with delinquency (B = .09, p = .005), but sleep quality was not associated with delinquency (p = .46). Conversely, for 4th graders, sleep quality (B = −.42, p = .01) was uniquely associated with delinquent behaviors, whereas time in bed showed only a marginal relationship with delinquency (B = .11, p = .08). Finally, among 3rd graders, none of the three sleep variables were associated with delinquency (ps = .41-.67).
Discussion
This study adds to the growing literature on self-reported time in bed and sleep quality among school-age youth, and simultaneously examines several internalizing and externalizing problems in association with these sleep constructs. As expected, both time in bed and sleep quality showed unique associations with internalizing and externalizing problems. The presentation of these symptoms differed for time in bed and sleep quality, and in some cases varied across grade and gender. As seen in previous research [3], time in bed and sleep quality were not associated, demonstrating that examining both time in bed and sleep quality is important for understanding a child’s sleep and associated problems.
Findings from this study provide evidence that the association between time in bed and child behavior problems appears to be curvilinear in nature. This adds to the current research on the curvilinear nature of sleep duration in youth [13, 15] by examining high and low levels of time in bed in association with multiple internalizing and externalizing symptoms among school-age youth. While children close to the sample’s average of 9.77 hours of time in bed were less likely to report internalizing or externalizing symptoms, both high and low amounts of time in bed were associated with higher levels of internalizing and externalizing symptoms, even when controlling for sleep quality, grade level, and gender. This pattern reached statistical significance with respect to depressive symptoms, anxiety, and irritability, while a similar but non-significant trend was found between time in bed and emotion dysregulation, proactive aggression, and reactive aggression. Understanding specific internalizing and externalizing symptoms and behaviors that may influence the strength of the curvilinear relationships is warranted. Interestingly, the association between anxiety and time in bed was slightly different, following a prominent positive linear pattern in addition to the significant quadratic trend. This suggests that spending a longer time in bed is more strongly associated with anxiety than spending a shorter amount of time in bed, and may be associated with previous research showing that children with clinically-significant levels of anxiety may experience difficulty falling asleep and staying asleep [61]. Overall, results of the current study suggest that time in bed is important to understanding the psychosocial functioning of school-age youth, as is considering both the linear and quadratic nature of this sleep problem.
Some age and gender differences were found in problems associated with time in bed. The relationships between time in bed and anxiety and depressive symptoms were driven by older participants (i.e., 5th graders) in the sample. This may be related to findings that children’s risk for declining time in bed [62] and increasing internalizing symptoms [40, 63] increases as they enter adolescence. Consistent with previous research [23], gender differences were not found within the internalizing model. Within the externalizing model, the association between time in bed and delinquency was significant for boys and 5th graders. This is not surprising given the increase in delinquency found as children enter adolescence, and the increased risk for delinquency engagement in boys compared to girls [39].
These findings add to the literature on the associations between self-reported time in bed and internalizing and externalizing symptoms among school-age youth, and indicate the importance of considering a child’s grade and gender in these associations. Although it has been difficult to specify exact sleep duration recommendations through empirical investigation [10, 12, 64], this study is consistent with previous findings supporting the importance of receiving an adequate amount of sleep for child well-being. The findings further highlight the importance of educating parents and clinicians on optimal sleep as not only constituting enough sleep but also monitoring for too much/too little sleep. Previous studies examining the effects of sleep deprivation through sleep restriction experiments has shown significant effects in neurobehavioral functioning for even 30–60 minute reductions in sleep [12]. However, sleep deprivation may also increase one’s sleep quality as a result of a physiological response to compensate for varied sleep time [12, 65]. Continuing to examine incremental differences at both high and low durations of sleep and time in bed, and the corresponding role of sleep quality in these associations, may inform recommendations on optimal sleep durations in youth. Further, providers should consider assessing sleep duration, or time in bed, in youth presenting with internalizing and externalizing symptoms, especially as they near adolescence, to inform a comprehensive intervention plan.
