Abstract
Background
Intramedullary headless screw (IMHS) has shown promise as an alternative to other fixation devices for metacarpal neck fractures. The purpose of this study was to assess the biomechanical performance of IMHS versus the commonly-used crossed K-wire technique. We hypothesized that IMHS fixation provides superior stability to K-wires.
Methods
A metacarpal neck fracture model in 23 human cadaveric metacarpals was created. The specimens were divided into two groups based upon fixation method: Group 1, 3 mm intramedullary headless screw; and Group 2, 0.045 inch crossed K-wires. A cantilever bending model was used to assess load-to-failure (LTF), maximum displacement, energy absorption, and stiffness.
Results
The mean LTF was 70.6 ± 30.1 N for IMHS and 97.5 ± 34.7 N for crossed K-wires. Mean stiffness was 11.3 ± 3.4 N/mm and 17.7 ± 7.8 N/mm for IMHS and crossed K-wires, respectively. The mean maximum displacement was 20.2 ± 4.6 mm for IMHS and 24.1 ± 3.7 mm for crossed K-wires. Moreover, mean energy absorption was 778.3 ± 528.9 Nmm and 1095.9 ± 454.4 Nmm, respectively, for IMHS and crossed K-wires. Crossed K-wires demonstrated significantly higher stiffness and maximum displacement than IMHS (p < 0.05).
Conclusions
IMHS fixation of unstable metacarpal neck fractures offers less stability compared to crossed K-wires when loaded in bending.
Clinical Relevance
Crossed K-wires offer superior stability for the treatment of metacarpal neck fractures. These results reveal that IMHS fixation is less favorable biomechanically and should be cautiously selected with regards to fracture stability.
Keywords: Biomechanical, fracture, intramedullary, metacarpal neck
Introduction
Metacarpal fractures are common injuries treated by the orthopaedist and hand surgeon. They are third in frequency in fractures of the hand and forearm, behind radius/ ulna fractures and phalangeal fractures, comprising 18% of these injuries as a whole.1 The majority of metacarpal fractures can often be treated non-operatively, with some combination of splinting, casting, buddy taping, and/ or early motion protocols. Non-operative treatment is not without its limits, however, as it is difficult to maintain rotational stability and length with this technique. This is particularly critical since it has been shown that for every 2 mm of shortening, a resulting extensor lag of 7° will occur that may lead to a “pseudoclawing” appearance.2 Operative indications for metacarpal neck fractures have differed in the literature, but most employ acceptable reduction parameters of no rotational deformity and angulation of 15° at the index finger, 20° at the middle, 30° at the ring, and 40 – 50° at the small, with published ranges of 20 – 70° for the small finger.3
In order to treat those fractures amenable to surgical intervention, numerous open and closed operative techniques for managing unstable metacarpal fractures have been proposed. These include, but are not limited to, closed reduction with percutaneous pinning in varying configurations, percutaneous insertion of locked or non-locked intramedullary nails, intramedullary wires, and open reduction with screws alone or plate/ screw constructs.4,6 Each method has presented with its own unique complication profile, such as wire tract infection, hardware prominence, and extensor tendon irritation, while all are associated with varying degrees of malunion, nonunion, and infection.7 Headless screws have been used for fixation of other hand fractures, carpal injuries, and radial head fractures with success seen in these arenas.8,10 Intramedullary headless screws have been applied to metacarpal shaft fractures as well as comminuted sub-capital fractures with success.4 Advantages of percutaneous, intramedullary headless screw fixation include minimal soft tissue dissection, rigid fixation in the distal fragment and isthmus of the metacarpal, and limited required immobilization time to prevent the stiffness that occurs all too commonly in these injuries. Mechanical analyses of the headless screw technique, however, are sparse and conflicting within the literature.11,12
The objective of the present study was to compare the biomechanical characteristics of intramedullary headless screw (IMHS) fixation with crossed K-wires (CKW) in metacarpal neck fractures. We hypothesized that IMHS is biomechanically superior to the percutaneous CKW construct.
Methods
Twenty-three age-matched cadaveric metacarpal specimens were used in this study. Specifically, metacarpals two (index), three (middle), four (ring), and five (small) were utilized. In order to introduce a replicable fracture, a transverse osteotomy was performed using a precision, thin-blade oscillating saw at the metacarpal neck of each specimen. A smooth osteotomy cut was
created in order to mitigate the challenges of reproducing the same interdigitating pattern among numerous osteotomies. Each of metacarpal specimens was then randomly assigned to undergo fixation by one of two distinct constructs. Eleven of the specimens were assigned to receive IMHS fixation while the remaining 12 underwent CKW pinning. The IMHS implants used were Medartis 3 mm CCS Speedtip screws (Basel, Switzerland). After over-drilling the metacarpal head with a cannulated drill bit, the screws were inserted in a retrograde manner with the guide wire placed in the dorsal, central half of the metacarpal in line with the intramedullary canal to a depth of approximately 1 mm below the level of the articular surface (Figure 1). CKW implants were 0.045 inches in diameter, non-threaded wires and were placed retrograde with a starting point at the collateral recess with care taken to engage the far cortex with the wire (Figure 2).