Consistent with previous research, findings also indicated that sleep quality plays an important role in internalizing and externalizing symptoms among school-age youth. Youth who reported poor sleep quality also reported a significant number of symptoms of several internalizing and externalizing symptoms, even when controlling for sleep duration. However, sleep quality was differentially associated with internalizing and externalizing symptoms in this study. Within the internalizing domain, sleep quality was associated with anxiety, depressive symptoms, and irritability, while it was not associated with emotion dysregulation. Although studies have consistently shown an association between sleep and these internalizing domains [4, 19, 20], the strengths of the relationships have varied across studies. As was found in previous research [23], the largest effect in this study was seen in the link between sleep quality and anxiety. The physiological hyperarousal that is thought to distinguish anxiety from depression [66, 67] may account for the differing effect sizes between anxiety and depression in association with sleep quality [68]. Anxiety-related sleep disturbances are also a common sleep problem in school-age youth [1], which may account for the strength in relationships in this sample. Gender and grade differences were not found for sleep quality within the internalizing model, which may relate to similar prevalence rates of internalizing symptoms found in school-age boys and girls [69].
Within the externalizing domain, sleep quality was negatively associated with reactive aggression and delinquency but not proactive aggression. Poor sleep has been associated with increases in impulsivity [26]. Given the impulsive nature of both reactive aggression and delinquency, compared to the planful, deliberate behavior characteristic of proactive aggression [70–72], the current findings are not surprising. The limited research looking at aggression subtypes and delinquency in relation to sleep has found poor sleep to be associated with reactive but not proactive aggression [9, 71, 73] as well as with risk-taking delinquent behavior [74, 75]. The current study furthers this literature by looking at self-reported sleep quality and aggression subtypes in addition to delinquency in a sample of school-age youth. In addition, grade differences were found between sleep quality and delinquency, with a significant relationship seen between sleep quality and delinquency found for 4th graders but not 3rd or 5th graders. Although low rates of delinquency were reported in this sample, the significant findings associated with delinquency highlight the importance of considering the association between sleep and delinquency in youth when developing prevention and intervention efforts. Future research should examine outcomes of addressing sleep in impulsive children.
Several limitations should be taken into account when considering the current findings. First, because all measurements relied solely on children’s answers to questionnaires, this can increase the risk of common method variance. In addition, internalizing symptoms may exacerbate reports of sleep problems, with studies finding that depressed youth report more subjective sleep problems than non-depressed youth, even when objective measures do not confirm this difference [76]. Although findings were in the expected direction overall, and prior studies have supported the use of child-reported data for those 7 years and older [77], the addition of other types of measurements as well as measurements of internalizing and externalizing symptoms and sleep quality and duration from multiple reporters (e.g., parents, teachers) for comparison of findings would be beneficial for future research. Second, this study did not utilize objective measures of sleep variables, but rather relied on self-reported time in bed and sleep quality. The addition of objective sleep measures, such as actigraphy or polysomnography, would provide more accurate, objective, and specific calculations of sleep duration and quality. Nonetheless, the duration that the child perceives having spent in bed and/or slept during the night, as well as a child’s experience of sleep quality, is valuable information in understanding a child’s subjective experience of sleep [6, 9]. This is particularly the case given that parents may not be aware of a child’s poor sleep quality [6, 7]. A related limitation is that the present study relied upon brief measures, which likely accounts for the relatively low internal consistency in sleep quality and delinquency scores. While the measures selected for the present study were useful as a broadband screeners in a school-based sample, future research would benefit from more targeted assessment of different types and dimensions of sleep problems, delinquency, and other study variables using well-validated instruments.
In addition, due to the cross-sectional design of the study, these results should not be viewed as predictive of cause-and-effect relationships. Future studies would benefit from using a longitudinal design to study sleep along with behavioral and emotional outcomes in children over time. Further, since only a narrow range of school grades was used, these results may not generalize to younger children or adolescents. Developmental differences in sleep exist throughout the lifespan [78], and therefore studies should examine these relationships across developmental periods. Finally, approximately 25% of students’ parents did not provide written consent for their child to participate. Without access to all students’ data, we are unable to assess whether there were potential differences in students who did and did not participate.
Despite these limitations, this study adds to the growing literature on the association between self-reported sleep problems and internalizing and externalizing symptoms in school-age youth. Few studies have focused on youth self-report of sleep behaviors, despite parents not always being aware of their child’s sleep difficulties. Given the differences previously found between parent and child report of sleep quality [6, 7], considering the perspective of the child on their sleep habits and problems is important for adequately assessing and addressing their sleep needs. Several studies have demonstrated the reliability and validity of child self-report measures of their sleep habits [9, 79]. Future research should consider inclusion of these measures to better understand sleep and associated outcomes among school-age youth. Furthermore, findings underscore the importance of promoting healthy patterns of sleep – in terms of both time in bed and sleep quality – for parents of school-age youth. Research should also continue to examine the curvilinear nature of time in bed to better understand the association between sleep problems and internalizing and externalizing symptoms as well as other outcomes such as academic functioning, and to improve our understanding of optimal sleep. Overall, the findings show the importance of addressing sleep problems in school-age youth to contribute to healthy psychosocial functioning.
Summary
Among this sample of elementary school children, curvilinear associations were found in the association between time in bed and anxiety, depressive symptoms, and irritability, and marginal curvilinear trends were found between time in bed and emotion dysregulation, reactive aggression, and proactive aggression. When looking at age and gender differences, the relation between time in bed and anxiety and depressive symptoms were driven by older participants, while time in bed and delinquency was significant for boys and 5th graders. Sleep quality was negatively associated with anxiety, depressive symptoms, irritability, reactive aggression, and delinquency engagement. No gender and grade differences were found in the model examining sleep quality and internalizing symptoms, while sleep quality and delinquency was significant for 4th graders, but not 3rd or 5th graders. Findings suggest that examining self-reported time in bed (both linear and quadratic) and sleep quality is important for understanding internalizing and externalizing symptoms associated with sleep in school-age youth. Incorporating self-reported sleep assessments into clinical practice may have implications for a child’s well-being.
Acknowledgements:
Portions of this research were completed with support from the American Psychological Foundation (Elizabeth Munsterberg Koppitz Child Psychology Graduate Student Fellowship, SCE) and the National Institute of Mental Health (K23MH108603, SPB). The content is solely the responsibility of the authors and does not necessarily represent the official views of any funding agency.
Footnotes
We considered whether the extreme observations for time in bed might exert a disproportionate effect on the model compared to other participants (i.e., possible outlier effects). To assess this, we re-estimated all models after dropping the cases with the maximum (14.5 hours) and minimum (5 hours) values. Results showed that nearly all parameter estimates that were previously significant or marginally significant (p < .1) remained within this range (ps = <.001 - .082). The only exception was that the previously marginally significant associations between time in bed and proactive aggression and delinquency became nonsignificant, both with and without the quadratic terms included in the model (all ps > .2). Thus, overall, the results appear to be largely unaffected by extreme values. Accordingly, all model results reported in this paper are based on analyses using all data from the entire sample.
References
- 1.Owens JA and Witmans M, Sleep problems. Curr Probl Pediatr Adolesc Health Care, 2004. 34(4): p. 154–79. [DOI] [PubMed] [Google Scholar]
- 2.Meijer AM, Habekothe HT, and Van Den Wittenboer GL, Time in bed, quality of sleep and school functioning of children. J Sleep Res, 2000. 9(2): p. 145–53. [DOI] [PubMed] [Google Scholar]
- 3.Meijer AM, et al. , Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. J Child Psychol Psychiatry, 2010. 51(11): p. 1278–86. [DOI] [PubMed] [Google Scholar]
- 4.Gregory AM and Sadeh A, Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev, 2012. 16(2): p. 129–36. [DOI] [PubMed] [Google Scholar]
- 5.Lewandowski AS, Toliver-Sokol M, and Palermo TM, Evidence-based review of subjective pediatric sleep measures. J Pediatr Psychol, 2011. 36(7): p. 780–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owens JA, et al. , Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr, 2000. 21(1): p. 27–36. [DOI] [PubMed] [Google Scholar]
- 7.Paavonen EJ, et al. , Sleep problems of school-aged children: a complementary view. Acta Paediatr, 2000. 89(2): p. 223–8. [DOI] [PubMed] [Google Scholar]
- 8.Dayyat EA, et al. , Sleep estimates in children: parental versus actigraphic assessments. Nat Sci Sleep, 2011. 3: p. 115–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becker SP, External validity of children’s self-reported sleep functioning: associations with academic, social, and behavioral adjustment. Sleep Med, 2014. 15(9): p. 1094–100. [DOI] [PubMed] [Google Scholar]
- 10.Matricciani LA, et al. , Never enough sleep: a brief history of sleep recommendations for children. Pediatrics, 2012. 129(3): p. 548–56. [DOI] [PubMed] [Google Scholar]
- 11.Hirshkowitz M, et al. , National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health, 2015. 1: p. 40–43. [DOI] [PubMed] [Google Scholar]