Figure 1.
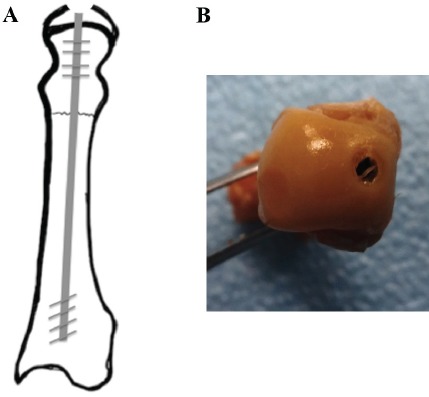
Schematic of intramedullary headless compression screw across metacarpal neck fracture.
Figure 2.
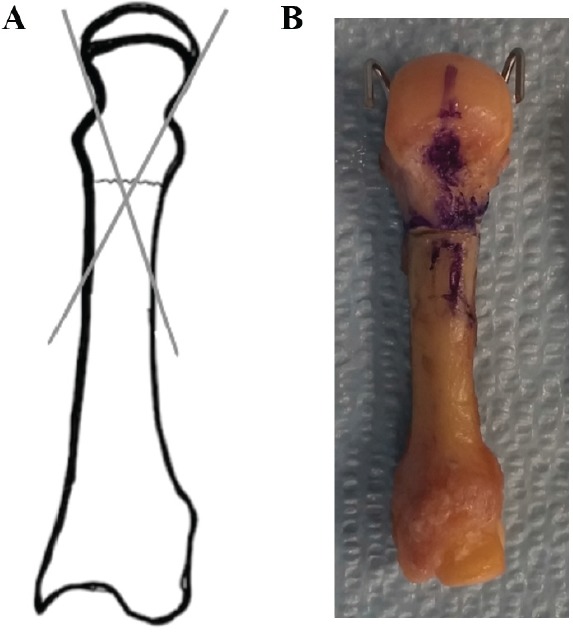
Schematic of placement of crossed K-wires, engaging the far cortex.
Each specimen was tested with a bending moment provided by a servo-hydraulic testing machine (MTS 858 Mini Bionix, MTS Systems, Corp.; Eden Prairie, MN), as seen in Figure 3, and loaded to failure at the distal fragment. Failure was defined as a distinct change in the load-displacement curve, and the load was incrementally increased until the fixation construct failed by implant deformity, loss of reduction, or metacarpal fracture. Mechanical parameters that were calculated and recorded included stiffness (slope of the linear portion of the stress/ strain curve, N/ mm), load-to-failure (N), maximum displacement (displacement at failure, mm), and energy absorption (area under the curve, Nmm).
Figure 3.
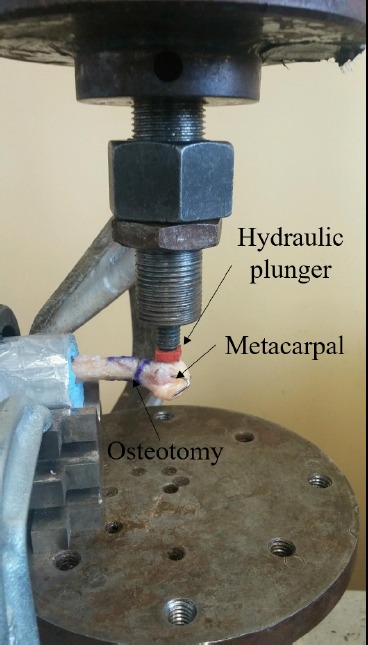
MTS machine with metacarpal mounted.
Data are presented as mean and standard deviation (SD). For statistical analyses, groups were initially assessed for normality of distribution using the Kolmogorov-Smirnov test and then compared using an unpaired student’s t-test. For those variables failing the normality test, a nonparametric Mann-Whitney U Test was implemented. R-project statistical software (R Foundation, Boston, MA) were used for all statistical analyses. A p-value of less than 0.05 was considered to be significant.
Results
The biomechanical characteristics of both IMHS and CKW constructs are shown in Table 1. Of the fixation constructs, CKW demonstrated a higher stiffness (17.7 N/ mm) than IMHS (11.3 N/ mm). This difference was statistically significant (p = 0.02).
Table I.