- 12.Sadeh A, Gruber R, and Raviv A, The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev, 2003. 74(2): p. 444–55. [DOI] [PubMed] [Google Scholar]
- 13.Eide ER and Showalter MH, Sleep and Student Achievement. Eastern Economic Journal, 2012. 38: p. 512–524. [Google Scholar]
- 14.Javaheri S, et al. , Association of short and long sleep durations with insulin sensitivity in adolescents. Journal of Pediatrics, 2011. 158: p. 617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yen CF, King BH, and Tang TC, The association between short and long nocturnal sleep durations and risky behaviours and the moderating factors in Taiwanese adolescents. Psychiatry Res, 2010. 179(1): p. 69–74. [DOI] [PubMed] [Google Scholar]
- 16.Lowry R, et al. , Association of Sleep Duration with Obesity among US High School Students. J Obes, 2012. 2012: p. 476914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konen T, Dirk J, and Schmiedek F, Cognitive benefits of last night’s sleep: daily variations in children’s sleep behavior are related to working memory fluctuations. J Child Psychol Psychiatry, 2015. 56(2): p. 171–82. [DOI] [PubMed] [Google Scholar]
- 18.Liu X, et al. , Sleep patterns and sleep problems among schoolchildren in the United States and China. Pediatrics, 2005. 115(1 Suppl): p. 241–9. [DOI] [PubMed] [Google Scholar]
- 19.Gregory AM and Sadeh A, Annual Research Review: Sleep problems in childhood psychiatric disorders - a review of the latest science. J Child Psychol Psychiatry, 2016. 57(3): p. 296–317. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien LM, The neurocognitive effects of sleep disruption in children and adolescents. Child Adolesc Psychiatr Clin N Am, 2009. 18(4): p. 813–23. [DOI] [PubMed] [Google Scholar]
- 21.Johnson EO, Chilcoat HD, and Breslau N, Trouble sleeping and anxiety/depression in childhood. Psychiatry Res, 2000. 94(2): p. 93–102. [DOI] [PubMed] [Google Scholar]
- 22.Becker SP, Ramsey RR, and Byars KC, Convergent validity of the Child Behavior Checklist sleep items with validated sleep measures and sleep disorder diagnoses in children and adolescents referred to a sleep disorders center. Sleep Med, 2015. 16(1): p. 79–86. [DOI] [PubMed] [Google Scholar]
- 23.Alfano CA, et al. , Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress Anxiety, 2009. 26(6): p. 503–12. [DOI] [PubMed] [Google Scholar]
- 24.Gregory AM, et al. , Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics, 2006. 118(3): p. 1124–32. [DOI] [PubMed] [Google Scholar]
- 25.Ivanenko A, et al. , Sleep complaints and psychiatric symptoms in children evaluated at a pediatric mental health clinic. J Clin Sleep Med, 2006. 2(1): p. 42–8. [PubMed] [Google Scholar]
- 26.Gruber R, et al. , Impact of sleep extension and restriction on children’s emotional lability and impulsivity. Pediatrics, 2012. 130(5): p. e1155–61. [DOI] [PubMed] [Google Scholar]
- 27.Soffer-Dudek N, et al. , Poor sleep quality predicts deficient emotion information processing over time in early adolescence. Sleep, 2011. 34(11): p. 1499–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stanger C and Lewis M, Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. Journal of Clinical Child Psychology, 1993. 22(1): p. 107–115. [Google Scholar]
- 29.Phares V, Compas BE, and Howell DC, Perspectives on Child Behavior Problems: Comparisons of Children’s Self-Reports W ith Parent and Teacher Reports. Psychological Assessment, 1989. 1(1): p. 68–71. [Google Scholar]
- 30.Aronen ET, et al. , Sleep and psychiatric symptoms in school-age children. J Am Acad Child Adolesc Psychiatry, 2000. 39(4): p. 502–8. [DOI] [PubMed] [Google Scholar]
- 31.Chervin RD, et al. , Conduct problems and symptoms of sleep disorders in children. J Am Acad Child Adolesc Psychiatry, 2003. 42(2): p. 201–8. [DOI] [PubMed] [Google Scholar]
- 32.Pesonen AK, et al. , Sleep duration and regularity are associated with behavioral problems in 8-year-old children. Int J Behav Med, 2010. 17(4): p. 298–305. [DOI] [PubMed] [Google Scholar]
- 33.Sadeh A, Gruber R, and Raviv A, Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Dev, 2002. 73(2): p. 405–17. [DOI] [PubMed] [Google Scholar]
- 34.Shang CY, Gau SS, and Soong WT, Association between childhood sleep problems and perinatal factors, parental mental distress and behavioral problems. J Sleep Res, 2006. 15(1): p. 63–73. [DOI] [PubMed] [Google Scholar]
- 35.Fallone G, et al. , Experimental restriction of sleep opportunity in children: effects on teacher ratings. Sleep, 2005. 28(12): p. 1561–7. [DOI] [PubMed] [Google Scholar]
- 36.Smedje H, Broman JE, and Hetta J, Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: a study based on parents’ perceptions. Eur Child Adolesc Psychiatry, 2001. 10(1): p. 1–9. [DOI] [PubMed] [Google Scholar]
- 37.Holley S, Hill CM, and Stevenson J, An hour less sleep is a risk factor for childhood conduct problems. Child Care Health Dev, 2011. 37(4): p. 563–70. [DOI] [PubMed] [Google Scholar]
- 38.Matricciani L, Olds T, and Petkov J, In search of lost sleep: secular trends in the sleep time of school-aged children and adolescents. Sleep Med Rev, 2012. 16(3): p. 203–11. [DOI] [PubMed] [Google Scholar]
- 39.Moffitt TE and Caspi A, Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Dev Psychopathol, 2001. 13(2): p. 355–75. [DOI] [PubMed] [Google Scholar]
- 40.Costello EJ, et al. , Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry, 2003. 60(8): p. 837–44. [DOI] [PubMed] [Google Scholar]
- 41.Cronbach LJ, Coefficient alpha and the internal structure of tests. Psychometrika, 1951. 6: p. 297–334. [Google Scholar]
- 42.Zeman J, Shipman K, and Penza-Clyve S, Development and initial validation of the Children’s Sadness Management Scale. Journal of Nonverbal Behavior, 2001. 25: p. 187–205. [Google Scholar]
- 43.Zeman J, Shipman K, and Suveg C, Anger and sadness regulation: Predictions to internalizing and externalizing symptoms in children. Journal of Clinical Child and Adolescent Psychology, 2002. 31: p. 393–398. [DOI] [PubMed] [Google Scholar]
- 44.Irwin DE, et al. , An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Quality of Life Research, 2010. 19: p. 595–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Angold A, et al. , Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 1995. 5: p. 237–249. [Google Scholar]
- 46.Messer SC, et al. , Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: Factor composition and structure across development. International Journal of Methods in Psychiatric Research, 1995. 5: p. 251–262. [Google Scholar]
- 47.Sharp C, Goodyer IM, and Croudace TJ, The Short Mood and Feelings Questionnaire (SMFQ): a unidimensional item response theory and categorical data factor analysis of self-report ratings from a community sample of 7-through 11-year-old children. J Abnorm Child Psychol, 2006. 34(3): p. 379–91. [DOI] [PubMed] [Google Scholar]
- 48.Stringaris A, et al. , The Affective Reactivity Index: A concise irritability scale for clinical and research settings. Journal of Child Psychology and Psychiatry, 2012. 53: p. 1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fergusson DM, Woodward LJ, and Horwood LJ, Childhood peer relationship problems and young people’s involvement with deviant peers in adolescence Journal of Abnormal Child Psychology, 1999. 27: p. 357–369. [DOI] [PubMed] [Google Scholar]
- 50.Rubens SL, et al. , The role of sleep in the relation between community violence exposure and delinquency among Latino adolescents. Journal of Community Psychology, 2014. 42: p. 723–734. [Google Scholar]
- 51.Fite PJ, et al. , Perceived best friend delinquency moderates the link between contextual risk factors and juvenile delinquency. Journal of Community Psychology, 2012(40): p. 747–761. [Google Scholar]
- 52.Cohen J, et al. , Applied multiple regression/correlation analysis for the behavioral sciences, 3rd Edition 2003, New York, NY: Routledge. [Google Scholar]
- 53.Dodge KA and Coie JD, Social-information-processing factors in reactive and proactive aggression in children’s peer groups Journal of Personality and Social Psychology, 1987. 53: p. 1146–1158. [DOI] [PubMed] [Google Scholar]
- 54.Fite PJ, et al. , Longitudinal investigation of the link between proactive and reactive aggression and disciplinary actions. Journal of Psychopathology and Behavioral Assessment, 2011. 33: p. 205–214. [Google Scholar]
- 55.Fite PJ, Stoppelbein L, and Greening L, Proactive and reactive aggression in a child psychiatric inpatient population. J Clin Child Adolesc Psychol, 2009. 38(2): p. 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Enders CK and Bandalos DL, The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 2001. 8: p. 430–457. [PubMed] [Google Scholar]