Biomechanical characteristics of both fixation constructs
| IMHS | CKW | ||||
|---|---|---|---|---|---|
| Parameter | Mean (SD) | Range | Mean (SD) | Range | P-Value |
| Stiffness (N/mm) | 11.3 (3.4) | 5.8 - 16.2 | 17.7 (7.8) | 5.9 - 30.1 | 0.02 |
| Load-to-Failure (N) | 70.6 (30.1) | 32.8 - 123.8 | 97.5 (34.7) | 41.8 - 157.5 | 0.06 |
| Maximum Displacement (mm) | 20.2 (4.6) | 11.5 - 26.4 | 24.1 (3.7) | 19 - 30 | 0.04 |
| Energy Absorption (Nmm) | 778.3 (528.9) | 272.9 – 1,790.5 | 1,095.9 (454.4) | 397.8 – 1,933.3 | 0.14 |
IMHS, intramedullary headless screw; CKW, crossed K-wires; N, newtons; mm, millimeters; SD, standard deviation
Further analysis was performed of the load-to-failure. As with stiffness characteristics, CKW had a higher load-to-failure (97.5 N) compared to IMHS (70.6 N). However, this finding only trended toward, but did not achieve, statistical significance (p = 0.06).
The displacement at the time of failure was also evaluated. As with the other aforementioned parameters, CKW had a greater maximum displacement (24.1 mm) than IMHS (20.2 mm). This difference was statistically significant (p = 0.04).
Additionally, CKW had approximately 40% higher energy absorption (1,095.9 Nmm) when compared to IMHS (778.3 Nmm). Like the load-to-failure analysis, however, this difference was not statistically significant (p = 0.14).
Discussion
Of metacarpal fractures, the most common injury pattern is a metacarpal neck fracture, particularly among younger, active patients. Indications for surgery are largely dictated by the degree of dorsal angulation, with the more radial digits tolerating less deformity due to their more rapid decrease in grip strength with increasing angulation compared to the ulnar digits, as well as presence of a rotational deformity. With surgical complication rates as high as 36%, there appears to be no definitive consensus on the ideal fixation method for metacarpal neck fractures.13
Our results demonstrate the biomechanical superiority of CKW as compared to IMHS for the treatment of metacarpal neck fractures. This was evidenced by the significantly higher stiffness and maximum displacement required to induce construct failure with CKW fixation. Of note, consistent with this trend was the observation that CKW constructs also had higher load-to-failure values and energy absorption, although these two characteristics were not statistically significant. Overall, these findings indicate that CKW confers a more stable construct than IMHS. This contrasts with the limited extant literature, which includes only two studies investigating the mechanics of IMHS. Jones et al performed a comparative mechanical analysis of IMHS, CKW, and locking plate fixation for the treatment of metacarpal neck fractures in 30 specimens.12 Similar to the present study, they found no difference in the load-to-failure between the constructs. However, unlike the current investigation, they reported a higher stiffness with IMHS compared to CKW and similar maximum displacement between both. Their use of composite Sawbones instead of cadaveric specimens could account for such differences. Ultimately, Jones et al concluded that both methods provide comparable mechanical fixation properties. Additionally, Avery et al conducted a biomechanical evaluation of cadaveric metacarpal neck fractures treated with either IMHS or intramedullary K-wire fixation.11 They found IMHS to be superior in 3-point bending, axial loading, and load-to-failure. However, their analysis included a limited mechanical evaluation of only stiffness and load-to-failure, whereas the present study performed a more robust assessment with four parameters. Also, as noted, Avery et al compared IMHS to longitudinally-oriented intramedullary K-wires, which is an inherently different K-wire configuration than CKW. Other fixation methods for metacarpal neck fractures, such as the metacarpal sled, locking plate, and various other K-wire configurations have demonstrated comparable biomechanical profiles.14,16
While the findings of the present study indicate that the more traditional fixation method of CKW yields superior mechanical stability, recent clinical studies investigating IMHS have sparked interest in this newer technique. In a small series examining the short-term (average of 36 weeks) results of metacarpal neck and shaft fractures treated with IMHS, Doarn et al showed a mean return to work at six weeks and radiographic healing at 49 days.17 They supported the use of IMHS for these injuries due to the advantages of early motion without immobilization and relative technical ease. In another, larger series, 39 patients were evaluated after undergoing IMHS with 3-month follow-up.18 All patients had full motion with extensor lags resolving by three weeks, with full return of grip strength and radiographic union by six weeks. Concerns regarding the use of IMHS fixation include the necessary violation of the articular surface of the metacarpal with the drill and the implant. This was evaluated using 3-dimensional CT analysis and determined that the recommended dorsal starting point for the IMHS involved only 4% of the articular surface in the sagittal plane of motion and did not engage through most of this arc.19
This study, however, is not with its limitations. Specifically, the present study employed a relatively small sample size. Nonetheless, the sample size is similar to those utilized in other metacarpal fracture fixation studies, and it was large enough to detect multiple statistically significant differences between the two study groups.11, 12 Additionally, as the specimens were cadaveric, they were likely largely from older patients as compared to the typically younger patient who sustains a metacarpal neck fracture. Also, as the specimens were from various patient donors, there may be inherent differences in structural characteristics between the metacarpals, such as the bone mineral density, which could impact the mechanical testing results.