- 57.Kline RB, Principles and practice of structural equation modeling, 3rd Edition 2011, New York, NY: Guilford. [Google Scholar]
- 58.Muthén LK and Muthén BO, Mplus user’s guide, 7th Edition 2012, Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- 59.Satorra A and Bentler PM, A scaled difference chi-square test statistic for moment structure analysis. Psychometrika, 2001. 66: p. 507–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hu L and Bentler PM, Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 1999. 6: p. 1–55. [Google Scholar]
- 61.Forbes EE, et al. , Objective sleep in pediatric anxiety disorders and major depressive disorder. J Am Acad Child Adolesc Psychiatry, 2008. 47(2): p. 148–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Olds T, et al. , The relationships between sex, age, geography and time in bed in adolescents: a meta-analysis of data from 23 countries. Sleep Med Rev, 2010. 14(6): p. 371–8. [DOI] [PubMed] [Google Scholar]
- 63.Costello EJ, Copeland W, and Angold A, Trends in psychopathology across the adolescent years: what changes when children become adolescents, and when adolescents become adults? J Child Psychol Psychiatry, 2011. 52(10): p. 1015–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matricciani L, et al. , Children’s sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep, 2013. 36(4): p. 527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Devoto A, et al. , Effects of different sleep reductions on daytime sleepiness. Sleep, 1999. 22(3): p. 336–43. [DOI] [PubMed] [Google Scholar]
- 66.Clark LA and Watson D, Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications Journal of Abnormal Psychology, 1991. 100: p. 316–336. [DOI] [PubMed] [Google Scholar]
- 67.Laurent J and Ettelson R, An examination of the tripartite model of anxiety and depression and its application to youth. Clinical Child and Family Psychology Review, 2001. 4: p. 209–230. [DOI] [PubMed] [Google Scholar]
- 68.Bonnet MH and Arand DL, Hyperarousal and insomnia: state of the science. Sleep Med Rev, 2010. 14(1): p. 9–15. [DOI] [PubMed] [Google Scholar]
- 69.Angold A, et al. , Depression scale scores in 8–17-year-olds: Effects of age and gender. Journal of Child Psychology and Psychiatry, 2002. 43: p. 1052–1063. [DOI] [PubMed] [Google Scholar]
- 70.Card NA and Little TD, Differential relations of instrumental and reactive aggression with maladjustment: Does adaptivity depend on function?, in Aggression and Adaptation: The Bright Side to Bad Behavior, Hawley PH, Little TD, and Rodkin PC, Editors. 2007, Lawrence Erlbaum: Mahwah, New Jersey: p. 107–134. [Google Scholar]
- 71.Dodge KA, et al. , Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. Journal of Abnormal Psychology, 1997. 106: p. 37–51. [DOI] [PubMed] [Google Scholar]
- 72.Moffitt TE, et al. , Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology, 2002. 14: p. 179–207. [DOI] [PubMed] [Google Scholar]
- 73.Fite PJ, et al. , Anxiety symptoms account for the link between reactive aggression and sleep problems among Latino adolescents Child and Youth Care Forum, 2015. 44: p. 343–354. [Google Scholar]
- 74.Rubens SL, et al. , The Role of Sleep in the Relation between Community Violence Exposure and Delinquency among Latino Adolescents. Journal of Community Psychology, 2014. 42(6): p. 723–734. [Google Scholar]
- 75.O’Brien EM and Mindell JA, Sleep and risk-taking behavior in adolescents. Behav Sleep Med, 2005. 3(3): p. 113–33. [DOI] [PubMed] [Google Scholar]
- 76.Bertocci MA, et al. , Subjective sleep complaints in pediatric depression: a controlled study and comparison with EEG measures of sleep and waking. J Am Acad Child Adolesc Psychiatry, 2005. 44(11): p. 1158–66. [DOI] [PubMed] [Google Scholar]
- 77.Riley AW, et al. , The Child Report Form of the CHIP-Child Edition: reliability and validity. Med Care, 2004. 42(3): p. 221–31. [DOI] [PubMed] [Google Scholar]
- 78.Mindell JA and Meltzer LJ, Behavioural sleep disorders in children and adolescents. Annals Academy of Medicine Singapore, 2008. 37(8): p. 722–728. [PubMed] [Google Scholar]
- 79.Meltzer LJ, et al. , The Children’s Report of Sleep Patterns (CRSP): a self-report measure of sleep for school-aged children. J Clin Sleep Med, 2013. 9(3): p. 235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]