The biomechanical properties of the CKW technique were found to be superior to those of IMHS. This, coupled with their lower cost compared to the implants utilized in other fixation methods (such as IMHS and plate constructs), make CKW a preferred technique. However, the amount of strength required for stable fixation in the clinical setting has not been determined. Thus, biomechanically inferior constructs such as IMHS may be suitable for fixation and should be customized to the particular fracture. Given this, as well as the relative ease of insertion of the IMHS implants, the avoidance of postoperative immobilization, and the clinical outcomes as reported in the previously-cited studies, IMHS should still be placed in the surgeon’s toolbox for the treatment of metacarpal neck fractures.
Source of Funding
The authors received no funding for this study.
References
- 1.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 2.Strauch RJ, Rosenwasser MP, Lunt JG. Metacarpal shaft fractures: the effect of shortening on the extensor tendon mechanism. J Hand Surg Am. 1998;23(3):519–523. doi: 10.1016/S0363-5023(05)80471-X. [DOI] [PubMed] [Google Scholar]
- 3.Stern P. Fractures of the Metacarpals and Phalanges. In: Green DP, Pederson WC , Wolfe SW, eds. Operative Hand Surgery. 5th ed. New York:: Churchill Livingstone; 2005.. [Google Scholar]
- 4.Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(8):1260–1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 5.Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000;8(2):111–121. doi: 10.5435/00124635-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Orbay J. Intramedullary nailing of metacarpal shaft fractures. Tech Hand Up Extrem Surg. 2005;9(2):69–73. doi: 10.1097/01.bth.0000167253.31976.95. [DOI] [PubMed] [Google Scholar]
- 7.Kollitz KM, Hammert WC, Vedder NB, Huang JI. Metacarpal fractures: treatment and complications. Hand (N Y) 2014;9(1):16–23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Geissler WB. Cannulated percutaneous fixation of intra-articular hand fractures. Hand Clin. 2006;22(3):297–305. doi: 10.1016/j.hcl.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Hotchkiss RN. Displaced Fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5(1):1–10. doi: 10.5435/00124635-199701000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Rutgers M, Mudgal CS, Shin R. Combined fractures of the distal radius and scaphoid. J Hand Surg Eur Vol. 2008;33(4):478–483. doi: 10.1177/1753193408090099. [DOI] [PubMed] [Google Scholar]
- 11.Avery DM3rd,, Klinge S, Dyrna F, et al. Headless compression screw versus kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am. 2017;42(5):392.. doi: 10.1016/j.jhsa.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 12.Jones CM, Padegimas EM, Weikert N, Greulich S, Ilyas AM, Siegler S. Headless screw fixation of metacarpal neck fractures: a mechanical comparative analysis. Hand (N Y) 2017. 1558944717731859. [DOI] [PMC free article] [PubMed]
- 13.Padegimas EM, Warrender WJ, Jones CM, Ilyas AM. Metacarpal neck fractures: a review of surgical indications and techniques. Arch Trauma Res. 2016;5(3) doi: 10.5812/atr.32933. e32933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malasitt P, Owen JR, Tremblay MA, Wayne JS, Isaacs JE. Fixation for metacarpal neck fracture: a biomechanical study. Hand (N Y) 2015;10(3):438–443. doi: 10.1007/s11552-015-9744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Facca S, Ramdhian R, Pelissier A, Diaconu M, Liverneaux P. Fifth metacarpal neck fracture fixation: Locking plate versus K-wire? Orthop Traumatol Surg Res. 2010;96(5):506–512. doi: 10.1016/j.otsr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Wong TC, Ip FK, Yeung SH. Comparison between percutaneous transverse fixation and intramedullary K-wires in treating closed fractures of the metacarpal neck of the little finger. J Hand Surg Br. 2006;31(1):61–65. doi: 10.1016/j.jhsb.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 17.Doarn MC, Nydick JA, Williams BD, Garcia MJ. Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Hand (N Y) 2015;10(2):314–318. doi: 10.1007/s11552-014-9620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ruchelsman DE, Puri S, Feinberg-Zadek N, Leibman MI, Belsky MR. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390–2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Bergten PW, Mudgal CS, Leibman MI, Belsky MR, Ruchelsman DE. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(2):322–330. doi: 10.1016/j.jhsa.2012.09.029. [DOI] [PubMed] [Google Scholar]


